What do we already know about this topic?
The mass shadow in the superior lung field of a neonate is often the thymus, and extralobar pulmonary sequestration is generally present in the inferior left lobe.
How does your research contribute to the field?
It clarifies the points to be noted in the inspection and shows the procedure of the inspection with less invasiveness.
What are your research’s implications toward theory, practice, or policy?
Obtaining maximum information from routine tests will reduce the potential invasion of children.
Introduction
The shadow of the superior lung field with positive-silhouette sign, which is generally observed on a chest radiograph during the neonatal period, is often the normal thymus because it occupies a large proportion in the thoracic cavity.1 Furthermore, majority of the extralobar pulmonary sequestration (EPS) lies between the diaphragm and the lower lobe and is relatively rare in the superior mediastinum.2 On the other hand, in majority of neonatal care, routine tests are performed at the time of admission regardless of the chief complaint. These reveal a great deal of useful information about children who are unable to communicate their symptoms. Herein, we report a coincidental case of EPS without silhouette sign thymus-like shadows in the superior mediastinum.
Case Presentation
A 0-day-old boy with no abnormalities at the time of delivery was referred to the neonatal intensive care unit (NICU) due to low blood glucose level for 1 hour after birth. His mother underwent regular medical examinations, including ultrasonography, from the 14th week of pregnancy; however, no problems were detected. He was born in the Obstetrics Department by a scheduled Cesarean section at a gestational age of 38 weeks and 3 days and weighed 3534 g (+1.54 SD), Apgar score of 9/10 (1/5 minute) at birth. The hypoglycemia improved immediately after NICU admission with continuous administration of 10% glucose; thereafter, the patient’s course was uneventful without any hypoglycemia or other symptoms. Vital signs were normal at the time of admission (heart rate, 135 bpm; respiratory rate, 54 bpm; blood pressure, 59/37 mmHg). Front chest/abdominal radiography was performed as indicated for screening patients with hypoglycemia without respiratory symptoms. No abnormalities were found from the physical findings, and the breathing sound was normal, so no images were taken from lateral side. The mass shadow that appeared in the right superior lung field seemed reminiscent of the thymus at first glance because the contour and trachea/cardiac shadow were not displaced. However, on further consideration, a silhouette sign that would normally be impossible would be negative if it were a thymus (Figure 1). Ultrasound was performed from the back, and a solid, uniform, high-echogenicity mass was observed. At the same time, pulsatile blood vessels flowing into the mass were observed; however, visualization was difficult due to the thoracic spine and the origin was not identified (Figure 2A). The next a magnetic resonance imaging (MRI) scan revealed a mass clearly, however even with this, the inflowing blood vessels could not be visualized (Figure 2B). Additional contrast-enhanced computed tomography (CT) examinations identified EPS based on the feeding arteries from the aorta (Figure 2C) and the draining veins into azygos vein, the trachea without communication. No complications such as lung hypoplasia and congenital heart malformations were found. The patient gained weight during hospitalization and was discharged without signs of infection or respiratory problems. A follow-up examination will be planned in the future to determine further management.
Figure 1.

Circular mass shadow in the right superior lung field without silhouette sign by chest-abdominal radiograph examination.
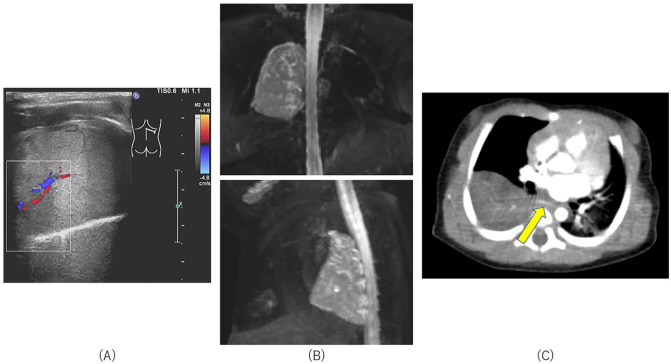
Figure 2.
(A) In ultrasonography, a mass with uniform internal structure and high-echogenicity and blood vessels flowing into the mass at day 0. (B) A mass of 30 × 31 × 52 mm with a clear boundary (viewed from the front: horizontal diameter × vertical diameter × height) in the region that was in contact with the thoracic cage of the right superior lung lobe by Magnetic resonance imaging at day 7. (C) Abnormal blood vessels extending from the aorta to the extralobar pulmonary sequestration (arrow point) as observed on contrast computed tomography examination at day 13.
Discussion and Conclusion
The interpretation of the chest radiograph is important for pediatric physicians, and knowledge of the silhouette sign is useful to evaluate the lesion location and plan sequential examinations. Although ultrasound, CT and MRI have been recently recognized as useful diagnostic tools, the plain chest radiograph remains a basic tool for the assessment of pediatric patients. Pediatricians should get as much information as possible from this tool. This is because it is necessary to recognize that repeated radiograph and CT examinations are synonymous with radiation exposure. The CT needed for diagnosis is approximately 85 times more exposed than the chest radiograph.3 Filming during the sensitive childhood phase increases the risk of subsequent leukemia and tumors.4 Therefore, it is acceptable only if the profits outweigh it, but a solid strategy is required to support that point.
The silhouette sign is a classical method reported by Felson et al,5 when the organ or mass is anatomically adjacent to the heart or large blood vessels, the boundary is obscured and is called the “silhouette sign positive.” The thymus is a pair of left and right organs that primarily originate from the third pharyngeal pouches and descends the anterior mediastinum along the parietal pericardium. It is generally known that the normal thymus increases in size from the sixth week of life of the fetus until adolescence and then regresses gradually.6 Therefore, the right thymus in the anterior mediastinum obscures the right cardiac border; that is, the silhouette sign is positive. During the neonatal period, it is projected as a mass shadow because it is relatively large with respect to the rib cage as observed on a chest radiograph. Siegel et al1 reported that the normal infant thymus size as 2.68 cm (±0.7 cm) to the right and 2.97 cm (±0.7 cm) to the left. These typical findings are “wave sign” and “sail signs,” but atypical round images are often drawn. In this case, the shape and size of the shadow and the image without exclusion to the surrounding area were consistent with the thymus. However, the silhouette sign was negative and further examination led to the diagnosis.
In recent years, abnormalities in the fetus have been discovered early in pregnancy due to the improved image resolution of the ultrasonic tomography apparatus. Therefore, almost all congenital thoracic malformations can be found using prenatal ultrasound.7 However, pediatricians must be aware of these illnesses because prenatal diagnosis is not perfect. Pulmonary sequestration occurs when excess lung buds develop on the caudal side of normal lung buds and move to the caudal side with the development of the esophagus. Although the prognosis is generally uneventful, there is a space-occupied lesion in the thoracic cavity that may cause lung compression, resulting in lung hypoplasia that hinders maturation. Furthermore, this condition has been classified into intralobar [84.0% (1873/2231)] and extralobar [16.0% (358/2231)] subtypes based on the presence or absence of common visceral pleura, respectively,2 and most of the EPS [77.4% (103/133)] is detected on the left side and in the lower lung field [78.9% (105/133)].8 Surgery is a common treatment option as it is possible that the torsion of the feeding vessels may occur due to the absence of lung ligaments that fix the fractionated lungs. However, certain cases remain asymptomatic throughout life, and the timing of the appropriate surgery has not yet been confirmed.9 Regarding the present case, because EPS was detected by radiograph without any symptoms after birth, future adverse events can be predicted and managed more carefully.
To summarize, even asymptomatic EPS, which resembles the thymus, can be diagnosed by careful interpretation of the chest radiograph. However, this case was not pathologically evaluated. Further investigation of the accumulation sites and clinical symptoms of this disease is required.
Footnotes
Author Contributions: TN mainly drafted the manuscript and made the Figure; TN and NI contributed to the conception and design of this report; SS, MK, and KM critically reviewed the manuscript; MM supervised the whole process. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Consent for Publication: Informed consent was obtained from the parent. The patient’s records/information were anonymized to protect the confidentiality of the patient’s personal information.
ORCID iD: Tomohiko Nishino  https://orcid.org/0000-0003-4287-979X
https://orcid.org/0000-0003-4287-979X
References
- 1.Siegel MJ, Glazer HS, Wiener JI, Molina PI.Normal and abnormal thymus in childhood: MR imaging. Radiology. 1989;172:367-371. [DOI] [PubMed] [Google Scholar]
- 2.Wei Y, Li F.Pulmonary sequestration: a retrospective analysis of 2625 Cases in China. Eur J Cardiothorac Surg. 2011;40:e39-e42. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Communicating radiation risks in paediatric imaging; information to support healthcare discussions about benefit and risk. 2016. Accessed on November 26, 2020. https://www.who.int/ionizing_radiation/pub_meet/radiation-risks-paediatric-imaging/en/
- 4.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Felson B, Felson H.Localization of intrathoracic lesions by means of the postero-anterior roentgenogram; the silhouette sign. Radiology. 1950;55:363-374. [DOI] [PubMed] [Google Scholar]
- 6.Shah SS, Lai SY, Ruchelli E, Kazahaya K, Mahboubi S.Retropharyngeal aberrant thymus. Pediatrics. 2001;108:E94. [DOI] [PubMed] [Google Scholar]
- 7.Annunziata F, Bush A, Borgia F, et al. Congenital lung malformations: unresolved issues and unanswered questions. Front Pediatr. 2019;7:239. doi: 10.3389/fped.2019.00239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Savic B, Birtel FJ, Tholen W, Funke HD, Knoche R.Lung sequestration: report of seven cases and review of 540 published cases. Thorax. 1979;34:96-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robson VK, Shieh HF, Wilson JM, Buchmiller TL.Non-operative management of extralobar pulmonary sequestration: a safe alternative to resection? Pediatr Surg Int. 2020;36:325-331. [DOI] [PubMed] [Google Scholar]