Abstract
Introduction:
During the coronavirus disease 2019 (COVID-19) pandemic, primary and secondary healthcare workers (HCWs) have faced unprecedented stress, jeopardizing their mental well-being.
Aims:
To compare risk perception and psychological distress between primary and secondary HCWs.
Method:
A cross-sectional web-based survey was conducted with HCWs in Qatar from April 5 to July 5, 2020. Psychological distress and risk perception were assessed using the Kessler Psychological Distress Scale, a perceived COVID-19 risk questionnaire, and a sociodemographic questionnaire.
Results:
Of the 4417 participating HCWs, 3421 (90.3%) felt that their job increased their risk of COVID-19 exposure, 3759 (90.9%) accepted this as part of their job, and 3440 worried that this also increased the risk of exposure to their families. Moreover, 2911 (84.8%) believed that their employer would look after their needs if they contracted COVID-19. Moderate to severe psychological distress was present in 1346 (30.5%) HCWs. Primary HCWs were less likely to experience moderate to severe psychological distress than secondary HCWs (adjusted OR, 0.48; 95% CI 0.29-0.77, P = .003). Secondary HCWs who worked in COVID-19 designated areas had greater psychological distress.
Conclusions:
HCWs’ exposure to outbreaks has various psychological effects, which may have long-term consequences and affect their decision-making capacity. Strategies to enhance the mental well-being of HCWs exposed to COVID-19 should be introduced immediately.
Keywords: COVID-19, primary healthcare worker, psychological distress, risk perception, secondary healthcare worker
Introduction
The coronavirus disease of 2019 (COVID-19) broke out in Wuhan (Hubei, China) in December 2019; since then, a significant number of COVID-19 cases have been reported worldwide, and the World Health Organization (WHO) declared COVID-19 as a pandemic on March 11, 2020.
Thousands of health care workers (HCWs) worldwide face coronavirus disease 2019 (COVID-19) directly or indirectly during patient care, which places them under tremendous pressure. Research conducted during the COVID-19 pandemic has shown that, among HCWs in China, 50.3% experienced depression, 44.6% experienced anxiety, and 34.0% experienced insomnia.1 A study in Italy found that 49.38% of HCWs reported post-traumatic stress disorder symptoms, 24.73% severe depression, 19.80% anxiety, 8.27% insomnia, and 21.90% high perceived stress.2 A recent study from Qatar reported high perceived stress and PTSD symptoms among intensive care unit staff caring for COVID-19 infected patients.3 The health, safety, and mental well-being of HCWs are crucial not only for ensuring continuous and consistent patient care but also for containment of outbreaks.4 Previous studies during the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome outbreaks showed that HCWs experienced extreme stress related to the risk of infection, stigmatization, understaffing, and uncertainty; additionally, extensive support provision for HCWs was a major concern during and after the outbreaks.5,6 Furthermore, a meta-analysis of the psychological reactions of HCWs in previous outbreaks has shown the impact of personal caregiving and socioeconomic stressors; for instance, having children at home, an infected family member, and a lower household income were associated with adverse mental health outcomes.7 The World Health Organization (WHO)8 identifies healthcare institutions as central during a pandemic, as they provide protection for HCWs through initiatives to monitor infections, personal safety protocols, and anti-viral medications; WHO recommends ensuring sufficient resources for frontline HCWs because maintaining their mental and psychosocial well-being during this period is as critical as ensuring their physical health. HCWs are routinely exposed to the risk of infection; accordingly, concerns about spreading infections to their own families and co-workers may place further pressure on them.
The Current Study
Qatar’s healthcare service is divided into primary, secondary, and tertiary care. HCWs during a pandemic may perform roles that alternate between primary and secondary care systems; specifically, the primary care system provides outpatient services to the public, and suspected cases of COVID-19 are automatically moved to secondary care, which offers round-the-clock, multidisciplinary, and acute inpatient services, including the use of intensive care units. Therefore, secondary HCWs tend to have more extended contact with COVID-19 patients, as they are involved in treating severely ill patients, potentially increasing their perceived risk and psychological distress. However, primary HCWs may be at a higher risk of contracting COVID-19 than secondary HCWs because they are first exposed to the general public, who may not be aware of their COVID-19 status; meanwhile, secondary HCWs usually receive pre-arrival notice about patients to be better prepared to deal with specific cases. Our research aimed to examine risk perception, the prevalence and severity of psychological distress among HCWs, and compare these between primary and secondary healthcare settings.
Methods
Participants
The Primary Health Care Corporation (PHCC) provides primary outpatient care through 27 primary health care centers distributed across 3 regions: Central, Western, and Northern Qatar. The Hamad Medical Corporation (HMC) is the main secondary and tertiary healthcare system and is one of the leading hospital service providers in the Middle East; it manages 12 hospitals, the National Ambulance Service, and home and residential care services.
This cross-sectional survey was conducted between April 5 and July 5, 2020, during the peak of the COVID-19 pandemic in Qatar. In total, 4606 responses were received. Of the 760 surveys received from primary care settings, 14 had incomplete answers and were excluded; 746 completed questionnaires were analyzed. In total, 3846 responses were received from secondary care settings; we eliminated 175 that had incomplete answers, including 3671 complete questionnaires in the analysis.
Ethical Statement
All procedures involving human participants were approved by the Medical Research Centre, HMC (approval number: MRC-01-20-170). Participation in this study was voluntary, and anonymity was assured. All participants were informed that their decision to participate would be considered as their consent to participate in and complete the survey.
Measures
The Kessler Psychological Distress Scale (K10) is a well-validated clinical measure of psychological distress with high factorial and construct validity. It has 10 questions, and each answer is scored from 1 (none of the time) to 5 (all of the time). Scores for the 10 questions are summed, yielding a minimum score of 10 and a maximum of 50. High scores indicate high levels of psychological distress.9
The 2001 Victorian Population Health Survey10 adopts a set of cut-off scores to identify the likelihood of having a mental disorder (in this study, psychological distress). Scores were interpreted as: 10 to 19 = likely to be well, 20 to 24 = mild, 25 to 29 = moderate, and 30 to 50 = severe disorder.
COVID-19 risk perception in the work and personal lives of HCWs was evaluated by a set of self-administered questions adapted from the questionnaire used in a survey on risk perception and impact of SARS on work and personal lives of HCWs in Singapore.11 This questionnaire has been used in studies conducted in Asia and the Middle East.12-14 The questions were adapted to meet the objectives of our research. The questionnaire included 23 questions: 7 on personal concerns, 4 on family, and 12 on work; these items were measured as yes, no, or not sure. Cronbach’s alpha coefficient value was calculated to determine and assess the reliability and internal consistency of the risk perception questionnaire, which was found to be 0.83 (95% confidence interval [CI] 0.811-0.842), indicating good reliability and internal consistency. Content validity was assessed by clinical subject matter experts, and it was found that the above-mentioned tool was adequate to use in addressing such concerns. Even though K10 is a well-validated tool, Cronbach’s alpha was calculated to check the internal consistency and reliability of the questionnaire in this population and was found to be 0.95 (95% CI: 0.948-0.952), indicating strong reliability and internal consistency.
A sociodemographic questionnaire collected data on age, sex, marital status, whether the respondent had children, whether the respondent lived with his/her family, job designation, place of work, and whether the respondent worked in a COVID-19-designated site.
Statistical Analysis
Quantitative and categorical data were presented as mean ± standard deviation and frequency (percentage). Associations between 2 or more qualitative variables were assessed using the chi-square (χ2) test or Fisher’s Exact test. Univariate and multivariate logistic regression analyses (adjusted for potential predictors and confounders) were applied to determine and assess the predictive value of potential predictors and risk factors (demographic characteristics and variables related to risk perception) associated with moderate to severe psychological distress. The results of logistic regression analyses were presented as odds ratio (OR) with corresponding 95% CI. All P-values were 2-tailed, and P-values <.05 were considered statistically significant. Statistical analyses were conducted using SPSS 24.0 (SPSS Inc. Chicago, IL) and Epi-info (Centers for Disease Control and Prevention, Atlanta, GA).
Results
Most respondents were women (n = 2920; 66.1%), between the ages of 20 and 44 years (n = 3549; 80.3%), married (n = 3389; 76.7%), living with their families (n = 3236; 73.3%), and had children (n = 3109; 70.4%). The majority were nurses (n = 3285; 74.4%), followed by doctors (n = 857; 19.4%) and paramedics (n = 275; 6.2%). More than half of the respondents (n = 2349; 53.2%) worked in COVID-19-designated areas. The comparison of sociodemographic characteristics of primary and secondary HCWs is presented in Table 1.
Table 1.
Baseline Sociodemographic Characteristics of Primary and Secondary Healthcare Workers.
| Sociodemographic variables | PC (n = 746) n (%) | SC (n = 3671) n (%) | Total (N = 4417) n (%) | χ2 | P value |
|---|---|---|---|---|---|
| Age (years) | |||||
| 20-34 | 276 (37.0) | 1789 (48.7) | 2065 (46.8) | 38.79 | <.0001 |
| 35-44 | 280 (37.5) | 1204 (32.8) | 1484 (33.6) | ||
| 45-54 | 153 (20.5) | 526 (14.3) | 679 (15.4) | ||
| 55-65+ | 37 (5.0) | 152 (4.1) | 189 (4.3) | ||
| Sex | |||||
| Male | 234 (31.4) | 1263 (34.4) | 1497 (33.9) | 2.55 | .110 |
| Female | 512 (68.6) | 2408 (65.6) | 2920 (66.1) | ||
| Marital status | |||||
| Single | 90 (12.1) | 783 (21.3) | 873 (19.8) | 34.92 | <.0001 |
| Married | 622 (83.4) | 2767 (75.4) | 3389 (76.7) | ||
| Divorced/separated/widowed | 34 (4.6) | 121 (3.3) | 155 (3.5) | ||
| Children | |||||
| Yes | 588 (78.8) | 2521 (68.7) | 3109 (70.4) | 30.63 | <.0001 |
| No | 158 (21.2) | 1150 (31.3) | 1308 (29.6) | ||
| Living with family | |||||
| Yes | 627 (84.0) | 2609 (71.1) | 3236 (73.3) | 53.31 | <.0001 |
| No | 119 (16.0) | 1062 (28.9) | 1181 (26.7) | ||
| Occupation | |||||
| Doctor | 212 (28.4) | 645 (17.6) | 857 (19.4) | 33.11 | <.0001 |
| Nurse | 534 (71.6) | 2751 (74.9) | 3285 (74.4) | ||
| Paramedic | 0 | 275 (7.5) | 275 (6.2) | ||
| Working in a COVID-19 designated area | |||||
| Yes | 448 (60.0) | 1901 (51.8) | 2349 (53.2) | 17.03 | <.0001 |
| No | 298 (40.0) | 1770 (48.2) | 2068 (46.8) | ||
Abbreviations: PC, primary care; SC, secondary care.
Risk Perception Among Primary and Secondary HCWs
Personal concerns
Most primary and secondary HCWs (n = 3421; 90.3%) felt that their jobs put them at greater risk of exposure to COVID-19 and 75.9% (n = 2992) were concerned about contracting COVID-19. However, 90.9% (n = 3759) of HCWs accepted that the risk of contracting COVID-19 was part of their job, while 15.2% (n = 550) felt that they should not be looking after COVID-19 patients. Additionally, 8.7% (n = 342) of HCWs reported that they might look for another job because of the risk involved. About 67% (n = 2671) felt torn between the dedication to their job and responsibility toward their loved ones. Nearly 51.9% (n = 2109) spent their time thinking about the COVID-19 pandemic. There were no significant differences between primary and secondary HCWs.
Family-related concerns
Of the overall HCWs, 90.4% (n = 3808) felt that their family could be worried about their health and most (84.4%; n = 3440) were worried that their family could be at higher risk of contracting COVID-19 owing to their job. Around three-quarters (76.3%; n = 3232) were concerned about talking to their families about the risk to which they were exposed. Nearly half of HCWs (48.4%; n = 1818) felt that people would stigmatize them and their families owing to their job. No statistically significant differences were found between the 2 HCW groups.
Work-related concerns
Most primary and secondary HCWs (84.8%, n = 2911) were confident that their employer would look after their needs if they contracted COVID-19. Three-quarters of the HCWs were worried that there would be inadequate staff to handle the increased demand. They also anticipated increased workloads, working overtime, and even having to do work not generally included in their job description. Additionally, 37.1% (n = 1352) of HCWs felt that it was acceptable if colleagues resigned or took sick leave owing to their fear of contracting COVID-19. The only statistically significant difference between the groups was that primary HCWs were more likely to be upset when patients attended the hospital for minor illnesses during the pandemic than secondary HCWs (51.9% primary HCWs vs 40.9% secondary HCWs; χ2 = 27.89; P < .0001).
Psychological Distress
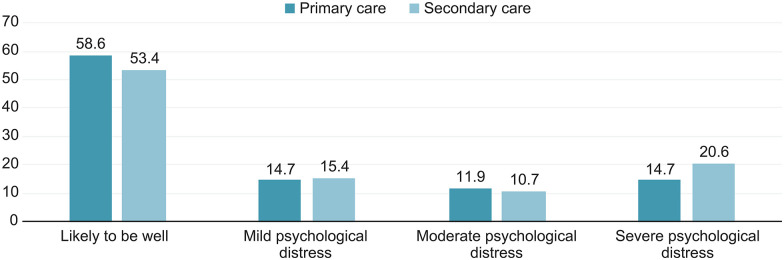
Overall, 54.2% (n = 2396) of HCWs were in the likely to be well group, 15.3% (n = 675) in the mild distress group, 10.9% (n = 481) in the moderate distress group, and 19.6% (n = 865) in the severe distress group. A comparison of K10 scores between the primary and secondary HCWs is presented in Figure 1.
Figure 1.
The comparison of psychological distress of healthcare workers in primary and secondary care settings in Qatar.
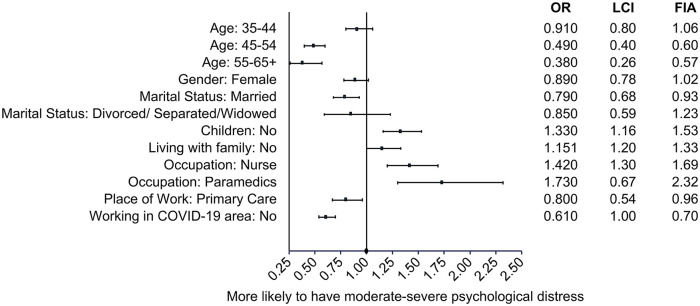
Univariate logistic regression of sociodemographic variables and moderate to severe psychological distress
Moderate and severe distress responses were grouped together (30.5%; n = 1346) to assess their possible association with sociodemographic and risk perception variables. Of the 1346 respondents, 34.0% (n = 702) were found to have moderate to severe psychological distress in the 20 to 34 years age group, 32.1% (n = 476) in the 35 to 44 group, 20.2% (n = 137) in the 45 to 54 group, and 16.4% (n = 31) in the >55 group (P < .0001).
Overall, 32.1% (n = 481) of the men and 29.6% (n = 865) of the women experienced moderate to severe psychological distress (P = .087). Additionally, 34.5% of the HCWs (n = 301) who were single, 31% (n = 48) of those who were divorced/widowed, and 29.4% (n = 997) of those who were married experienced moderate to severe psychological distress (P = .015).
Further, 34.9% (n = 456) of the HCWs without children and 28.6% (n = 890) of those with children experienced moderate to severe psychological distress (p < .0001). Of the HCWs who were living with family, 29.7% (n = 960) experienced moderate to severe psychological distress, whereas 32.7% (n = 386) of those who were not living with their family experienced it (P = .054).
Overall, 36% (n = 99) of the paramedics, 31.6% (n = 1037) of the nurses, and 24.5% (n = 210) of the doctors experienced moderate to severe psychological distress (P < .0001). Of the secondary HCWs, 31.2% (n = 1147) had moderate to severe psychological distress, compared to 26.7% (n = 199) of the primary HCWs (P = .013).
Of the secondary HCWs working in a COVID-19-designated area, 35.2% (n = 828) experienced moderate to severe psychological distress, compared to 25.0% (n = 518) of the HCWs working in non-COVID-19-designated areas (P < .0001). The effect of sociodemographic variables on moderate to severe psychological distress is presented in Figure 2.
Figure 2.
Univariate logistic regression: effect of sociodemographic variables on moderate to severe psychological distress.
Univariate logistic regression of risk perception variables and moderate to severe psychological distress
Personal concerns
Overall, 35.1% (n = 1189) of those who perceived a more significant risk of exposure to COVID-19 had moderate to severe psychological distress, compared to 10.5% (n = 38) of those who did not perceive a more considerable risk (P < .0001).
Those who did not perceive a greater exposure risk were less likely to experience moderate to severe psychological distress (OR = 0.22; 95% CI: 0.15-0.31). Similarly, those who were not afraid of falling ill with COVID-19 (OR = 0.20; 95% CI: 0.16-0.24) or were not thinking about the COVID-19 pandemic all the time (OR = 0.14; 95% CI: 0.12-0.17) were less likely to have moderate to severe psychological distress. However, those who did not accept the risk of contracting COVID-19 as part of their job were more likely to suffer from moderate to severe psychological distress (OR = 2.37; 95% CI: 1.91-2.94). Despite experiencing moderate to severe psychological distress, 73.2% (n = 739) of HCWs felt that they could take care of COVID-19 patients (P < .0001).
Family-related concerns
Almost all (94.4%; n = 1216) HCWs who reported having moderate to severe psychological distress were concerned that people close to them would be at high risk of contracting COVID-19. HCWs who were not worried that their family was at an increased risk of contracting COVID-19 owing to their job (OR = 0.24; 95% CI: 0.18-0.31) and who were not concerned about talking to their family about the risk to which they were exposed (OR = 0.28; 95% CI: 0.23-0.34) were less likely to have moderate to severe psychological distress. Overall, 49% (n = 879) of the HCWs who felt that people would avoid them or their family owing to their job had moderate to severe psychological distress, compared to 15.4% (n = 295) of those who did not feel that people would avoid them or their family (P < .0001). The effect of risk perception variables (personal and family-related concerns) on moderate to severe psychological distress is presented in Table 2.
Table 2.
Univariate Logistic Regression: Effect of Risk Perception Variables (Personal and Family Concerns) on Moderate to Severe Psychological Distress.
| Risk perception variables (personal/family concerns) | Yes/no | n (%) | OR (95% CI) | P value |
|---|---|---|---|---|
| My job would put me at a greater risk of exposure to COVID-19. | Yes | 1189 (35.1) | 1 | <.0001 |
| No | 38 (10.5) | 0.22 (0.15-0.31) | ||
| I am afraid of falling ill with COVID-19. | Yes | 1149 (38.8) | 1 | <.0001 |
| No | 104 (11.4) | 0.20 (0.16-0.24) | ||
| I should not be looking after COVID-19 patients. | Yes | 270 (50.0) | 1 | <.0001 |
| No | 739 (24.3) | 0.32 (0.27-0.39) | ||
| I accept that the risk of contracting COVID-19 is a part of the job. | Yes | 1032 (27.7) | 1 | <.0001 |
| No | 177 (47.6) | 2.37 (1.91-2.94) | ||
| I might look for another job because of this risk. | Yes | 234 (70.3) | 1 | <.0001 |
| No | 827 (23.1) | 0.13 (0.10-0.16) | ||
| I find myself thinking about the COVID-19 pandemic all the time. | Yes | 1014 (48.7) | 1 | <.0001 |
| No | 232 (12.0) | 0.14 (0.12-0.17) | ||
| I am torn between the dedication to my job and responsibility toward my loved ones. | Yes | 1091 (41.3) | 1 | <.0001 |
| No | 158 (12.1) | 0.20 (0.16-0.24) | ||
| I feel people close to me would be at a high risk of getting COVID-19 owing to my job. | Yes | 1216 (35.7) | 1 | <.0001 |
| No | 72 (11.6) | 0.24 (0.18-0.31) | ||
| I feel people close to me would be worried about my health owing to my current job. | Yes | 1272 (33.7) | 1 | <.0001 |
| No | 39 (9.8) | 0.21 (0.15-0.30) | ||
| I would be concerned about telling my family about the risk I am exposed to. | Yes | 1169 (36.5) | 1 | <.0001 |
| No | 137 (13.8) | 0.28 (0.23-0.34) | ||
| I feel that people would avoid my family members or me because of my job. | Yes | 879 (48.9) | 1 | <.0001 |
| No | 295 (15.4) | 0.19 (0.16-0.22) |
Abbreviations: OR, odds ratio; CI, confidence interval.
Work-related concerns
A total of 23.4% (n = 674) of the HCWs who thought their employer would look after their needs if they contracted COVID-19 experienced moderate to severe psychological distress, compared to 53.8% (n = 276) of those who believed that their employer would not look after them. HCWs who believed that their employer would not look after them (OR = 3.81; 95% CI: 3.13-4.62) were also more likely to have moderate to severe psychological distress. HCWs who were not worried about the lack of staff at work to handle the increased demand (OR = 0.29; 95% CI: 0.24-0.35), did not anticipate an increased workload (OR = 0.21; 95% CI: 0.17-0.25), and were willing to do work not usually in their job description (OR = 0.37; 95% CI: 0.32-0.44) were all less likely to experience moderate to severe psychological distress. Of the HCWs who experienced moderate to severe psychological distress, 92% (n = 1185) were concerned about the availability of personal protective equipment (P < .001). The effect of risk perception variables (work-related concerns) on moderate to severe psychological distress is presented in Table 3.
Table 3.
Univariate Logistic Regression: Effect of Risk Perception Variables (Work Concerns) on Moderate to Severe Psychological Distress.
| Risk perception variables (work concerns) | Yes/no | n (%) | OR (95% CI) | P value |
|---|---|---|---|---|
| I get upset when patients attend to the hospital for minor illnesses during this pandemic. | Yes | 692 (41.2) | 1 | <.0001 |
| No | 501 (22.2) | 0.41 (0.36-0.47) | ||
| I am worried there would be inadequate staff at my workplace to handle the increased demand. | Yes | 1064 (38.1) | 1 | <.0001 |
| No | 166 (15.1) | 0.29 (0.24-0.35) | ||
| I feel there would be more conflict amongst colleagues at work. | Yes | 916 (48.4) | 1 | <.0001 |
| No | 247 (14.3) | 0.18 (0.15-0.21) | ||
| I would feel more stressed at work. | Yes | 1213 (44.7) | 1 | <.0001 |
| No | 71 (5.6) | 0.07 (0.06-0.10) | ||
| I feel that I would have an increase in workload. | Yes | 1091 (40.3) | 1 | <.0001 |
| No | 146 (12.2) | 0.21 (0.17-0.25) | ||
| I feel I would have to work overtime. | Yes | 876 (36.3) | 1 | <.0001 |
| No | 292 (23.7) | 0.54 (0.47-0.64) | ||
| I would have to do work not normally done by me. | Yes | 953 (38.2) | 1 | <.0001 |
| No | 237 (18.6) | 0.37 (0.32-0.44) | ||
| I am concerned about the negative impact of social media information on my work. | Yes | 852 (41.5) | 1 | <.0001 |
| No | 340 (18.4) | 0.32 (0.27-0.37) | ||
| I am concerned about the availability of protective equipment at my workplace. | Yes | 1185 (34.0) | 1 | <.0001 |
| No | 102 (14.6) | 0.33 (0.27-0.41) | ||
| I am concerned about the inadequate infection control measures taken by my colleagues. | Yes | 961 (38.6) | 1 | <.0001 |
| No | 255 (17.6) | 0.34 (0.29-0.40) | ||
| I feel it is acceptable for colleagues to resign/take a sick leave because of their fear of getting COVID-19. | Yes | 628 (46.9) | 1 | <.0001 |
| No | 487 (21.5) | 0.31 (0.27-0.36) | ||
| I am confident that my employer will look after my needs if I contract COVID-19. | Yes | 674 (23.4) | 1 | <.0001 |
| No | 276 (53.8) | 3.81 (3.13-4.62) |
Abbreviations: OR, odds ratio; CI, confidence interval.
The distribution of sociodemographic variables in primary and secondary HCWs who had moderate to severe psychological distress is presented in Table 4.
Table 4.
Distribution of Sociodemographic Characteristics Between Primary and Secondary Care among Participants Who Had Moderate to Severe Psychological Distress.
| Sociodemographic variables | PC, n (%) 199 (26.7) | SC, n (%) 1147 (31.2) | χ2 | P value |
|---|---|---|---|---|
| Age (years) | ||||
| 20-34 | 66 (33.2) | 636 (55.4) | 49.70 | <.0001 |
| 35-44 | 83 (41.7) | 393 (34.3) | ||
| 45-54 | 39 (19.6) | 98 (8.5) | ||
| 55-65+ | 11 (5.5) | 20 (1.7) | ||
| Sex | ||||
| Male | 68 (34.2) | 413 (36.0) | 0.25 | <.618 |
| Female | 131 (65.8) | 734 (64.0) | ||
| Marital status | ||||
| Single | 25 (12.6) | 276 (24.1) | 17.26 | < 0001 |
| Married | 161 (80.9) | 836 (72.9) | ||
| Divorced/separated/widowed | 13 (6.5) | 35 (3.1) | ||
| Children | ||||
| Yes | 151 (75.9) | 739 (64.4) | 9.93 | <.002 |
| No | 48 (24.1) | 408 (35.6) | ||
| Living with family | ||||
| Yes | 172 (86.4) | 788 (68.7) | 26.07 | <.0001 |
| No | 27 (13.6) | 359 (31.3) | ||
| Occupation | ||||
| Doctor | 64 (32.2) | 146 (12.7) | 60.79 | <.0001 |
| Nurse | 135 (67.8) | 902 (78.6) | ||
| Paramedic staff | 0 (0) | 99 (8.6) | ||
| Working in a COVID-19 designated area | ||||
| Yes | 119 (59.8) | 709 (61.8) | 0.29 | <.590 |
| No | 80 (40.2) | 438 (38.2) | ||
Abbreviations: PC, primary care; SC, secondary care.
Predictors of moderate to severe psychological distress using multivariate logistic regression
In the multivariate logistic regression, all variables, apart from sex and marital status, were found to be significantly associated with moderate to severe psychological distress. This analysis indicated that primary HCWs were significantly less likely to have moderate to severe psychological distress than secondary HCWs (Adjusted OR = 0.48; 95% CI: 0.29-0.77, P = .003).
Discussion
During the current COVID-19 crisis, HCWs may be at high risk of psychological distress. Our study focused on risk perception and its psychological impact on HCWs, as this may provide important information about their needs. Furthermore, it may represent a focal point for developing stronger policies to sustain HCWs throughout this challenging time.
To the best of our knowledge, this is the first cross-sectional study on risk perception and psychological distress in HCWs during the COVID-19 pandemic in Qatar and the largest study conducted in the Middle East. Previous studies have shown that many HCWs experience psychological distress during widespread disasters because of their exposure, vulnerability, and long and intensive hours of work.15,16 Our results have shown that HCWs in Qatar experienced psychological distress during the outbreak of COVID-19, as indicated by studies of past epidemics.11,17 Our study also indicated that HCWs have shown commitment to their profession and acknowledged that the possibility of contracting COVID-19 is part of their duty. Studies show that finding meaning, purpose, and value in one’s work is correlated with less mental exhaustion in clinicians.18-20
Notably, one-third of the HCWs (34%; n = 702) who experienced moderate to severe psychological distress in our sample were aged between 20 and 34 years; this age group represents younger professionals (ie, nurses, residents, and fellows). A possible explanation for this result relates to their lack of experience or previous exposure, which may justify their higher levels of psychological distress compared with older age groups. Moreover, the fact that they may be nearer to the first point of contact compared with more senior staff may increase the psychological distress of younger age groups during a pandemic. A recent study found that General Practitioners are worried about the continuity of regular care for patients during the pandemic; this may become a threat for the general health in the population and for the provision of primary healthcare in the near and distant future.21
While some researchers have investigated the prevalence of psychological problems among HCWs during the COVID-19 pandemic,1,22 our analysis of the existing literature in PubMed, Google Scholar, and PsycINFO found that, to date, only 1 study23 investigated the distribution of psychological problems in different groups of HCWs. In particular, we did not identify any study comparing primary and secondary HCWs. Importantly, our findings showed a higher percentage of HCWs with moderate to severe psychological distress in secondary care than in primary care settings.
The COVID-19 pandemic has provided lessons for improving the processes underlying mental well-being and psychosocial support in Qatar. Accordingly, in collaboration with the Ministry of Public Health and PHCC, the Mental Health Service in the HMC has launched a new helpline to support people experiencing mental health problems due to the current COVID-19 pandemic. This helpline is operated by a team of mental health professionals who provide assessment and assistance to callers across 4 main categories: children and parents, adults, older people, and HCWs. Reassurance, psychosocial support, measures to enhance protection for HCWs, and activities that impart knowledge and skills could help minimize psychological distress in HCWs and improve the workforce’s overall efficiency during a pandemic.
Limitations
This cross-sectional study has some limitations. First, despite indicating possible associations between variables, we could not demonstrate causality. Second, the results were based on self-reported questionnaires that investigated the psychological impact and risk perception, which may differ from clinical diagnostic criteria. Third, we were unable to measure or detect pre-existing psychological distress compared to newly emerging symptoms. Fourth, although we targeted doctors, nurses, and paramedics, we did not explore specific job designations or years of experience of these HCWs. Fifth, the impacts of secondary stressors (eg, financial strains and personal and relationship situations) were not measured, even though they may also affect risk perception among HCWs. Finally, the current research study was conducted to investigate the risk perception of the COVID-19 pandemic, to determine and assess the prevalence and severity of psychological distress among HCWs, and to compare these domains between primary and secondary care settings 2 distinct types of healthcare. However, all statistical comparisons presented were exploratory analyses, which might limit the generalizability of the comparative conclusions.
Conclusions
The issue of psychological distress encountered by HCWs during this pandemic may arise even during the second wave of COVID-19 or other future health emergencies. It is important that interventions to encourage resilience in clinicians and to mitigate this form of psychological distress are developed and implemented, a statement consistent with previous research.24 Our study showed that the reaction of HCWs to outbreaks might have a range of psychological effects. Considering the likelihood of the long-term consequences that these may evoke and the possible association with reduced decision-making capacity, these mental health implications and perceived tensions become particularly alarming. Indeed, the nature of HCWs’ job makes them more vulnerable to critical situations that could adversely affect their mental health, so addressing this issue during epidemics and outbreaks becomes critical. Thus, rapid and successful implementation of countermeasures is key to the mitigation of such adverse mental health outcomes, whereas failing to consider these psychological effects may have an operational impact on the capacity of institutions to respond to health emergencies.
Acknowledgments
We would like to thank all primary and secondary healthcare staff who participated in this project. Additionally, we would like to extend our sincere gratitude to the Medical Research Centre for their ongoing and unrestricted support.
Footnotes
Author contributions: NK, AH, and MA conceptualized and designed the study. NK and AH participated in manuscript writing. BE performed the literature review and wrote the manuscript. PC analyzed the data and interpreted the results. RP, JV, and JG collected the data. All authors contributed to the design, result analysis, and study implementation. All authors have approved the final article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Bushra Elhusein  https://orcid.org/0000-0003-0803-1138
https://orcid.org/0000-0003-0803-1138
Data Availability: The data that support the findings of this study are available from the corresponding author, BE, upon reasonable request.
References
- 1.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kader N, Elhusein B, Chandrappa N, et al. Perceived stress and post-traumatic stress disorder symptoms among intensive care unit staff caring for severely ill coronavirus disease 2019 patients during the pandemic: a national study. Ann Gen Psychiatry. Preprint. Posted online May 13, 2021 doi: 10.21203/rs.3.rs-511538/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang C, Xu H, Rebaza A, Sharma L, Dela Cruz CS.Protecting healthcare workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8(3):e13. doi: 10.1016/S2213-2600(20)30066-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee SM, Kang WS, Cho A-R, Kim T, Park JK.Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-127. doi: 10.1016/j.comppsych.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245-1251. [PMC free article] [PubMed] [Google Scholar]
- 7.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D.Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. The World Health Report 2006—working Together for Health. WHO; 2006. Accessed May 28, 2021. https://www.who.int/whr/2006/whr06_en.pdf [Google Scholar]
- 9.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 10.Victoria Government Department of Health and Human Services. Victorian Population Health Survey 2001: selected findings. 2002. Accessed May 28, 2021. https://www2.health.vic.gov.au/about/publications/policiesandguidelines/Victorian-population-health-survey-2001-Selected-findings
- 11.Koh D, Lim MK, Chia SE, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med Care. 2005;43(7):676-682. doi: 10.1097/01.mlr.0000167181.36730.cc [DOI] [PubMed] [Google Scholar]
- 12.Algarni S, Almalki H, Raddadi R.Epidemic and pandemic events preparedness in Ministry of Health hospitals, Jeddah 2017: a cross sectional study. Int J Adv Res. 2017;5(11):590-589. doi: 10.21474/ijar01/5806 [DOI] [Google Scholar]
- 13.El Gaafary MM, Abd Elaziz KM, Abdel-Rahman AG, Allam MF.Concerns, perceived impacts and preparedness of health care workers in a referral hospital in Egypt in facing influenza (H1N1) epidemic. J Prev Med Hyg. 2010;51(3):105-109. [PubMed] [Google Scholar]
- 14.Wong TY, Koh GCH, Cheong SK, et al. Concerns, perceived impact and preparedness in an avian influenza pandemic: a comparative study between healthcare workers in primary and tertiary care. Ann. Acad. Med. 2008;37(2):96-102. [PubMed] [Google Scholar]
- 15.Chong M-Y, Wang W-C, Hsieh W-C, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185(2):127-133. doi: 10.1192/bjp.185.2.127 [DOI] [PubMed] [Google Scholar]
- 16.Grace SL, Hershenfield K, Robertson E, Stewart DE.The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. 2005;46(5):385-391. doi: 10.1176/appi.psy.46.5.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA.Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14(1):7-14. doi: 10.3121/cmr.2016.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callahan K, Christman G, Maltby L.Battling burnout: strategies for promoting physician wellness. Adv Pediatr. 2018;65(1):1-17. doi: 10.1016/j.yapd.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 19.Murali K, Makker V, Lynch J, Banerjee S.From burnout to resilience: an update for oncologists. Am Soc Clin Oncol Educ Book. 2018;38(38):862-872. doi: 10.1200/EDBK_201023 [DOI] [PubMed] [Google Scholar]
- 20.Tak HJ, Curlin FA, Yoon JD.Association of intrinsic motivating factors and markers of physician well-being: a national physician survey. J Gen Intern Med. 2017;32(7):739-746. doi: 10.1007/s11606-017-3997-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verhoeven V, Tsakitzidis G, Philips H, Van Royen P.Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10:e039674. doi: 10.1136/bmjopen-2020-039674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242-250. doi: 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Que J, Shi L, Deng J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020;33(3):e100259. doi: 10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heath C, Sommerfield A, von Ungern-Sternberg BS.Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020;75(10):1364-1371. doi: 10.1111/anae.15180 [DOI] [PMC free article] [PubMed] [Google Scholar]