Abstract
Introduction
Congenital hepatic cyst is a rare hepatobiliary malformation that can present as an asymptomatic, unilocular, upper abdominal cystic mass in the fetus.
Cases
We report two cases of congenital hepatic cyst in which the diagnosis was made by prenatal ultrasound at 25 and 33 weeks’ gestation. The diagnosis was confirmed postnatally by abdominal ultrasound and radiologic imaging studies. Although the infants remained asymptomatic, laparoscopic excision was performed due to the increasing size of the cyst in both cases. Pathological examination of the resected specimens confirmed a simple cyst in one case and an epidermoid cyst in the other.
Conclusions
Our cases and those described in the literature demonstrate the usefulness of incidental prenatal detection of congenital hepatic cyst, especially during late pregnancy. Such a diagnosis can allow for proper perinatal surveillance, selection of the route of delivery, and timely postnatal surgical intervention if required.
Keywords: Congenital anomalies, fetal ultrasound, hepatic cyst, prenatal diagnosis
Introduction
Congenital hepatic cysts are rare, often isolated, and usually asymptomatic, unilocular, fluid-filled spaces located within the liver that are present at birth. Histologically, they are usually lined by cuboid epithelia and surrounded by a fibrous capsule.1 Although they do not connect to the biliary tree or contain bile, they are thought to arise from aberrant bile ducts or intrahepatic peribiliary glands.1 Congenital hepatic cysts are amenable for detection by prenatal ultrasound.2 However, in the vast majority of cases they develop late in pregnancy and, therefore, can only be identified incidentally if a third-trimester scan is performed due to other obstetric indications. With the increasing use of obstetric ultrasound for the evaluation of intrauterine growth and fetal wellbeing in the third trimester of pregnancy,3 a significant number of fetal anomalies are currently detected for the first time during late pregnancy.4 In this report, we describe two cases of congenital hepatic cyst incidentally detected by obstetric ultrasound after 24 weeks’ gestation. The prenatal diagnosis was confirmed through postnatal imaging studies and histologically after laparoscopic excision of the cysts.
Case reports
Case 1. A 39-year-old woman, gravida 3, para 0 was referred to our fetal medicine center for further evaluation of a unilocular, cystic mass measuring 31 × 28 × 28 mm in the fetal upper abdomen, detected during a routine third-trimester scan at 33 weeks’ gestation. Her medical and family histories were noncontributory and the pregnancy was otherwise uncomplicated. Obstetric ultrasound examination at our center at 34 weeks’ gestation revealed a unilocular cystic mass measuring 44 × 43 × 31 mm and located between the umbilical vein and the stomach, close to both the inferior surface of the liver and the anterior abdominal wall (Figure 1(a) and (b)). Color Doppler ultrasound demonstrated no blood flow within the mass. There were no associated anomalies and, in particular, there were no signs of mass compression of adjacent organs, despite a mild increase in the size of the cyst in comparison to the previous scan. However, the umbilical vein was noted to be displaced to the right by the cyst. The fetal stomach, gallbladder, and kidneys were identified to be separate from the cystic mass, thus ruling out duodenal obstruction, choledochal cyst, and hydronephrosis or renal cyst.2 A congenital hepatic cyst was considered the most probable diagnosis. Fetal magnetic resonance imaging (MRI) was requested to further delineate the nature of the cyst and its relationship with adjacent organs. However, this examination was not performed due to the patient’s lack of financial resources and other administrative factors. At 35 weeks, the patient was admitted to her local hospital with the clinical diagnosis of intrahepatic cholestasis of pregnancy. Obstetric ultrasound at admission revealed that the fetal abdominal cyst had remained stable in size. Based on the severity of the cholestasis, an elective Caesarean section was performed at 36.5 weeks’ gestation to avoid a traumatic delivery and decrease the chances of cyst rupture during delivery. A male infant weighing 3245 g was delivered and had an uneventful postnatal course. An abdominal ultrasound scan on day three confirmed the presence of a cyst measuring 46 × 46 × 28 mm, which was located in segment IV of the liver (Figure 1(c)). This was further confirmed by computed tomography at six weeks (Figure 2). Routine blood tests, including a liver function panel, were normal. In addition, tumor and germ cell markers were also evaluated; serum α-fetoprotein levels were elevated (1294 ng/mL, normal range 40–1000) and β-hCG levels were normal (1.1 mIU/mL, normal <5). At two months of age, the infant underwent a laparoscopic resection of the cyst due to continuous increase in its size to 52 × 47 × 30 mm (Figure 3). After an uneventful recovery, the infant was discharged in good condition. Histopathology of the surgical specimen revealed a solitary benign hepatic cyst. Immunohistochemistry studies showed that the epithelium was positive for CK7 (cytokeratin 7), confirming biliary tract in origin, and negative for D2-40 (podoplanin) and CD34, ruling out the presence of lymphatic, mesothelial, and vascular derived cells (Figure 4). Abdominal ultrasound at four months reported no recurrence of the cyst. The infant is currently one year of age, asymptomatic, and thriving.
Figure 1.
Case 1. Axial (a) and parasagittal (b) ultrasound views of the fetal abdomen at 34 weeks’ gestation show a 44 × 43 × 31 mm cystic mass (asterisk) between the stomach (st) and the umbilical vein (uv). Note that the cyst is in close contact with the fetal anterior abdominal wall and displaces, but does not compress, the umbilical vein. (c) Postnatal abdominal ultrasound shows a hepatic cyst (between calipers) measuring 51 × 30 mm. L, liver.
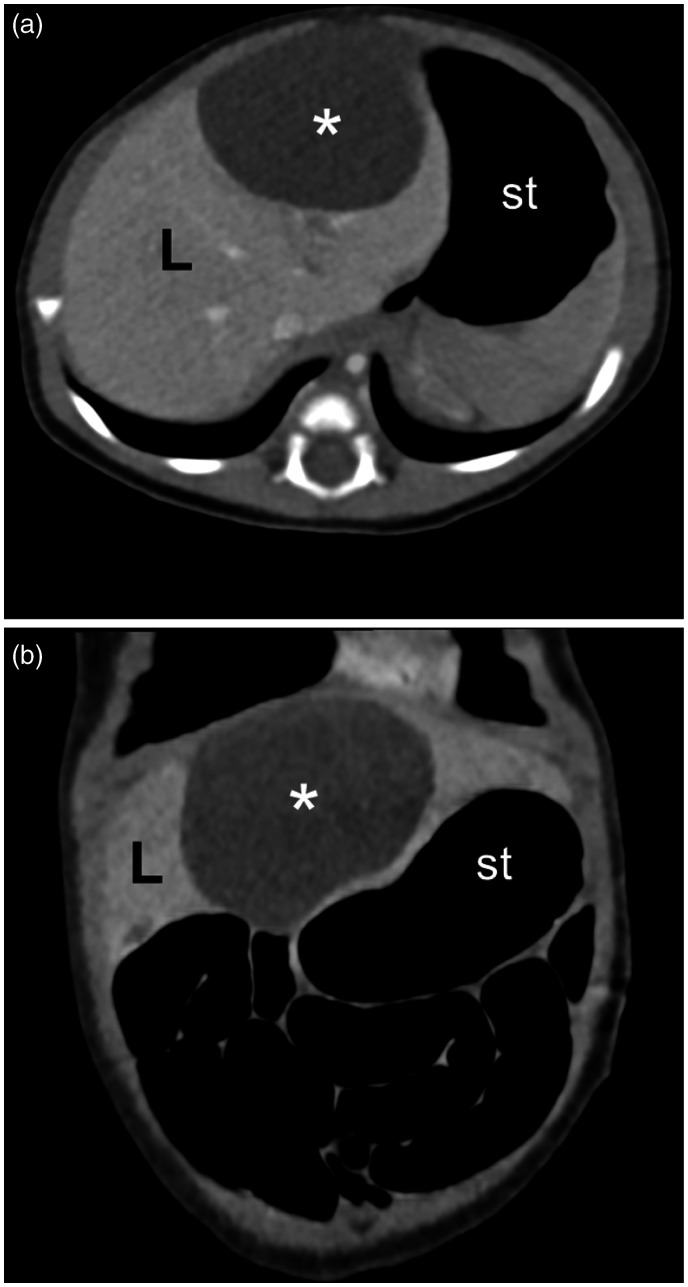
Figure 2.
Case 1. Postnatal axial (a) and coronal (b) contrast-enhanced abdominal computed tomography images at six weeks show a hypodense mass (asterisk) within the liver (L), consistent with a nonparasitic simple congenital hepatic cyst. st, stomach.
Figure 3.
Case 1. Laparoscopic view of the hepatic cyst (C) before excision.
Figure 4.
Case 1. Histopathology of the resected specimen revealed a simple cyst. (a) Note cyst lining, composed of a monolayer cubic epithelium, and the surrounded fibrous wall and hepatic tissue (H&E, 10×). (b) Immunohistochemistry staining of the epithelia was positive for CK7 (arrows).
Case 2. A 20-year-old primigravida underwent a routine obstetric ultrasound at 25 weeks’ gestation. The patient’s past medical history included a solitary kidney, chronic hypertension, insulin resistance, and obesity. Prenatal ultrasound revealed a unilocular cyst measuring 20 mm in diameter located in the fetal left upper abdominal quadrant. No associated anomalies were detected and, in particular, the fetal stomach, gallbladder, and kidneys were deemed normal in appearance and separate from the cyst. Subsequent prenatal course was complicated by a urinary tract infection, which was treated with intravenous antibiotics, and maternal hypertension, which was managed with bed rest and methyldopa. A follow-up ultrasound examination at 33 weeks’ gestation revealed that the abdominal cyst had remained stable in size. Due to the maternal complications, a Caesarean section was performed at 37 weeks delivering a male infant weighing 3175 g. Postnatal abdominal ultrasound confirmed the presence of a unilocular cyst measuring 23 × 19 × 13 mm in segment IV of the liver (Figure 5(a)). The infant had an uneventful neonatal course, was discharged on day five, and remained asymptomatic throughout his first year of life. However, a follow-up abdominal ultrasound at 15 months revealed a large unilocular hepatic cyst measuring 85 × 56 mm that displaced intrahepatic vascular structures (Figure 5(b)). A subsequent abdominal MRI and cholangiography confirmed a hepatic cyst measuring 91 × 72 × 62 mm, with no connection to the biliary tree but displacing the gallbladder and hepatic vessels (Figure 6). Based on this finding, the infant was referred to our tertiary pediatric surgery center. At referral, routine blood tests, liver function tests, and serum tumor markers including α-fetoprotein and β-hCG levels were within normal ranges. Due to the size and location of the lesion, the patient underwent laparoscopic deroofing. The anterior wall of the cyst was resected and the inner surface was ablated using a monopolar electrocautery. An intraoperative cholangiogram through the gallbladder revealed no biliary leak, after which a cholecystectomy was performed uneventfully to avoid subsequent iatrogenic biliary leaking. The infant recovered well and was discharged on day two. Histopathology revealed a benign epidermoid cyst (Figure 7). Abdominal ultrasound at two- and six months after surgery revealed residual fibrotic tissue in the surgical site, which remains under observation.
Figure 5.
Case 2. Abdominal ultrasound views of a congenital hepatic cyst. (a) At one day of life, a simple unilocular cyst located in liver and measuring 23 × 19 × 13 mm was confirmed. (b) At 15 months, the hepatic cyst (between calipers) had grown considerably, now measuring 85 × 56 mm. Note internal debris probably representing desquamated epithelial cells.
Figure 6.
Case 2. Preoperative abdominal MRI at 15 months. (a) Coronal and (b) axial T2-weighted images show a hepatic cyst (asterisk). L, liver. (c) Magnetic resonance cholangiography shows the hepatic cyst (asterisk). Note that there is no connection between the cyst and the biliary tree (arrows).
Figure 7.
Case 2. Histopathology of the resected specimen revealed an epidermoid cyst. (a) Note cyst lining composed of a keratinized squamous epithelia (H&E, 40×). (b) Epithelial cells displayed immunoreactivity for CK AE1/AE3, stained as dark brown.
Discussion
The ultrasound detection of an abdominal cyst in the fetus poses significant perinatal diagnostic and management challenges. The main differential diagnoses include any cystic mass originating from either the gastrointestinal, hepatobiliary, or urogenital tracts.2 If located in the upper abdomen, these conditions include duodenal obstruction, choledochal cyst, hepatic cyst, pancreatic cyst, splenic cyst, mesenteric cyst, and enteric duplication cyst.2 In this report, two cases of congenital hepatic cysts were described. In the first, a large unilocular cyst was first detected during a routine third-trimester scan. Remarkably, the routine second-trimester scan was reported as normal strongly suggesting that the cyst developed later in pregnancy. This is in line with a previous report suggesting a similar prenatal course, in which a large 40 × 38 × 34 mm hepatic cyst was first detected at 34 weeks’ gestation after a normal second trimester scan.5 In our case the cyst was relatively moderate in size when compared to other reports, which even describe cysts that fill the entire fetal abdominal cavity.6 As the infant remained asymptomatic, the cyst was monitored by ultrasound. However, due to the increasing size of the cyst, a laparoscopy resection was performed at two months of age with good clinical results. In the second case, a small unilocular cyst was detected during a late second-trimester scan. The cyst remained stable in size with no associated perinatal complications. The infant remained asymptomatic; however, a follow-up abdominal scan at 15 months revealed a large hepatic cyst prompting referral for surgery. Minimally invasive laparoscopic surgery with cyst deroofing was considered the best option in order to avoid damaging the surrounding normal hepatic tissue. Histopathology showed an epidermoid cyst, which is a rare type of hepatic cyst.7 Recent clinical evidence has shown that epidermoid hepatic cysts are indeed characterized by antenatal onset and slow postnatal growth,7 which is consistent with the clinical features present in our case.
Although the occurrence of an abdominal cystic mass in the fetus is rare, it is a well-recognized condition in fetuses and neonates.2 Among those presenting in the prenatal period, hepatic cysts are nevertheless one of the less common etiologies. Indeed, according to a recent review on this topic, fewer than 30 cases diagnosed prenatally have been reported in the literature, with a large single pediatric surgery referral center series reporting only 11 cases.1 Another large referral pediatric surgery center reported no cases of hepatic cyst in their 22-year experience with prenatally diagnosed abdominal cysts.8 Congenital hepatic cyst is a rare condition and usually they are small and resolve or remain asymptomatic during infancy.1,9 It is therefore possible that this condition has been largely underrecognized or grossly underreported, which may explain the low number of cases described in the literature.
The routine and widespread use of obstetric ultrasound in antenatal care now provides the opportunity to detect abdominal cysts prenatally. Prenatal ultrasound features that can help with the differential diagnosis between hepatic and other abdominal cysts include the location of the cyst, presence of peristaltic movements, and connection with the gallbladder or stomach.2 Interestingly, hepatic cysts have been reported occurring as early as 12–13 weeks’ gestation,10 with a high rate of spontaneous resolution in early pregnancy.11 Their occurrence or persistence in late pregnancy, however, has a special significance as it may determine the route of delivery, as well as whether or not percutaneous aspiration or surgical resection will be needed during the perinatal period or early infancy. As most congenital hepatic cysts are asymptomatic, an ultrasound examination late in pregnancy is the only available method for detecting these cases. This can easily be achieved at the time of the routine measurement of the abdominal circumference for estimating fetal weight, at which time three normal anechoic structures in the fetal upper abdomen are evident during the sweep, i.e. from left to right the stomach, umbilical vein, and gallbladder. Any additional anechoic structure at this level may suggest the presence of an abdominal cyst and the corresponding differential diagnosis, including hepatic cyst, should be considered.
Once a hepatic cyst is diagnosed, perinatal surveillance should be undertaken to monitor the size of the cyst and determine if surgery is indicated. As symptomatology depends on the size rather than the location of the cyst,9 the most recommended technique to monitor the size of a hepatic cyst is ultrasound, which is noninvasive, widely accessible, and less expensive than other imaging techniques. However, if surgery is considered, other techniques such as computed tomography and MRI, as illustrated in our cases, can provide extremely detailed images of the lesion and surrounding structures in order to plan any necessary surgical strategies. In addition, preoperative determination of tumor and germ cell markers, such as α-fetoprotein and β-hCG, is useful in cases of hepatic tumors, which in the event of malignancy is an important piece of information for follow-up after surgery. Finally, as demonstrated by our cases, laparoscopic excision seems to be a good alternative to open surgery in selected cases. This technique has proven to be safe when removing even large or symptomatic hepatic cysts, with minimal complications and rapid postoperative recovery in the pediatric population.12
Acknowledgements
The authors are grateful to Jorge Conejero, MD, for referring case 1 and to Jorge Becker, MD, for his assistance in collecting the prenatal information from case 2.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by an unrestricted research grant from the Sociedad Profesional de Medicina Fetal ‘Fetalmed’ Ltda., Chile.
Ethical approval: Written informed consent for publication of their clinical details and clinical images was obtained from the parents. This study was approved by the Institutional Review Boards of the FETALMED Maternal-Fetal Diagnostic Center (Estoril 50, Santiago, Chile; approval June 2020) and “Luis Calvo Mackenna” Hospital, NHS (Antonio Varas 360, Santiago, Chile; approval July 2020), Santiago, Chile.
Guarantor: Waldo Sepulveda.
Contributors: WS wrote the first draft of the manuscript. WS, FS, and GG analyzed patient data and wrote the final version of the manuscript. GG performed the surgical procedures and was in charge of the postoperative care of the infants. CA and EA performed the histopathology studies. All authors reviewed and approved the final version of the manuscript.
ORCID iD: Waldo Sepulveda https://orcid.org/0000-0002-3856-574X
References
- 1.Allan M, Davenport M.Congenital hepatic cysts. In: Lima M, Reinberg O. (eds) Neonatal surgery. Contemporary strategies from fetal life to the first year of age. Cham: Springer Nature Switzerland AG, 2019, pp. 401− 408. [Google Scholar]
- 2.McEwing R, Hayward C, Furness M.Foetal cystic abdominal masses. Australas Radiol 2003; 47: 101−110. [DOI] [PubMed] [Google Scholar]
- 3.Bricker L, Medley N, Pratt JJ.Routine ultrasound in late pregnancy (after 24 weeks’ gestation). Cochrane Database Syst Rev 2015; 6: CD001451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ficara A, Syngelaki A, Hammami A, et al. Value of routine ultrasound examination at 35–37 weeks’ gestation in diagnosis of fetal abnormalities. Ultrasound Obstet Gynecol 2020; 55: 75−80. [DOI] [PubMed] [Google Scholar]
- 5.Macken MB, Wright JR, Lau H, et al. Prenatal sonographic detection of congenital hepatic cyst in third trimester after normal second-trimester sonographic examination. J Clin Ultrasound 2000; 28: 307−310. [DOI] [PubMed] [Google Scholar]
- 6.Okumura M, Liao AW, Brizot ML, et al. Sonographic detection of a giant solitary hepatic cyst in utero. J Ultrasound Med 2008; 27: 1663−1665. [DOI] [PubMed] [Google Scholar]
- 7.Morrow MK, Li A, Perez-Atayde AR, et al. Congenital epidermoid cyst of the liver: a rare entity characterized by antenatal onset, slow postnatal growth, and consistent histologic and immunohistologic features. Pediatr Dev Pathol 2020; 23: 181−188. [DOI] [PubMed] [Google Scholar]
- 8.Thakkar HS, Bradshaw C, Impey L, et al. Post-natal outcomes of antenatally diagnosed intra-abdominal cysts: a 22-year single-institution series. Pediatr Surg Int 2015; 31: 187−190. [DOI] [PubMed] [Google Scholar]
- 9.Celebi S, Kutluk G, Bestas CB, et al. Current diagnosis and management of simple hepatic cysts detected prenatally and postnatally. Pediatr Surg Int 2014; 30: 599−604. [DOI] [PubMed] [Google Scholar]
- 10.Sepulveda W, Dickens K, Casasbuenas A, et al. Fetal abdominal cysts in the first trimester: prenatal detection and clinical significance. Ultrasound Obstet Gynecol 2008; 32: 860−864. [DOI] [PubMed] [Google Scholar]
- 11.Bronstein M, Nizar K, Weiner Z.Significance of early prenatal diagnosis of fetal hepatic cyst. J Clin Ultrasound 2009; 37: 65−68. [DOI] [PubMed] [Google Scholar]
- 12.Linden AF, Pulcrano ME, Duffy BJ, et al. Laparoscopic excision of congenital hepatic cysts in the pediatric population: a case series and literature review. J Laparoendosc Adv Surg Tech A 2016; 26: 493−497. [DOI] [PubMed] [Google Scholar]