Abstract
Objectives
To describe the situation of COVID-19-related stigma towards patients with COVID-19 and people from the city of Wuhan in China and to assess the associations between COVID-19-related stigma, health literacy and sociodemographic characteristics during March 2020, the early stage of the pandemic.
Design
A cross-sectional online survey.
Setting
The study surveyed 31 provinces in China.
Participants
This study surveyed 5039 respondents in China.
Outcome measures
Public stigma towards both patients with COVID-19 and Wuhan residents was measured. Binary logistic regression was used to identify the factors associated with public COVID-19-related stigma.
Results
Among the participants, 122 (2.4%) reported themselves and 254 (5.0%) reported the communities they lived in as holding a stigmatising attitude towards patients with COVID-19, respectively. Additionally, 114 (2.5%) and 475 (10.3%) reported that themselves and the communities they lived in, respectively, held a stigma against people from Wuhan, which was the most severely affected area in China. People aged over 40, lived in areas with severe epidemics (adjusted OR (aOR)=2.03, 95% CI (1.05 to 3.92)) and who felt it difficult to find and understand information about COVID-19 (aOR=1.91, 95% CI (1.08 to 3.37); aOR=1.88, 95% CI (1.08 to 3.29)) were more likely to stigmatise patients with COVID-19. People who were male, aged 41–50 and had difficulty understanding information (aOR=2.08, 95% CI (1.17 to 3.69)) were more likely to stigmatise people from Wuhan.
Conclusions
Patients with COVID-19 and Wuhan residents suffered stigma at both the individual and the community levels. Those who had low health literacy, who lived in areas with a large number of COVID-19 cases and who were of ethnic minorities were more likely to stigmatise others. Tailored interventions are encouraged to improve health literacy and consequently to reduce public COVID-19-related stigma.
Keywords: COVID-19, mental health, public health
Strengths and limitations of this study.
This was a rapid study to describe the situation of public COVID-19-related stigma during the early stage of the pandemic in China and to assess the associations between stigma, health literacy and other factors.
This is a cross-sectional study with an oversampling of ethnic minorities and a balance of urban and rural residents.
The survey data rely on self-reporting, and therefore participants’ responses may be biased due to social desirability.
Introduction
Stigma can be defined as a social label associating an individual with characteristics of prejudice and discrimination.1 2 Individuals suffering from stigma often feel shamed, stressed and isolated, leading to negative changes in their health behaviours.3 4 For example, individuals being stigmatised for a health condition may delay or avoid treatment, and may not seek access to health services, which compromises the outcome of their medical condition.5
In the field of infectious disease, stigma has been recognised as a global issue.6 In recent decades, many studies concerning stigma as related to infectious diseases have been conducted, including but not limited to HIV,7–9 tuberculosis10–12 and severe acute respiratory syndrome (SARS).13 14 The relationship between knowledge and stigma is well documented for infectious disease prevention measures that do not require social distancing. For example, people with higher education levels and HIV-related knowledge were less likely to stigmatise patients with HIV.7 15 This may be due to the fact that people with more HIV-related knowledge had a better understanding that they were not likely to get infected with HIV through social interactions (such as handshake, hug and cheek kiss). However, emerging infectious diseases that are evolving in nature and have uncertain transmission patterns often cause panic among individuals and communities, as was seen with SARS, H1N1 and COVID-19. The transmission of certain infectious diseases through social interactions can ignite public stigma towards disease-related groups14 following the introduction of social distancing policies to prevent such diseases. Previous studies have noted that social distancing measures may affect the attitudes of individuals and communities towards people with stigmatising conditions and may lead to stigma.14 16 In studies on COVID-19-related stigma, attention has been focused on stigma facing healthcare workers or residents in areas affected by the COVID-19 pandemic.17 18 However, few studies have explored the relationship between knowledge and stigma in emerging infectious diseases that require social distancing.
Health literacy is usually defined as an individual’s ability to obtain and process health information and take appropriate action.19 Knowledge is an important dimension of health literacy.20 Previous studies investigating the relationship between health literacy and stigma have mostly focused on mental illnesses and chronic diseases, and have shown that patients with low health literacy were more likely to feel stigmatised.21–23 Few studies have investigated the relationship between health literacy and stigma towards infectious diseases that require social distancing in China.
Studies on stigma related to infectious diseases have revealed that it is not only individual patients who face stigma from infectious diseases, but that entire racial or ethnic groups who have or are perceived as having a higher likelihood of being infected can face stigmatisation.24 Wuhan, the capital of Hubei Province, was the most severely affected area during the COVID-19 pandemic in China. In order to control the spread of COVID-19, the Chinese government took unprecedented measures, including locking down Wuhan and requiring all Wuhan residents who migrated to other provinces before Wuhan was locked down to receive nucleic acid tests. A considerable portion of confirmed COVID-19 cases in many provinces were imported cases from Wuhan.25 Despite the government and media calling for tolerance, the development of a stigma towards residents of Wuhan was inevitable. For example, in some communities, residents of Wuhan were not allowed to enter and suffered unfair treatment. Therefore, this study explores the situation of stigma faced by patients with COVID-19 and stigma faced by residents of Wuhan.
The aims of this study are (1) to describe the situation of public COVID-19-related stigma during the early stage of the COVID-19 pandemic in China and (2) to assess the associations between stigma, health literacy and sociodemographic characteristics.
Methods
Study design and participants
The WHO declared COVID-19 as a pandemic in March 2020, and our study was conducted between 1 March and 16 March 2020. As of 16 March 2020, there were more than 80 000 confirmed cases in China and more than 100 000 cases globally, and during this time, people in China were under strict social distancing policies. This was a national cross-sectional survey conducted in 31 provinces, municipalities and autonomous regions (hereafter, provinces) in China, except for Hong Kong, Macao and Taiwan.
The questionnaire was developed for this study (online supplemental additional file 1). Tools to measure public COVID-19-related stigma were adapted from a previous study.26 Two online focus groups were conducted to discuss the questionnaire design, with six people with public health and medical backgrounds in each group. Two independent experts with backgrounds in public health and risk communication reviewed and further developed the questionnaire. We conducted 30 online one-to-one interviews with respondents of different ages and education levels to pretest the questionnaire. The final questionnaire included sociodemographic characteristics, public COVID-19-related stigma and health literacy during the COVID-19 pandemic. Logic questions were set up to verify the validity of the data.
bmjopen-2021-048983supp001.pdf (122.3KB, pdf)
The respondents included in this study were aged over 16 years old and could read Mandarin. We conducted convenience sampling in 31 provinces, and 100–200 families were selected from each province. The member from each household whose birth date was closest to the survey date was invited to complete the questionnaire to ensure randomness in sampling. Younger family members were encouraged to assist elderly family members in completing the questionnaire, if necessary. Before the investigation, investigators received online trainings, and thus, they were responsible for quality control. Respondents could fill in the questionnaire by scanning QR codes or clicking the questionnaire link on smartphones, tablets and other mobile devices. A sample size of 3062 was estimated based on a prevalence estimate of 50%, the ±2% margin of error and upward adjusted by 20% considering potential non-response. We set up a target sample for ethnic minorities residents and oversampled respondents who lived in Wuhan, as it was the centre of the pandemic. We intentionally balanced respondents from urban and rural areas while conducting this survey. Before completing the questionnaire, respondents were informed in the consent statement that this was an anonymous and voluntary survey. No compensation was provided to respondents.
Patient and public involvement
Patients were not involved in the design, management or reporting of this study.
Measurements
Sociodemographic characteristics
The sociodemographic characteristics comprised gender, age, education, ethnicity, urbanicity and monthly household income. According to the data of confirmed COVID-19 cases in 31 provinces officially announced by the Chinese government as of 1 March 2020, the 31 provinces were divided into four groups. Hubei province, the statistical outlier with the highest number of confirmed cases, was classified as the high-risk group. The rest of the 30 provinces were divided into three groups (low-risk group, medium-risk group and medium-high-risk group), with each group containing 10 provinces based on their ranking of number of confirmed cases.
Health literacy
Questions on health literacy about COVID-19 were adapted from previous studies27 28 and measured using two questions: (1) To what extent do you agree with the following statements, ‘it is difficult for me to find correct and comprehensive information about COVID-19’?; (2) To what extent do you agree with the following statements, ‘it is difficult for me to understand information I got about COVID-19’? Each question was answered using a 5-point Likert scale ranging from 1 to 5 (1=strongly disagree; 2=disagree; 3=neutral; 4=agree; 5=strongly agree).
Stigma
Questions on public COVID-19-related stigma were adapted from previous studies.26 29 Four questions, including public stigma towards patients with COVID-19 and residents of Wuhan at the individual and community levels were used, respectively. The study participants who chose the following options: ‘It is their problem and I don’t want to get COVID-19 by trying to help them,’ and ‘I am afraid of them and avoid them because they may infect me,’ were classified as ‘stigmatised,’ those who chose options ‘I feel compassion and desire to help,’ ‘I feel compassion but tend to stay away from them,’ and ‘I have no particular feeling,’ were classified as ‘not stigmatised.’26 People who lived in Wuhan were automatically exempted from stigma questions related to residents of Wuhan.
Data analysis
All data were analysed using IBM SPSS Statistics V.23.0 for Windows. Descriptive analyses included means for continuous variables and percentages for categorical data. χ2 tests were conducted to compare COVID-19-related stigma between groups. Binary logistic regression analysis was used to examine the association of the independent variables with COVID-19-related stigma. All comparisons were two-tailed. The significance threshold was p value <0.05.
Results
The response rate of this survey was 94.7%. Of the 5124 participants who completed the questionnaire, 85 (1.7%) were excluded because they were younger than 16 years old or answered logical questions incorrectly. A total of 5039 participants (table 1) with an average age of 33.0 (SD=12.5) were included for analysis. Most of them were female, were of Han ethnicity, received senior high school education, had a monthly household income above US$705 US and lived in a medium case area.
Table 1.
Sample characteristics (N=5039)
| Variables | n | % |
| Age (years) | ||
| ≤20 | 774 | 15.4 |
| 21–30 | 1914 | 38.0 |
| 31–40 | 885 | 17.6 |
| 41–50 | 959 | 19.0 |
| ≥51 | 507 | 10.1 |
| Gender | ||
| Male | 2090 | 41.5 |
| Female | 2949 | 58.5 |
| Education level | ||
| Junior high school or less | 668 | 13.3 |
| Senior high school and junior college | 2528 | 50.2 |
| College and above | 1843 | 36.6 |
| Ethnicity | ||
| Han | 4234 | 84.0 |
| Minorities | 805 | 16.0 |
| Urbanicity | ||
| Urban | 2492 | 49.5 |
| Rural | 2547 | 50.5 |
| Monthly household income (US$) | ||
| <422 | 846 | 16.8 |
| 422–704 | 1485 | 29.5 |
| 705–1407 | 1422 | 28.2 |
| 1408–2815 | 858 | 17.0 |
| >2815 | 428 | 8.5 |
| Province by confirmed patients | ||
| Low case area | 1374 | 27.3 |
| Low-medium case area | 1386 | 27.5 |
| Medium case area | 1681 | 33.4 |
| High case area | 598 | 11.9 |
At the individual level (table 2), the majority (70.2%) of participants reported they felt compassion for and desired to help patients with COVID-19, 1045 (20.7%) reported they felt compassion for patients with COVID-19 but tended to avoid them, 29 (0.6%) expressed their unwillingness to help patients with COVID-19 and 93 (1.8%) expressed fear of patients with COVID-19. Less than 1% of participants expressed their unwillingness to help residents of Wuhan and 74 (1.6%) expressed fear of residents of Wuhan. At the community level, 254 (5.0%) participants reported their communities rejected patients with COVID-19, and 475 (10.3%) participants reported residents of Wuhan were rejected by their communities. Approximately one-third of participants reported that they had difficulties finding comprehensive and correct information about COVID-19, and 759 (15.0%) of the participants reported that it was difficult to understand the information they received about COVID-19.
Table 2.
Stigma and health literacy during the COVID-19 epidemic
| Variables | n | % |
| Stigma towards patients with COVID-19 (N=5039) | ||
| Statement closest to your feeling about people with COVID-19 | ||
| I feel compassion and desire to help | 3536 | 70.2 |
| I feel compassion but tend to stay away from them | 1045 | 20.7 |
| It is their problem and I don’t want to get COVID-19 by trying to help them | 29 | 0.6 |
| I am afraid of them and avoid them because they may infect me | 93 | 1.8 |
| I have no particular feeling | 336 | 6.7 |
| How was patient with COVID-19 usually regarded/treated in your community? | ||
| Most people reject him/her | 254 | 5.0 |
| Most people are friendly, but they generally try to avoid | 1141 | 22.6 |
| The community mostly supports and helps him/her | 725 | 14.4 |
| I don’t have the experience | 2919 | 57.9 |
| Stigma towards Wuhan people (n=4628)* | ||
| Statement closest to your feeling about Wuhan people | ||
| I feel compassion and desire to help | 3323 | 71.8 |
| I feel compassion but tend to stay away from them | 883 | 19.1 |
| It is their problem and I don’t want to get COVID-19 by trying to help them | 40 | 0.9 |
| I am afraid of them and avoid them because they may infect me | 74 | 1.6 |
| I have no particular feeling | 308 | 6.7 |
| How was Wuhan people usually regarded/treated in your community? | ||
| Most people reject him/her | 475 | 10.3 |
| Most people are friendly, but they generally try to avoid | 1784 | 38.6 |
| The community mostly supports and helps him/her | 2097 | 45.3 |
| I don’t have the experience | 272 | 5.9 |
| Health literacy (N=5039) | ||
| It is difficult for me to find correct and comprehensive information about COVID-19 | ||
| Strongly disagree | 218 | 4.3 |
| Disagree | 1541 | 30.6 |
| Neutral | 1679 | 33.3 |
| Agree | 1230 | 24.4 |
| Strongly agree | 371 | 7.4 |
| It is difficult for me to understand information I got about COVID-19 | ||
| Strongly disagree | 348 | 6.9 |
| Disagree | 2471 | 49.0 |
| Neutral | 1461 | 29.0 |
| Agree | 587 | 11.6 |
| Strongly agree | 172 | 3.4 |
*Participants who lived in Wuhan were automatically exempted from stigma questions related to residents of Wuhan.
Figure 1 shows the number of cumulative confirmed COVID-19 cases from the 31 provinces on the investigation data (1 March 2020). Figure 2 illustrates the proportion of individual stigma towards patients with COVID-19 in each province. People living in Hubei, Anhui, Guizhou, Tianjin and Yunnan provinces had a relatively high stigma percentage of over 4% of the population. Figure 3 shows that more than 4% of the respondents living in Guizhou, Yunnan and Qinghai provinces expressed a stigma towards residents of Wuhan. The proportion of reported stigma towards residents of Wuhan in Henan, Shanxi, Ningxia, Chongqing and Zhejiang provinces was between 3% and 4%.
Figure 1.
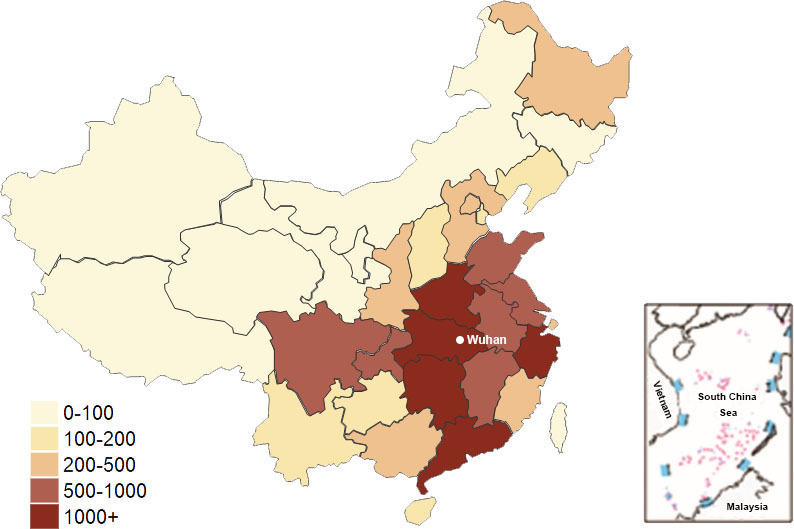
Number of confirmed COVID-19 cases by province.
Figure 2.
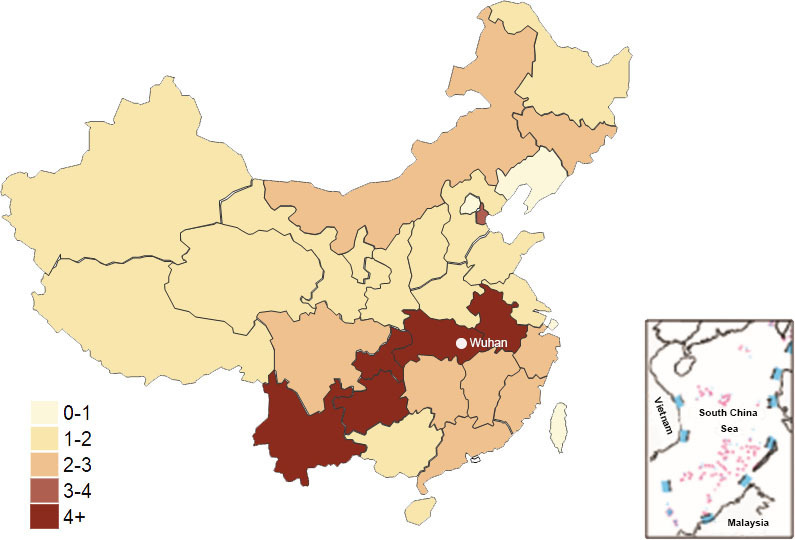
Proportion of stigma reported towards patients with COVID-19 by province (%).
Figure 3.
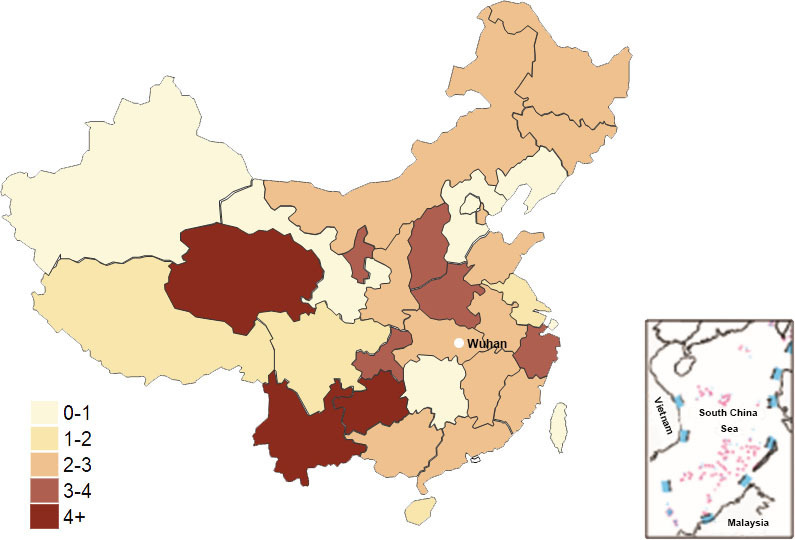
Proportion of stigma reported towards Wuhan residents by province (%).
As shown in table 3, the prevalence of stigma towards patients with COVID-19 among people over 50 was significantly higher than that of people under 20 (5.1% vs 1.2%, p<0.001). Compared with people who had a junior high school or lower degree, people with a college or higher degree reported lower levels of stigma towards patients with COVID-19 (2.0% vs 4.0%, p=0.01). Ethnic minorities showed a higher level of (3.6% vs 2.2%, p=0.024) stigma towards patients with COVID-19 than did Han respondents. Participants who felt it was easy to find and understand information about COVID-19 expressed lower stigma towards patients with COVID-19 than did those who felt it was difficult (1.4% vs 3.7%, p<0.001; 1.5% vs 4.5%, p<0.001). Individual stigma towards residents of Wuhan was more prevalent among male than female respondents (3.4% vs 1.8%, p<0.001) and was relatively high among those who felt it was hard to understand COVID-19-related information (4.4% vs 1.8%, p<0.001).
Table 3.
Univariate analysis of individual stigma towards patients with COVID-19 and Wuhan residents
| Variables | Patients with COVID-19 (N=5039) | P value | Wuhan residents (n=4628)* | P value | ||
| Stigma | χ² | Stigma | χ² | |||
| Gender | 3.742 | 0.053 | 12.25 | <0.001 | ||
| Male | 61 (2.9) | 66 (3.4) | ||||
| Female | 61 (2.1) | 48 (1.8) | ||||
| Age (years) | 32.43 | <0.001 | 4.053 | 0.399 | ||
| ≤20 | 9 (1.2) | 11 (1.5) | ||||
| 21–30 | 34 (1.8) | 43 (2.4) | ||||
| 31–40 | 17 (1.9) | 20 (2.6) | ||||
| 41–50 | 36 (3.8) | 26 (3.0) | ||||
| ≥51 | 26 (5.1) | 14 (3.0) | ||||
| Education level | 9.216 | 0.010 | 2.606 | 0.272 | ||
| Junior high school or less | 27 (4.0) | 21 (3.3) | ||||
| Senior high school and junior college | 59 (2.3) | 59 (2.5) | ||||
| College and above | 36 (2.0) | 34 (2.1) | ||||
| Ethnicity | 5.660 | 0.017 | 1.174 | 0.279 | ||
| Han | 93 (2.2) | 90 (2.4) | ||||
| Minorities | 29 (3.6) | 24 (3.0) | ||||
| Urbanicity | 0.060 | 0.807 | 0.129 | 0.720 | ||
| Urban | 59 (2.4) | 51 (2.4) | ||||
| Rural | 63 (2.5) | 63 (2.5) | ||||
| Monthly household Income (US$) | 5.875 | 0.209 | 0.481 | 0.975 | ||
| <422 | 20 (2.4) | 20 (2.4) | ||||
| 422–704 | 47 (3.2) | 38 (2.7) | ||||
| 705–1407 | 27 (1.9) | 31 (2.4) | ||||
| 1408–2815 | 17 (2.0) | 17 (2.3) | ||||
| >2815 | 11 (2.6) | 8 (2.2) | ||||
| Province by confirmed patients | 4.169 | 0.244 | 2.374 | 0.498 | ||
| Low case area | 24 (1.7) | 30 (2.2) | ||||
| Low-medium case area | 38 (2.7) | 41 (3.0) | ||||
| Medium case area | 42 (2.5) | 39 (2.3) | ||||
| High case area | 18 (3.0) | 4 (1.9) | ||||
| It is difficult for me to find correct and comprehensive information about COVID-19 | 19.21 | <0.001 | 5.448 | 0.066 | ||
| Disagree | 24 (1.4) | 30 (1.8) | ||||
| Neutral | 39 (2.3) | 39 (2.5) | ||||
| Agree | 59 (3.7) | 45 (3.1) | ||||
| It is difficult for me to understand information I got about COVID-19 | 25.87 | <0.001 | 16.17 | <0.001 | ||
| Disagree | 43 (1.5) | 46 (1.8) | ||||
| Neutral | 45 (3.1) | 37 (2.8) | ||||
| Agree | 34 (4.5) | 31 (4.4) | ||||
*Participants who lived in Wuhan were automatically exempted from stigma questions related to residents of Wuhan.
Logistic regression (table 4) indicated that participants aged over 40, who were of ethnic minorities (adjusted OR (aOR)=2.71, 95% CI (1.67 to 4.38)) and who felt it was difficult to find and understand information about COVID-19 (aOR=1.91, 95% CI (1.08 to 3.37); aOR=1.88, 95% CI (1.08 to 3.29)) were more likely to stigmatise patients with COVID-19. Compared with people living in low case areas, people living in low-medium and high case areas were 1.74 and 2.03 times more likely to stigmatise patients with COVID-19, respectively. Females were found to be less likely to stigmatise residents of Wuhan when compared with males (aOR=0.55, 95% CI (0.38 to 0.81)). Participants aged 41–50 and those with difficulty understanding information (aOR=2.08, 95% CI (1.17 to 3.69)) were more likely to stigmatise residents of Wuhan.
Table 4.
Factors associated with COVID-19-related stigma
| Individual stigma towards patients with COVID-19 (N=5039) |
Individual stigma towards Wuhan residents (n=4628)† |
|||
| Model 1‡ aOR (95% CI) |
Model 2§ aOR (95% CI) |
Model 1‡ aOR (95% CI) |
Model 2§ aOR (95% CI) |
|
| Gender (ref: male) | ||||
| Female | 0.73 (0.51 to 1.05) | 0.79 (0.55 to 1.15) | 0.52 (0.36 to 0.76)** | 0.55 (0.38 to 0.81)** |
| Age (ref: ≤20) (years) | ||||
| 21–30 | 1.77 (0.81 to 3.83) | 1.67 (0.77 to 3.64) | 1.87 (0.93 to 3.77) | 1.80 (0.89 to 3.64) |
| 31–40 | 2.11 (0.88 to 5.05) | 2.08 (0.87 to 5.01) | 2.17 (0.97 to 4.87) | 2.14 (0.95 to 4.81) |
| 41–50 | 4.00 (1.82 to 8.79)** | 3.99 (1.81 to 8.83)** | 2.34 (1.09 to 5.04)* | 2.34 (1.09 to 5.05)* |
| ≥51 | 5.21 (2.31 to 11.73)*** | 5.28 (2.34 to 11.94)*** | 2.05 (0.88 to 4.76) | 2.03 (0.87 to 4.74) |
| Educational level (ref: junior high school or less) | ||||
| Senior high school and junior college | 0.85 (0.51 to 1.42) | 0.96 (0.57 to 1.60) | 0.94 (0.54 to 1.65) | 1.06 (0.60 to 1.85) |
| College and above | 0.67 (0.37 to 1.22) | 0.82 (0.45 to 1.51) | 0.64 (0.34 to 1.21) | 0.76 (0.40 to 1.45) |
| Ethnicity (ref: Han) | ||||
| Minorities | 2.68 (1.66 to 4.32)*** | 2.71 (1.67 to 4.38)*** | 1.52 (0.93 to 2.50) | 1.52 (0.93 to 2.50) |
| Urbanicity (ref: urban) | ||||
| Rural | 0.86 (0.58 to 1.28) | 0.87 (0.58 to 1.30) | 0.97 (0.65 to 1.45) | 0.96 (0.64 to 1.44) |
| Monthly household income (US$) (ref: <422) | ||||
| 422–704 | 1.36 (0.79 to 2.34) | 1.52 (0.88 to 2.63) | 1.11 (0.64 to 1.95) | 1.18 (0.67 to 2.07) |
| 705–1407 | 0.82 (0.44 to 1.52) | 0.95 (0.51 to 1.77) | 1.01 (0.56 to 1.83) | 1.11 (0.61 to 2.03) |
| 1408–2815 | 0.92 (0.45 to 1.88) | 1.08 (0.53 to 2.21) | 1.02 (0.51 to 2.06) | 1.14 (0.56 to 2.31) |
| >2815 | 1.23 (0.55 to 2.76) | 1.55 (0.68 to 3.50) | 1.00 (0.41 to 2.41) | 1.15 (0.48 to 2.80) |
| Province by confirmed patients (ref: low case area) | ||||
| Low-medium case area | 1.77 (1.04 to 3.00)* | 1.74 (1.02 to 2.96)* | 1.44 (0.88 to 2.34) | 1.40 (0.86 to 2.29) |
| Medium case area | 1.64 (0.96 to 2.79) | 1.61 (0.94 to 2.74) | 1.10 (0.67 to 1.81) | 1.09 (0.66 to 1.80) |
| High case area | 2.15 (1.12 to 4.13)* | 2.03 (1.05 to 3.92)* | 0.78 (0.26 to 2.29) | 0.78 (0.26 to 2.29) |
| It is difficult for me to find correct and comprehensive information about COVID-19 (ref: disagree) | ||||
| Neutral | 1.49 (0.85 to 2.62) | 1.20 (0.70 to 2.06) | ||
| Agree | 1.91 (1.08 to 3.37)* | 1.12 (0.64 to 1.98) | ||
| It is difficult for me to understand information I got about COVID-19 (ref: disagree) | ||||
| Neutral | 1.62 (1.01 to 2.61)* | 1.40 (0.86 to 2.29) | ||
| Agree | 1.88 (1.08 to 3.29)* | 2.08 (1.17 to 3.69)* | ||
*p<0.05, **p<0.01, ***p<0.001.
†Participants who lived in Wuhan were automatically exempted from stigma questions related to residents of Wuhan.
‡Model 1 was a logistic regression analysis without considering the health literacy.
§Model 2 included the health literacy to see the possible impact of health literacy on stigmatising attitudes.
aOR, adjusted OR.
Discussion
To our knowledge, there are currently few studies investigating public COVID-19-related stigma during the early stage of the pandemic in China. Our study described the situation of stigma towards patients with COVID-19 and residents of Wuhan at both the individual and the community levels. Consequently, our results verified the correlation between better health literacy and lower stigma during a pandemic of an emerging infectious disease and showed the difference in stigma in regions with different COVID-19 epidemic severities on a large scale across China. Additionally, we identified that sociodemographic factors, such as gender, age and ethnicity, affected public COVID-19-related stigma.
Historically, infectious diseases have long been associated with stigma. During the early stage of the COVID-19 pandemic, potentially deadly conditions, the lack of effective treatments, and rumours increased the risk of stigmatisation. The stigma associated with COVID-19 threatens the physical and mental health of patients with COVID-19 and residents of Wuhan. In the long run, stigmatisation also damages the cultural fabric of society and undermines efforts to control pandemics, creating an atmosphere of fear and distrust. Previous studies identified COVID-19-related public stigma as more prevalent and severe when compared with our findings. According to a global survey involving 173 countries, nearly a third of participants believed that people talked badly or gossiped about other people who were thought to be associated with COVID-19, and 21.9% of participants believed people who had COVID-19 were not respected by the community.30 An online survey in February 2020 in China also showed that about half of participants reported they would avoid people from Hubei and 16.9% would even try to expel them from their communities.31 The low prevalence of stigma in our study may be partly explained by the fact that the Chinese government began campaigns in the media to reduce stigma towards patients with COVID-19 and people from Wuhan during the early stage of the pandemic.31 COVID-19-related stigma is not unique to China and has been reported in the USA, Australia, Nepal and other countries.17 These facts should remind health policy makers to attach more importance to community-based stigma reduction interventions and campaigns.
Our study added to the literature by exposing the negative association between health literacy and COVID-19-related stigma. Stigma can be understood as a human instinct to protect themselves from potentially fatal infectious diseases,32 even though this instinctual response often leads to bias.33 Lack of knowledge has been shown to be a major driver of these biases and stigmatisations. Previous studies on mental disease identified a negative correlation between health literacy and stigma.34 35 Consequently, in the field of infectious diseases, higher literacy concerning one disease may possibly help reduce disease-related stigma. Our study suggested that higher COVID-19-related health literacy, specifically, a better ability to find and understand COVID-19 information, might help reduce stigma towards patients with COVID-19 and residents of Wuhan. Additionally, it has been suggested that health literacy interventions, such as educational lectures to improve public knowledge and literacy, could help reduce stigma in the field of mental health.36 Thus, further studies are needed to verify effective measures to reduce stigma during an emerging infectious disease, such as information campaigns from health services or the media, and sessions in workplaces and schools.
To reduce stigma, this study described the geographic distribution of stigma during the early stage of the pandemic to improve intervention precision by allowing for the targeting of high-stigma areas. Our research found that people in different regions held differing degrees of stigmatisation. In general, provinces that were close to Wuhan, such as Anhui and Chongqing, and provinces with more ethnic minorities, such as Yunnan and Guizhou, had higher levels of stigma towards patients with COVID-19. Similarly, the proportion of respondents who held stigma towards residents of Wuhan was relatively high in provinces close to Wuhan, such as Henan, Chongqing and Shanxi, and provinces with more ethnic minorities such as Qinghai, Yunnan, Guizhou and Ningxia. A study using South Korean data revealed that the risk of COVID-19 increased with higher area morbidity,37 and the danger appraisal hypothesis stated that an individuals’ perception of danger would make them choose a safer social distance.38 Another study on SARS-related stigma conducted in Hong Kong showed that living in a geographical location with a large number of cases could increase stigmatising attitudes. Specifically, residents living on the block with the most patients with SARS reported holding the highest level of stigmatising attitudes.13 During the COVID-19 pandemic, most countries around the world reported high-risk perceptions.39 Similarly, in our study, people living in areas severely affected by the COVID-19 pandemic were at higher risk of social interaction with potential patients with COVID-19. Thus, they might have higher risk perceptions, expect to have less social interaction with potential patients with COVID-19 and therefore may hold higher levels of stigma. Interestingly, there was no significant regional difference in attitudes towards residents of Wuhan. A possible reason was that the public perceived the risk posed by patients with COVID-19 to be higher than that posed by residents of Wuhan.
Our study also showed the influence of sociodemographic characteristics on public COVID-19-related stigma, which might help identify subgroups that are more likely to stigmatise others during the pandemic. Consistent with previous studies, we found females were more tolerant towards residents of Wuhan, while people over 40 years old and ethnic minorities were more likely to stigmatise patients with COVID-19.15 40 The elderly were more likely to progress to severe disease after infection or suffer complications from COVID-19 than younger adults, and had higher perceived susceptibility and perceived severity during the pandemic,41 which might explain why the elderly were more likely to hold stigmatising attitudes. The majority of ethnic minorities in China live in less developed mountainous inland or border districts in the western region, and possess relatively low levels of education and income, which have been identified as negative influencing factors for stigma in previous studies and may partially explain their higher levels of stigmatisation.42 43 A previous study revealed that groups with higher education and income levels had lower levels of stigma towards patients with related diseases.22 However, this difference was not found in our study. One possible reason for this may be that, during the COVID-19 pandemic, China conducted a large-scale publicity campaign through traditional and social media, such as China Central Television, WeChat official accounts and short video platforms,44 which may have helped reduce barriers related to education and economic status in accessing adequate information concerning COVID-19.
There are some limitations to this study. First, this is a cross-sectional study, so it cannot verify the causal relationship between stigma-related variables. Second, this is an online survey, and people who did not have access to the internet were not included, which may result in selection bias. However, as of December 2020, China’s internet penetration rate was 70.4%, and most people in China had access to the internet via smartphones.45 Third, health literacy and stigmatising attitudes rely on self-reporting and may thus lead to an underestimation of the impact of health literacy on stigma.46 Fourth, we chose a snowball sampling method rather than a representative sampling method, due to the social distancing policies in place during our investigation. However, we ensured both the balance of urban–rural samples and the randomness of each sample in each household during the survey to reduce related bias. Fifth, this study does not differentiate among participants by their profession or relationship to the disease. It is possible that health personnel or those who have been discriminated against and know the reality of the virus offered different responses, just as people who have been infected may also show less stigma (although the number of people reporting infection in our surveyed population was low).
Conclusion
Patients with COVID-19 and residents of Wuhan have suffered stigma at both the individual and the community levels. Those who had low health literacy, who lived in areas with a large number of COVID-19 cases and who were of ethnic minorities were more likely to stigmatise others in the early stage of the pandemic. Although a COVID-19 vaccine is available globally, it will still take time to achieve herd immunity. We recommend joint actions of all sectors of our society, including but not limited to governments, health institutions and public figures, such as athletes, communicators and social influencers to reduce the COVID-19-related stigmatisation. Health policy makers should include early prevention and elimination of stigma into emergency preparedness plans for infectious diseases. Community-based stigma reduction interventions targeted the ethnic minorities and those lived near the epidemic centre are encouraged to support the most stigmatised groups. In addition, information campaigns to offer a better access and easy understandable messages thus to increase public health literacy of infectious diseases by medical authorities and the media are recommended.
Supplementary Material
Acknowledgments
We would like to thank Jiayao Xu, Yiyi Zhou, Fangyuan Jiang and Yuling Wan for their great assistance to conduct this survey. We are grateful to data collectors for their work and all respondents for their participation in the study. We would like to thank Xianhong Huang for reviewing the data analysis.
Footnotes
XW and HZ contributed equally.
Contributors: XZ, XW and HZ made substantial contributions to the study design and supervised the data collection. TJ, LL, YZ and YP contributed to the data collection and interpretation. TJ wrote the substantial parts of the manuscript. All authors critically revised, reviewed and approved the final version the manuscript.
Funding: This research study was supported by the National Social Science Fund of China (grant number 20VYJ063) and Zhejiang University Special Scientific Research Fund for COVID-19 Prevention and Control (grant number 2020XGZX045). The funding body has no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The protocol for this study was approved by the Ethics Committee of the School of Public Health, Zhejiang University (No. ZGL202002-3).
References
- 1.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health 2013;103:777–80. 10.2105/AJPH.2012.301056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pescosolido BA. The public stigma of mental illness: what do we think; what do we know; what can we prove? J Health Soc Behav 2013;54:1–21. 10.1177/0022146512471197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng C, Li X, Du H, et al. Experiences of stigma and health service utilization among young rural-to-urban migrants in China: the mediation role of social capital. Vulnerable Child Youth Stud 2020;15:97–109. 10.1080/17450128.2019.1640918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elliot VL, Morgan D, Kosteniuk J, et al. Health-related stigma of noncommunicable neurological disease in rural adult populations: a scoping review. Health Soc Care Community 2019;27:e158–88. 10.1111/hsc.12694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnyder N, Panczak R, Groth N, et al. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry 2017;210:261–8. 10.1192/bjp.bp.116.189464 [DOI] [PubMed] [Google Scholar]
- 6.Cobos Manuel I, Jackson-Perry D, Courvoisier C, et al. [Stigma and HIV: relevant for everyone]. Rev Med Suisse 2020;16:744–8. [PubMed] [Google Scholar]
- 7.Ware KB. Assessment of pharmacy student perceptions toward common stigmas associated with persons living with HIV. Am J Pharm Educ 2020;84:ajpe7270. 10.5688/ajpe7270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeng C, Li L, Hong YA, et al. A structural equation model of perceived and internalized stigma, depression, and suicidal status among people living with HIV/AIDS. BMC Public Health 2018;18:138. 10.1186/s12889-018-5053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asamoah CK, Asamoah BO, Agardh A. A generation at risk: a cross-sectional study on HIV/AIDS knowledge, exposure to mass media, and stigmatizing behaviors among young women aged 15-24 years in Ghana. Glob Health Action 2017;10:1331538. 10.1080/16549716.2017.1331538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George LS, Rakesh PS, Vijayakumar K, et al. Social stigma associated with TB and HIV/AIDS among Kudumbashree members: a crosssectional study. J Family Med Prim Care 2020;9:4062–6. 10.4103/jfmpc.jfmpc_437_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mukerji R, Turan JM. Exploring manifestations of TB-related stigma experienced by women in Kolkata, India. Ann Glob Health 2018;84:727–35. 10.29024/aogh.2383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang S-H, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis 2014;18:168–73. 10.5588/ijtld.13.0181 [DOI] [PubMed] [Google Scholar]
- 13.Lee S, Chan LYY, Chau AMY, et al. The experience of SARS-related stigma at Amoy gardens. Soc Sci Med 2005;61:2038–46. 10.1016/j.socscimed.2005.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Person B, Sy F, Holton K. National center for infectious diseases/SARS community outreach team. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis 2004;10:358–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong LP. Prevalence and factors associated with HIV/AIDS-related stigma and discriminatory attitudes: a cross-sectional nationwide study. Prev Med 2013;57 Suppl:S60–3. 10.1016/j.ypmed.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 16.Fischer LS, Mansergh G, Lynch J, et al. Addressing disease-related stigma during infectious disease outbreaks. Disaster Med Public Health Prep 2019;13:989–94. 10.1017/dmp.2018.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh R, Subedi M. COVID-19 and stigma: social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian J Psychiatr 2020;53:102222. 10.1016/j.ajp.2020.102222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duan W, Bu H, Chen Z. COVID-19-related stigma profiles and risk factors among people who are at high risk of contagion. Soc Sci Med 2020;266:113425. 10.1016/j.socscimed.2020.113425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 20.Wei Y, McGrath PJ, Hayden J, et al. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry 2015;15:291. 10.1186/s12888-015-0681-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackert M, Mabry-Flynn A, Donovan EE, et al. Health literacy and perceptions of stigma. J Health Commun 2019;24:856–64. 10.1080/10810730.2019.1678705 [DOI] [PubMed] [Google Scholar]
- 22.Johnco C, Rapee RM. Depression literacy and stigma influence how parents perceive and respond to adolescent depressive symptoms. J Affect Disord 2018;241:599–607. 10.1016/j.jad.2018.08.062 [DOI] [PubMed] [Google Scholar]
- 23.Mackert M, Donovan EE, Mabry A, et al. Stigma and health literacy: an agenda for advancing research and practice. Am J Health Behav 2014;38:690–8. 10.5993/AJHB.38.5.6 [DOI] [PubMed] [Google Scholar]
- 24.Hoppe T. “Spanish flu”: when infectious disease names blur origins and stigmatize those infected. Am J Public Health 2018;108:1462–4. 10.2105/AJPH.2018.304645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect 2020;80:401–6. 10.1016/j.jinf.2020.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Datiko DG, Jerene D, Suarez P. Stigma matters in ending tuberculosis: nationwide survey of stigma in Ethiopia. BMC Public Health 2020;20:190. 10.1186/s12889-019-7915-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Zhou X, Leesa L, et al. The effect of vaccine literacy on parental trust and intention to vaccinate after a major vaccine scandal. J Health Commun 2018;23:413–21. 10.1080/10810730.2018.1455771 [DOI] [PubMed] [Google Scholar]
- 28.Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12:80. 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chowdhury MRK, Rahman MS, Mondal MNI, et al. Social impact of stigma regarding tuberculosis hindering adherence to treatment: a cross sectional study involving tuberculosis patients in Rajshahi City, Bangladesh. Jpn J Infect Dis 2015;68:461–6. 10.7883/yoken.JJID.2014.522 [DOI] [PubMed] [Google Scholar]
- 30.Dye TD, Alcantara L, Siddiqi S, et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open 2020;10:e046620. 10.1136/bmjopen-2020-046620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He J, He L, Zhou W, et al. Discrimination and social exclusion in the outbreak of COVID-19. Int J Environ Res Public Health 2020;17:2933. 10.3390/ijerph17082933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhanot D, Singh T, Verma SK, et al. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2021;8:577018. 10.3389/fpubh.2020.577018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baldassarre A, Giorgi G, Alessio F, et al. Stigma and discrimination (SAD) at the time of the SARS-CoV-2 pandemic. Int J Environ Res Public Health 2020;17:6341. 10.3390/ijerph17176341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Svensson B, Hansson L. How mental health literacy and experience of mental illness relate to stigmatizing attitudes and social distance towards people with depression or psychosis: a cross-sectional study. Nord J Psychiatry 2016;70:309–13. 10.3109/08039488.2015.1109140 [DOI] [PubMed] [Google Scholar]
- 35.Lopez V, Sanchez K, Killian MO, et al. Depression screening and education: an examination of mental health literacy and stigma in a sample of Hispanic women. BMC Public Health 2018;18:646. 10.1186/s12889-018-5516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Milin R, Kutcher S, Lewis SP, et al. Impact of a mental health curriculum on knowledge and stigma among high school students: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2016;55:383–91. 10.1016/j.jaac.2016.02.018 [DOI] [PubMed] [Google Scholar]
- 37.Weinstein B, da Silva AR, Kouzoukas DE, et al. Precision mapping of COVID-19 vulnerable locales by epidemiological and socioeconomic risk factors, developed using South Korean data. Int J Environ Res Public Health 2021;18:604. 10.3390/ijerph18020604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tee YC, Earnshaw VA, Altice FL, et al. Evaluating physicians’ intention to discriminate against patients living with HIV in Malaysia. AIDS Behav 2019;23:1039–47. 10.1007/s10461-018-2362-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dryhurst S, Schneider CR, Kerr J, et al. Risk perceptions of COVID-19 around the world. J Risk Res 2020;23:994–1006. 10.1080/13669877.2020.1758193 [DOI] [Google Scholar]
- 40.Mannarini S, Rossi A. Assessing mental illness stigma: a complex issue. Front Psychol 2018;9:2722. 10.3389/fpsyg.2018.02722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Irigoyen-Camacho ME, Velazquez-Alva MC, Zepeda-Zepeda MA, et al. Effect of income level and perception of susceptibility and severity of COVID-19 on Stay-at-Home preventive behavior in a group of older adults in Mexico City. Int J Environ Res Public Health 2020;17:7418. 10.3390/ijerph17207418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ransing R, Ramalho R, de Filippis R, et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brain Behav Immun 2020;89:555–8. 10.1016/j.bbi.2020.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang S, Lo ECM, Liu J, et al. A review of the dental caries status of ethnic minority children in China. J Immigr Minor Health 2015;17:285–97. 10.1007/s10903-013-9916-3 [DOI] [PubMed] [Google Scholar]
- 44.Zhong B-L, Luo W, Li H-M, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020;16:1745–52. 10.7150/ijbs.45221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.China Internet Network Information Center . Statistical report on the development of the Internet in China, 2021. Available: https://http://www.cnnic.net.cn/
- 46.Michaels PJ, Corrigan PW. Measuring mental illness stigma with diminished social desirability effects. J Ment Health 2013;22:218–26. 10.3109/09638237.2012.734652 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-048983supp001.pdf (122.3KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.


