Abstract
Brewed tea (Camellia sinensis) is a major dietary source of flavonoids, in particular flavan-3-ols. Tea consumption has been suggested to be inversely associated with a decreased risk of cardiovascular disease (CVD). Several biological mechanisms support the inverse relationship between tea flavonoid intake and CVD risk. Given the recent accumulating evidence from various systematic reviews regarding the role of tea as a beverage in reducing CVD risk and severity, we conducted an umbrella review to describe and critically evaluate the totality of evidence to date. We searched the PubMed, Web of Science, Cochrane Database of Systematic Reviews, and BIOSIS databases for systematic reviews published between January 1, 2010 and February 22, 2020 reporting relationships between tea (C. sinensis) consumption and CVD mortality, CVD diagnosis or incidence, CVD events, stroke events, blood pressure, endothelial function, blood lipids and triglycerides, and inflammatory markers. Herein, we describe results from 23 included systematic reviews. Consistently consuming 2 cups of unsweet tea per day offers the right levels of flavonoids to potentially decrease CVD risk and its progression. This is supported by the consistency between a recent high-quality systematic review and dose-response meta-analyses of population-based studies demonstrating beneficial effects of consumption on CVD mortality, CVD events and stroke events and medium- to high-quality systematic reviews of intervention studies that further elucidate potential benefits on both validated (i.e., SBP, DBP, total cholesterol, and LDL-cholesterol) and emerging risk biomarkers of CVD (TNF-ɑ and IL-6). On the basis of this umbrella review, the consumption of tea as a beverage did not seem to be harmful to health; therefore, the benefits of moderate consumption likely outweigh risk. Future large, clinical intervention studies will provide better mechanistic insight with the ability to confirm the outcome effects shown across observational studies. The review protocol was registered on PROSPERO (https://www.crd.york.ac.uk/PROSPERO/) as CRD42020218159.
KEY MESSAGES
It is reasonable to judge that 2 cups of unsweet tea per day has the potential to decrease CVD risk and progression due to its flavonoid content.
The primary side effects of tea documented in human studies are hepatotoxicity and gastrointestinal disturbances (i.e., vomiting and diarrhea) after high-dose supplemental intake.
Additional clinical research is needed to fully elucidate the effects of tea flavonoids on markers of CVD, as many studies were under-powered to detect changes.
Keywords: Tea, cardiovascular diseases, Camellia sinensis, flavonoids, heart diseases
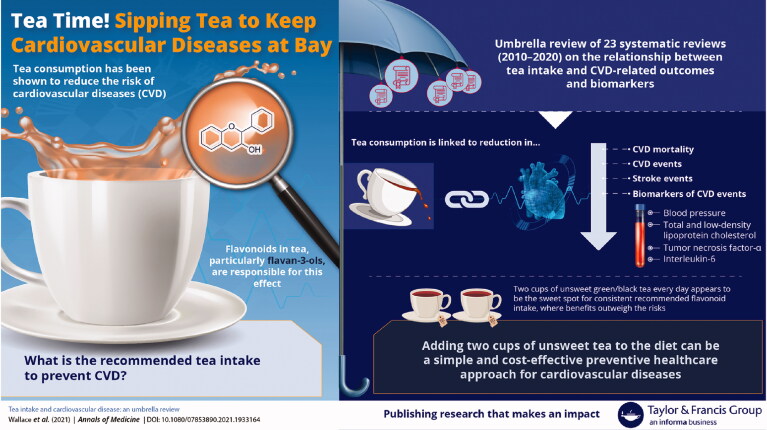
Graphical Abstract
Introduction
Brewed tea (Camellia sinensis) is a major dietary source of flavonoids, in particular flavan-3-ols [1]. Results of population studies commonly suggest that tea consumption is inversely associated with several health outcomes [2]. Shorter-term clinical intervention studies provide additional evidence that tea consumption has the potential to affect intermediate outcomes and biomarkers of disease in healthy, at-risk, and diseased populations [3,4]. Several recent systematic reviews have demonstrated these distinct effects, particularly in regard to cardiovascular disease (CVD) [2–4], the leading cause of death worldwide [5,6]. In the presence of suboptimal fruit, vegetable, and whole grain intake [7], unsweet tea may have increased potential to improve human health by providing consumers plant-derived dietary bioactive compounds such as flavonoids. This idea is supported by food intake data indicating that tea is a commonly consumed beverage worldwide; tea intake is secondary only to water [8]. Approximately one-fifth of Americans report drinking tea on a daily basis [9]. Tea consumers are shown to have about 20 times the flavonoid intake of non-consumers [9]. However, the amount of flavonoids and other dietary bioactives present in tea depends on several factors, including (1) their concentration in tea leaves; (2) the quantity of tea leaves used to prepare the infusion; (3) the volume of water used to prepare the infusion; (4) the water temperature, brew time, and agitation used to prepare the infusion; (5) the pH of the water used to prepare the infusion, thermal processing (for commercial preparations), and duration between preparation and consumption; and (6) the volume of tea consumed [1]. Similarly, the chemical composition of commercial tea extracts can vary greatly depending on the source material, extraction technique (e.g., water, alcohol, other solvent), type of industrial processing, and nature of the finished product.
Several biological mechanisms support the inverse relationship between tea flavonoid intake and CVD risk. The effects of tea flavonoids on endothelial function, nitric oxide–dependent vasorelaxation, and blood pressure are among the biological mechanisms cited most frequently in the peer-reviewed scientific literature [1,3,4,8,10,11]. The effects of tea on health are expected to be somewhat contingent on how tea is consumed (e.g., unsweet vs. sweetened). It is also important to note that exposures encountered from the use of pure compounds and tea extracts (e.g., dietary supplements) tend to be much higher in dose and have been shown to exhibit different efficacy and safety profiles. A 2018 systematic review of 159 intervention studies found that green tea preparations result in hepatic adverse events in a dose-dependent manner when ingested in large bolus amounts but not when consumed as brewed tea or extracts in beverages, or as a component of food [12]. According to the U.S. Department of Agriculture (USDA) Flavonoid Database [13], one cup (236.6 mL) of black or green tea provides approximately 280 or 338 mg of total flavonoids to the diet, respectively.
Given the recent accumulating evidence from various systematic reviews regarding the role of tea as a beverage in reducing CVD risk and severity, we conducted an umbrella review to describe and critically evaluate the totality of evidence to date.
Materials and methods
An umbrella review of systematic reviews was conducted and is presented according to standardised methodology [14–16]. The review protocol was registered on PROSPERO (https://www.crd.york.ac.uk/PROSPERO/) as CRD42020218159. Two authors (TCW and AK) independently performed abstract and full-text screening, data extraction, and quality assessment of included systematic reviews. Discrepancies were resolved by consensus.
Data sources and literature search
We searched the PubMed, Web of Science, Cochrane Database of Systematic Reviews, and BIOSIS databases for systematic reviews published between January 1, 2010 and February 22, 2020 reporting relationships between tea (C. sinensis) consumption and CVD mortality, CVD diagnosis or incidence, CVD events, stroke events, blood pressure, endothelial function, blood lipids and triglycerides, and inflammatory markers. Detailed search terms and strategies used for each database are presented in Supplemental Table 1. Missing data or additional information were requested from corresponding authors of articles when necessary.
Table 1.
Characteristics of included systematic reviews of population-based studies.
| Reference | Variable | Mean Age (y) | Study Population (Age ≥ 18 y) |
Included Studies (N) | Follow-Up (y) | Quality (ROB) Assessment |
Effects Model | Meta-Analysis Outcomes |
Heterogeneity |
Quality of Systematic Review | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR (95% CI) | p Value | I2 (%) | p Value | |||||||||
| CVD mortality | ||||||||||||
| Chung et al. [2] | Green and black tea | NR | Healthy | 17 | 5–18.7 | New Castle-Ottawa | Mixed(dose-response) | 0.96 (0.94 to 0.98) | .0001 | 72.4 | .0001 | High |
| Green and black tea | <65 | Healthy | 15 | 7.7–18.7 | New Castle-Ottawa | Mixed(dose-response) | 0.98 (0.96 to 0.99) | .012 | 58.5 | .002 | ||
| Green and black tea | ≥65 | Healthy | 4 | 5–11 | New Castle-Ottawa | Mixed(dose-response) | 0.89 (0.83 to 0.96) | .001 | 59.5 | .06 | ||
| CVD events CVD events | ||||||||||||
| Chung et al. [2] | Green and black tea | NR | Healthy | 7 | 5.6–15 | New Castle-Ottawa | Mixed(dose-response) | 0.98 (0.96 to 1.00) | .085 | 76.5 | .0001 | High |
| Zhang et al. [33] | Green and black tea | NR | NR | 4 | 3.8–24 | New Castle-Ottawa | Random (dose-response) | 0.73 (0.53 to 0.99) | .045 | NR | NR | Moderate |
| Stroke events | ||||||||||||
| Chung et al. [2] | Green and black tea | NR | Healthy | 13 | 5–24 | New Castle-Ottawa | Mixed(dose-response) | 0.96 (0.93 to 0.99) | .002 | 63.9 | .001 | High |
| Shen et al. [29] | Green tea | 20–89 | Healthy | 5 | Median: 11.5 | NR | Random (dose-response) | 0.83 (0.72 to 0.96) | <.01 | 70.2 | NR | Critically low |
| Black tea | 20–89 | Healthy | 13 | Median: 11.5 | NR | Random (dose-response) | 0.91 (0.83 to 0.98) | 0.17 | 26.8 | NR | ||
| Zhang et al. [33] | Green and black tea/placebo | NR | NR | 2 | 3.8–24 | New Castle-Ottawa | Random (dose-response) | 0.82 (0.73 to 0.92) | .001 | 77 | <.001 | Moderate |
95% CI = 95% confidence interval, NR = not reported, ROB = risk of bias, RR = relative risk.
Study selection
Inclusion and exclusion criteria used to assess study eligibility incorporated the PICOS (Population, Intervention, Comparison, Outcome, Study design) format and are presented using the USDA Nutrition Evidence Systematic Review format [7]. Inclusion and exclusion criteria are presented in Supplemental Table 2. Systematic review eligibility was restricted to peer-reviewed, English-language studies in adults (aged ≥18 years). Systematic reviews that solely assessed effects of alcohol or solvent extracts of tea leaves, tea supplements, or herbal teas were excluded from this umbrella review. Reference lists of included systematic reviews were cross-checked to ensure no relevant systematic reviews were overlooked.
Table 2.
Characteristics of included systematic reviews of clinical trials.
| Reference | Intervention/ Control | Intervention/ Control (N) | Age (y) | Study Population (Age ≥ 18 y) | Included Studies (N) | Follow-Up | Quality (ROB) Assessment | Effects Model | Meta-Analysis Outcomes |
Heterogeneity |
Quality of Systematic Review | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | p Value | I2 (%) | p Value | ||||||||||
| Total cholesterol | |||||||||||||
| Araya-Quintanilla et al. [18] | Black tea/placebo | 243/172 | 53.22 | Hypercholesterolaemia or high cholesterol diagnosis | 6 | 3–20 wk | Cochrane | Random | MD: −1.67 mg/dL (−5.47 to 8.80) | .65 | 100 | <.00001 | Low |
| Asbaghi et al. [19] | Green tea/placebo | 300/212 | 50–65 | Type2 diabetes | 7 | 4–16 wk | Cochrane | Random | WMD: −6.81 mg/dL (−15.13 to 1.52) | .109 | 83 | .000 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 75/42 | 25–60 | Healthy or high CVD risk | 3 | 3–6 mo | Cochrane | Random | MD: NR | NR | 84 | NR | High |
| Green tea/placebo | 172/155 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: −0.62 mmol/L (−0.77 to − 0.46) | NR | N/A | NR | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 184/136 | ≥18 | Healthy | 5 | 4–24 wk | Cochrane | Random | WMD: 6.82 mg/dL (−2.79 to 16.44 | NR | 0.0 | .857 | High |
| Green and black tea/placebo | 219/201 | ≥18 | Atrisk of CVD | 7 | 4–24 wk | Cochrane | Random | WMD: 1.36 mg/dL (−4.05 to 6.77 | NR | 0.0 | .939 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/ 117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 11 | 3–16 wk | Downs and Black’s | Random | MD: −0.15 mmol/L (−0.27 to − 0.02) | NR | 55 | NR | Moderate |
| Kim et al. [22] | Green tea/placebo | NR | 11–65 | All (included some adolescents) | 19 | 3–24 wk | ADA Research Design Implementation Checklist | Random | WMD: −5.46 mg/dL (−9.59 to − 1.32) | NR | 45 | NR | Low |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 12 | NR | Cochrane | Random | SMD: −0.24 mmol/L (−0.47 to 0.00) | .05 | 68 | NR | Moderate |
| Black tea/placebo | 138/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 3 | NR | Cochrane | Fixed | SMD: −0.16 mmol/L (−0.43 to 0.10) | .24 | 41 | NR | ||
| Green tea/placebo | 451/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 9 | NR | Cochrane | Random | SMD: −0.26 mmol/L (−0.57 to 0.05) | .10 | 74 | NR | ||
| Liu et al. [30] | Green and black tea/placebo | 291/292 | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: −0.37 mmol/L (−1.01 to 0.26) | .290 | 93 | <.01 | Low |
| Onakpoya et al. [27] | Green tea/placebo | 1487 (total) | 6–71 | Normotensive or hypertensive | 19 | 3–24 wk | Independently assessed | Random | MD:−0.13 mmol/L (−0.2 to 0.07) | NR | 8 | <.0001 | Moderate |
| Xu et al. [31] | Green tea/placebo | 3024 (total) | NR | Normal weight, overweight, or obese | 31 | 3 wk to 12 mo | Cochrane | Random | WMD:−4.66 mg/dL (−6.36 to − 2.96) | <.0001 | 23.2 | .124 | Low |
| Zhao et al. [34] | Black tea/placebo | 15–77 | NR | Healthy, hypercholesterolaemia, prediabetes | 10 | 3 wk to 6 mo | Jadad | Random | MD: −2.04 mg/dL (−6.43 to 2.35) | .363 | 0 | .472 | High |
| LDL cholesterol | |||||||||||||
| Araya-Quintanilla et al. [18] | Black tea/placebo | 243/172 | 53 | Hypercholesterolaemia | 6 | 3–20 wk | Cochrane | Random | MD: −3.21 mg/dL (−11.02 to 4.60) | .42 | 100 | <.0001 | Low |
| Asbaghi et al. [19] | Green tea/placebo | 277/192 | 50–65 | Type2 diabetes | 6 | 4–16 wk | Cochrane | Random | WMD: −0.37 mg/dL (−4.13 to 3.40) | .849 | 46.5 | .082 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 92/52 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD:−0.43 mmol/L (−0.56 to − 0.31) | NR | 34 | <.0001 | High |
| Green tea/placebo | 172/155 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: −0.64 mmol/L (−0.77 to − 0.52) | NR | 21 | <.0001 | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 149/114 | ≥18 | Healthy | 3 | 4–24 wk | Cochrane | Random | WMD: 3.84 mg/dL (−6.96 to 14.64 | NR | 0.0 | .620 | High |
| Green and black tea/placebo | 219/198 | ≥18 | Atrisk of CVD | 7 | 4–24 wk | Cochrane | Random | WMD: 0.72 mg/dL (−5.76 to 7.20 | NR | 19.4 | .281 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 10 | 3–16 wk | Downs and Black’s | Random | MD: −0.16 mmol/L (−0.22 to − 0.09) | NR | 0 | NR | Moderate |
| Kim et al. [22] | Green tea/placebo | NR | 11–65 | All (included some adolescents) | 19 | 3–24 wk | ADA Research Design Implementation Checklist | Random | WMD: −5.30 mg/dL (−9.99 to − 0.62) | NR | 71 | <.08 | Low |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 14 | NR | Cochrane and Jadad | Random | SMD: −0.31 mmol/L (−0.55 to − 0.06) | NR | 75 | .01 | Moderate |
| Black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 4 | NR | Cochrane and Jadad | Random | SMD: −0.29 mmol/L (−1.02 to 0.43) | NR | 89 | .43 | ||
| Green tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 10 | NR | Cochrane and Jadad | Random | SMD: −0.30 mmol/L (−0.52 to − 0.08) | NR | 59 | .0008 | ||
| Liu et al. [30] | Green and black tea/placebo | 305/306 | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: −0.63 mmol/L (−1.06 to − 0.20) | .0057 | NR | NR | Low |
| Momose et al. [26] | Green tea/placebo | 1339 (total) | 28–60 | Healthy | 17 | 3–14 wk | Jadad | Random | WMD: −7.38 mg/dL (−9.25 to − 5.50) | <.00001 | 25 | .16 | Critically low |
| Onakpoya et al. [27] | Green tea/placebo | 1422 (total) | 6–71 | Normotensive or hypertensive | 17 | 3–24 wk | Independently assessed | Random | MD: −0.19 mmol/L (−0.3 to 0.09) | NR | 70 | .0004 | Moderate |
| Xu et al. [31] | Green tea/placebo | 3005 (total) | NR | Normal weight, overweight, or obese | 29 | 3 wk to 12 mo | Cochrane | Random | WMD: −4.55 mg/dL (−6.31 to − 2.80) | <.0001 | 28.1 | .082 | Low |
| Zhao et al. [34] | Black tea/placebo | 15–77 | NR | Healthy, hypercholesterolaemia, prediabetes | 9 | 3 wk to 6 mo | Jadad | Random | MD: −4.64 mg/dL (−8.99 to − 0.30) | .036 | 0 | .584 | High |
| HDL cholesterol | |||||||||||||
| Araya-Quintanilla et al. [18] | Black tea/placebo | 243/172 | 53 | Hypercholesterolaemia | 6 | 3–20 wk | Cochrane | Random | MD: 0.38 mg/dL (−1.12 to 1.87) | .62 | 100 | <.0001 | Low |
| Asbaghi et al. [19] | Green tea/placebo | 277/192 | 50–65 | Type2 diabetes | 6 | 4–16 wk | Cochrane | Random | WMD: −3.10 mg/dL (−10.16 to 3.95) | .389 | 95.4 | .000 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 90/56 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: −0.01 mmol/L (−0.06 to 0.04) | NR | 36 | .02 | High |
| Green tea/placebo | 177/155 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: 0.01 mmol/L (−0.08 to 0.11) | NR | 39 | .18 | ||
| Green tea/placebo | 177/155 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Fixed | MD: −0.01 mmol/L (−0.27 to 0.07) | NR | NR | NR | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 161/123 | ≥18 | Healthy | 4 | 4–24 wk | Cochrane | Random | WMD: −1.02 mg/dL (−5.65 to 3.61) | NR | 19.1 | .295 | High |
| Green and black tea/placebo | 143/200 | ≥18 | Atrisk of CVD | 7 | 4–24 wk | Cochrane | Random | WMD: 1.16 mg/dL (−0.32 to 2.65) | NR | 0.0 | .829 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 9 | 3–16 wk | Downs and Black’s | Random | MD: 0.01 mmol/L (−0.05 to 0.06) | NR | 49 | .05 | Moderate |
| Kim et al. [22] | Green tea/placebo | NR | 11–65 | All (included some adolescents) | 19 | 3–24 wk | ADA Research Design Implementation Checklist | Random | WMD: −0.27 mg/dL (−1.26 to 1.09) | NR | 51 | >.6 | Low |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 9 | NR | Cochrane and Jadad | Random | SMD: 0.18 mmol/L (0.01 to 0.35) | .03 | 52 | .0004 | Moderate |
| Liu et al. [30] | Green and black tea/placebo | 305/306 | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: 0.13 mmol/L (−0.27 to 0.53) | .3629 | NR | NR | Low |
| Momose et al. [26] | Green tea/placebo | 1339 (total) | 28–60 | Healthy | 17 | 3–14 wk | Jadad | Random | WMD:−0.07 mg/dL (−0.91 to 1.05) | .89 | 80 | <.00001 | Critically low |
| Onakpoya et al. [27] | Green tea/placebo | 1344 (total) | 6–71 | Normotensive or hypertensive | 17 | 3–24 wk | Independently assessed | Random | MD: −0.01 mmol/L (−0.08 to 0.06) | NR | 90 | .79 | Moderate |
| Xu et al. [31] | Green tea/placebo | 3073 (total) | NR | Normal weight, overweight/obese | 29 | 3 wk to 12 mo | Cochrane | Random | WMD: 0.23 mg/dL (−0.45 to 0.91) | .50 | 34.8 | .035 | Low |
| Zhao et al. [34] | Black tea/placebo | 15–77 | NR | Healthy, hypercholesterolaemia, prediabetes | 10 | 3 wk to 6 mo | Jadad | Random | MD: −1.15 mg/dL (−3.04 to 0.75) | .236 | 0 | .616 | High |
| Triglycerides | |||||||||||||
| Araya-Quintanilla et al. [18] | Black tea/placebo | 243/172 | 53 | Hypercholesterolaemia | 6 | 3 wk to 20 wk | Cochrane | Random | MD: 0.28 mg/dL (−3.89 to 4.45) | .90 | 100 | <.0001 | Low |
| Asbaghi et al. [19] | Green tea/placebo | 300/212 | 50–65 | Type2 diabetes | 7 | 4–16 wk | Cochrane | Random | WMD: −12.79 mg/dL (−24.74 to − 0.84) | .036 | 69.8 | .000 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 93/56 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: NR | NR | 64 | NR | High |
| Green tea/placebo | 172/155 | 25–60 | Healthy or high CVD risk | 4 | 3–6 mo | Cochrane | Random | MD: −0.08 mmol/L (−0.24 to 0.07) | .29 | 0 | .41 | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 185/129 | ≥18 | Healthy | 5 | 4–24 wk | Cochrane | Random | WMD: 17.47 mg/dL (−1.40 to 36.34) | NR | 0.0 | .449 | High |
| Green and black tea/placebo | 200/185 | ≥18 | Atrisk of CVD | 6 | 4–24 wk | Cochrane | Random | WMD: −4.80 mg/dL (−19.81 to 10.22) | NR | 0.0 | .531 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 10 | 3–16 wk | Downs and Black’s | Random | MD: 0.10 mmol/L (−0.13 to 0.32) | NR | 80 | <.0001 | Moderate |
| Kim et al. [22] | Green tea/placebo | NR | 11–65 | All (included some adolescents) | 19 | 3–24 wk | ADA Research Design Implementation Checklist | Random | WMD: −3.00 mg/dL (−2.73 to 8.73) | NR | 0 | >.6 | Low |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 13 | NR | Cochrane and Jadad | Random | SMD: −0.13 mmol/L (−0.38 to 0.12) | .30 | 73 | <.0001 | Moderate |
| Liu et al. [30] | Green and black tea/placebo | 245/246 | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: −0.03 mmol/L (−0.42 to 0.36) | .995 | NR | NR | Low |
| Momose et al. [26] | Green tea/placebo | 1339 (total) | 28–60 | Healthy | 17 | 3–14 wk | Jadad | Random | WMD: −1.55 mg/dL (−7.32 to 10.41) | .73 | 95 | <.00001 | Critically low |
| Onakpoya et al. [27] | Green tea/placebo | 1354 (total) | 6–71 | Normotensive or hypertensive | 17 | 3–24 wk | Independently assessed | Random | MD: −0.02 mmol/L (−0.16 to 0.12) | NR | 53 | .79 | Moderate |
| Xu et al. [31] | Green tea/placebo | 3025 (total) | NR | Normal weight, overweight, or obese | 29 | 3 wk to 12 mo | Cochrane | Random | WMD: 3.77 mg/dL (−8.90 to 1.37) | .15 | 56.5 | .0001 | Low |
| Systolic blood pressure | |||||||||||||
| Greyling et al. [20] | Black tea/placebo | 378 (total) | 33–73 | Healthy, hypertensive | 11 | 1–26 wk | Delphi | Random | MD: −1.8 mmHg (−2.80 to − 0.70) | .0013 | 35 | .11 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 60/63 | 25–60 | Healthy or high CVD risk | 2 | 3–6 mo | Cochrane | Fixed | MD: −1.85 mmHg (−3.22 to − 0.48) | .01 | 0 | .49 | High |
| Green tea/placebo | 83/84 | 25–60 | Healthy or high CVD risk | 2 | 3–6 mo | Cochrane | Fixed | MD:−3.18 mmHg (−5.25 to − 1.11) | 0 | 0 | 0.72 | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 104/104 | ≥18 | Healthy | 3 | 4–24 wk | Cochrane | Random | NR | NR | NR | High | |
| Green and black tea/placebo | 127/126 | ≥18 | Atrisk of CVD | 5 | 4–24 wk | Cochrane | Random | WMD: 0.36 mg/dL (−3.04 to 3.75) | NR | 28.7 | .23 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 13 | 3–16 wk | Downs and Black’s | Random | MD: −2.08 mmHg (−3.06 to − 1.05) | NR | 0 | NR | Moderate |
| Li et al. [23] | Green tea/placebo | 971 (total) | 29–54 | Obese or overweight | 14 | 3 wk to 3 mo | Cochrane | Random | MD: −1.42 mmHg (−2.47 to − 0.36) | .008 | 52 | .01 | High |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 9 | NR | Cochrane and Jadad | Random | SMD: −0.16 mmHg (−0.41 to 0.09) | .20 | 64 | .001 | Moderate |
| Liu et al. [30] | Green and black tea/placebo | NR | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: −0.83 mmHg (−1.75 to 0.09) | .0769 | 93 | <.01 | Low |
| Ma et al. [46] | Black tea/placebo | 556/559 | 20–75 | Healthy, elevated blood pressure, or hypertensive | 12 | 1 day to 6 mo | Cochrane | Random | WMD:−1.04 mmHg (−2.05 to − 0.03) | .04 | 71 | .00001 | Moderate |
| Mahdavi-Roshan et al. [25] | Green or black tea/placebo | 203/205 | 52 ± 6 | Hypertensive or elevated blood pressure | 5 | 1–24 wk | Cochrane | Random | WMD: −4.81 mmHg (−8.4 to − 1.58) | .004 | 93.9 | <.001 | Moderate |
| Black tea/placebo | NR | 52 ± 6 | Hypertensive or elevated blood pressure | 3 | 1–24 wk | Cochrane | Random | WMD: −2.67 mmHg (−6.37 to − 1.04) | .158 | 78 | .0003 | ||
| Green tea/placebo | NR | 52 ± 6 | Hypertensive or elevated blood pressure | 2 | 1–24 wk | Cochrane | Random | WMD: −6.22 mmHg (−9.92 to − 2.52) | .001 | 91 | .000 | ||
| Onakpoya et al. [27] | Green tea/placebo | 1342 (total) | 6–71 | Normotensive or hypertensive | 18 | 3–24 wk | Independently assessed | Random | MD:−1.94 mmHg (−2.95 to − 0.93) | .0002 | 8 | .36 | Moderate |
| Yarmolisnky et al. [32] | Green or black tea/placebo | 834 (total) | 16–73 | Prehypertensive/hypertensive | 10 | ≥2 mo | Cochrane | Random | MD: −2.36 mmHg (−4.20 to − 0.52) | NR | 0 | .99 | Moderate |
| Green or black tea/placebo | 834 (total) | 16–73 | Prehypertensive/hypertensive | 10 | ≥2 mo | Cochrane | Fixed | MD: −2.93 mmHg (−5.69 to − 0.17) | NR | NR | NR | ||
| Diastolic blood pressure | |||||||||||||
| Greyling et al. [20] | Black tea/placebo | 378 (total) | 33–73 | Healthy or hypertensive | 11 | 1–26 wk | Delphi | Random | MD: 1.3 mmHg (−1.80 to − 0.80) | .0013 | 20 | .26 | Moderate |
| Hartley et al. [3] | Black tea/placebo | 60/63 | 25–60 | Healthy or high CVD risk | 2 | 3–6 mo | Cochrane | Fixed | MD: −1.27 mmHg (−3.06 to 0.53) | NR | 0 | .53 | High |
| Green tea/placebo | 83/84 | 25–60 | Healthy or high CVD risk | 2 | 3–6 mo | Cochrane | Fixed | MD: −3.42 mmHg (−4.54 to − 2.30) | NR | 0 | .39 | ||
| Igho-Osagie et al. [49] | Green and black tea/placebo | 104/104 | ≥18 | Healthy | 3 | 4–24 wk | Cochrane | Random | NR | NR | NR | High | |
| Green and black tea/placebo | 127/126 | ≥18 | Atrisk of CVD | 5 | 4–24 wk | Cochrane | Random | WMD: 0.18 mmHg (−3.00 to 3.36) | NR | 54.2 | .068 | ||
| Khalesi et al. [11] | Green tea/placebo | 123/117 | 28.9–80 | Healthy, or with hypertension, diabetes, or vascular disease | 13 | 3–16 wk | Downs and Black’s | Random | MD: −1.71 mmHg (−2.86 to − 0.56) | NR | 52 | .02 | Moderate |
| Li et al. [23] | Green tea/placebo | 971 (total) | 29–54 | Obese or overweight | 14 | 3 wk to 3 mo | Cochrane | Random | MD: −1.25 mmHg (−2.32 to − 0.19) | .02 | 74 | <.001 | High |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 9 | NR | Cochrane and Jadad | Random | SMD: −0.16 mmHg (−0.47 to 0.16) | .20 | 77 | <.00001 | Moderate |
| Liu et al. [30] | Green and black tea/placebo | NR | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: −0.89 mmHg (−1.73 to 0.05) | .0388 | 92 | <.01 | Low |
| Ma et al. [46] | Black tea/placebo | 556/559 | 20–75 | Healthy, elevated blood pressure, or hypertensive | 12 | 1-day to 6 mo | Cochrane | Random | WMD:−0.59 mmHg (−1.05 to − 0.13) | .01 | 71 | .00001 | Moderate |
| Mahdavi-Roshan et al. [25] | Green and black tea/placebo | 203/205 | 52 ± 6 | Hypertensive/elevated blood pressure | 5 | 1–24 wk | Cochrane | Random | WMD: −1.98 mmHg (−3.77 to − 0.20) | .029 | 86.3 | <.001 | High |
| Black tea/placebo | NR | 52 ± 6 | Hypertensive/elevated blood pressure | 3 | 1–24 wk | Cochrane | Random | WMD: −1.44 mmHg (−3.89 to 1.02) | .251 | 77 | .004 | ||
| Green tea/placebo | NR | 52 ± 6 | Hypertensive/elevated blood pressure | 2 | 1–24 wk | Cochrane | Random | WMD: −2.36 mmHg (−4.8 to 0.09) | .059 | 85 | .000 | ||
| Onakpoya et al. [27] | Green tea/placebo | 1342 (total) | 6–71 | Normotensive or hypertensive | 18 | 3–24 wk | Independently assessed | Random | MD: −0.98 mmHg (−2.14 to 0.18) | .1 | 62 | NR | Moderate |
| Yarmolisnky et al. [32] | Green or black tea/placebo | 834 (total) | 16–73 | Prehypertensive/hypertensive | 10 | ≥2 mo | Cochrane | Random | MD: −1.77 mmHg (−3.03 to − 0.52) | NR | 0 | .58 | Moderate |
| Green or black tea/placebo | 834 (total) | 16–73 | Prehypertensive/hypertensive | 10 | ≥2 mo | Cochrane | Fixed | MD: −2.40 mmHg (−4.22 to − 0.57) | NR | NR | NR | ||
| Tumour necrosis factor-α | |||||||||||||
| Haghighatdoost et al. [21] | Green tea/placebo | 256 (total) | 17–74.3 | Free of acute inflammatory diseases | 8 | 2–48 wk | Delphi | Random | WMD: −0.5 pg/mL (−0.96 to − 0.03) | .036 | 96.9 | .000 | High |
| C-reactive protein | |||||||||||||
| Haghighatdoost et al. [21] | Green tea/placebo | 887 (total) | 17–74.3 | Free of acute inflammatory diseases | 15 | 2–48 wk | Delphi | Random | WMD: 0.05 mg/L (−0.18 to 0.28) | .692 | 96.8 | .000 | High |
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 6 | NR | Cochrane and Jadad | Random | SMD: −0.21 mg/L (−0.77 to 0.34) | .45 | 85 | NR | Moderate |
| Black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 4 | NR | Cochrane and Jadad | Random | WMD: −0.14 mg/L (−0.68 to 0.41) | .62 | 90 | NR | ||
| Green tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 2 | NR | Cochrane and Jadad | Random | SMD: −0.10 mg/L (−0.10 to 0.91) | .85 | 85 | NR | ||
| Serban et al. [28] | Green tea/placebo | 199/165 | 20–60 | All adults | 11 | 2 wk to 3 mo | Cochrane | Random | WMD: 0.085 mg/L (−0.225 to 0.395) | .592 | NR | NR | Low |
| Green tea/placebo | 199/165 | 20–60 | Healthy | 11 | 2 wk to 3 mo | Cochrane | Random | WMD: −0.028 mg/L (−0.216 to 0.160) | .769 | NR | NR | ||
| Green tea/placebo | 199/165 | 20–60 | Cardiometabolic diseases | 11 | 2 wk to 3 mo | Cochrane | Random | WMD: 0.260 mg/L (−0.815 to 1.334) | .636 | NR | NR | ||
| Interleukin-6 | |||||||||||||
| Haghighatdoost et al. [21] | Green tea/placebo | NR | 17–74.3 | Free of acute inflammatory diseases | 7 | 2–48 wk | Delphi | Random | WMD: 1.38 pg/mL (0.13 to 2.63) | .031 | 96 | <.0001 | High |
| Haemoglobin A1c | |||||||||||||
| Li et al. [24] | Green and black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 3 | NR | Cochrane and Jadad | Fixed | WMD: −0.14% (−0.39 to 0.10) | .26 | 0 | NR | Moderate |
| Black tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 1 | NR | Cochrane and Jadad | Fixed | WMD: −0.37% (−1.04 to 0.30) | .28 | N/A | NR | ||
| Green tea/placebo | 589/446 | NR | Obese adults with BMI ≥ 25 kg/m2 and diagnosed with metabolic syndrome | 1 | NR | Cochrane and Jadad | Fixed | WMD: −0.11% (−0.38 to 0.16) | .43 | 0 | NR | ||
| Liu et al. [30] | Green and black tea/placebo | 46/45 | NR | Metabolic syndrome | 10 | NR | Cochrane | Random | SMD: 0.21% (−0.46 to 0.89) | .552 | 53 | .14 | Low |
| Xu et al. [50] | Green tea/placebo* | NR | NR | All adults | 11 | 3 wk to 12 mo | Jadad | Random | WMD: −0.006% (−0.12 to 0.01) | .07 | 1.7 | .43 | Low |
*Systematic review included studies absent of placebo (i.e. no intervention was the control arm).
ADA: American Dietetic Association; BMI: body mass index; CVD: cardiovascular disease; HDL: high-density lipoprotein; LDL: low-density lipoprotein; MD: mean difference; N/A: XX, NR: not reported; ROB: risk of bias; SMD: standard mean difference; WMD: weighted mean difference.
Data extraction
Standardised data-extraction forms were used to abstract data from included systematic reviews of population-based and clinical studies separately. The following information was extracted independently from each eligible systematic review of population-based studies: the first author, year of publication, study population and age, number of included studies, follow-up time, outcomes, quality assessment tool(s), effects model(s), meta-analysis outcome(s), and heterogeneity. The following information was extracted independently from each eligible systematic review of clinical studies: the first author, year of publication, type of intervention and control, total number of individuals in the intervention and control, study population and age, number of included studies, follow-up time, outcomes, quality assessment tool(s), effects model(s), meta-analysis outcome(s), and heterogeneity. The estimated summary effect with its corresponding 95% confidence interval (95% CI) was extracted from meta-analyses of each included systematic review, when available, as was the I2 statistic.
Evaluation of quality and grading of evidence
The methodological quality of all included systematic reviews was assessed using the AMSTAR (A MeaSurement Tool to Assess systematic Reviews) critical appraisal tool [17]. The AMSTAR 2 tool used in this review is an updated version of AMSTAR that enables more detailed assessment of systematic reviews that include randomised or nonrandomized studies of healthcare interventions. AMSTAR 2 has been shown to be a reliable and valid tool for assessing the quality of systematic reviews [17].
Role of the funding source
No funding was accepted for this study.
Results
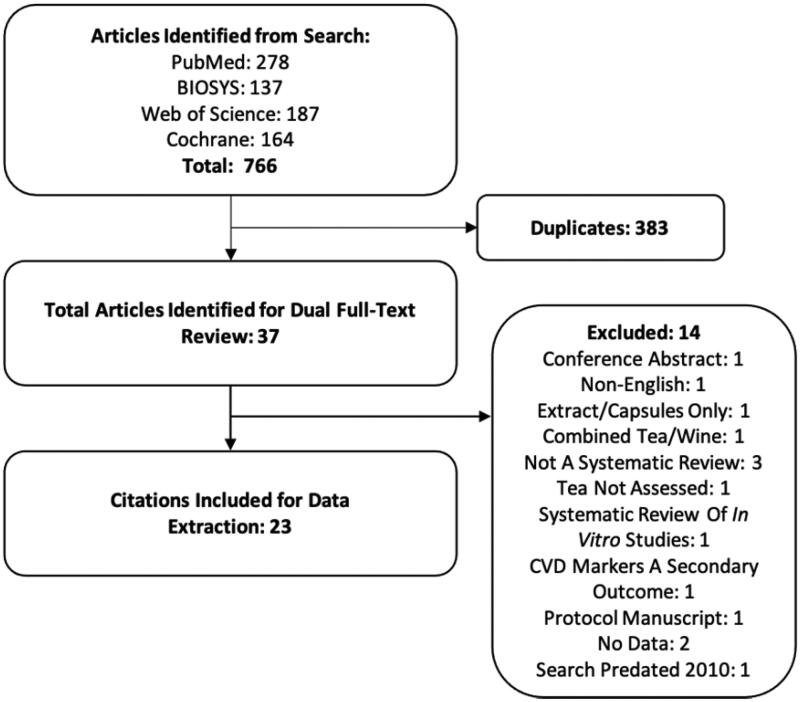
Our literature search strategy identified 766 publications for dual title and abstract review. Of these, 383 were removed as duplicates. Thirty-seven publications were subject to dual full-text screening [2,3,11,18–51]. We excluded 14systematic reviews for the following reasons: one was a conference abstract [35], one was a non-English publication [44], one publication included only extracts or capsules [39], one study combined tea and wine with tea in the analyses [37], three were not systematic reviews [41,42,45], one publication did not assess tea intake [43], one publication was a systematic review of in vitro studies [36], one publication included CVD markers only as a secondary outcome [38], one publication was a protocol manuscript [51], two publications did not contain data [47,48], and one publication search predated 2010 [40]. Twenty-three publications [2,3,11,18–34,46] remained after dual full-text screening and searching the reference lists of included systematic reviews. The results of our systematic search and selection of eligible systematic reviews are shown in Figure 1. The quality of the systematic reviews varied from low to high. AMSTAR 2 strongly recommends that individual ratings not be combined to create an overall score and that the user should consider the potential impact of an inadequate rating for each item [17]. Lack of providing information on funding sources for studies included in each systematic review was the most common weakness detected in the included systematic reviews, followed by providing a list of excluded studies. The authors judged these two items to be noncritical weaknesses, and the quality assessments were rarely affected detrimentally by these items alone. The next common weakness among included systematic reviews was the absence of an explicit statement that the review methods were established prior to the conduct of the review. The authors judged this to be a critical weakness but made an attempt to search independently for registration in the Campbell Collaboration, Cochrane Collaboration, and PROSPERO databases when it was not reported explicitly within the study. Authors commonly reported that study selection or data extraction had been conducted induplicate, but not both. This may represent an error in reporting among systematic reviews and emphasises the need for peer-reviewed journals to better implement standards for reporting of systematic reviews.
Figure 1.
Flow-diagram of study selection process. CVD: cardiovascular disease.
Systematic reviews of population-based studies
A total of three systematic reviews assessed effects of tea intake and CVD outcomes [2,29,33]. The results and AMSTAR2 quality assessment of these included systematic reviews are presented in Table 1.
CVD mortality
A single systematic review and mixed effects dose-response meta-analysis assessing effects of tea consumption on CVD mortality was identified from our literature search [2]. Meta-analysis of 19 studies showed that each cup (236.6 mL) increase in daily black or green tea was associated with a 4% lower risk of CVD mortality (pooled adjusted relative risk [RR]: 0.96; 95%CI: 0.94 to 0.98; p = .0001). Subgroup meta-analysis of four studies showed a greater magnitude of association in elderly individuals aged ≥65years; each cup (236.6 mL) increase in daily black or green tea was associated with a 11% lower risk of CVD mortality (pooled adjusted RR: 0.89; 95%CI: 0.83 to 0.96; p = .001) [2]. The quality of this systematic review was judged to be high (Table 1).
CVD Events
Two systematic reviews assessing effects of tea consumption on CVD events were identified from our literature search [2,33]. A recent systematic review and mixed effects dose-response meta-analysis of population-based studies showed tea consumption to have a significant inverse relationship with CVD events. Meta-analysis of seven studies showed that each cup increase in daily black or green tea was associated with a 2% lower risk of CVD events (pooled adjusted RR: 0.98; 95%CI: 0.96 to 1.00; p = .085) [2]. The quality of this systematic review was judged to be high. Consistent with this systematic review, a separate older systematic review and random effects dose-response meta-analysis of population-based studies showed tea consumption to have a significant relationship with CVD events. Meta-analysis of four studies showed that each 3-cup increase in daily black or green tea was associated with a 27% lower risk of CVD events (pooled adjusted RR: 0.73; 95%CI: 0.53to 0.99; p = .045) [33]. The quality of these systematic reviews was judged to be moderate to high (Table 1).
Stroke events
Three systematic reviews assessing effects of tea consumption on stoke events were identified from our literature search [2,29,33]. A recent systematic review and mixed effects dose-response meta-analysis of population-based studies showed tea consumption to have a significant inverse relationship with stroke events. Meta-analysis of 13 studies showed that each cup increase in daily black or green tea was associated with a 4% lower risk of stroke events (pooled adjusted RR: 0.96; 95%CI: 0.93 to 0.99; p = .002) [2]. The quality of this systematic review was judged to be high. Two older systematic reviews show consistent results. A former systematic review and random effects dose-response meta-analysis of population-based studies by Shen et al. showed tea consumption to have a significant relationship with stroke events. Meta-analysis of five studies showed that each 3-cup increase in daily black or green tea was associated with a 17% lower risk of CVDevents (pooled adjusted RR: 0.83; 95%CI: 0.72 to 0.96; p < .01) [29]. The quality of this systematic review was judged to be critically low. Another systematic review and random effects dose-response meta-analysis of population-based studies by Zhang et al. showed tea consumption to have a significant relationship with stroke events. Meta-analysis of two studies showed black or green tea to be associated with a 18% lower risk of CVD events (pooled adjusted RR: 0.82; 95% CI: 0.73 to 0.92; p = .001) [33]. The quality of this systematic review was judged to be moderate (Table 1).
Systematic reviews of randomized controlled trials
Total cholesterol
Eleven systematic reviews assessing effects of tea consumption on total cholesterol were identified from our literature search [3,11,18,19,22,24,27,30,31,34,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type-2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. One study included some adolescents [22]. Li et al. found a significant decrease in total cholesterol among obese individuals with a body mass index (BMI) ≥25 kg/m2 diagnosed with metabolic syndrome who consumed green and black tea (combined) vs. placebo (standard mean difference [SMD]: 0.24 mmol/L; 95% CI: −0.47 to 0.00; p = .05) in a random effects meta-analysis [24]. No effects were reported for green tea vs. placebo or black tea vs. placebo [24]. Xu et al. found a significant decrease in total cholesterol among normal weight, overweight, and obese individuals (combined) who consumed green tea vs. placebo (weighted mean difference [WMD]: −4.66 mg/dL; 95% CI: 6.36 to −2.96; p = .0001) in a random effects meta-analysis [31]. The remaining nine older systematic reviews found no significant effects on total cholesterol across various populations [3,11,18,19,22,27,30,34,49], which may be due to a smaller number of studies and overall sample size. The quality of these systematic reviews was judged to be low to high (Table 2).
Low-density lipoprotein cholesterol
Twelve systematic reviews assessing effects of tea consumption on low-density lipoprotein (LDL) cholesterol were identified from our literature search [3,11,18,19,22,24,26,27,30,31,34,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type-2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. One study included some adolescents [22]. Li et al. found a significant decrease in LDL cholesterol among obese individuals (BMI ≥25 kg/m2) diagnosed with metabolic syndrome who consumed green and black tea (combined) vs. placebo (SMD: −0.31 mmol/L; 95% CI: −0.55 to −0.06; p = not reported [NR]) and green tea vs. placebo (SMD: −0.30 mmol/L; 95% CI: −0.52 to −0.08; p = NR) in a random effects meta-analysis [24]. No effects were reported for black tea vs. placebo [24]. Liu et al. found a significant decrease in LDL cholesterol among individuals with metabolic syndrome who consumed green and black tea (combined) vs. placebo in a random effects meta-analysis (SMD: −0.63 mmol/L; 95% CI: −1.06 to −0.20; p = .0057) [30]. Xu et al. found a significant decrease in LDL cholesterol among normal weight, overweight, and obese individuals (combined) who consumed green tea vs. placebo (WMD: −4.55 mg/dL; 95% CI: −6.31 to −2.80 mg/dL; p = .0001) in a random effects meta-analysis [31]. Momose et al. found a significant decrease in LDL cholesterol among healthy individuals who consumed green tea vs. placebo (WMD: −7.38 mg/dL; 95% CI: −9.25 to −5.50; p < .00001) in a random effects meta-analysis [26]. Zhao et al. found a significant decrease in LDL cholesterol among healthy, hypercholesterolemic, and prediabetic individuals who consumed black tea vs. placebo (mean difference [MD]: −4.64 mg/dL; 95% CI: −8.99 to −0.30; p = .036) in a random effects meta-analysis [34]. Khalesi et al. found a significant decrease in LDL cholesterol among healthy, hypertensive, and diabetic individuals, and those with vascular disease who consumed green tea vs. placebo (MD: −0.16 mmol/L; 95% CI: −0.22 to −0.09; p = NR) in a random effects meta-analysis [11]. Hartley et al. conducted a Cochrane review and found a significant decrease in LDL cholesterol among healthy and high-risk individuals who consumed black tea vs. placebo (MD: −0.43 mmol/L; 95% CI: −0.56 to −0.31; p = NR) and green tea vs. placebo (MD: −0.64 mmol/L; 95% CI: −0.77 to −0.52; p = NR) in a random effects meta-analysis [3]. Kim et al. found a significant decrease in LDL cholesterol among individuals of various health status who consumed green tea vs. placebo (WMD: −5.30 mg/dL; 95% CI: −9.99 to −0.62; p = NR) in a random effects meta-analysis [22]. The remaining four older systematic reviews found no significant effects on LDL cholesterol across various populations [18,19,27,49], which may be due to a smaller number of studies and overall sample size. The quality of these systematic reviews was judged to be critically low to high (Table 2).
High-density lipoprotein cholesterol
Twelve systematic reviews assessing effects of tea consumption on high-density lipoprotein (HDL) cholesterol were identified from our literature search [3,11,18,19,22,24,26,27,30,31,34,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type-2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. One study included some adolescents [22]. These systematic reviews consistently failed to show significant effects on HDL cholesterol across various populations [3,11,18,19,22,24,26,27,30,31,34,49]. The quality of these systematic reviews was judged to be critically low to high (Table 2).
Triglycerides
Eleven systematic reviews assessing effects of tea consumption on triglycerides were identified from our literature search [3,11,18,19,22,24,26,27,30,31,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type 2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. One study included some adolescents [22]. Asbaghi et al. (2020) found a significant decrease in triglycerides among individuals with type 2 diabetes who consumed green tea vs. placebo (WMD: −12.79 mg/dL; 95% CI: −24.74 to −0.84; p = .036) in a random effects meta-analysis [19]. The remaining 10 systematic reviews found no significant effects on triglycerides across various populations [3,11,18,22,24,26,27,30,31,49]. The quality of these systematic reviews was judged to be critically low to high (Table 2). Inconsistency may be due to differences in health status of participants. The systematic reviews also had an overall small sample size and differences in the how participants (e.g. healthy, at-risk, and diseased) were grouped in the analyses.
Systolic blood pressure
Eleven systematic reviews assessing effects of tea consumption on systolic blood pressure (SBP) were identified from our literature search [3,11,20,23–25,27,30,32,46,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type-2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. Ma et al. found a significant decrease in SBP among individuals with hypertension or elevated blood pressure who consumed black tea vs. placebo (WMD: −1.04 mmHg; 95% CI: −2.05 to −0.03; p = .04) [46]. Mahdavi-Roshan et al. (2020) found a significant decrease in SBP among individuals with hypertension or individuals with elevated blood pressure who consumed green or black tea vs. placebo (WMD: −4.81 mmHg; 95% CI: −8.4 to −1.58; p = .004), black tea vs. placebo (WMD: −2.67 mmHg; 95% CI: −6.37 to −1.04; p = .158), and green tea vs. placebo (WMD: −6.22 mmHg; 95% CI: −9.92 to −2.52; p = .001) in a random effects meta-analysis [25]. Li et al. found a significant decrease in SBP among obese or overweight individuals who consumed green tea vs. placebo (MD: −1.42 mmHg; 95% CI: −2.47 to −0.36; p = .008) in a random effects meta-analysis [23]. Yarmolisnky et al. found a significant decrease in SBP among prehypertensive and hypertensive individuals who consumed green or black tea vs. placebo in a random effects (MD: −2.36 mmHg; 95% CI: −4.20 to −0.52; p = NR) and fixed effects meta-analysis (MD: −2.93 mmHg; 95% CI: −5.69 to −0.17; p = NR) [32]. Greyling et al. (2014) found a significant decrease in SBP among healthy and hypertensive individuals who consumed green or black tea vs. placebo (MD: −1.8 mmHg; 95% CI: −2.80 to −0.70; p = .0013) in a random effects meta-analysis [20]. Khalesi et al. found a significant decrease in SBP among healthy individuals and those with hypertension, diabetes, and vascular disease who consumed green tea vs. placebo (MD: −2.08 mmHg; 95% CI: −3.06 to −1.05; p = NR) in a random effects meta-analysis [11]. Onakpoya et al. found a significant decrease in SBP among normotensive or hypertensive individuals who consumed green tea vs. placebo (MD: −1.94 mmHg; 95% CI: −2.95 to −0.93; p = NR) in a random effects meta-analysis [27]. Hartley et al. conducted a Cochrane review and found a significant decrease in SBP among healthy and high-risk individuals who consumed black tea vs. placebo in (MD: −1.85 mmHg; 95% CI: −3.22 to −0.48; p = .01) and green tea vs. placebo (MD: −3.18 mmHg; 95% CI: −5.25 to −1.11; p = .00) in a fixed effects meta-analysis [3]. The remaining three older systematic reviews found no significant effects on SBP across various populations [24,30,49], which may be due to a smaller number of studies and overall sample size. The quality of these systematic reviews was judged to be low to high (Table 2).
Diastolic blood pressure
Eleven systematic reviews assessing effects of tea consumption on diastolic blood pressure (DBP) were identified from our literature search [3,11,20,23–25,27,30,32,46,49]. Study populations ranged from healthy individuals and the general adult population to individuals with high CVD risk, hypercholesterolaemia, type-2 diabetes, prediabetes, obesity with metabolic syndrome, or hypertension. Ma et al. found a significant decrease in DBP among individuals with hypertension or elevated blood pressure who consumed black tea vs. placebo (WMD: −0.59 mmHg; 95% CI: −1.05 to −0.13; p = .01) [46]. Mahdavi-Roshan et al. (2020) found a significant decrease in DBP among individuals with hypertension or elevated blood pressure who consumed green or black tea vs. placebo (WMD: −1.98 mmHg; 95% CI: −3.77 to − 0.20; p = .029), but not black tea vs. placebo or green tea vs. placebo, in a random effects meta-analysis [25]. Li et al. found a significant decrease in DBP among obese or overweight individuals who consumed green tea vs. placebo (MD: −1.25 mmHg; 95% CI: −2.32 to −0.19; p = .02) in a random effects meta-analysis [23]. Yarmolisnky et al. (2015) found a significant decrease in DBP among prehypertensive and hypertensive individuals who consumed green or black tea vs. placebo in a random effects (MD: −1.77 mmHg; 95% CI: −3.03 to −0.52; p = NR) and fixed effects meta-analysis (MD: −2.40 mmHg; 95% CI: −4.22 to −0.57; p = NR) [32]. Greyling et al. found a significant decrease in DBP among healthy and hypertensive individuals who consumed green or black tea vs. placebo (MD: −1.3 mmHg; 95% CI: −1.80 to −0.80; p = .0013) in a random effects meta-analysis [20]. Khalesi et al. found a significant decrease in DBP among healthy individuals and in those with hypertension, diabetes, and vascular disease who consumed green tea vs. placebo (MD: −1.71 mmHg; 95% CI: −2.86 to −0.56; p = NR) in a random effects meta-analysis [11]. Hartley et al. conducted a Cochrane review and found a significant decrease in DBP among healthy and high-risk individuals who consumed green tea vs. placebo (MD: −3.42 mmHg; 95% CI: −4.54 to −2.30; p = NR), but not black tea vs. placebo, in a fixed effects meta-analysis [3]. The remaining three older systematic reviews found no significant effects on DBP across various populations [24,27,30,49] which may be due to a smaller number of studies and overall sample size.The quality of these systematic reviews was judged to be low to high (Table 2).
Tumour necrosis factor-α
One systematic review assessing effects of tea consumption on tumour necrosis factor-α (TNF-α) was identified from our literature search [21]. Haghighatdoost et al. found a significant decrease in TNF-α among individuals free of acute inflammatory diseases who consumed green tea vs. placebo (WMD: −0.5 pg/mL; 95% CI: −0.96 to −0.03; p = .036) [21]. The quality of this systematic review was judged to be high (Table 2).
C-reactive protein
Three systematic reviews assessing effects of tea consumption on C-reactive protein (CRP) were identified from our literature search [21,24,28]. Study populations ranged from healthy individuals to those with obesity with metabolic syndrome or cardiometabolic diseases. None of the three systematic reviews found significant effects on CRP across various populations. The quality of these systematic reviews was judged to be low to high (Table 2).
Interleukin-6
One systematic review assessing effects of tea consumption on interleukin-6 (IL-6) was identified from our literature search [21]. Haghighatdoost et al. found a significant increase in IL-6 among individuals free of acute inflammatory diseases who consumed green tea vs. placebo (WMD: −1.38 pg/mL; 95% CI: 0.13 to 2.63; p = .031) [21]. The quality of this systematic review was judged to be high (Table 2).
Haemoglobin A1c
Three systematic reviews assessing effects of tea consumption on haemoglobin A1c (HbA1c) were identified from our literature search [24,30,50]. Study populations ranged from individualswith metabolic syndrome to those who were obese with metabolic syndrome. None of the systematic reviews found significant effects on HbA1c across various populations [24,30,50]. The quality of these systematic reviews was judged to be low to moderate (Table 2).
Discussion
In this umbrella review, we describe results from 23 systematic reviews that investigated the role of tea in reducing CVD risk. Based on the scientific literature presented, it is reasonable to judge that 2cups of unsweet tea per day has the potential to decrease CVD risk and progression due to its flavonoid content. Aside from the included systematic reviews, it is important to note that a recent two-sample Mendelian randomisation analysis provided evidence that a genetically predicted extra daily cup of tea is associated with a reduced risk of small vessel stroke (odds ratio: 0.79; 95% CI: 0.69 to 0.91; p = .0001) [52], lending greater biological plausibility to our findings. Tea flavonoids seem to decrease LDL cholesterol, SBP, and DBP across both healthy and at-risk populations, although larger study sample sizes and consistency limit these findings. Beneficial effects seem to be most distinct when healthy and at-risk populations are analysed together, alluding to the sample size issues noted above and by Igho-Osagie et al. [49]. It is possible that the sample sizes present in most intervention studies were insufficient to show modest effects on biomarkers such as blood pressure and lipids. Differences in tea consumed as a beverage vs. supplement also seem to exist, as demonstrated when comparing the systematic reviews from Igho-Osagie et al. [49] and Hartley et al. [3]. Igho-Osagie et al. [49] did not include studies in which tea extracts or supplements were administered as the intervention. Adherence issues are likely to be more apparent across whole food or beverage versus supplemental interventions. Adding to this conundrum, the systematic reviews reviewed in this umbrella review failed to provide sufficient information on the variation in chemical composition of tea beverages, supplements, and/or extracts used among included intervention studies.
Other mechanisms may also be responsible for the effects seen on CVD incidence, and outcomes seen across observational studies. Tea flavonoids have been thought to improve blood flow by enhancing endothelial nitric oxide bioavailability [4]. During the past two decades, flow-mediated dilation (FMD) has been used increasingly as a tool to assess effects of interventions on endothelial function in humans. Several (but not all) prospective studies indicate inverse relationships between FMD and CVD risk in healthy and diseased individuals [10–12,14–19]. An earlier systematic review of randomised controlled trials predating our literature search found that a mean daily dose of 500 mL of tea (about 2cups) increased FMD by about 2.6% arterial diameter (95% CI: 1.9to3.3%; p < .001; n = 9) compared to placebo [4]. An updated systematic review in this area is needed. Tea flavonoids seem to exert beneficial effects on some but not all markers of inflammation; however, larger controlled intervention studies are needed to fully elucidate these effects.
Since tea consumption is widespread and associated with multiple health attributes, it is also important to consider potential toxicological effects. Nervousness, anxiety, heart irregularities, headaches, tremors, hypotension, restlessness, insomnia, irritation of the gastrointestinal mucosa, diuresis, and daytime irritability are some potential side effects of tea consumption [53,54]. Most of these effects were shown when tea was consumed during a fasted state. The primary side effects documented in human studies are hepatotoxicity and gastrointestinal disturbances (i.e. vomiting and diarrhoea) after high-dose supplemental intake [54]. A 2018 systematic review assessed adverse events among 159 human intervention studies and found catechin-rich green tea preparations to result in hepatic adverse events in a dose-dependent manner when ingested in large amounts via supplements but not when consumed as brewed tea, extracts in beverages, or as part of food [12]. Toxicological evidence from laboratory studies suggests that hepatotoxic effects are strongly associated with certain dosing conditions (e.g. bolus dose via gavage, fasting) and positively correlated with total catechin and epigallocatechin gallate (EGCG) content. This systematic review concluded that an observed safe level of 704 mg of EGCG per day might be considered for green tea preparations in beverage form based on human adverse event data [12]. According to the USDA Flavonoid Database [13], brewed green tea contains an average of 126.6 mg of total catechins and 77.8 mg of EGCG per 100 mL as consumed, on the basis of 1 g of leaf/100 mL of infusion. It should be noted that the larger amount of flavonoids present in tea extracts or supplements may exhibit a variety of drug–nutrient interactions that are likely not apparent through beverage tea intake [55]. There are limited data in pregnant and lactating women and among other susceptible subpopulations. Consumption of tea as a beverage in humans at physiologically reasonable levels appears to be safe.
Our umbrella review has several strengths and limitations. Quality assessment of the included systematic reviews by AMSTAR 2 is a major strength. Our umbrella review is limited due to the reliance on previously published systematic reviews, leaving the opportunity that missed studies may have an influence on our findings. To circumvent this dilemma, we included all (not just the most recent) systematic reviews within the past 10 years and made judgements based on the consistency of evidence over time. There is known overlap between studies included amongst similar systematic reviews; however, consistency of the results reported by different researchers analysing similar data reduces the chance of confirmation bias. As previously stated, the small sample sizes present in many meta-analyses within included systematic reviews may also be a limiting factor for detecting more modest effects of tea. Additional large, randomised intervention studies of both healthy and at-risk populations assessing the effects of beverage tea intake on CVD outcomes and biomarkers can help increase the evidence supporting our reported effects.
Conclusion
A consistent intake of tea at levels around 2cups per day seems to have the potential to decrease CVD risk and progression due to its flavonoid content. This is supported by the consistency between a recent high-quality systematic review and dose-response meta-analyses of population-based studies demonstrating beneficial effects of consumption on CVD mortality, CVD events and stroke events and medium- to high-quality systematic reviews of intervention studies that further elucidate potential benefits on both validated (i.e., SBP, DBP, total cholesterol, and LDL-cholesterol) and emerging risk biomarkers of CVD (TNF-ɑ and IL-6). On the basis of this umbrella review, the consumption of tea as a beverage did not seem to be harmful to health; therefore, the benefits of moderate consumption likely outweigh risk. Future large, clinical intervention studies are needed to provide additional mechanistic insight (e.g., effects on FMD) to confirm the outcome effects shown across observational studies.
Funding Statement
No funding was accepted for this umbrella review.
Disclosure statement
No potential conflict of interest reported by AK. TCW has received prior research funding within the last 3-years from Unilever.
References
- 1.Haufe TC, Ho KKHY, Ferruzzi MG, et al. Potential health effects of tea. Nutr Today. 2018;53(5):213–228. [Google Scholar]
- 2.Chung M, Zhao N, Wang D, et al. Dose–response relation between tea consumption and risk of cardiovascular disease and all-cause mortality: a systematic review and meta-analysis of population-based studies. Adv Nutr. 2020;11(4):790–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hartley L, Flowers N, Holmes J, et al. Green and black tea for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;2013(6):Cd009934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ras RT, Zock PL, Draijer R.. Tea consumption enhances endothelial-dependent vasodilation; a meta-analysis. PLoS One. 2011;6(3):e16974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang H, Dwyer-Lindgren L, Lofgren KT, et al. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2071–2094. [DOI] [PubMed] [Google Scholar]
- 7.Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services 2020 . Available from: https://www.dietaryguidelines.gov/2020-advisory-committee-report.
- 8.McKay DL, Blumberg JB.. The role of tea in human health: an update. J Am Coll Nutr. 2002;21(1):1–13. [DOI] [PubMed] [Google Scholar]
- 9.Song WO, Chun OK.. Tea is the major source of flavan-3-ol and flavonol in the US diet. J Nutr. 2008;138(8):1543S–1547S. [DOI] [PubMed] [Google Scholar]
- 10.Schreuder THA, Eijsvogels TMH, Greyling A, et al. Effect of black tea consumption on brachial artery flow-mediated dilation and ischaemia–reperfusion in humans. Appl Physiol Nutr Metab. 2014;39(2):145–151. [DOI] [PubMed] [Google Scholar]
- 11.Khalesi S, Sun J, Buys N, et al. Green tea catechins and blood pressure: a systematic review and meta-analysis of randomised controlled trials. Eur J Nutr. 2014;53(6):1299–1311. [DOI] [PubMed] [Google Scholar]
- 12.Hu J, Webster D, Cao J, et al. The safety of green tea and green tea extract consumption in adults–results of a systematic review. Regul Toxicol Pharmacol. 2018;95:412–433. [DOI] [PubMed] [Google Scholar]
- 13.US Department of Agriculture . USDA ARS Food Composition Databases 2019. Available from: https://ndb.nal.usda.gov.
- 14.Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ. 2009;181(8):488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aromataris E, Fernandez R, Godfrey CM, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement. 2015;13(3):132–140. [DOI] [PubMed] [Google Scholar]
- 16.Aromataris E, Fernandez R, Godfrey C, et al. Chapter 10: umbrella reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. Adelaide, Australia: JBI; 2020. [Google Scholar]
- 17.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Araya-Quintanilla F, Gutiérrez-Espinoza H, Moyano–Gálvez V, et al. Effectiveness of black tea versus placebo in subjects with hypercholesterolemia: a PRISMA systematic review and meta-analysis. Diabetes Metab Syndr. 2019;13(3):2250–2258. [DOI] [PubMed] [Google Scholar]
- 19.Asbaghi O, Fouladvand F, Moradi S, et al. Effect of green tea extract on lipid profile in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab Syndr. 2020;14(4):293–301. [DOI] [PubMed] [Google Scholar]
- 20.Greyling A, Ras RT, Zock PL, et al. The effect of black tea on blood pressure: a systematic review with meta-analysis of randomized controlled trials. PLoS One. 2014;9(7):e103247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haghighatdoost F, Hariri M.. The effect of green tea on inflammatory mediators: a systematic review and meta‐analysis of randomized clinical trials. Phytother Res. 2019;33(9):2274–2287. [DOI] [PubMed] [Google Scholar]
- 22.Kim A, Chiu A, Barone MK, et al. Green tea catechins decrease total and low-density lipoprotein cholesterol: a systematic review and meta-analysis. J Am Diet Assoc. 2011;111(11):1720–1729. [DOI] [PubMed] [Google Scholar]
- 23.Li G, Zhang Y, Thabane L, et al. Effect of green tea supplementation on blood pressure among overweight and obese adults: a systematic review and meta-analysis. J Hypertens. 2015;33(2):243–254. [DOI] [PubMed] [Google Scholar]
- 24.Li X, Wang W, Hou L, et al. Does tea extract supplementation benefit metabolic syndrome and obesity? A systematic review and meta-analysis. Clin Nutr. 2020;39(4):1049–1058. [DOI] [PubMed] [Google Scholar]
- 25.Mahdavi-Roshan M, Salari A, Ghorbani Z, et al. The effects of regular consumption of green or black tea beverage on blood pressure in those with elevated blood pressure or hypertension: a systematic review and meta-analysis. Complement Ther Med. 2020; 51:102430. [DOI] [PubMed] [Google Scholar]
- 26.Momose Y, Maeda-Yamamoto M, Nabetani H.. Systematic review of green tea epigallocatechin gallate in reducing low-density lipoprotein cholesterol levels of humans. Int J Food Sci Nutr. 2016;67(6):606–613. [DOI] [PubMed] [Google Scholar]
- 27.Onakpoya I, Spencer E, Heneghan C, et al. The effect of green tea on blood pressure and lipid profile: a systematic review and meta-analysis of randomized clinical trials. Nutr Metab Cardiovasc Dis. 2014;24(8):823–836. [DOI] [PubMed] [Google Scholar]
- 28.Serban C, Sahebkar A, Antal D, et al. Effects of supplementation with green tea catechins on plasma C-reactive protein concentrations: a systematic review and meta-analysis of randomized controlled trials. Nutrition. 2015;31(9):1061–1071. [DOI] [PubMed] [Google Scholar]
- 29.Shen L, Song L-g, Ma H, et al. Tea consumption and risk of stroke: a dose-response meta-analysis of prospective studies. J Zhejiang Univ Sci B. 2012;13(8):652–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu W, Wan C, Huang Y, et al. Effects of tea consumption on metabolic syndrome: a systematic review and meta‐analysis of randomized clinical trials. Phytother Res. 2020;34(11):2857–2866. [DOI] [PubMed] [Google Scholar]
- 31.Xu R, Yang K, Li S, et al. Effect of green tea consumption on blood lipids: a systematic review and meta-analysis of randomized controlled trials. Nutr J. 2020;19(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yarmolinsky J, Gon G, Edwards P.. Effect of tea on blood pressure for secondary prevention of cardiovascular disease: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2015;73(4):236–246. [DOI] [PubMed] [Google Scholar]
- 33.Zhang C, Qin Y-Y, Wei X, et al. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol. 2015;30(2):103–113. [DOI] [PubMed] [Google Scholar]
- 34.Zhao Y, Asimi S, Wu K, et al. Black tea consumption and serum cholesterol concentration: systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2015;34(4):612–619. [DOI] [PubMed] [Google Scholar]
- 35.Shulkin ML, Micha R, Rao M, et al. Abstract P279: major dietary risk factors for cardiometabolic disease: current evidence for causal effects and effect sizes from the global burden of diseases (GBD) 2015 study. Circulation. 2016;133(suppl 1):AP279. [Google Scholar]
- 36.Sánchez M, González-Burgos E, Iglesias I, et al. The pharmacological activity of Camellia sinensis (L.) Kuntze on metabolic and endocrine disorders: a systematic review. Biomolecules. 2020;10(4):603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peluso I, Miglio C, Morabito G, et al. Flavonoids and immune function in human: a systematic review. Crit Rev Food Sci Nutr. 2015;55(3):383–395. [DOI] [PubMed] [Google Scholar]
- 38.Payab M, Hasani‐Ranjbar S, Shahbal N, et al. Effect of the herbal medicines in obesity and metabolic syndrome: a systematic review and meta‐analysis of clinical trials. Phytother Res. 2020;34(3):526–545. [DOI] [PubMed] [Google Scholar]
- 39.Lau SO, Georgousopoulou EN, Kellett J, et al. The effect of dietary supplementation of green tea catechins on cardiovascular disease risk markers in humans: a systematic review of clinical trials. Beverages. 2016;2(2):16. [Google Scholar]
- 40.Huang J, Frohlich J, Ignaszewski AP.. The impact of dietary changes and dietary supplements on lipid profile. Can J Cardiol. 2011;27(4):488–505. [DOI] [PubMed] [Google Scholar]
- 41.Eng QY, Thanikachalam PV, Ramamurthy S.. Molecular understanding of epigallocatechin gallate (EGCG) in cardiovascular and metabolic diseases. J Ethnopharmacol. 2018;210:296–310. [DOI] [PubMed] [Google Scholar]
- 42.Deng C, Lu Q, Gong B, et al. Stroke and food groups: an overview of systematic reviews and meta-analyses. Public Health Nutr. 2018;21(4):766–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Del Bo C, Bernardi S, Marino M, et al. Systematic review on polyphenol intake and health outcomes: is there sufficient evidence to define a health-promoting polyphenol-rich dietary pattern? Nutrients. 2019;11(6):1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baladia E, Basulto J, Manera M, et al. Effect of green tea or green tea extract consumption on body weight and body composition; systematic review and meta-analysis. Nutr Hosp. 2014;29(3):479–490. [DOI] [PubMed] [Google Scholar]
- 45.Amiot MJ, Riva C, Vinet A.. Effects of dietary polyphenols on metabolic syndrome features in humans: a systematic review. Obes Rev. 2016;17(7):573–586. [DOI] [PubMed] [Google Scholar]
- 46.Ma C, Zheng X, Yang Y, et al. The effect of black tea supplementation on blood pressure: a systematic review and dose-response meta-analysis of randomized controlled trials. Food Funct. 2021;12(1):41–56. [DOI] [PubMed] [Google Scholar]
- 47.Luvián-Morales J, Varela-Castillo FO, Flores-Cisneros L, et al. Functional foods modulating inflammation and metabolism in chronic diseases: a systematic review. Crit Rev Food Sci Nutr. 2021;:1–22. [DOI] [PubMed] [Google Scholar]
- 48.Medina-Vera I, Gómez-de-Regil L, Gutiérrez-Solis AL, et al. Dietary strategies by foods with antioxidant effect on nutritional management of dyslipidemias: a systematic review. Antioxidants. 2021;10(2):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Igho-Osagie E, Cara K, Wang D, et al. Short-term tea consumption is not associated with a reduction in blood lipids or pressure: a systematic review and meta-analysis of randomized controlled trials. J Nutr. 2020;150(12):3269–3279. [DOI] [PubMed] [Google Scholar]
- 50.Xu R, Bai Y, Yang K, et al. Effects of green tea consumption on glycemic control: a systematic review and meta-analysis of randomized controlled trials. Nutr Metab (Lond)). 2020;17(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morze J, Osadnik T, Osadnik K, et al. Comparative effect of nutraceuticals on lipid profile: a protocol for systematic review and network meta-analysis. BMJ Open. 2020;10(8):e032755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang M, Bai Y, Wang Z, et al. Higher tea consumption is associated with decreased risk of small vessel stroke. Clin Nutr. 2021;40(3):1430–1435. [DOI] [PubMed] [Google Scholar]
- 53.American Botanical Council . The ABC clinical guide to herbs. Austin, TX: American Botanical Council; 2003. [Google Scholar]
- 54.Bedrood Z, Rameshrad M, Hosseinzadeh H.. Toxicological effects of Camellia sinensis (green tea): a review. Phytother Res. 2018;32(7):1163–1180. [DOI] [PubMed] [Google Scholar]
- 55.Srinivas NR. Recent trends in preclinical drug-drug interaction studies of flavonoids–review of case studies, issues and perspectives. Phytother Res. 2015;29(11):1679–1691. [DOI] [PubMed] [Google Scholar]