Abstract
Objectives:
The aim of this systematic review was to evaluate the effect of piezocision as an adjunctive procedure to accelerate orthodontic tooth movement.
Materials and Methods:
Randomized controlled trials and controlled clinical trials that investigated the effectiveness of piezocision on accelerating orthodontic tooth movement were identified through electronic and manual searches. The literature search, study inclusion, risk of bias assessment, and data extraction were performed by two reviewers independently.
Results:
Four eligible studies were included in this review. All studies reported accelerated tooth movement after piezocision, and three reported a significant reduction of treatment duration in the piezocision group. No deleterious effects on periodontal status, pain perception, satisfaction, root resorption, or anchorage control were reported in any studies.
Conclusion:
Based on currently available information, weak evidence supports that piezocision is a safe adjunct to accelerate orthodontic tooth movement, at least in the short term. More high-quality clinical trials to determine the long-term effects and optimal protocol for piezocision are needed to draw more reliable conclusions.
Keywords: Corticotomy, Piezocision, Orthodontics, Tooth movement
INTRODUCTION
The demand for comprehensive orthodontic treatment has grown rapidly in recent years. The mean duration of orthodontic treatment is approximately 24 months, which could be even longer depending on case severity, treatment plan, and individual characteristics.1 Prolonged treatment could increase the risk of numerous complications including caries, periodontal diseases, and root resorption.2,3 Thus, accelerating orthodontic tooth movement (OTM) and the resultant shortening of treatment duration is always one of the primary goals for orthodontists.
As early as the 1950s, Köle4 introduced surgery involving elevation of a full-thickness flap and removal of interdental alveolar cortical bone. This technique has been claimed to allow movement of bone blocks rather than moving single teeth individually, thus being more efficient and inducing less root resorption and retention time.4 Subsequently, the efficacy of corticotomy on promoting OTM was further validated in a series of clinical reports.5,6 Recent studies indicated that corticotomy-induced acceleration of OTM was associated with a regional acceleratory phenomenon (RAP), which is characterized by transient localized demineralized bone and exacerbated bone turnover in injured regions.7,8 However, the acceptance of corticotomy-assisted orthodontics among patients is low, mainly because of the invasive procedures and postoperative discomfort and complications.9
Recently, a minimally invasive surgery has been introduced as an alternative to conventional corticotomy.10 The scalpel and mallet were employed to pass through the gingiva and create a wound in the cortical alveolar bone, thus initiating RAP and the consequent acceleration of OTM.10 Thereafter, this procedure was optimized by using piezoelectric devices rather than scalpels and mallets and termed piezocision.11
With the merit of minimal invasiveness, piezocision is more promising for clinical application than conventional corticotomy and has been investigated extensively. A recent animal study revealed that piezocision could elicit alveolar bone demineralization and osteoclast recruitment, thus facilitating tooth movement in a rat model.12 Moreover, several clinical reports have determined the effectiveness of piezocision in accelerating OTM.13–17 However, the methodological heterogeneity and inconclusive results of these studies could bias the evidence and mislead clinical practice. Therefore, a critical systematic review addressing this topic would be beneficial to clinicians. The aim of the present study was to review and summarize systematically the evidence regarding the effectiveness of piezocision on accelerating OTM.
MATERIALS AND METHODS
This systematic review was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).18 The literature search, study inclusion, methodology quality assessment, and data extraction were carried out in duplicate by two review authors. Any discrepancy was discussed with a third reviewer for consensus.
Search Strategy
Electronic bibliographic sources including PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, China National Knowledge Infrastructure (CNKI), and System for Information on Grey Literature in Europe (SIGLE) were searched until October 2016. The search strategy was a combination of Medical Subject Headings (Mesh) and free-text words for PubMed and was optimized for each database, respectively. The details of the search strategy are summarized in Table 1. In addition, relevant journals and reference sections of retrieved studies were manually searched. There was no language restriction.
Table 1.
Search Strategies for Each Database
| Step |
PubMed |
Embase, CENTRAL,CNKI & SIGLE |
| 1 | Piezosurgery [Mesh] OR piezoelectric OR piezocision OR piezo* | Piezosurgery OR piezoelectric OR piezocision OR piezo* |
| 2 | Orthodontics [Mesh] OR orthodont* | Orthodontics OR orthodont* |
| 3 | Tooth movement [Mesh] OR move* OR retract* | Tooth movement OR move* OR retract* |
| 4 | 1 AND 2 AND 3 | 1 AND 2 AND 3 |
Inclusion Criteria
The trials that met the following criteria were included: (1) the study was a prospective randomized controlled trial (RCT) or a controlled clinical trial (CCT), (2) the participants were healthy and required comprehensive orthodontic treatment, (3) the study investigated the efficacy of piezocision on accelerating OTM, and (4) the outcomes included rate of tooth movement, accumulative moved distance, or required treatment time.
Data Extraction
After study inclusion, a customized form was used for data extraction from reserved records. Relevant information including study designs, sample characteristics, details of surgical procedures and orthodontic treatment, outcome measures, follow-up duration, and results were extracted by two reviewers independently.
The primary outcome of this review was any indicator of tooth movement velocity. The secondary outcome included potential complications such as root resorption and discomfort and the impact on patients' quality of life.
Risk of Bias Assessment
The risk of bias of recruited studies was determined using the Cochrane Collaboration's tool for assessing risk of bias. Seven domains of bias were evaluated: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other bias.19 Each domain was judged as high, unclear, or low risk of bias by two reviewers independently. The primary study was categorized as low risk if all seven domains were assessed as low risk of bias, as unclear risk if any domain was assessed as unclear risk of bias, and as high risk when any domain was judged as high risk of bias.19
Data Synthesis
Meta-analysis was planned for quantitative synthesis when there was sufficient homogeneity in the methodology and original data or primary studies. Otherwise, the results were summarized qualitatively.
RESULTS
Study Inclusion
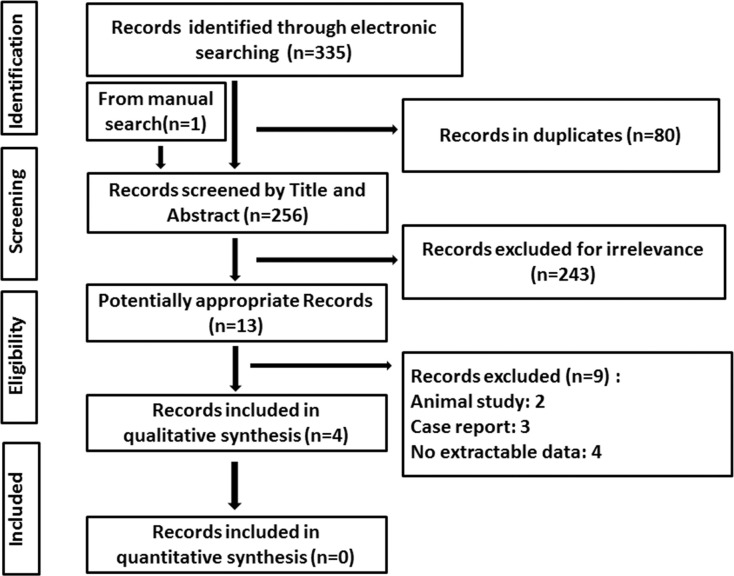
The electronic and manual search initially identified 336 relevant records. After removal of duplicate citations, a total of 256 articles were screened by reading titles and abstracts, and 243 studies were excluded. Subsequently, the 13 remaining studies were read in full text for eligibility assessment according to the inclusion criteria. In total, 4 studies were included in this review.14–17 The kappa score regarding the agreement level was .94, which could serve as the indicator of low interexaminer bias.20 The details of study inclusion are shown in the PRISMA flow diagram (Figure 1).
Figure 1.
PRISMA flow diagram of study selection.
Study Characteristics
The general information of the included studies is summarized in Table 2. Among the four studies, two were CCTs14,15 and the other two were RCTs.16,17 A total of 67 patients were enrolled in this review, with the sample size of individual studies ranging from 10 to 24. The two CCTs14,15 used split-mouth designs and recruited both adults and adolescents, while the two RCTs16,17 employed parallel-arm designs and enrolled adults exclusively. In terms of types of tooth movement, the two CCTs14,15 used canine retraction as the study model while the two RCTs16,17 focused on the alignment phase and entire treatment, respectively. One study15 compared the efficacy between piezocision and conventional corticotomy. Sample size calculation was adopted in the 2 RCTs.16,17 The repeatability of measurements was identified in all included studies.14–17
Table 2.
Overview of Included Studiesa
| Study ID |
Study Design |
Origin |
Description of Participants |
Grouping |
Type of Intervention |
Type of Tooth Movement |
Conflicts of Interest |
| Mehr (2013)17 | RCT | United States | n =13; F:8; M:5; mean age: 28.72 y | E:M:2; F:5; age: 29.12 ± 12.15 y C:M:3; F:3;age: 26.35 ± 7.73 y | E: piezoelectric corticotomy + OTM C: OTM | Complete alignment of mandibular anterior teeth (3-3) | Unclear |
| Aksakalli et al. (2016)14 | CCT | Turkey | n = 10; F: 6; M: 4; age: 16.3 ± 2.4 y | Split-mouth design, randomly selecting experimental side | E: piezoelectric corticotomy + OTM C: OTM | Distalization of maxillary canine | Unclear |
| Abbas et al. (2016)15 | CCT | Egypt | n = 20; age: 15–25 y | Group1: n = 10; Group 2: n = 10 Split-mouth design, randomly selecting side for surgery | Group 1: one side conventional corticotomy + OTM, the contralateral side OTM Group 2: one side piezoelectric corticotomy + OTM, the contralateral side OTM | Distalization of maxillary canine | None declared |
| Charavet et al. (2016)16 | RCT | Belgium | n = 24; F: 15; M: 9; age: 30 ± 8 y | E: n = 12; age: 27 y, 21–32 y C: n = 12; age: 35 y, 26–39 y | E: piezoelectric corticotomy + OTM C: OTM | Entire orthodontic treatment | None declared |
E indicates piezocision group/side; C, control group/side; OTM, orthodontic tooth movement.
Risk of Bias Assessment
The details of bias risk assessment are summarized in Figure 2. Of the four studies, three were identified as having an unclear risk of bias,15–17 and the other one was assessed as high risk of bias.14 Randomization was performed in two RCTs16,17 and partially in one CCT.15 Blinding to personnel or participants was difficult in these studies since scars of surgical procedures are noticeable. However, tooth movement velocity might be exempt from bias caused by the absence of blinding, since the regimens of orthodontic treatment were previously developed and strictly conducted in all trials. Therefore, blinding in included studies was set by default as unclear risk of bias. Two studies were assessed as unclear risk of bias in the domain of attrition bias since they lacked an analysis of dropouts.16,17 Two studies were assessed as unclear risk of bias in the domain of other bias since they used a split-mouth design.14,15
Figure 2.
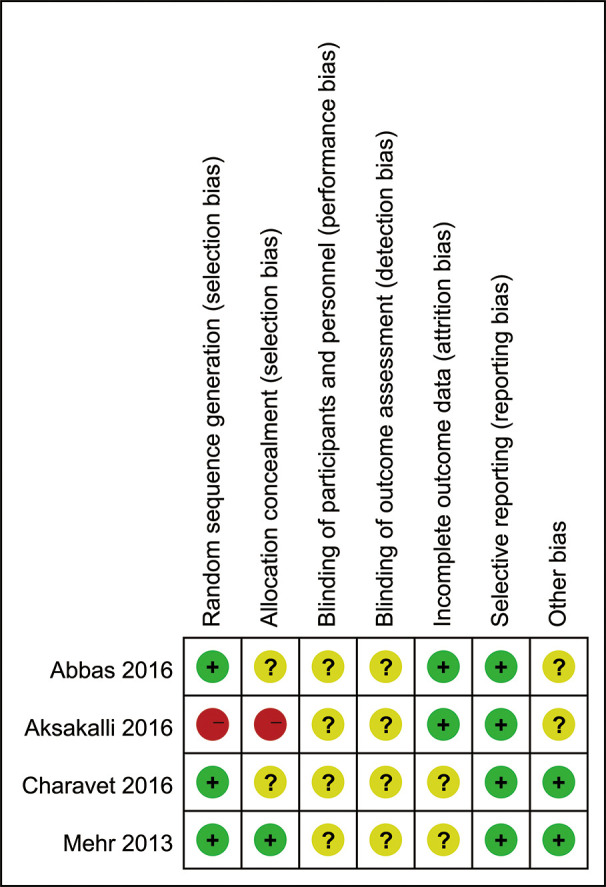
Risk of bias summary for included studies.
Effect of Interventions
The original data of the included studies could not be statistically pooled since there was a significant difference in participant ages, surgical protocols, types of tooth movement, and follow-up duration (Tables 2 and 3). Therefore, the results of these trials are systematically summarized below.
Table 3.
Characteristic of Interventions and Results
| Study ID |
Surgical Procedure Details |
Orthodontic Treatment |
| Mehr (2013)17 | Three 4-mm vertical gingiva incisions were made interproximally between lower canines and lateral incisors and central incisors labially; subsequently, a piezosurgery knife (BS1 insert, Satelec Acteon group) was used to create cortical alveolar incisions to a depth of 1 mm. | Lower 6 to 6 were bonded with self-ligation bracket. After piezocision, the dentition was aligned using sequential archwires. The alignment were considered complete when irregularity of lower 3-3 was less than 1 mm and the improvement of alignment did not exceed 0.5 mm between two consecutive appointments. |
| Aksakalli et al. (2016)14 | After placing vertical interproximal incision (10 mm) along maxillary canines, a piezosurgery knife (BS1 insert, piezotome, Merignac, France) was used to create cortical alveolar incision with a depth of 3 mm. | After alignment with moderate anchorage and the following piezocision, the upper 0.016 × 0.022-inch stainless steel wire was ligated. The maxillary canine was retracted by a force of 150g using elastomeric chains. |
| Abbas et al. (2016)15 | Corticotomy: submarginal flap was used, followed by vertical cuts and perforations along the canine root. Piezocision corticotomy: interproximal incisions were made along canine root 2 mm below papillae, followed by interproximally cortical alveolar incisions using piezotome (VarioSUrg3; NSK, Tokyo, Japan). | After complete alignment, one maxillary premolar was randomly selected and extracted on the day before surgery and the other extracted on the day of surgery. A 0.016 × 0.022-inch stainless steel wire was tied back immediately after surgery, and an NiTi closed-coil spring was used to apply a force of 150g for canine retraction. |
| Charavet et al. (2016)16 | 5-mm-long and 3-mm-deep corticotomies were made below each interdental papilla using vertical piezoelectric device at 1 week after orthodontic appliance placement. No hard or soft tissue augmentations. | All patients were featured with mild crowding and required treatment for both arches. The teeth were aligned by sequential Cu-NiTi archwires (0.014 inch to 0.018 × 0.025 inch) and 0.019 × 0.025-inch stainless steel wires. Further adjustments were performed when needed. |
Table 3.
Extended
| Follow-ups |
Tooth Movement Measurement |
Primary Results |
Other Results |
| Entire alignment phase | Time taken to reach complete alignment. Reduction in the irregularity assessed by Little's Irregularity Index. | Piezocision brought about faster tooth movement in the first 4–5 wk but did not induce significant reduction in overall treatment time. | Piezocision had no significant influence on levels of pain and satisfaction with treatment. |
| Entire canine retraction | Duration of canine retraction; the amount of canine movement was evaluated by difference of distance from canine to medial end of the third rugae in digital models. | Piezocision induces higher rate and less duration of canine retraction. | Piezocision had no obvious impact on transversal changes and gingival indices. |
| 3 months | Distance between the cusp tip of canine to the rugae line, assessed on a scanned cast | Rate of canine movement was higher in experimental sides than in control sides in both groups. Corticotomy produced a greater rate of canine movement than piezocision at most of time points. | Both conventional and piezoelectric corticotomy induced less root resorption, while it had no impact on gingival indices and anchorage loss. |
| Entire orthodontic treatment | Duration of the overall orthodontic treatment | The treatment duration was significantly reduced by 43% in the piezocision group as compared with the control group. | Compared with the control group, piezocision improved patient satisfaction, while it had no obvious effect on periodontal parameters, pain, or root resorptions. |
Rate of Tooth Movement
In all included studies, appliances were activated immediately after piezocision and adjusted at short intervals (approximately 1 weeks to 1 month). The efficacy of piezocision was compared with a control group in all four studies and with conventional corticotomy in one study.15 Mehr et al.17 observed more reduction of the irregularity index in the first 4 to 5 weeks after piezocision compared with the control group (0.109 ± 0.033 vs 0.068 ± 0.025, P = .035). However, the acceleration declined and resulted in no difference in the overall duration of alignment (98.5 ± 30.38 days vs 118.4 ± 40.77 days, P = .43).17 Two studies reported that the rate of canine distalization was significantly enhanced in quadrants treated with piezocision.14,15 Moreover, Abbas et al.15 found that conventional corticotomy produced a higher rate of canine crown movement than piezocision at 2 (0.5 ± 0.05 mm vs 0.40 ± 0.07 mm, P < .001), 4 (0.6 ± 0.05 mm vs 0.5 ± 0.07 mm, P < .001), 10 (0.94 ± 0.05 mm vs 0.84 ± 0.05 mm, P < .001), and 12 weeks (1.22 ± 0.08 mm vs 0.99 ± 0.10 mm, P < .001) after surgery.15 Charavet et al.16 investigated the effect of piezocision on the entire treatment of patients presenting with mild crowding and revealed the duration was reduced by 43% in the piezocision group (P < .0001).
Periodontal Parameters
Of the four included studies, three investigated the impact of piezocision on periodontal health by evaluating indices including plaque index, gingival index, bleeding index, recession depth, and pocket depth (Table 3).14–16 No studies in this review reported adverse effects of piezocision on periodontal status. Aksakalli et al.14 revealed that gingival index scores measured prior to and after canine retraction were similar in both groups (P > .05). Abbas et al.15 reported that piezocision had no obvious influence on gingival index and plaque index scores (P > .05).15 Charavet et al.16 found periodontal parameters including recession depth, plaque index, pocket depth, and bleeding index remained unchanged after treatment and were similar in the piezocision and control groups (P > .05).16
Root Resorption
The effect of piezocision on root resorption was evaluated in two studies.15,16 One study assessed canine root lengths before and after retraction using CBCT and found that both piezocision and conventional corticotomy reduced root resorption significantly compared with the control sides (P > .05).15 In another study, root lengths were measured at baseline and posttreatment using CT scans, and no increase of root resorption was observed in participants treated with piezocision or in the control group (P > .05).16
Pain and Discomfort
Two studies used a visual analog scale to evaluate pain intensity among participants.16,17 Charavet et al.16 found that the pain level of participants in the piezocision group reached an average of 6.0 ± 1.9 (maximum = 10), which was similar to the control group (P > .05). Mehr et al.17 reported that there was no obvious difference in pain scores (maximum = 100) between the piezocision and control groups immediately (21.53 ± 25.68 vs 9.23 ± 13.14, P = .39), 1 hour (29.45 ± 22.68 vs 12.92 ± 18.55, P = .11), 12 hours (0.5 ± 0.05 vs 0.40 ± 0.07, P > .05), and 7 days (0.5 ± 0.05 vs 0.40 ± 0.07, P > .05) after first wire placement.
Treatment Satisfaction
Patient satisfaction with orthodontic treatment was investigated using questionnaires in two studies.16,7 The level of satisfaction in the piezocision groups was significantly higher than the control group in one study (P = .012).16 In another study, the satisfaction levels were similar between the two groups (P = .23).17
Anchorage Control
Only one study in the review focused on the effect of piezocision on anchorage control. Abbas et al.15 assessed molar movement on the experimental and control sides of the piezocision and conventional corticotomy groups based on scanned casts and reported that neither piezocision (3 ± 0.38 mm vs 3.25 ± 0.52 mm, P = .221) nor conventional corticotomy (2.99 ± 0.55 mm vs 3.13 ± 0.42 mm, P = .346) influenced anchorage control.15
DISCUSSION
To the best of our knowledge, this is the first systematic review addressing the efficacy of piezocision on accelerating OTM. Because of methodological heterogeneity and the noncomparability of original data of the enrolled studies, performing a meta-analysis was not possible. Therefore, currently available evidence has been synthesized qualitatively in the review.
Despite the variation of piezocision and orthodontic procedures, all included studies observed faster tooth movement after surgery (Tables 2 and 3). Mehr et al.17 found that the rate of tooth movement was enhanced by 1.6 times in the first 4 to 5 weeks but resulted in no significant reduction of overall duration.14 Similarly, Charavet et al.16 reported the acceleratory effect decreased over treatment. These results conform to the biological mechanism of RAP, which is characterized by transient bone demineralization and increased bone metabolism, and could decline to normal levels after a certain period.21 Moreover, it should be noted that the lengths and depths of the incisions in Mehr et al.17 was much smaller than in Charavet et al.16 (4 × 1 mm vs 10 × 3 mm, Table 3), which could contribute to the more rapid decrease of acceleration in the former study. Both of the other studies reported faster canine retraction in the piezocision group.14,15 Taking the included studies together, currently available evidence supports that piezocision could accelerate tooth movement, while the acceleration would gradually decline over time. However, this conclusion should be interpreted with caution since the sample size was small (Table 2), there were methodological flaws (Figure 2), and substantial heterogeneity existed among included studies.
Studies included in this review have raised a question regarding the association between extent of the surgery performed and the acceleratory effect on OTM. Charavet et al.16 adopted more extensive surgery than Mehr et al.17 and obtained more lasting acceleration (Table 3). This suggests that the scope of the incisions could be positively associated with piezocision-induced acceleration. However, the high variation in piezocision protocols among included studies could also impair the robustness of the current review. It should be noted that the surgery performed in Abbas et al.15 involved the removal of bundle bone at the extraction sockets, which is more extensive than conventional piezocision.11 Standardizing the procedures when planning clinical trials is essential for evaluating the real effects of piezocision on OTM. Based on current information, incisions of more depth and length could result in stronger acceleration but also pose higher risks of periodontal problems and discomfort.22 Future studies should compare different procedures for their efficacy and complications to determine the optimal surgical protocol.
Periodontal health has always been one of the major concerns in corticotomy-assisted orthodontics. Because of the conservative procedures used, piezocision could be more protective to periodontal conditions compared with conventional corticotomy.7,9 Three studies examined the potential sequela of piezocision in periodontal tissue by evaluating several periodontal indices (Table 3).14–16 Although the original data could not be pooled statistically, all these studies showed consistently that performing piezocision had no obvious adverse effects on periodontal status (Table 3). Current information seems to support that piezocision is safe to periodontal tissues, while more studies are needed to evaluate this issue quantitatively. Moreover, whether piezocision outperforms conventional corticotomy in protecting periodontal health is also unclear.
A previous animal study found that corticotomy decreased periodontal ligament hyalinization and root resorption in dogs undergoing experimental orthodontic treatment.23 Similarly, a histological study found less hyalinization necrosis of periodontal ligament and root resorption on the pressure side of extracted premolars after corticotomy-facilitated arch expansion compared with the control group.24 This indicates that corticotomy could decrease the likelihood of periodontal hyalinization and subsequent root resorption. Two studies in this review focused on the effect of piezocision on root resorption.15,16 One study observed less root resorption on the experimental side through CBCT,15 and the other found that root resorption did not increase after treatment in the piezocision group using CT scans.16 This suggests that piezocision-assisted orthodontic treatment seems to have no adverse effects on root length. Nevertheless, a recent clinical trial suggested that piezocision could increase root resorption, especially when applied close to the roots.22 Regardless, future studies are required to identify the potential effect of piezocision on root resorption.
Pain perceptions were briefly assessed in two studies.16,17 Both studies adopted a visual analog scale to evaluate pain levels after piezocision and found pain perceptions in the first week after surgery were similar to those receiving orthodontic treatment only (Table 3). On the contrary, conventional corticotomy has been reported to induce severe pain after operations.25 Therefore, piezocision might be an alternative to conventional corticotomy for patients with a low pain tolerance.
Only one study in this review compared the effect of piezocision and conventional corticotomy on orthodontic treatment.15 Conventional corticotomy was found to produce more efficient canine movement. However, the 3-month (12 weeks) cumulative movement after surgery was 0.99 ± 0.10 mm in the piezocision group and 1.22 ± 0.08 mm in the conventional corticotomy group, indicating the difference could be clinically insignificant.15 Participants in the two groups were similar in terms of other variables including root resorption, periodontal condition, and anchorage control.15 Previous clinical reports proposed the merit of higher stability of corticotomy-assisted orthodontics,26 while only one study investigated the entire course of orthodontic treatment16 and no study investigated relapse in patients receiving piezocision. More well-designed studies with longer follow-up duration are needed before reaching a conclusion on the efficacy comparison between piezocision and conventional corticotomy.
Several limitations exist in the performance of this systematic review. First, although a comprehensive literature search was conducted, the shortage of high-quality clinical trials is evident. The four studies included were assessed as unclear or high risk of bias, one of which was preliminary and has not been published yet.17 Also, the heterogeneity among studies could influence conclusion credibility. Taking the extraction pattern as an example, two studies recruited patients indicated for maxillary premolar extraction,14,15 one study recruited patients indicated for nonextraction treatment in the mandible,17 and the other study had no inclusion criteria regarding extraction pattern.16 Lastly, statistical pooling was not performed because outcome measures were not comparable, and it was therefore not possible to evaluate the effect size of piezocision.
CONCLUSION
Weak evidence supports that piezocision could accelerate OTM and has no negative effects on periodontal health and pain perceptions, at least in the short term. The effects of piezocision on patient satisfaction, root resorption, and anchorage control are inconclusive. Future studies should focus more on standardizing piezocision procedures. More high-quality RCTs investigating the optimal protocol and the long-term effects of piezocision are required before recommendations for orthodontic practice can be made conclusively.
ACKNOWLEDGMENT
This work was supported by the National Nature Science Foundation of China Nos. 11372202 and 31470904, and by Orthodontic National Key Clinical Specialty Construction Program of China, West China Hospital of Stomatology, Sichuan University.
REFERENCES
- 1.Fisher MA, Wenger RM, Hans MG. Pretreatment characteristics associated with orthodontic treatment duration. Am J Orthod Dentofacial Orthop. 2010;137:178–186. doi: 10.1016/j.ajodo.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 2.Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992;101:403–407. doi: 10.1016/0889-5406(92)70112-N. [DOI] [PubMed] [Google Scholar]
- 3.Pandis N, Nasika M, Polychronopoulou A, Eliades T. External apical root resorption in patients treated with conventional and self-ligating brackets. Am J Orthod Dentofacial Orthop. 2008;134:646–651. doi: 10.1016/j.ajodo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 4.Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959;12:515–529. doi: 10.1016/0030-4220(59)90153-7. [DOI] [PubMed] [Google Scholar]
- 5.Generson RM, Porter JM, Zell A, Stratigos GT. Combined surgical and orthodontic management of anterior open bite using corticotomy. J Oral Surg. 1978;36:216–219. [PubMed] [Google Scholar]
- 6.Gantes B, Rathbun E, Anholm M. Effects on the periodontium following corticotomy-facilitated orthodontics. Case reports. J Periodontol. 1990;61:234–238. doi: 10.1902/jop.1990.61.4.234. [DOI] [PubMed] [Google Scholar]
- 7.Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 8.Wang L, Lee W, Lei DL, Liu YP, Yamashita DD, Yen SL. Tissue responses in corticotomy- and osteotomy-assisted tooth movements in rats: histology and immunostaining. Am J Orthod Dentofacial Orthop. 2009;136:770e1–11. doi: 10.1016/j.ajodo.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Cassetta M, Di Carlo S, Giansanti M, Pompa V, Pompa G, Barbato E. The impact of osteotomy technique for corticotomy-assisted orthodontic treatment (CAOT) on oral health-related quality of life. Eur Rev Med Pharmacol Sci. 2012;16:1735–1740. [PubMed] [Google Scholar]
- 10.Kim SJ, Park YG, Kang SG. Effects of corticision on paradental remodeling in orthodontic tooth movement. Angle Orthod. 2009;79:284–291. doi: 10.2319/020308-60.1. [DOI] [PubMed] [Google Scholar]
- 11.Dibart S, Sebaoun JD, Surmenian J. Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent. 2009;346:348–350. 30:342–344, [PubMed] [Google Scholar]
- 12.Dibart S, Yee C, Surmenian J, et al. Tissue response during piezocision-assisted tooth movement: a histological study in rats. Eur J Orthod. 2014;36:457–464. doi: 10.1093/ejo/cjt079. [DOI] [PubMed] [Google Scholar]
- 13.Dibart S, Surmenian J, Sebaoun JD, Montesani L. Rapid treatment of Class II malocclusion with piezocision: two case reports. Int J Periodontics Restorative Dent. 2010;30:487–493. [PubMed] [Google Scholar]
- 14.Aksakalli S, Calik B, Kara B, Ezirganli S. Accelerated tooth movement with piezocision and its periodontal-transversal effects in patients with Class II malocclusion. Angle Orthod. 2016;86:59–65. doi: 10.2319/012215-49.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbas NH, Sabet NE, Hassan IT. Evaluation of corticotomy-facilitated orthodontics and piezocision in rapid canine retraction. Am J Orthod Dentofacial Orthop. 2016;149:473–480. doi: 10.1016/j.ajodo.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 16.Charavet C, Lecloux G, Bruwier A, et al. Localized piezoelectric alveolar decortication for orthodontic treatment in adults: a randomized controlled trial. J Dent Res. 2016;95:1003–1009. doi: 10.1177/0022034516645066. [DOI] [PubMed] [Google Scholar]
- 17.Mehr R. Efficiency of Piezotome-Corticision Assisted Orthodontics in Alleviating Mandibular Anterior Crowding: A Randomized Controlled Clinical Trial [master's thesis] Storrs, Conn: University of Connecticut; 2013. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009. 339:b2535. [PMC free article] [PubMed]
- 19.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011. 343:d5928. [DOI] [PMC free article] [PubMed]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 21.Buschang P, Campbell P, Ruso S. Accelerating tooth movement with corticotomies: is it possible and desirable? Semin Orthod. 2012;18:286–294. [Google Scholar]
- 22.Patterson BM, Dalci O, Papadopoulou AK, et al. Effect of piezocision on root resorption associated with orthodontic force: a microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2017;151:53–62. doi: 10.1016/j.ajodo.2016.06.032. [DOI] [PubMed] [Google Scholar]
- 23.Iino S, Sakoda S, Ito G, Nishimori T, Ikeda T, Miyawaki S. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am J Orthod Dentofacial Orthop. 2007;131:e441–e448. doi: 10.1016/j.ajodo.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Byloff-Clar H. Treatment with active plates with and without corticotomy in late cases (juvenile): clinical and histologic study. Stoma (Heidelb) 1967;20:134–141. [PubMed] [Google Scholar]
- 25.Al-Naoum F, Hajeer MY, Al-Jundi A. Does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? A split-mouth design randomized controlled trial. J Oral Maxillofac Surg. 2014;72:1880–1889. doi: 10.1016/j.joms.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Hernandez-Alfaro F, Guijarro-Martinez R. Endoscopically assisted tunnel approach for minimally invasive corticotomies: a preliminary report. J Periodontol. 2012;83:574–580. doi: 10.1902/jop.2011.110233. [DOI] [PubMed] [Google Scholar]