Supplemental Digital Content is available in the text.
Keywords: cocaine, heart transplantation, risk factor, survival, toxicology
Abstract
Background:
The opioid crisis has led to an increase in available donor hearts, although questions remain about the long-term outcomes associated with the use of these organs. Prior studies have relied on historical information without examining the toxicology results at the time of organ offer. The objectives of this study were to examine the long-term survival of heart transplants in the recent era, stratified by results of toxicological testing at the time of organ offer as well as comparing the toxicology at the time of donation with variables based on reported history.
Methods:
The United Network for Organ Sharing database was requested as well as the donor toxicology field. Between 2007 and 2017, 23 748 adult heart transplants were performed. United Network for Organ Sharing historical variables formed a United Network for Organ Sharing Toxicology Score and the measured toxicology results formed a Measured Toxicology Score. Survival was examined by the United Network for Organ Sharing Toxicology Score and Measured Toxicology Score, as well as Cox proportional hazards models incorporating a variety of risk factors.
Results:
The number and percent of donors with drug use has significantly increased over the study period (P<0.0001). Cox proportional hazards modeling of survival including toxicological and historical data did not demonstrate differences in post-transplant mortality. Combinations of drugs identified by toxicology were not associated with differences in survival. Lower donor age and ischemic time were significantly positively associated with survival (P<0.0001).
Conclusions:
Among donors accepted for transplantation, neither history nor toxicological evidence of drug use was associated with significant differences in survival. Increasing use of such donors may help alleviate the chronic donor shortage.
What Is New?
Increasing numbers of otherwise healthy people are dying in association with drug use. Whether use of drugs or alcohol impacts the outcome of heart transplants has remained controversial.
Previous research has relied on history of drug use, but the donor is dead and cannot provide actual truth.
This is the first study to look at combinations of drugs and analyze the effect on survival.
Whether the donor died with one drug or multiple, or simply history of drug use, survival was similar.
What are the Clinical Implications?
Donors with toxicology positive for multiple drugs were associated with similar survival to those with no drug use.
Drug use (historical or current) does not represent a contraindication to utilization of an otherwise appropriate donor for transplant.
With the increase in drug overdoses, this study suggests more liberal use of such donors may lead to an increase in heart transplants.
Previous guidelines have urged caution with use of donors with a history of drug use that does not seem warranted if the donor is carefully evaluated.
The number of heart transplants in the United States has risen significantly in the past few years, in part because of the increase in opioid use and resultant overdoses.1–3 Donors with drug use have increased, and the effect of various drugs on outcomes post-transplant has been controversial for decades. Drugs such as cocaine which are directly cardiotoxic are particularly of concern. Achieving excellent heart transplant outcomes is dependent on donor selection as primary graft dysfunction may result in adverse outcomes.4 Although there are many aspects considered when evaluating a donor heart, the social history and circumstances of death are critical elements. The donor is deceased, and therefore sometimes accurate information is not available. The United Network for Organ Sharing (UNOS) maintains the registry of all solid organ transplant activity in the United States and records information about donors and recipients, including usage of drugs. Prior studies have examined the effect of donor use of cocaine as well as illicit drugs, but these analyses were based on history, without actual toxicology results from the donor.
This study has 2 specific aims. First, to examine the correlation of donor toxicology data with short- and long-term post-transplant survival. Second, because all prior registry studies have used UNOS historical variables, it was of interest to examine the correlation of data garnered from historical accounts to toxicology from the terminal admission of the donor.
Methods
Data Availability
The data used to analyze were obtained from the United Network for Organ Sharing with a specific Data Use Agreement and an Eastern Virginia Medical School Institutional Review Board waiver of informed consent. The Toxicology field is free text and may contain protected health information. Requests for these data may be made at https:optn.transplant.hrsa.gov/data/request-data/.
Time Period and Study Group
Records regarding heart donors used for transplantation from January 1, 2007 to December 31, 2017 were investigated. Only adult transplant recipients were considered, regardless of donor age, as well as adult multiorgan recipients.
Primary Outcome of Interest
The primary outcome of interest was survival post-transplant over 1, 5, and 10 years. The UNOS file includes years of observation and information on whether the patient died or was alive at the end of the observation period.
UNOS Data
UNOS, under contract from the Organ Procurement and Transplant Network, has maintained a registry of data on all solid organ transplants performed in the United States since 1987. The UNOS Standard Transplant Analysis and Research file was requested with the addition of the donor toxicology field, linked by donor ID number. Because the request involved a free-text field, the local Institutional Review Board (Eastern Virginia Medical School) granted an approval with a waiver of informed consent.
Over time, the fields of data collected by UNOS have changed with additions and deletions. There are a variety of fields that indicate history of various types of drug use. In late 2006, a free-text field was added to capture the results of donor toxicology (typically urine toxicology). This field is not structured, and Organ Procurement Organization local coordinators enter the results of any toxicology testing, but this is subject to misspellings because no structure is imposed on data entry. This field is not mandatory and can be left blank.
Parsing of Donor Toxicology Field
A total of 51 205 donor offer toxicology records were parsed but not all donors were accepted for heart transplantation. A total of 23 748 donors were used for heart transplantation between 2007 and 2017. Various attempts were made to parse the free-text field automatically, but this proved impossible due to the wide variations in spelling of drugs, as well as abbreviations. Therefore, a custom program was written in Visual Basic for Microsoft Access (Microsoft, Redmond, Washington) to display the drug toxicology field along with checkboxes on a computer screen so the authors could manually parse the field and discern which drug results were positive. Specific fields were added for the following categories to cover numerous possible drugs which might be noted in the text field: cocaine, opiates, marijuana (tetrahydrocannabinol), alcohol, benzodiazepines, barbiturates, amphetamine, methamphetamine, phencyclidine, buprenorphine, ecstasy (3,4-methylenedioxymethamphetamine, MDMA), methadone, oxycodone, propoxyphene, synthetic opioid, acetaminophen, ethylene glycol, isopropanol, lithium, methanol, methaqualone, salicylates, tricyclic antidepressants. Logic was built into the Microsoft Access program to compare subsequent records and automatically parse fields for records with the exact same content as ones interpreted by the human operator.
Toxicology Score Definitions
A Measured Toxicology Score (MTS) was defined as the sum of the individual drug fields with 1 point for each positive field. For alcohol, any notation of a nonzero blood alcohol level was recorded as positive. No information on timing from admission to blood alcohol level was available, nor were specific levels captured. The sum of toxicology fields gave a range of 0 to 23 and allowed comparison of donors with multiple positive toxicology results. Because toxicology is not a mandated field, donors without a toxicology result are recorded as unknown. Because benzodiazepines and opioids are commonly given at the time of endotracheal intubation, urine toxicology could erroneously reflect medical administration.
The UNOS Standard Transplant Analysis and Research file includes 5 fields relating to drug and alcohol use which are detailed in Table I in the Data Supplement. The UNOS Toxicology Score (UTS) was defined as the sum of the true/false fields, with a possible range of 0 to 5. Fields are based on review of history with those providing organ donation consent. Donor cocaine use is represented by 2 fields for current use and history of cocaine use. Donor heavy alcohol use is defined as ≥2 alcoholic beverages (no size specified) per day. Lastly, there are 2 fields for history of and current use of other drugs.
Statistical Methods
Descriptive statistics were employed where appropriate with means and SDs for normally distributed variables and medians with interquartile ranges for non-normally distributed variables. For variables with an unknown category, these were included as appropriate as separate categories. The frequency of drug positive donors was compared across year of transplant by χ2 and contingency tables. One-way ANOVA was used to compare the means of normally distributed variables across categories. Linear regression was used to compare the correlation of UTS and MTS. Kaplan-Meier method was used to estimate post-transplant survival, stratified by various variables. Univariate comparisons of survival were examined with Mantel log-rank statistic and Kaplan-Meier plots. Cox proportional hazards models were constructed to analyze survival with the following covariates: UTS, MTS, UNOS specified heavy alcohol history, donor and recipient gender, donor and recipient age, ischemic time, toxicology positive for benzodiazepines, cocaine, opiates, alcohol, amphetamines (including amphetamine, methamphetamine, and MDMA), and marijuana. As detailed, 3 separate models were constructed. Model 1 included only UTS, model 2 with only MTS, and model 3 included UNOS specified heavy alcohol history, donor and recipient gender, donor and recipient age, ischemic time, toxicology positive for benzodiazepines, cocaine, opiates, alcohol, any amphetamines (including amphetamine, methamphetamine, and MDMA), and marijuana. Year of transplant was separately added to each model as a sensitivity analysis. Statistical analysis was performed with JMP 15.0 (SAS Institute, Cary, NC).
Results
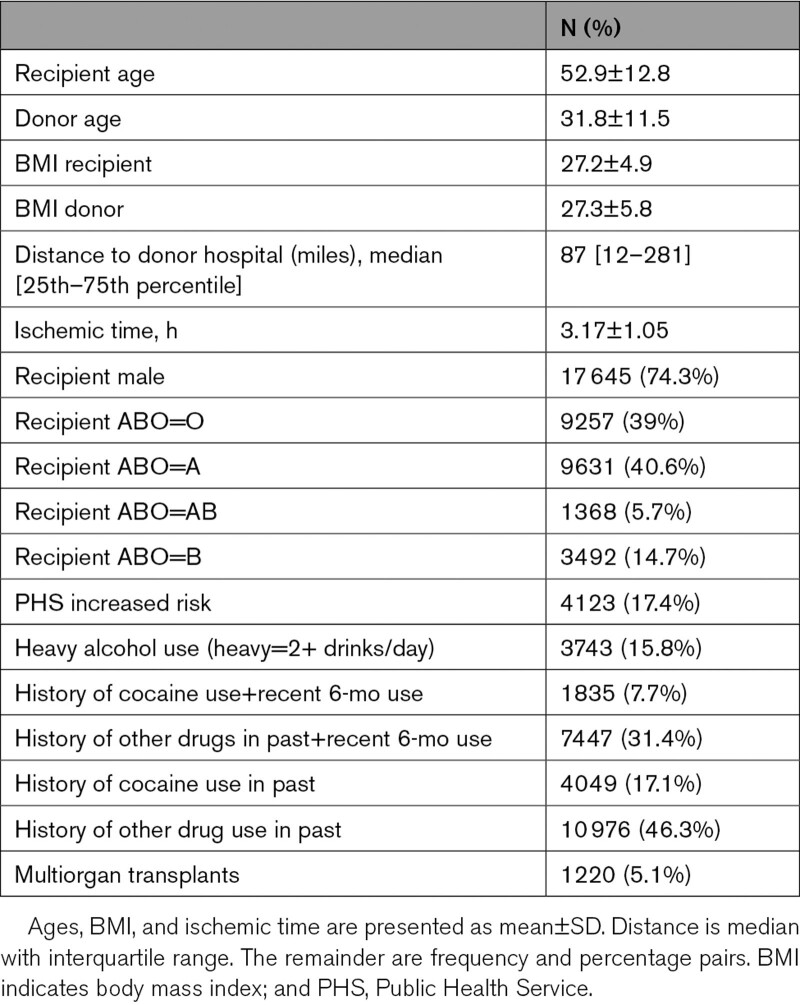
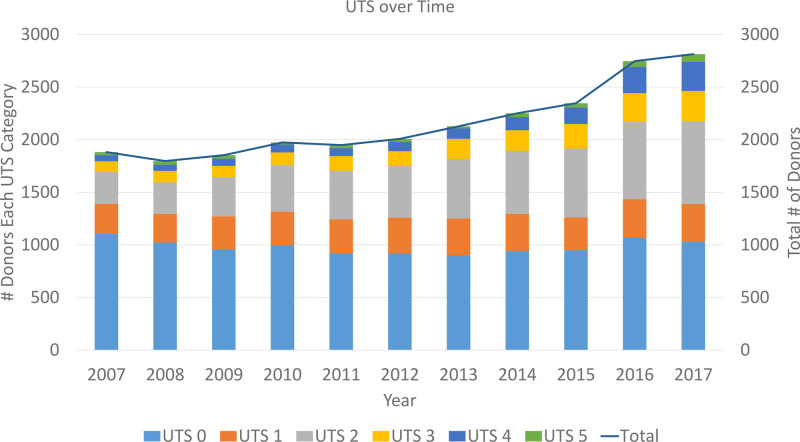
From January 1, 2007 to December 31, 2017, there were 23 748 adult heart transplants (recipient age 18 or older) entered in the UNOS registry. The demographics of transplanted patients are tabulated in Table 1. The UTS over time is depicted in Figure 1. The distribution of UTS over time is shown along with the total number of donor hearts used annually (reflected as a line). A steady increase in UTS categories 2, 3, 4, and 5 is noted over time. The majority of donors each year had a UTS of zero, with the next most common being a UTS of 2. Linear regression of UTS versus year of transplant shows a weak but statistically significant correlation (R2=0.03, P<0.0001). The percentage of donors with a UTS of one or higher has significantly increased over time as well (41.3%, 54.3%, 63.4% for years 2007, 2012, and 2017, respectively; χ2 test, P<0.0001).
Table 1.
Demographics of Transplant Recipients
Figure 1.
The United Network for Organ Sharing Toxicology Score (UTS) is a composite of all the positive drug categories from the donor record. These are based on history, not actual measured data from the donor. The most common UTS is 0 (no history of drug use), followed by UTS 2. From 2007 to 2017, the number of deceased donors has increased substantially (linear regression, R2=0.85, P<0.0001), along with the UTS values for donors. Linear regression of UTS vs year of transplant shows a weak but statistically significant correlation (R2=0.03, P<0.0001).
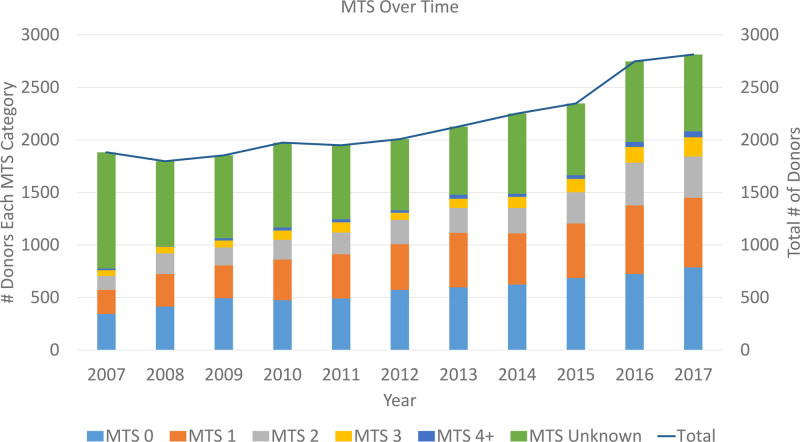
The MTS is depicted in Figure 2 and Table 2. The figure illustrates the steady increase in donor number (linear regression, R=0.85, P<0.0001), along with increases in all the donor toxicology categories, and a reduction in the number of donors not tested or with unknown results. There was a weak but statistically significant trend to increasing MTS over the years of the study (R2=0.01, P<0.0001). In recent years, most donors have either no toxicology information (listed as unknown MTS) or an MTS of 0 or 1. The next most common category is an MTS of 2. The percentage of donors with an MTS of one or higher has significantly increased over time as well (23.0%, 37.7%, 46.1% for years 2007, 2012, and 2017, respectively; χ2 test, P<0.0001).
Figure 2.
The Measured Toxicology Score (MTS) is a composite of all the positive findings on donor drug toxicology from the donor record. This score is based on findings (assuming testing is done) from the terminal admission when organ donation occurred. The figure illustrates the steady increase in donor number (linear regression, R2=0.85, P<0.0001), along with increases in all the donor toxicology categories, and a reduction in the number of donors not tested or with unknown results. There was a weak but statistically significant trend towards increasing MTS over the years of the study (R2=0.01, P<0.0001).
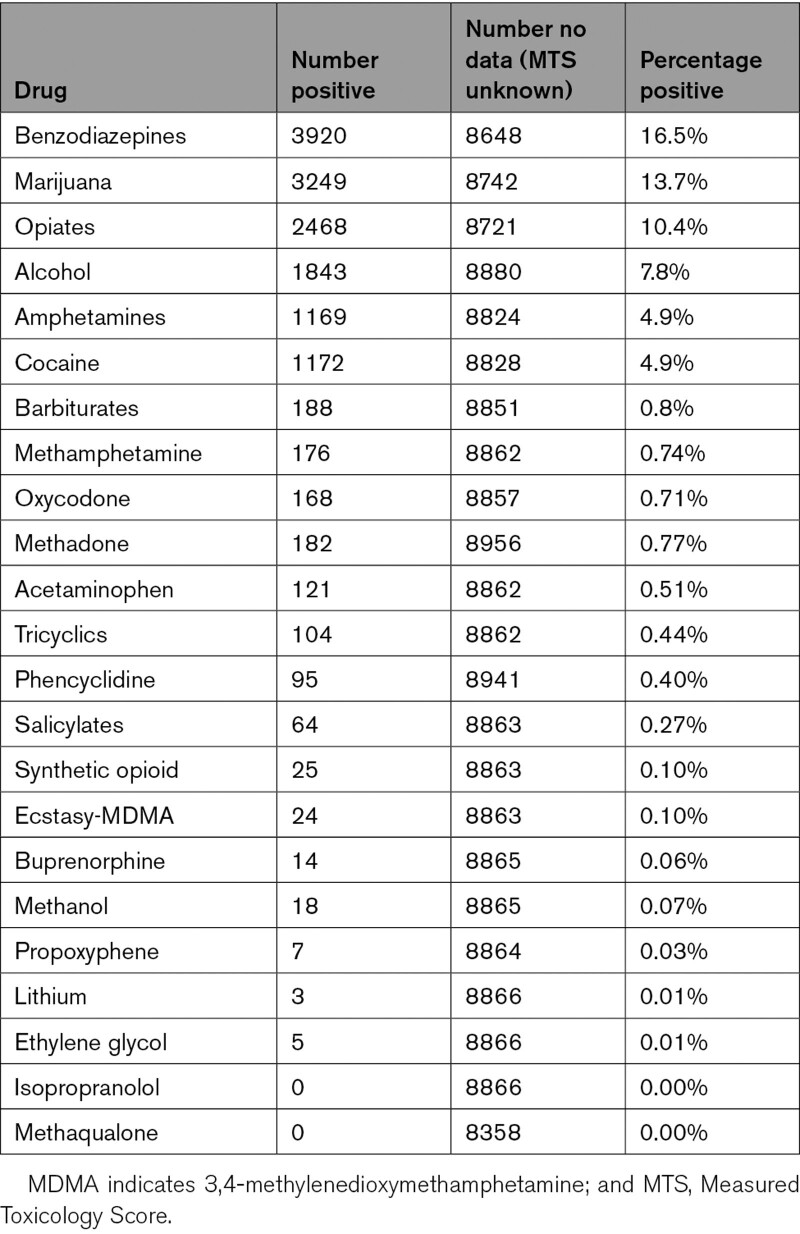
Table 2.
Drugs Detected in Donor Toxicology That Are Components in the MTS
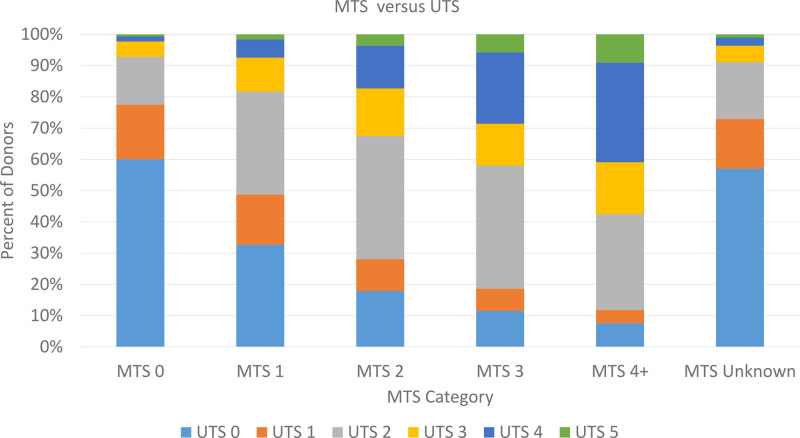
Figure 3 shows the comparison between UTS and MTS in graphical format. Sixty percent of the MTS 0 donors had a UTS of 0 as well, and as the MTS increased, the UTS did as well. Linear regression of MTS versus UTS demonstrated a significant correlation (R2=0.18, P<0.0001) Among patients where the UNOS current cocaine field was true, 49.4% (907/1835) had toxicology positive. For donors with UNOS current other drugs field positive, 64% (4764/7447) had toxicology positive for at least one drug. This dropped to 59.7% if benzodiazepines were excluded.
Figure 3.
This figure graphically illustrates the relation between the United Network for Organ Sharing Toxicology Score (UTS) and Measured Toxicology Score (MTS) across categories of MTS. Donors with either unknown MTS value (not tested) or negative drug screening have ≈50% chance of having a UTS of ≥1. Donors with 1 drug detected (MTS 1) may have a UTS of 0 in >30% of cases.
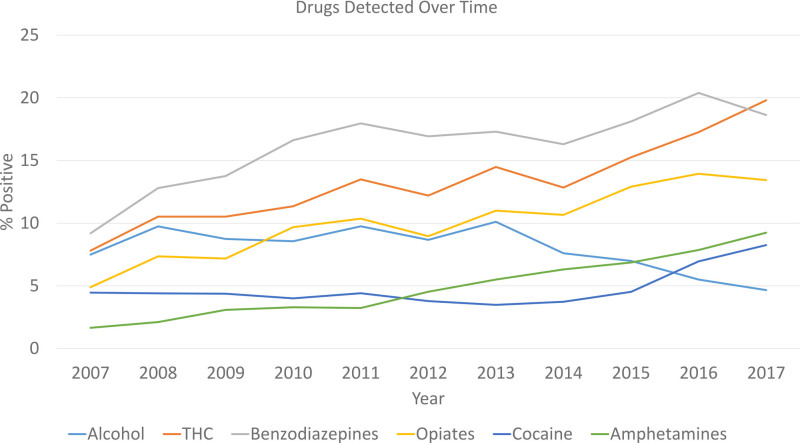
Figure 4 shows the frequency of the most common drugs of abuse found in donors over time. Positive alcohol by toxicology declined over time (subject to the limitations of the dataset), but all other drugs have increased from 2010 to 2017 (all comparisons over time, P<0.0001). The incidence of tetrahydrocannabinol, benzodiazepines, and cocaine has doubled, and amphetamines have increased >5-fold in the study period, whereas opiate use has nearly tripled. Because benzodiazepines are often used at the time of emergent intubation, it is not possible to ascertain how many positive toxicologies were related to this factor.
Figure 4.
Positive alcohol by toxicology declined over time (subject to the limitations of the dataset), but all other drugs have increased from 2010 to 2017 (all comparisons over time P<0.0001). The incidence of tetrahydrocannabinol (THC), benzodiazepines, and cocaine has doubled, and amphetamines (combination of all types) have increased >5-fold in the study period while opiate use has nearly tripled.
Survival Analysis
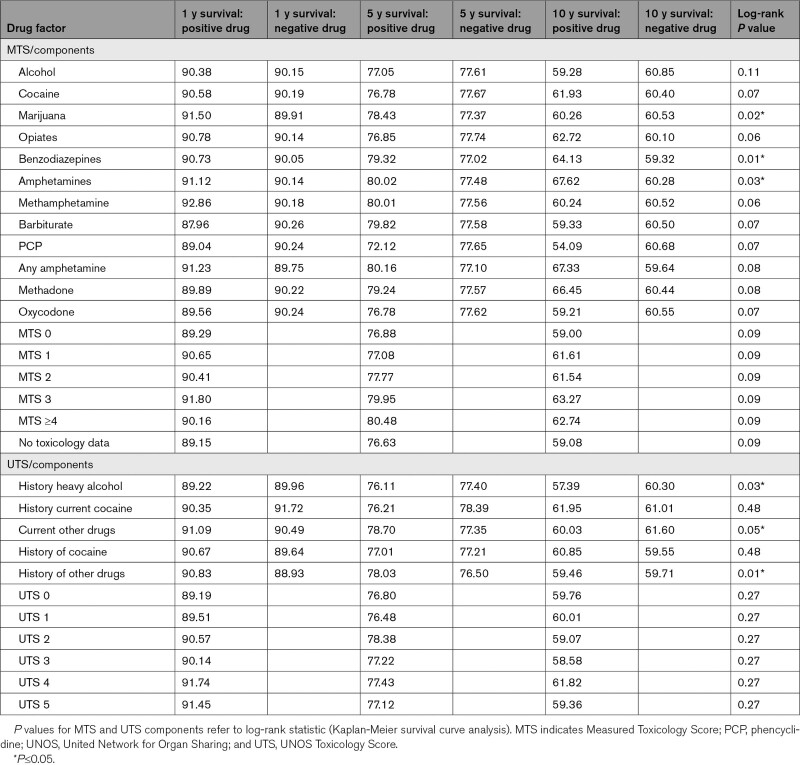
The survival of post-transplant recipients was examined, stratified by the various indices of donor drug use. Table 3 lists the 1-, 5-, and 10-year univariate survival for transplant patients divided by UTS, MTS as well as the components of each score (positive or negative), along with the P value for comparisons by Mantel log-rank test. For the overall cohort, the median follow-up was 3.07 years (interquartile range, 1.03–6.05 years). For the MTS variables, positive marijuana, benzodiazepines, and amphetamines were associated with statistically significant increased survival. For the UTS variables, current use of drugs (other than cocaine) and history of prior use of other drugs was associated with increased survival but heavy alcohol use was associated with lower survival. However, the magnitude of these differences was small, and these are not adjusted for other confounders.
Table 3.
Univariate Analysis of Survival
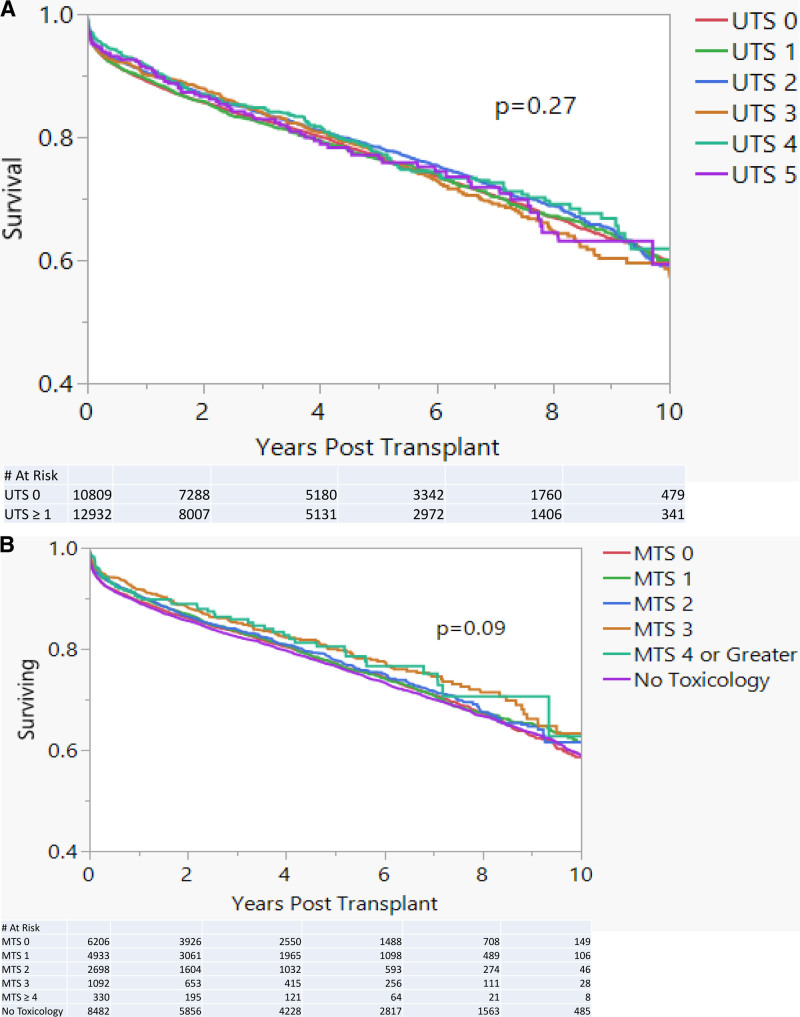
Figure 5A depicts Kaplan-Meier plots across UTS categories, and no significant difference is demonstrated (P=0.27). Similar findings were noted with analysis by MTS in Figure 5B (P=0.09) Given the common use of benzodiazepines medically, the analysis was repeated without benzodiazepines in the MTS calculation with no difference in results.
Figure 5.
Kaplan-Meier plots of survival by UTS and MTS of the donor, with no statistically significant survival difference noted with either score.A, Kaplan-Meier survival plot by value of United Network for Organ Sharing Toxicology Score (UTS). No statistically significant difference is detected (P=0.27). B, Kaplan-Meier survival plot by value of Measured Toxicology Score (MTS). No statistically significant difference is detected (P=0.09).
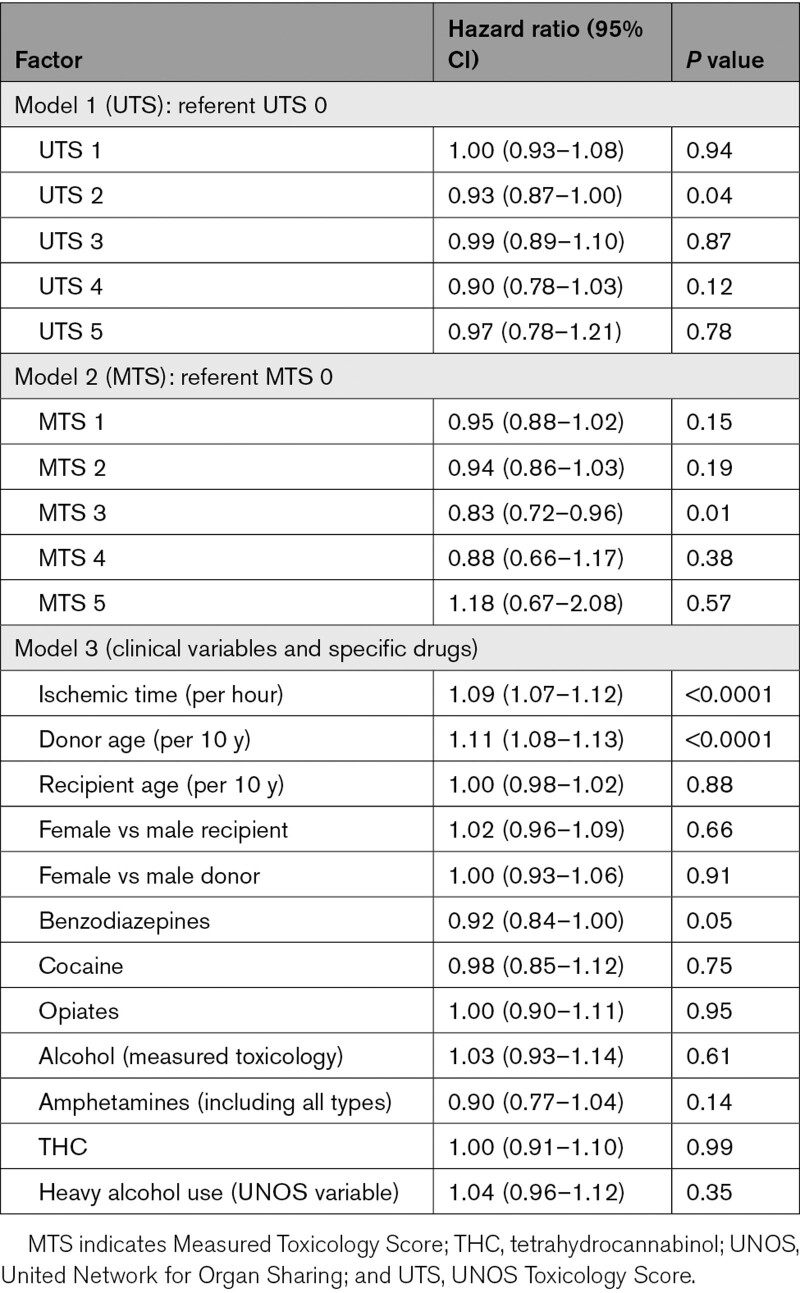
Cox proportional hazards modeling was used for multivariate analysis of variables associated with survival post-transplant. Three models were constructed. Model 1 included only the UTS, and model 2 included only the MTS. Model 3 included UNOS specified heavy alcohol history, donor and recipient gender, donor and recipient age, ischemic time, toxicology positive for benzodiazepines, cocaine, opiates, alcohol, any amphetamines (including amphetamine, methamphetamine, and MDMA), and marijuana. To focus on the influence of toxicology, the number of covariates was deliberately minimized, and factors such as donor/recipient size, gender mismatch, and others were not included.
Model 1 (UTS) did not demonstrate that UTS categories were associated with differences in survival. Model 2 for MTS was similar except that when comparing MTS 3 to 0, the point estimate of the hazard ratio was significant (0.83 [95% CI, 0.72–0.96], P=0.01).
For model 3, the predictors that were found to be statistically significant (P<0.0001) were donor age and ischemic time. The point estimates of the hazard ratio and 95% CIs are tabulated in Table 4. The individual toxicology positive for marijuana, cocaine, opiates, any amphetamines (amphetamine, methamphetamine, and MDMA), alcohol use by UNOS field, or donor alcohol toxicology were not associated with patient survival. There was no difference when year of transplant was added to each model (data not shown).
Table 4.
Cox Proportional Hazards Model of Post-Transplant Mortality vs Factors
Discussion
This is the largest study to examine drug use in heart transplant donors, and the only one to examine the actual toxicology data obtained during the terminal hospital admission. All previously published work relied on the data fields representing donor history from the UNOS database, and none has examined the donor toxicology text field. Using a custom program, the toxicology results for 23 748 donors used for cardiac transplantation over a 10-year period were parsed.
Several important findings are derived.
Over the study period, the number and percentage of donors with positive toxicology have increased significantly. Transplant teams increasingly need to consider the impact of drug history and toxicology as they evaluate prospective donors.
Donor toxicology (assessed by MTS score) is not associated with inferior survival outcomes with any drug, or combinations of drugs. This is the largest report of donors with amphetamine use, and the only report to examine the effect of multiple drugs present on toxicology.
The UNOS reported drug history fields (UTS score) roughly correlate with actual toxicology results but in a loose fashion. This is important for 2 reasons. First, clinicians may choose to decline a donor or consider it of marginal quality due to a positive history of drug use, which may not be substantiated. Second, all previously published analyses of the UNOS dataset have relied on these fields which have this inherent imprecision. These include analyses of alcohol, cocaine and other drugs, or drug intoxication in general.1,3,5–18
Previous analyses looking at the effects of donor drug use in heart transplantation have focused on cocaine use, a mix of risk factors, including methamphetamine use, drug intoxication death, and alcohol use.
Outcomes associated with donors having a history of cocaine use have been controversial. Although 2 case series suggested that these hearts are appropriate for transplantation,8,15 one group published a single case report of graft failure with an autopsy showing signs of cocaine cardiomyopathy.19 A prior large UNOS database analysis did not find any hazard short or long term with such donors5 and the International Society for Heart and Lung Transplant 2010 guidelines indicated “Hearts from donors with a history of past or current nonintravenous cocaine abuse can be used for transplantation provided cardiac function is normal and LVH is absent.”20 There was no guidance provided regarding donors with intravenous use of cocaine. Since that time multiple studies have supported the safety of selected donors with cocaine usage.10–13,21 Recently Vieira and colleagues published similar findings from the International Society for Heart and Lung Transplant Thoracic Organ Transplant registry, with 3246 donors with a history of cocaine use.22 Survival was similar to noncocaine donors but these donors were taken at a higher average sequence number indicating that they were seen as less desirable. Taken along with the current work, there should be little question regarding the safety of donors with cocaine use.
Use of amphetamines, crystal methamphetamine, and MDMA (ecstasy) are all associated with cardiotoxic effects,23–26 and therefore, use of donors with past or current use has been questioned. The only data in the literature are limited to abstracts with less than 50 cases total but there was no negative effect seen.14,17 There are no guidelines regarding use of such donors. The current study provides data on 1169 donors with various forms of amphetamine on toxicology, and no difference in survival is noted. Recent studies have looked at the UNOS cause of death field and have found that drug intoxication donor cause of death is not associated with adverse post-transplant outcomes.10,13
Alcohol is considered a cardiac toxin, and therefore, it is logical that use of donors with chronic use generates concern. An early case series in 1992 suggested that alcoholic donors had a higher rate of primary graft failure.9 A series from Cedars-Sinai reporting on patients from 1988 to 1993 also suggested early graft dysfunction may be worse with donors where even modest amounts of alcohol were taken habitually.7 The International Society for Heart and Lung Transplantation’s 2010 Guidelines for the Care of Heart Transplant Recipients suggest avoidance of such hearts but the guidance is vague: “In light of current information, the use of hearts from donors with a history of “alcohol abuse” remains uncertain, but it should probably be considered unwise.”
In 2015, a meta-analysis was published that suggested that alcohol is not a negative risk factor.27 This was followed by an analysis of >14 000 donors from the UNOS dataset which showed that donors with a history of alcohol use were not associated with worse outcomes.16 Recent publications support this and none show a difference in outcome with chronic alcohol use.12,13,28 The current study also supports the safety of such donors and should alleviate concerns about using hearts from donors with a history of significant alcohol use.
Future Directions
It will be important to look at the use of donors with reference to the MTS in particular, as the current report examines only those donors accepted for transplantation. Investigation of the characteristics of nonutilized but offered donors will be important. In addition, combinations of risk factors including donor age and characteristics of the donor will need to be considered to determine if there are donors who appear to be low risk but are not used due to drug toxicology findings. The new UNOS allocation system which went into effect October 18, 2018, also has changed the landscape of heart transplantation. The acuity of recipients has shifted even higher, and ischemic times may have lengthened as well with broader sharing. The effect of donor drug use is not clear in this population, but it is likely similar to what was shown in the current work.
Limitations
This work is based on the registry data of the UNOS database. This is subject to errors that may occur in entry of data. The donor toxicology results are based on individual local hospital labs and were not subject to a central lab review. Nevertheless, the UNOS data is what was available to centers to make organ placement decisions. Perhaps the biggest limitation of our data is that it is subject to inherent selection bias because only donors used for transplantation are reflected in the dataset.
Conclusions
This is the first and only study to look at the donor toxicology records for heart transplant recipients and examined the effect of various kinds of illicit drug use on mortality post-transplant. Post-transplant mortality is similar regardless of donor drug use, either singly or in combination. This dataset does not include information on donors not used for transplantation which imparts a selection bias. As with all transplant decisions, the clinical team needs to balance the risks and benefits and, in particular, the likelihood of a subsequent better offer.29 Based on these results, donor drug use should not impede use of an otherwise clinically acceptable donor.
Sources of Funding
None.
Disclosures
Dr Baran reports receiving consulting fees from the following companies in the prior 2 years: Getinge, Livanova, Abiomed, Abbott, MC3, and Procyrion. In addition, he has served as a speaker for Novartis and Pfizer for promotional programs in the past. Dr Herre reports research support from Analytics 4 Life, Boston Scientific, and EBR Systems, as well as consulting fees from Medtronic. He is also the Board Chair for LifeNet Health. Dr Yehya reports receiving consulting fees from Zoll, Akcea Therapeutics, and CareDx. Dr Copeland reports receiving consulting fees from Bridge to Life, and her spouse is a paid consultant for Syncardia. Dr Copeland reports receiving consulting fees from Syncardia. The other authors report no conflicts.
Supplemental Materials
Table I
Supplementary Material
Nonstandard Abbreviations and Acronyms
- MDMA
- 3,4-methylenedioxymethamphetamine
- MTS
- Measured Toxicology Score
- UNOS
- United Network for Organ Sharing
- UTS
- UNOS Toxicology Score
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCHEARTFAILURE.120.007433.
For Sources of Funding and Disclosures, see page 857.
Contributor Information
Justin Lansinger, Email: justinlansinger@gmail.com.
Ashleigh Long, Email: ashleighlong2015@gmail.com.
John M. Herre, Email: jmherre@sentara.com.
Amin Yehya, Email: axyehya@sentara.com.
Edward J. Sawey, Email: ejsawey@sentara.com.
Amit P. Badiye, Email: dramitbadiye@gmail.com.
Wayne Old, Email: wold2sail@icloud.com.
Jack Copeland, Email: hannahcopeland411@gmail.com.
Kelly Stelling, Email: kastelli@sentara.com.
Hannah Copeland, Email: hannahcopeland411@gmail.com.
References
- 1.Durand CM, Bowring MG, Thomas AG, Kucirka LM, Massie AB, Cameron A, Desai NM, Sulkowski M, Segev DL. The drug overdose epidemic and deceased-donor transplantation in the United States: a National Registry Study. Ann Intern Med. 2018;168:702–711. doi: 10.7326/M17-2451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehra MR, Jarcho JA, Cherikh W, Vaduganathan M, Lehman RR, Smits J, Stehlik J. The drug-intoxication epidemic and solid-organ transplantation. N Engl J Med. 2018;378:1943–1945. doi: 10.1056/NEJMc1802706 [DOI] [PubMed] [Google Scholar]
- 3.Vaduganathan M, Machado SR, DeFilippis EM, Bajaj N, Stehlik J, Mossialos E, Jarcho JA, Mehra MR. Organ donation and drug intoxication-related deaths in the United States. N Engl J Med. 2019;380:597–599. doi: 10.1056/NEJMc1810758 [DOI] [PubMed] [Google Scholar]
- 4.Kobashigawa J, Zuckermann A, Macdonald P, Leprince P, Esmailian F, Luu M, Mancini D, Patel J, Razi R, Reichenspurner H, et al. ; Consensus Conference participants. Report from a consensus conference on primary graft dysfunction after cardiac transplantation. J Heart Lung Transplant. 2014;33:327–340. doi: 10.1016/j.healun.2014.02.027 [DOI] [PubMed] [Google Scholar]
- 5.Brieke A, Krishnamani R, Rocha MJ, Li W, Patten RD, Konstam MA, Patel AR, Udelson JE, Denofrio D. Influence of donor cocaine use on outcome after cardiac transplantation: analysis of the United Network for Organ Sharing Thoracic Registry. J Heart Lung Transplant. 2008;27:1350–1352. doi: 10.1016/j.healun.2008.08.008 [DOI] [PubMed] [Google Scholar]
- 6.Caballero F, Lopez-Navidad A, Cotorruelo J, Txoperena G. Ecstasy-induced brain death and acute hepatocellular failure: multiorgan donor and liver transplantation. Transplantation. 2002;74:532–537. doi: 10.1097/00007890-200208270-00017 [DOI] [PubMed] [Google Scholar]
- 7.Freimark D, Aleksic I, Trento A, Takkenberg JJ, Valenza M, Admon D, Blanche C, Queral CA, Azen CG, Czer LS. Hearts from donors with chronic alcohol use: a possible risk factor for death after heart transplantation. J Heart Lung Transplant. 1996;15:150–159 [PubMed] [Google Scholar]
- 8.Freimark D, Czer LS, Admon D, Aleksic I, Valenza M, Barath P, Harasty D, Queral C, Azen CG, Blanche C. Donors with a history of cocaine use: effect on survival and rejection frequency after heart transplantation. J Heart Lung Transplant. 1994;13:1138–1144 [PubMed] [Google Scholar]
- 9.Houyel L, Petit J, Nottin R, Duffet JP, Macé L, Neveux JY. Adult heart transplantation: adverse role of chronic alcoholism in donors on early graft function. J Heart Lung Transplant. 1992;11:1184–1187 [PubMed] [Google Scholar]
- 10.Ising MS, Gallo M, Whited WM, Slaughter MS, Trivedi JR. Changing demographics of heart donors: the impact of donor drug intoxication on posttransplant survival. Am J Transplant. 2018;18:1790–1798. doi: 10.1111/ajt.14726 [DOI] [PubMed] [Google Scholar]
- 11.Jayarajan S, Taghavi S, Komaroff E, Shiose A, Schwartz D, Hamad E, Alvarez R, Wheatley G, Guy TS, Toyoda Y. Long-term outcomes in heart transplantation using donors with a history of past and present cocaine use. Eur J Cardiothorac Surg. 2015;47:e146–e150. doi: 10.1093/ejcts/ezu512 [DOI] [PubMed] [Google Scholar]
- 12.MacGowan GA, Dark JH, Corris PA, Nair AR. Effects of drug abuse, smoking and alcohol on donor hearts and lungs. Transpl Int. 2019;32:1019–1027. doi: 10.1111/tri.13468 [DOI] [PubMed] [Google Scholar]
- 13.Okoh AK, Chan O, Schultheis M, Gupta M, Shah A, Gold J, Russo MJ, Lee LY, Camacho M. Association between increased-risk donor social behaviors and recipient outcomes after heart transplantation. Clin Transplant. 2020;34:e13787. doi: 10.1111/ctr.13787 [DOI] [PubMed] [Google Scholar]
- 14.Rush J, Kittleson M, Patel J, Stimpson E, Kao T, Liou F, Aintablian T, Siddiqui S, Chang DH, Czer L, et al. Is there a risk of cocaine and methamphetamine use in heart donors? J Heart Lung Transplant. 2015;34:S276–S277. doi: 10.1016/j.healun.2015.01.775 [Google Scholar]
- 15.Shea KJ, Sopko NA, Ludrosky K, Hoercher K, Smedira NG, Taylor DO, Starling RC, Gonzalez-Stawinski GV. The effect of a donor’s history of active substance on outcomes following orthotopic heart transplantation. Eur J Cardiothorac Surg. 2007;31:452–6. discussion 456. doi: 10.1016/j.ejcts.2006.12.015 [DOI] [PubMed] [Google Scholar]
- 16.Taghavi S, Jayarajan SN, Komaroff E, Shiose A, Schwartz D, Hamad E, Alvarez R, Wheatley G, Guy TS, Toyoda Y. Use of heavy drinking donors in heart transplantation is not associated with worse mortality. Transplantation. 2015;99:1226–1230. doi: 10.1097/TP.0000000000000514 [DOI] [PubMed] [Google Scholar]
- 17.Velleca A, Kao T, Kearney B, Patel J, Kittleson M, Levine R, Dimbil S, Mersola S, Hamilton M, Esmailian F, et al. Intravenous methamphetamine does not appear to be a contraindication for heart donation in heart transplantation. J Heart Lung Transplant. 2019;38:S92. doi: 10.1016/j.healun.2019.01.213 [Google Scholar]
- 18.Warraich HJ, Lu D, Cobb S, Cooper LB, DeVore A, Patel CB, Rosenberg PB, Schroder JN, Daneshmand MA, Milano CA, et al. Trends and outcomes of cardiac transplantation from donors dying of drug intoxication. Am Heart J. 2018;199:92–96. doi: 10.1016/j.ahj.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 19.Houser SL, MacGillivray T, Aretz HT. The impact of cocaine on the donor heart: a case report. J Heart Lung Transplant. 2000;19:609–611. doi: 10.1016/s1053-2498(00)00082-6 [DOI] [PubMed] [Google Scholar]
- 20.Costanzo MR, Dipchand A, Starling R, Anderson A, Chan M, Desai S, Fedson S, Fisher P, Gonzales-Stawinski G, Martinelli L, et al. ; International Society of Heart and Lung Transplantation Guidelines. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29:914–956. doi: 10.1016/j.healun.2010.05.034 [DOI] [PubMed] [Google Scholar]
- 21.Fiorelli AI, Branco JN, Dinkhuysen JJ, Oliveira Junior JL, Pereira TV, Dinardi LF, Santos MM, Dias RR, Pereira LA, Stolf NA. Risk factor analysis of late survival after heart transplantation according to donor profile: a multi-institutional retrospective study of 512 transplants. Transplant Proc. 2012;44:2469–2472. doi: 10.1016/j.transproceed.2012.07.025 [DOI] [PubMed] [Google Scholar]
- 22.Vieira JL, Cherikh WS, Lindblad K, Stehlik J, Mehra MR. Cocaine use in organ donors and long-term outcome after heart transplantation: an International Society for Heart and Lung Transplantation registry analysis. J Heart Lung Transplant. 2020;39:1341–1350. doi: 10.1016/j.healun.2020.08.018 [DOI] [PubMed] [Google Scholar]
- 23.Civelli VF, Sharma R, Sharma O, Sharma P, Heidari A, Singh S. Methamphetamine-induced Takotsubo cardiomyopathy with hypotension, resolved by low-dose inotropes. Am J Ther. 2019;28:e498–e501. doi: 10.1097/MJT.0000000000001100 [DOI] [PubMed] [Google Scholar]
- 24.Schwarzbach V, Lenk K, Laufs U. Methamphetamine-related cardiovascular diseases. ESC Heart Fail. 2020;7:407–414. doi: 10.1002/ehf2.12572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varian KD, Gorodeski EZ. The other substance abuse epidemic: methamphetamines and heart failure. J Card Fail. 2020;26:210–211. doi: 10.1016/j.cardfail.2020.01.007 [DOI] [PubMed] [Google Scholar]
- 26.Zhao SX, Seng S, Deluna A, Yu EC, Crawford MH. Comparison of clinical characteristics and outcomes of patients with reversible versus persistent methamphetamine-associated cardiomyopathy. Am J Cardiol. 2020;125:127–134. doi: 10.1016/j.amjcard.2019.09.030 [DOI] [PubMed] [Google Scholar]
- 27.Jacob KA, de Heer LM, de Heer F, Kluin J. Chronic alcoholic donors in heart transplantation: a mortality meta-analysis. Int J Cardiol. 2015;191:7–10. doi: 10.1016/j.ijcard.2015.04.253 [DOI] [PubMed] [Google Scholar]
- 28.Newman J, Liebo M, Lowes BD, Ilias Basha H, Peled Y, Cendrowski E, Zolty R, Douglas D, Um JY, McGee E, Jr, et al. The effect of donor alcohol abuse on outcomes following heart transplantation. Clin Transplant. 2019;33:e13461. doi: 10.1111/ctr.13461 [DOI] [PubMed] [Google Scholar]
- 29.Baran DA, Copeland H, Copeland J. What number are we? Circ Heart Fail. 2019;12:e005823. doi: 10.1161/CIRCHEARTFAILURE.118.005823 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to analyze were obtained from the United Network for Organ Sharing with a specific Data Use Agreement and an Eastern Virginia Medical School Institutional Review Board waiver of informed consent. The Toxicology field is free text and may contain protected health information. Requests for these data may be made at https:optn.transplant.hrsa.gov/data/request-data/.