Summary
The high prevalence of post-acute sequelae of SARS-CoV-2 infection (PASC) is a significant health concern. In particular, virus-specific immunity in patients who suffer from chronic neurologic symptoms after acute SARS-CoV-2 infection remain poorly understood. Here, we report that Neuro-PASC patients have a specific immunological signature composed of humoral and cellular responses that are biased towards different SARS-CoV-2 structural proteins compared to healthy COVID convalescents, including a significant elevation in Nucleocapsid-specific antibody and T cell responses. Interestingly, the severity of cognitive deficits or quality of life markers in Neuro-PASC patients are associated with reduced effector molecule expression in memory T cells. Furthermore, we demonstrate a sustained elevation in T cell responses to SARS-CoV-2 mRNA vaccines in Neuro-PASC patients compared with healthy COVID convalescents. These data provide a framework for the rational design of predictive biomarkers and therapeutics for long COVID syndrome.
Keywords: COVID-19 immunity, T cell memory, Neuro-PASC, long COVID, vaccine-induced immunity
Introduction
SARS-CoV-2 is the causative agent of a worldwide pandemic that started in Wuhan, China in December, 2019. There have been more than 240 million cases and over 5 million deaths globally attributable to COVID-19 disease (1). Although highly effective vaccines are now used to prevent severe disease and death caused by SARS-CoV-2, long-term sequelae of SARS-CoV-2 infection are increasingly becoming an important medical concern.
SARS-CoV-2 infection can result in a wide spectrum of clinical manifestations ranging from asymptomatic carriage to severe multi-organ dysfunction (2–4), and predictive biomarkers to prognosticate either of these clinical outcomes are currently lacking. Globally, the estimated fatality rate following SARS-CoV-2 infection is approximately 2%, but not all patients recover to their baseline states (5). “Long COVID” affects an estimated 30% of all infected people and includes symptoms persisting more than 28 days after SARS-CoV-2 infection, termed “post-acute sequelae of SARS-CoV-2 infection” or PASC (6, 7). Greater than two-thirds of hospitalized COVID patients experience ongoing fatigue, breathlessness, and psychiatric issues such as post-traumatic stress disorder (PTSD) 4–8 weeks after discharge (8). Although the majority of people with prior SARS-CoV-2 infection experience mild disease not requiring hospitalization, more than half of these individuals have symptoms persisting more than 4 months after acute infection (9). Many people who survived Middle-East Respiratory Virus (MERS) and the original SARS-CoV epidemic also experienced PTSD and neurological impairments up to 3.5 years after acute infection (10, 11), suggesting that long-term neurological sequelae are a common consequence of certain coronavirus infections more broadly. Recent studies on recovered COVID-19 patients similarly showed significant cognitive deficits in attention, working memory, and emotional processing months after the resolution of acute infection (12).
Numerous studies suggest that T cells are necessary for the clearance of SARS-CoV-2. In particular, CD4+ T cell responses directed against the Spike protein were found in 100% of healthy COVID convalescents (13), and virus-specific T cell responses were sub-optimal or impaired in severely ill COVID patients (14). Post-mortem autopsies of COVID patients found innate immune cells but not lymphocytes were enriched in lung infiltrate, and that these patients exhibit impaired germinal center formation in lung draining lymph nodes suggesting a defective T follicular helper cell response in severe COVID (15). Additional studies have shown that CD8+ T cell depletion after SARS-CoV-2 infection of rhesus macaques impairs anamnestic immune protection after subsequent re-infection (16). However, though prior studies have suggested a role for T cells in protecting against acute SARS-CoV-2 infection, these studies did not include those with lingering PASC. Thus, the contribution of virus-specific T cell responses to the etiology of chronic Neuro-PASC remain poorly understood.
Here, we focus on a cohort of mostly non-hospitalized long COVID patients presenting with neurological symptoms (“Neuro-PASC”) who exhibit a reduction in quality of life with regards to cognitive and fatigue parameters (17). Our studies show three critical findings: Firstly, that Neuro-PASC patients exhibit decreased Spike-specific but increased Nucleocapsid- and Membrane-specific T cell responses compared with healthy convalescents. Secondly, that the severity of cognitive deficits and quality of life markers were associated with enhanced cytolytic granule expression in memory T cell subsets. Thirdly, we demonstrate that T cell responses to SARS-CoV-2 vaccination are more robust compared with control groups, but may result in aberrant kinetics. Together, these data suggest wide-scale immunological alterations in Neuro-PASC patients, with important implications for both appropriate diagnostic and treatment strategies.
Results
Clinical characteristics of Neuro-PASC patient cohorts
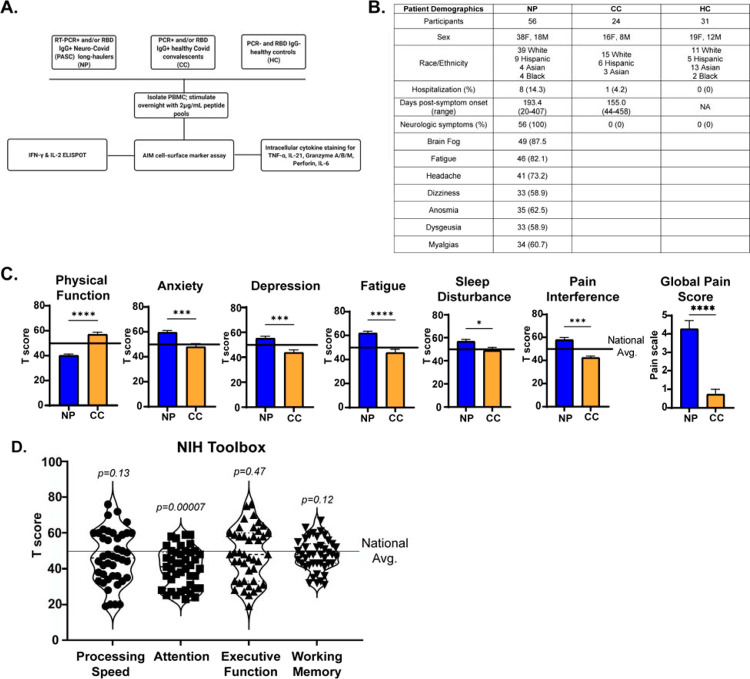
We enrolled a total of 111 participants prior to SARS-CoV-2 vaccination drawn from the Neuro-COVID-19 outpatient clinic at Northwestern Memorial Hospital or from the surrounding Chicago area. This included 56 Neuro-PASC patients (“NP” in figure legends; confirmed RT-PCR+ or anti-SARS-CoV-2 Spike IgG+) meeting Infectious Disease Society of America clinical criteria for COVID-19 starting after February 2020 and had neurologic symptoms lasting at least 6 weeks post-infection, as previously reported (17). Among those, 48 (86%) were never hospitalized for pneumonia or hypoxemia. We additionally recruited 24 healthy COVID convalescents without lasting symptoms (RT-PCR+ or seropositive for anti-SARS-CoV-2 Spike RBD IgG, “CC” in figure legends); and 31 healthy controls who were RT-PCR- and seronegative for SARS-CoV-2 Spike-IgG (“HC” in figure legends; study description in Fig. 1A).
Figure 1: Study design and clinical data.
A.) Flow chart describing study populations and experimental assays for each sample. B.) Table showing subject demographics and neurologic symptoms. C.) PROMIS-57 patient-reported survey T scores for Neuro-PASC (NP; n=36) and COVID convalescents (CC; n=13) groups. D.) NIH Toolbox cognitive T scores for NP (n=43). Horizontal black line represents the U.S. national average T score of 50; p values relative to US national average by one sample Wilcoxon signed rank test. *p<0.05, ***p<0.005, ****p<0.0001 by two-tailed Student’s t test.
Neuro-PASC patients displayed a constellation of neurological symptoms similar to those previously reported by our group and in other studies (Fig. 1B). In addition, we utilized standardized methods to quantify their quality of life and cognitive disturbances relative to healthy convalescents. Results from the patient reported outcomes information system (PROMIS-57) survey (18) showed that Neuro-PASC patients scored significantly lower on physical function and higher on anxiety, depression, pain and other metrics compared with COVID convalescent subjects or the national average (Fig. 1C). NIH toolbox tests administered to Neuro-PASC patients assessing their cognitive function (19) found them to have significantly lower T scores in the attention module, which was indicative of cognitive dysfunction relative to the national average (Fig. 1D).
Neuro-PASC is associated with a distinct immunodominance hierarchy.
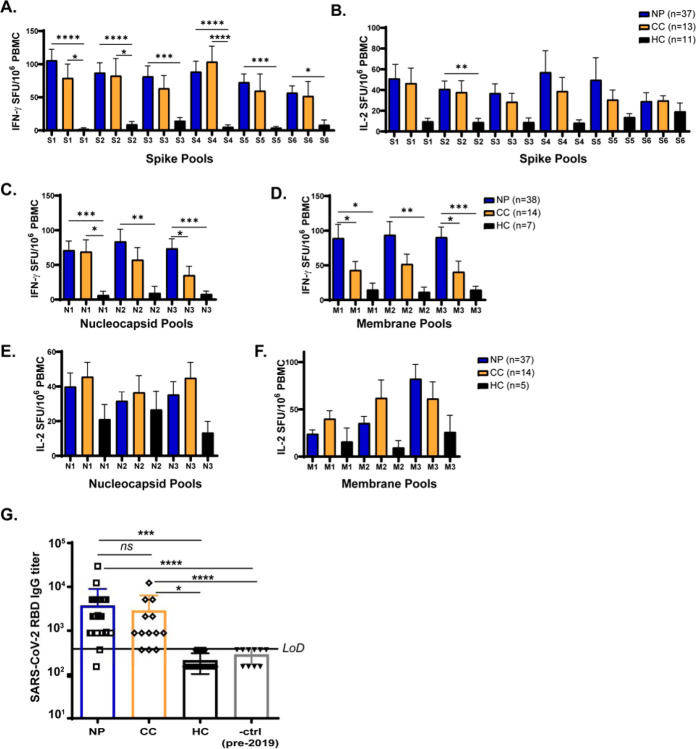
To measure virus-specific T cell responses in Neuro-PASC patients, we performed IFN-γ and IL-2 ELISPOT. Bulk peripheral blood mononuclear cells (PBMC) from each subject were stimulated with peptide pools derived from the Spike (S), Nucleocapsid (N), or Membrane (M) proteins of SARS-CoV-2 (Fig. S1). IFN-γ+ and IL-2+ T cell responses to S sub-pools were similar between Neuro-PASC and COVID convalescent subjects (Fig. 2A–B). However, Neuro-PASC individuals tended to have higher IFN-γ+ T cells against all N and M peptide pools, while COVID convalescents displayed specificity for different regions of N protein and lower responses against M peptides (Fig. 2C–D), indicative of different immunodominance hierarchies between groups. No significant differences were found in IL-2 production, and healthy controls exhibited some response to N pools likely caused by cross-reactivity with endemic coronaviruses (Fig. 2E–F). Importantly, hospitalization prior to the development of Neuro-PASC did not affect the magnitude of IFN-γ responses to viral proteins (Fig. S2). Though post-hospitalized Neuro-PASC patients trended towards lower IFN-γ+ T cell responses, these were statistically non-significant. Antibody titers against the Spike receptor-binding domain (RBD) also did not differ between Neuro-PASC and COVID convalescent groups (Fig. 2G).
Figure 2: Neuro-PASC reactivity to SARS-CoV-2 N and M peptides compared to healthy COVID convalescents.
A-B.) NP (PCR+ or seropositive Neuro-PASC) and CC (PCR+ or seropositive healthy COVID convalescent) groups display similar IFN-γ and IL-2 responses to peptides from SARS-CoV-2 Spike protein by ELISPOT. C-D.) NP samples show significantly enhanced IFN-γ responses to the N3 peptide pool (C) and to the M1 and M3 peptide pools (D) compared with CC or HC. E-F.) N- and M- specific IL-2 production did not significantly differ between subject groups. G.) Spike RBD IgG endpoint titer quantification for NP, CC, and HC groups. LOD = limit of detection. Data representative of 10 experiments with all conditions plated in duplicate. *p<0.05, **p<0.01, ***p<0.005, ****p<0.0001 by two-way ANOVA with Tukey’s posttest.
CD4+ Tfh cells display opposing reactivity to SARS-CoV-2 S- and N-proteins in Neuro-PASC vs. healthy COVID convalescents
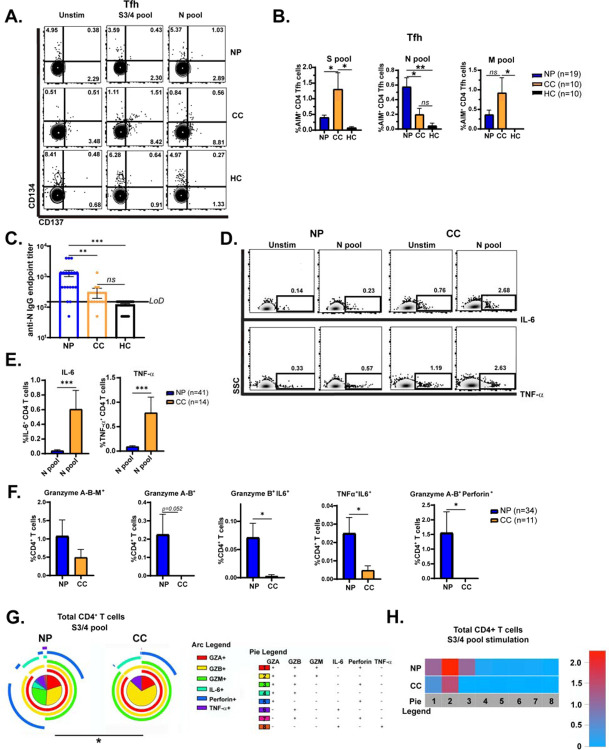
RNA-Seq analysis of CD4+ T cells from hospitalized and non-hospitalized COVID patients showed that severe disease is associated with elevated T follicular helper (Tfh) proportions relative to patients with mild disease (20). We sought to determine whether Tfh responses (see gating scheme in Fig. S3C) could similarly differentiate Neuro-PASC patients from healthy convalescents. Immunophenotyping showed that there were no differences in total percentages of T cell subsets, including Tfh cells, between groups (Fig. S4). The activation-induced marker (AIM) assay measures cytokine-independent, antigen-specific T cell activation and has been previously used to detect TCR-mediated activation of SARS-CoV-2-specific T cells (13, 21) and we used this method to investigate Tfh cell activation. Nucleocapsid-specific CD134+CD137+ (AIM+) Tfh cells were significantly elevated in Neuro-PASC compared with COVID convalescents, while the opposite trend was observed in Spike pool-specific activation (Fig. 3A–B). Interestingly, the magnitude of N-specific Tfh cell activation did not correlate with the time since acute infection in either Neuro-PASC or COVID convalescents (Fig. S5A) despite reports showing that antibody titers against N protein decrease rapidly post-infection (22) which would presumably lead to decreased Nucleocapsid-specific Tfh cell activation over time. Indeed, Nucleocapsid-specific IgG titers were in contrast significantly elevated in Neuro-PASC compared with COVID convalescents (Fig. 3C), consistent with the enhanced Nucleocapsid-specific CD4+ Tfh cell activation shown in 3B. Similar to Tfh cells, there was no correlation between anti-N IgG titers and time post-symptom onset for either Neuro-PASC or COVID convalescent subjects (Fig. S5B). Previous studies found that IgG titers against N protein decline to undetectable levels in 40% of COVID convalescents within 4 months (23). We largely did not observe this decline in Neuro-PASC patients despite collecting their blood samples an average of 193 days post-symptom onset (Fig. 1B).
Figure 3: Tfh cell activation and CD4+ T cell polyfunctionality in response to SARS-CoV-2 structral proteins in Neuro-PASC.
A.) FACS plots showing that Ag-specific CD4+ Tfh from NP patients are more highly activated in response to N peptide pool stimulation compared with CC, but less activated by Spike peptides. B.) Quantification of AIM+ Tfh cell activation to S, N, and M peptides. C.) Anti-SARS-CoV-2 Nucleocapsid IgG endpoint titers for NP, CC, and HC subjects shown in 3B. NP patients display significantly elevated anti-N IgG titers compared with CC subjects. D.) CD4+ T cells from NP produce significantly less IL-6 and TNF-α in response to N pool stimulation compared with CC individuals. E.) Quantification of cytokine production from D. F.) CD4+ T cells from NP subjects have enhanced polyfunctionality and granzyme production after S3/4 peptide stimulation compared with CC subjects. G.) Pie graphs show CD4+ T cells from CC subjects have enhanced production of granzymes A & B, granzyme B & IL-6, and TNF-α & IL-6 compared with NP subjects in response to SARS-CoV-2 S3/4 pool stimulation. H.) Heatmap quantifying polyfunctionality in different categories of cytokine production between groups. NP subjects produced 2-fold more granzymes A/B/M than CC. Data combined from 6 independent experiments with NP n=34, CC n=11. *p<0.05, **p<0.01, ***p<0.005 using one-way ANOVA with Bonferroni’s posttest (B, C); two-tailed Student’s t Test with Welch’s correction (E, F) or a Permutation test (G). All pie graphs are showing data after subtracting background (unstimulated condition; Fig. S6A).
CD4+ T cell cytokine production and polyfunctionality to SARS-CoV-2 peptides differ in Neuro-PASC vs. healthy COVID convalescents
To further probe the effector functions of Nucleocapsid-specific CD4+ T cells, we determined whether Neuro-PASC and COVID convalescent subjects had altered patterns of cytokine production after N pool stimulation. CD4+ T cells from Neuro-PASC patients expressed lower levels of IL-6 and TNF-α in an antigen-specific manner relative to COVID convalescents following stimulation with Nucleocapsid peptides (Fig. 3D–E). CD4+ T cells can also produce cytolytic granules (24, 25), and viral infections can induce expansion of CD4+ T effector memory cells that secrete copious amounts of cytolytic granules upon antigen encounter (26). We therefore investigated granzyme, Perforin, IL-6, and TNF-α expression in CD4+ T cells following stimulation with Spike peptide pools. Neuro-PASC patients had significant elevations in dual and triple cytokine- and cytolytic granule-producing CD4+ T cells after S3/4 pool stimulation, including in granzyme A/B+, granzyme-B/IL-6+, TNF-α/IL-6+, and granzyme A/B-Perforin+ CD4+ T cells (Fig. 3F). Spike-specific CD4+ T cells from Neuro-PASC subjects also demonstrated enhanced polyfunctionality, while COVID convalescents had significantly more CD4+ T cells limited to producing granzymes A/B/M after Spike pool stimulation (category 2 in yellow, Fig. 3G). A heatmap quantifying this effect showed that Neuro-PASC CD4+ T cells had a 2-fold elevation in granzyme A/B/M, granzyme A/B-Perforin, or granzyme A/B/M-Perforin, while COVID convalescents largely produced only granzyme A/B/M in response to Spike peptides (Fig. 3G–H). This data suggests that cytotoxic responses to Spike protein in CD4+ T cells from healthy COVID convalescents significantly differ from those experiencing chronic neurologic symptoms.
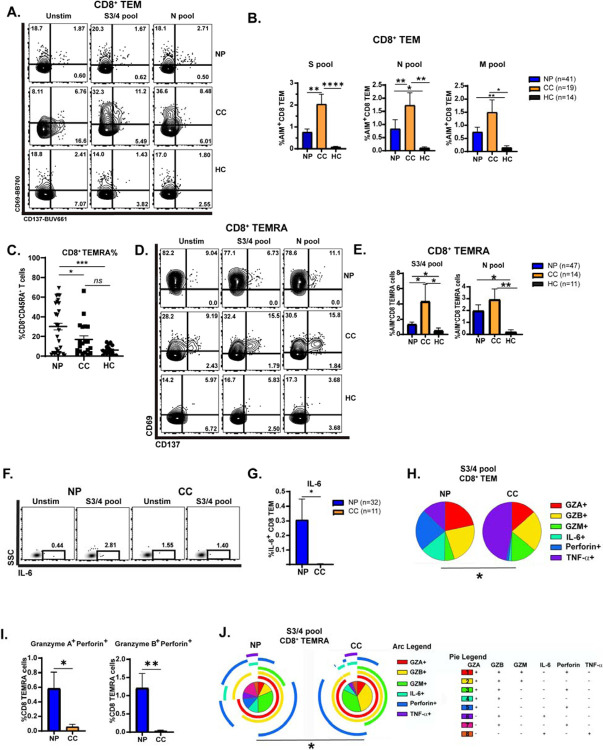
CD8+ memory T cell functionality in Neuro-PASC patients
CD8+ memory T cells are crucial for clearing virally infected cells (27). Memory CD8+ cells can persist for several years after SARS-CoV infection (28), reflecting their importance in preventing severe recurring disease. However, little is known about how memory CD8+ T cells function in Neuro-PASC vs. healthy COVID convalescents. CD8+ T effector memory cells (TEM or TEMRA; gating strategy in Fig. S3A) which are poised for rapid cytotoxic function upon antigen re-encounter exhibited significant antigen-driven activation in COVID convalescents but in Neuro-PASC patients (Fig. 4A–B). Total percentages of CD8+ TEMRA cells were significantly elevated in Neuro PASC patients (Fig. 4C), but despite their increased numbers, CD8+ TEMRA cells were less activated by S3/4 peptides and showed a trend towards decreased activation after N pool stimulation compared with COVID convalescents subjects (Fig. 4D–E).
Figure 4: CD8+ memory T cell activation and function in Neuro-PASC.
A.) Selected FACS plots showing CD8 TEM cells are less activated in NP vs. CC groups after S and N peptide pool stimulation. B.) Quantification of AIM+ CD8 TEM cells after S, N, and M peptide stimulation. C.) CD8+ TEMRA cells accumulate significantly in PBMC from NP subjects compared with CC or HC. D.) CD8+ TEMRA cells from NP patients are less activated by S3/4 and N pools compared with those from CC subjects. E.) Quantification of AIM+ CD8+ TEMRA cells from D. F-G.) CD8+ TEM from NP have significantly enhanced IL-6 production after S3/4 stimulation compared with CC. H.) Pie charts demonstrating that S3/4-specific CD8+ TEM are polarized to produce more TNF-α or granzyme B in CC group while those from NP patients produce significantly more IL-6 and Perforin. I.) CD8+ TEMRA from NP patients have elevated granzyme and Perforin production after S3/4 stimulation compared to CC subjects. J.) CD8+ TEMRA from CC subjects are less polyfunctional in response to S3/4 stimulation compared with NP subjects. Data combined from 5 independent experiments with n=34 NP, n=11 CC. *p<0.05, **p<0.01 using two-tailed Student’s t test with Welch’s correction (B, C, E, G, I) or Permutation test (H, J). All pie graphs are showing data after subtracting background (unstimulated condition; Fig. S6 B–C).
Similarly, antigen stimulation resulted in altered cytokine production in CD8+ T cell subsets from Neuro-PASC and COVID convalescents. Effector molecule production in CD8+ T cells was similar across groups in the unstimulated condition, despite showing some statistically significant differences in Perforin and granzyme B production (Fig. S6B). However, stimulation with the S3/4 pool induced greater IL-6 production in CD8+ TEM from the Neuro-PASC group compared to COVID convalescents (Fig. 4F–G). S3/4 pool stimulation also enhanced production of granzymes A or B and Perforin from CD8+ TEMRA cells in the Neuro-PASC group, whereas polyfunctionality in granzyme production was more limited in COVID convalescent subjects (Fig. 4I, J, S6C), demonstrating that CD8+ T cell memory subsets have enhanced polyfunctionality in Neuro-PASC patients after antigenic stimulation.
Impaired cognition and decreased quality of life metrics correlate with distinct patterns of polyfunctionality in memory T cell subsets
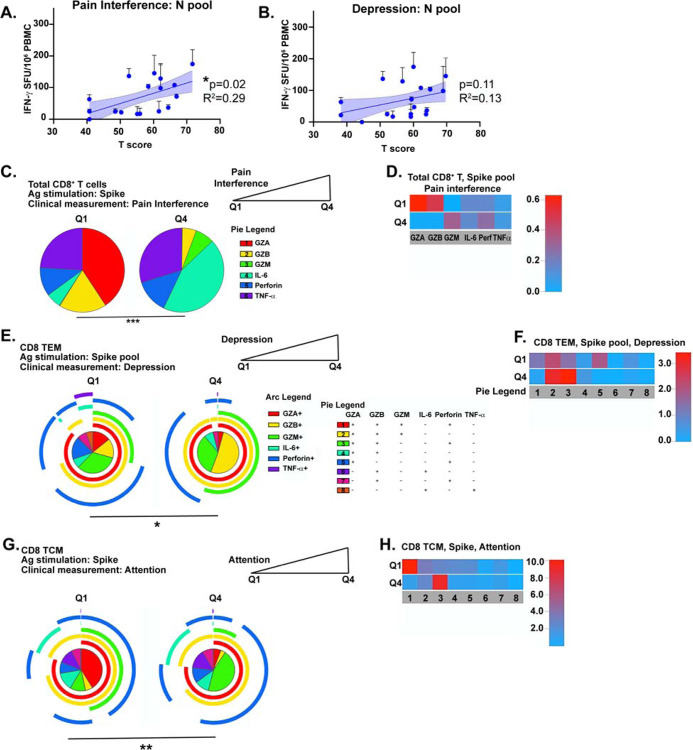
Having shown that Tfh and T cell memory responses differed between subject groups, we next sought to probe whether within-group differences in T cell responses correlated with various clinical measures in Neuro-PASC patients. We found a significant positive correlation between the magnitude of IFN-γ production to N protein and higher pain interference scores (Fig. 5A). There was also a trend towards a positive correlation between high scores for depression and the magnitude of the N-specific T cell response (Fig. 5B). To look at associations between clinical parameters and T cell activation, we separated T scores from NIH Toolbox or PROMIS-57 measurements (Fig. 1C–D) into quartiles and only the lowest and highest groups (Q1 vs. Q4) were used for analysis (Fig. S7A, red boxes). Neuro-PASC subjects reporting high (Q4) pain interference scores produced significantly less granzyme A or B and more IL-6 than those with low scores (Fig. 5C–D) from CD8+ T cells after S pool stimulation. Further, patients reporting low depression scores had highly polyfunctional Spike-specific CD8+ TEM, while those reporting high levels of depression had TEM producing ~3-fold higher granzymes A, B, and M alone (category 2; Fig. 5E, F). The severity of cognitive impairment could also be significantly correlated with T cell responses. Patients scoring low on executive function tests had CD8+ TCM polarized towards granzymes A, B, M and Perforin production, while those with high executive function were biased to produce granzymes A, B, and Perforin (Fig. 5G–H). Similar analyses were performed for other CD8+ and CD4+ memory T cell subsets, and significant differences by quartile were also found in correlations with depression, processing speed, working memory, and global pain (Fig. S7B–K). These data show that the severity of cognitive deficits or quality of life measures can be significantly correlated with differences in SARS-CoV-2-specific memory T cell function.
Figure 5: Correlation of psycho-cognitive clinical measures with CD8+ T cell function in Neuro-PASC.
A.) Higher T cell responses to N pool stimulation are positively correlated with high pain scores in NP patients. B.) A positive trend exists between elevated N-specific IFN-γ production and higher depression scores in NP patients. C.) NP patients scoring high on pain interference have Spike-specific CD8+ T cells producing more IL-6 than those scoring low. D.) Heatmap showing NP with low pain scores have Spike-specific CD8+ T cells producing significantly more granzymes A or B than those reporting high pain levels. E.) Pie graph to demonstrate that NP patients in Q4 for depression have significantly enhanced production of granzymes A/B/M compared with patients with low depression scores. F.) Heatmap demonstrating that NP patients with high depression scores had Spike-specific CD8+ TEM producing 3-fold higher levels of granzymes A, B, and M or Perforin than those scoring low on depression. G.) Spike-specific CD8+ TCM from NP patients with high scores for executive function are more polarized to produce granzymes A/B/M compared with NP patients from Q1. H.) Heatmap showing Spike-specific CD8+ TCM in Q1 NP patients are more polyfunctional and produce 8–10x more granzymes A/B/M and Perforin than those in Q4. Data representative of 5 independent experiments with n=8–9/quartile. All pie graphs showing Ag-specific cytokine production are background subtracted (unstimulated conditions). *p<0.05, **p<0.01, ****p<0.001 using Permutation tests.
SARS-CoV-2 vaccination induces more robust Spike-specific T cell responses in Neuro-PASC while displaying aberrant kinetics compared to COVID convalescents
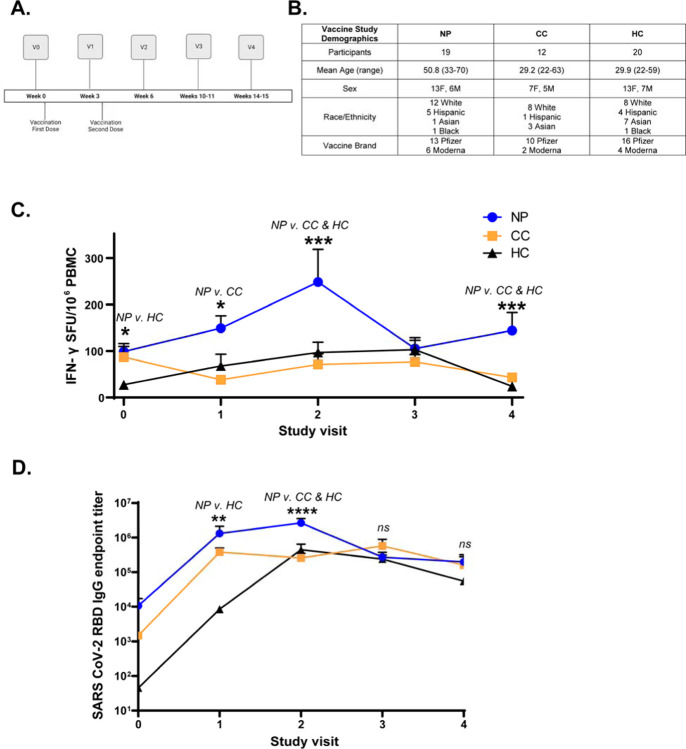
Although prior studies have shown that COVID convalescents develop more potent anti-Spike antibody responses following vaccination relative to uninfected individuals (29, 30), it is unclear whether vaccine-elicited immune responses are impacted by lingering PASC symptoms. We conducted a longitudinal study assessing Spike-specific antibody and T cell responses post-vaccination (study design and patient demographics in Fig. 6A–B). While this study is ongoing, we report data from the first 4 months comparing responses in Neuro-PASC, COVID convalescents, and unexposed healthy control subjects (sample sizes per study visit shown in Fig. S8). The magnitude and kinetics of the T cell response in COVID convalescents and healthy control subjects were similar and peaked at V3. However, Neuro-PASC patients had significantly elevated T cell responses compared with other groups at V2 after the second vaccine dose (Fig. 6C; individual pool data shown in Fig. S9), similar to what was seen with antibody titers at this same timepoint (Fig. 6D). IFN-γ-specific T cell responses remained high at 4 months post-vaccination in Neuro-PASC patients while not differing from pre-vaccination levels in both COVID convalescents and unexposed healthy controls. Vaccination also induced robust SARS-CoV-2 Spike RBD IgG titers in all groups tested by 3 weeks post-2nd dose, with the highest titers found in Neuro-PASC patients. Antibody titers declined to similar levels in all groups by 3 months post-1st dose, but trended higher in Neuro-PASC than in healthy control subjects at visit 4 (Fig. 6D). To our knowledge, these are the first data that longitudinally compare the T cell response to vaccination in Neuro-PASC patients with healthy COVID convalescents and unexposed individuals.
Figure 6: Spike-specific T cell and antibody responses after vaccination in Neuro-PASC and COVID convalescents.
A.) Vaccine study visit timeline. V0 was obtained before the first dose of either Pfizer or Moderna mRNA vaccines. V1 and V2 were conducted 3 weeks after the first and second doses, respectively. B.) Vaccine study subject demographics. C.) IFN-γ production from Spike-specific T cells do not significantly increase in CC and HC groups while remaining high in NP at 4 months post-vaccination. Total S-specific IFN-γ SFU calculated by averaging responses from each sub-pool for each participant (data in Fig. S9). D.) Longitudinal anti-Spike RBD IgG responses from V0–V4 across groups. Antibody titers are highest in NP patients at V2 and wane most quickly in HC subjects. Titers were not significantly different pre-vaccination (V0) between NP and CC individuals. Data combined from 10 individual experiments with all ELISA conditions done in triplicate and all ELISPOT conditions plated in duplicate. *p<0.05, **p<0.01, ***p<0.005, ****p<0.0001 by two-way ANOVA with Tukey’s posttest or by two-tailed Student’s t test.
Overall, our study demonstrates that Neuro-PASC patients have elevated IFN-γ responses to internal proteins of SARS-CoV-2 (N and M proteins), enhanced activation of Tfh cells linked to increased anti-Nucleocapsid antibody production, but impaired CD8+ T cell memory compared with healthy COVID convalescents. There were also correlations between the severity of cognitive deficits or quality of life impairments and increased cytolytic granule production. Importantly, vaccination resulted in robust increases Spike-specific T cell responses in Neuro-PASC patients vs. all other groups, regardless of prior COVID exposure, while also displaying aberrant kinetics. Together, we show that Neuro-PASC patients exhibit distinct activation and effector signatures in multiple aspects of the memory T cell response which may inform treatment options down the line.
Discussion
COVID-19 is well-recognized as a multi-organ disease with long-term sequelae associated with neurological dysfunction. PASC has been reported in up to 87% of those hospitalized with SARS-CoV-2 pneumonia and in 30% of those with mild disease who do not require hospitalization (31–33). Long-term sequelae after other coronavirus infections can persist for years (10); therefore, it is important to specifically characterize SARS-CoV-2-specific immune responses in long COVID patients. Most studies on effector and memory T cell responses to SARS-CoV-2 have focused on acute infection or healthy convalescents as opposed to those with long COVID (34–36). We aimed to fill this knowledge gap and determine whether and how T cell phenotype and function differ in patients with Neuro-PASC and healthy COVID-19 convalescents.
Clinically, neuro-PASC resembles myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), which many patients report as a post-viral infectious complication (37). The causes of ME/CFS remain elusive, and the underlying mechanisms of Neuro-PASC remain similarly unknown. One hypothesis for the etiology of Neuro-PASC is that symptoms could be caused by direct infection of the CNS. SARS-CoV-2 gains entry into the central nervous system through the olfactory bulb and has been shown to infect neurons in vitro, which is supported by findings of viral protein expression in cortical neurons from post-mortem autopsies and presence of virus in the brain in mouse models of infection (38–40). However, another study was unable to find any evidence of SARS-CoV-2 in the brains of 4 patients with neurological symptoms during acute infection (41), suggesting that infection of the nervous system may be transient. Further studies in acutely infected Neuro-COVID patients did not find any SARS-CoV-2 RNA present in the CSF, though they did identify enhanced presence of exhausted T cells and dedifferentiated monocytes (42). However, all of these prior studies were conducted on patients with acute SARS-CoV-2 infection as opposed to Neuro-PASC, and thus mechanisms for neurological dysfunction may differ. As lumbar punctures or brain biopsies are not indicated in neuro-PASC outpatients, reproducing the above study results in outpatient populations is not possible. Additional hypotheses for Neuro-PASC pathogenesis include a contribution of autoimmune mechanisms which is suggested by the skewed ratio of females to males affected, similar to that seen in rheumatoid arthritis or systemic lupus erythematosus (43, 44), as well as the possibility of persistent SARS-CoV-2 infection in the periphery (45). Much of our findings on the SARS-CoV-2 T cell response in neuro-PASC patients supports this latter hypothesis.
Ag-specific IFN-γ and IL-2 production was similar between Neuro-PASC and COVID convalescent groups in response to stimulation by different SARS-CoV-2 Spike peptide pools (Fig. 2A–B). However, T cells from Neuro-PASC patients retained high IFN-γ responses to all N- and M-peptide pools tested, while COVID convalescents had a reactivity limited to N1 and N2 peptide pools with little IFN-γ production in response to M pools (Fig. 2C–D). The presence of an immunodominance hierarchy in COVID convalescents is the expected outcome of an effective memory response to SARS-CoV-2 infection. Studies have shown that while a primary CD4+ or CD8+ T cell response to influenza A or LCMV infection is highly diverse and contains T cells reactive to many viral proteins and epitopes, the memory response preferentially contains T cells responding to specific immunodominant viral antigens (46, 47). This effect is more pronounced in the CD8+ T cell compartment where memory responses are dependent on the ability of dendritic cells to present viral antigen (48) or on antigen availability (49). The evident lack of a narrow and targeted IFN-γ response to N- and M-peptides in Neuro-PASC patients thus suggests that they are unable to effectively generate a memory response to SARS-CoV-2. Though there were no differences observed in the magnitude or specificity of the IFN-γ response to SARS-CoV-2 Spike peptides, this is somewhat expected as memory T cell responses to Spike protein remain diverse after both infection (13) and vaccination (50). It is additionally not surprising that differences in reactivity were observed for IFN-γ and not IL-2 T cell responses between Neuro-PASC and COVID convalescent groups (Fig. 2B, E–F). Studies have demonstrated that while Ag-specific T cells produce IL-2 as a proliferation factor, IFN-γ production is largely confined to the memory T cell compartment (51), which is largely where we see differences in activation and reactivity between groups (Fig. 4).
Antibody production is a key outcome measure after SARS-CoV-2 infection, and Tfh cell activation can inform the effectiveness of an antibody response. Stimulation with SARS-CoV-2 N peptides activated Tfh cells in Neuro-PASC but not COVID convalescent subjects (Fig. 3A–B). Tfh cell activation is crucial to the establishment of germinal centers in secondary lymphoid organs, ultimately resulting in B cell maturation into long-lived plasma cells that can continuously produce class-switched, high-affinity antibodies (52). The magnitude of the Tfh cell response is dependent on the amount of antigen available and directly correlates with the magnitude of the B cell response (53). Indeed, the same Neuro-PASC patients with high N-specific Tfh cell activation also displayed anti-N IgG titers significantly greater than COVID convalescent subjects (Fig. 3C) despite the fact that we obtained their samples more than 6 months on average after acute infection. Altogether, these findings are consistent with the potential existence of a persisting Nucleocapsid antigen reservoir resulting in enhanced N-specific Tfh cell activation in Neuro-PASC patients. Clinical reports have identified cases of persistent SARS-CoV-2 infection in the nasopharynx lasting up to 63 days (54) and many patients re-tested RT-PCR+ for SARS-CoV-2 up to 38 days post-discharge (55). The nasopharynx is not the only possible testing site, however, as there are numerous studies showing that infectious SARS-CoV-2 particles can be detected in fecal matter and can persist for up to 70 days post-symptom onset (56, 57). Gastrointestinal symptoms also did not have to be present in order to test RT-PCR+ for SARS-CoV-2 in stool samples (58). Thus, it is possible that the gut may also act as a reservoir for persistent SARS-CoV-2 infection which leads to aberrant T cell responses and the development of Neuro-PASC.
Effective generation of T cell memory responses is crucial to protect against future infections with the same pathogen. CD8+ TEM cells from COVID convalescents exhibited normal patterns of activation to S, N, and M peptides while Neuro-PASC patients displayed very little TEM activation (Fig. 4A–B), suggestive of CD8 memory T cell dysfunction. Studies on convalescents from the original SARS-CoV epidemic found that the majority of Ag-specific CD8+ memory T cells were TEM, and these persisted up to 4 years after infection (59). Resolution of acute infection is a necessary precondition for the development and maintenance of memory T cells. In particular, protracted viral infections favor the generation of short-lived effector cells and exhausted T cells (60, 61), which is why chronic infections often limit the formation and/or function of memory T cells (62). This has been shown with chronic LCMV infection in mice, which induced aberrantly functioning Ag-specific memory CD8+ T cells requiring the presence of viral peptide rather than simply the homeostatic cytokines IL-7 and IL-15 to proliferate (63, 64). The inability of CD8+ TEM to become activated by antigenic stimulation in Neuro-PASC patients is thus suggestive of a chronic infection state wherein viral antigen can persist but limits the formation of CD8+ T cell memory.
Further providing support to the chronic infection hypothesis in Neuro-PASC patients, there was a significant elevation in CD8+ TEMRA cells in Neuro-PASC patients over COVID convalescent or unexposed healthy control groups (Fig. 4C). CD8+ TEMRA cells are terminally differentiated memory T cells that do not traffic through secondary lymphoid organs, and their induction during viral infection can be protective (65). Yet, they have also been shown to accumulate during persistent viral infections and contribute to immunosenescence (66). In contrast to increased cell numbers, CD8+ TEMRA reactivity to Spike peptides was decreased in Neuro-PASC patients over COVID convalescents (Fig. 4E). Functionally, the polarization in granzyme production in S3/4-specific CD8+ TEMRA cells from COVID convalescents (Fig. 4J) suggests higher cytotoxic capacity compared with Neuro-PASC patients and coincides with their higher activation state in Fig. 4E. Ag-specific CD8+ TEMRA cells are both expanded and functionally active in people with significant anti-Dengue virus immunity, and this phenotype is seen as a goal for vaccine-induced protection (65). We propose that CD8+ TEMRA cells are more expanded but less functionally active in Neuro-PASC patients compared with healthy convalescents as a consequence of inappropriate CD8+ T cell memory formation.
We also showed that CD8+ T effector memory cells from Neuro-PASC subjects produced considerable amounts of IL-6 in response to Spike peptides, while COVID convalescents tended towards enhanced TNF-α production (Fig. 4F–H). Vaccination against the intracellular pathogen Shigella flexneri showed that polyfunctional TNF-α-producing CD8+ TEM were an important correlate of protection (67). Despite multiple reports indicating that enhanced TNF-α production is correlated with worse COVID-19 outcomes (68–70), we speculate that Ag-specific TNF-α production is protective in our model system because we are looking at chronically and not acutely infected Neuro-PASC patients. In contrast, IL-6 is known to suppress TH1 differentiation (71) and promoted pathogen survival and exacerbated clinical disease during the original SARS-CoV infection (72). Indeed, studies in severely ill, hospitalized COVID-19 patients demonstrated that high serum levels of IL-6 significantly correlated with poor clinical outcome (34). These data suggest a role for enhanced IL-6 production by CD8+ TEM in the pathogenesis of Neuro-PASC, and open new avenues of research for the treatment of long COVID through limiting IL-6 activity.
Clinically, Neuro-PASC patients reported significantly elevated levels of anxiety, depression, fatigue, sleep disturbance and pain as well as decreased physical function compared with healthy convalescents (Fig. 1C). The severity of these deficits was highly correlated with Ag-specific enhancements in polyfunctionality and decreases in polarization of various memory T cell subsets (Fig. 5, S7). It is possible that T cell function contributes to the genesis and persistence of some of these symptoms. Studies in rodents have shown that T cell activation and function can affect the severity of pain and analgesia (73, 74). Indeed, pain is a common hallmark of chronic viral infection (75) and recognized among post-COVID sequelae (76); it might follow then that aberrant T cell activation can associate with high pain scores. Additionally, reports have shown that transcriptional programs in immunity and inflammation were differentially regulated in CD4+ T cells from patients with depression compared with healthy controls (77). Treg cells may also decrease depressive behavior through negative regulation of inflammation (78), and Neuro-PASC patients do display elevated TH1-type cytokine production to S pool stimulation compared with healthy controls (Fig. 2, 6) while not displaying any compensatory upregulation in Treg total numbers or function (data not shown). T cell-derived cytokines can also impact learning and memory. Studies in mouse models of West Nile and Zika viral encephalitis have demonstrated that IFN-γ production from CD8+ T cells in the brain is responsible for neuronal apoptosis and spatial learning deficits (79). Thus, there is a precedent for correlating T cell function with cognitive deficits, pain, or depression. Ag-specific cytokine signatures associated with the severity of cognitive and quality of life deficits in Neuro-PASC patients may therefore provide some predictive value in terms of clinical outcomes.
Preliminary reports showed that the Pfizer mRNA vaccine elicits a T cell response 7 days after completion of the full prime-boost protocol (80) and induces CD8+ memory T cell activation (81), but until our studies there has been no data on longitudinal T cell responses primed by vaccination and how these vary between groups with different types of prior SARS-CoV-2 exposure. Our results demonstrate for the first time that vaccine-elicited immune responses are significantly divergent in Neuro-PASC versus healthy COVID convalescents (Fig. 6C). The magnitude of Spike-specific IFN-γ production by T cells remained high in Neuro-PASC patients out to 4 months post-vaccination while not significantly higher than pre-vaccination levels in COVID convalescents and healthy controls along the same timeline (Fig. 6C). Neuro-PASC patients also demonstrated higher antibody titers after receiving the second dose of the vaccine compared with other groups, though titers were similar in all groups at 11–15 weeks post-1st dose (Fig. 6D). Interestingly, there was significant decline in Spike-specific IFN-γ responses in Neuro-PASC patients between weeks 6 and 10 post-first dose before stabilizing at week 15 (visit 4). We speculate that vaccination may induce a short-lasting increase in the effector T cell response at 6 weeks post-1st dose before contracting to baseline levels at 10 weeks. However, IFN-γ+ T cell responses continue to remain elevated through 15 weeks in Neuro-PASC patients, unlike COVID convalescents or healthy controls, possibly due to persistent stimulation with Spike protein antigens which may not be present in other groups.
These data suggest that the mRNA vaccines do not induce robust long-term T cell responses in many individuals, regardless of prior COVID exposure, if they are not Neuro-PASC patients. Yet, despite vaccines enhancing Spike-specific IFN-γ production in Neuro-PASC T cells, the fact that these responses continue to increase rather than decline at 15 weeks post-vaccination suggests that Neuro-PASC patients may still have an active SARS-CoV-2 infection or a persistent antigen reservoir rather than developing a robust T cell memory response. Therefore, it is possible that alternate SARS-CoV-2 vaccines that induce long-lasting memory T cell responses in previously unexposed individuals as well as healthy COVID convalescents are needed in order to mediate long-term protection from infection. Conversely, vaccination strategies may need to be more fully evaluated for long COVID patients who might have a persistent infection as they may be less effective in the absence of viral clearance. Indeed, current clinical guidance from the CDC recommends that vaccination be delayed until 3 months after acute infection in unvaccinated COVID convalescents. Thus, determinants of vaccine efficacy that include measurement of T cell memory induction should be carefully considered. Together, these data show that enhanced Tfh responses, broad scale dysfunction in CD8+ T cell memory generation and aberrant T cell responses to vaccination are hallmarks of Neuro-PASC and require further study to inform treatment and vaccination strategies across the population.
Limitations of study
One limitation of our study is the relatively small sample size of unvaccinated Neuro-PASC patients. This was due to the wide implementation of SARS-CoV-2 vaccines in Chicago area soon after beginning study enrollment. Another limitation was not being able to control for time of sample collection with respect to date of COVID-19 symptom onset. As it is possible that neuro-PASC could be the result of a persistent infection, further investigations would require testing of potential cryptic reservoirs, including stool samples from Neuro-PASC patients.
Materials and Methods
Ethics Statement
This study was approved by the Northwestern University Institutional Review Board (Koralnik Lab, IRB STU00212583). Informed consent was obtained from all enrolled participants. Samples were de-identified before banking.
Study participants, NIH Toolbox, and PROMIS-57 data collection
We enrolled consenting unvaccinated adult outpatients seen in the Neuro-PASC-19 clinic at Northwestern Memorial Hospital from September 2020-June 2021, including 56 Neuro-PASC patients with documented PCR+ or seropositive IgG results for SARS-CoV-2. In parallel, we recruited 24 unvaccinated healthy COVID convalescents from the surrounding community who tested PCR+ for SARS-CoV-2 but had no lingering neurological symptoms and 31 healthy controls who tested PCR- for SARS-CoV-2 and were also seronegative for IgG against SARS-CoV-2 Spike RBD. All study subjects remained living throughout the period of observation. Heparinized blood samples were collected one time from each subject at an average of 155–315 days post-symptom onset (as in Fig. 1B). Other demographic information is contained in Fig. 1B. Neuro-PASC patients completed a cognitive function evaluation in the clinic coincident or near the date of their blood sample acquisition with the National Institutes of Health (NIH) Toolbox v2.1 instrument, including assessments of: processing speed (pattern comparison processing speed test); attention and executive memory (inhibitory control and attention test); executive function (dimensional change card sort test); and working memory (list sorting working memory test) (19, 82). PROMIS-57 was administered to Neuro-PASC and COVID convalescent subjects an average of 72 days post-sample collection. Both PROMIS-57 and NIH Toolbox results are expressed as T-scores adjusted for age, education, gender, and race/ethnicity with a score of 50 representing the normative mean/median of the US reference population with a standard deviation of 10. Lower cognition T-scores indicate worse performance while higher fatigue, depression, anxiety, or pain interference T-scores indicate greater symptom severity.
PBMC and plasma collection
30mL of venous blood from study volunteers was collected in blood collection tubes containing sodium heparin from BD Biosciences. Whole blood was layered on top of 15mL of Histopaque 1077 (Sigma-Aldrich) in 50mL Leucosep blood separation tubes (Greiner Bio-One) and spun at 1000g for 18min at RT. Plasma was collected and stored at −80°C. The PBMC layer was collected and washed 2x in sterile PBS before red blood cell lysis with ACK buffer (Quality Biologicals). PBMCs were used in assays either immediately or frozen down for use in the near term.
SARS-CoV-2 peptide antigens
All S, N and M peptide arrays used in ELISPOT and flow cytometry studies were obtained from BEI Resources, NIAID, NIH: Peptide Array, SARS-Related Coronavirus 2 Spike (S) Protein; NR-52402, Nucleocapsid (N) Protein, NR-52404; Membrane (M) Protein, NR-52403. The S peptide array consisted of 181 peptides of 13–17aa in length and split into 6 sub-pools (S1–S6) containing 30–31 peptides each. The N peptide array consisted of 59 peptides of 13–17aa each split into 3 sub-pools containing 29–30 peptides each. The M peptide array consisted of 31 peptides of 12–17aa and split into 3 sub-pools of 10–11 peptides each (Fig. S1). All peptides were dissolved in either sterile H2O or 50% sterile H2O-DMSO up to 1mL for a universal 1mg/mL stock concentration. Peptides were used at a final concentration at 2μg/mL in all assays.
IgG Spike RBD and Nucleocapsid ELISA
Antigen-specific total antibody titers were measured by ELISA as described previously (Dangi et al., 2020; Palacio et al., 2020). In brief, 96-well flat-bottom MaxiSorp plates (Thermo Scientific) were coated with 1 μg/ml of Spike RBD for 48 hr at 4°C. Plates were washed three times with wash buffer (PBS + 0.05% Tween 20). Blocking was performed with blocking solution (PBS + 0.05% Tween 20 + 2% bovine serum albumin), for 4 hr at room temperature. 6 μl of sera was added to 144 μl of blocking solution in the first column of the plate, 1:3 serial dilutions were performed until row 12 for each sample, and plates were incubated for 60 min at room temperature. Plates were washed three times with wash buffer followed by addition of secondary antibody conjugated to horseradish peroxidase, goat anti-human IgG (H + L) (Jackson ImmunoResearch) diluted in blocking solution (1:1000) and 100 μl/well was added and incubated for 60 min at room temperature. After washing plates three times with wash buffer, 100 μl/well of Sure Blue substrate (SeraCare) was added for 1 min. Reaction was stopped using 100 μl/well of KPL TMB Stop Solution (SeraCare). Absorbance was measured at 450 nm using a Spectramax Plus 384 (Molecular Devices). SARS-CoV-2 RBD and N proteins used for ELISA were produced at the Northwestern Recombinant Protein Production Core by Dr. Sergii Pshenychnyi using plasmids that were produced under HHSN272201400008C and obtained from BEI Resources, NIAID, NIH: Vector pCAGGS containing the SARS-related coronavirus 2, Wuhan-Hu-1 spike glycoprotein gene (soluble, stabilized), NR-52394 and receptor binding domain (RBD), NR-52309, nucleocapsid gene NR-53507.
Cell stimulation and IFN-γ/IL-2 ELISPOT
Multiscreen-IP plates (Millipore-Sigma) were coated overnight at 4°C with 2μg/mL anti-IFN-γ (clone 1-D1K, Mabtech) or 5μg/mL anti-IL-2 (clone MT2A91/2C95, Mabtech), washed with sterile PBS, and blocked with complete RPMI-10% FBS. PBMC isolated from Neuro-PASC, COVID convalescent, and healthy control subjects were used either freshly isolated or after thawing and resting overnight in media containing 10ng/μL recombinant human IL-15 (Peprotech) at 37°C, 5% CO2. Cells were then plated at a concentration of 2.5×105 cells/well in 100μL of media and stimulated with the indicated antigen mixtures from SARS-CoV-2 at a concentration of 2μg/mL in complete RPMI medium containing 5% human AB serum (Sigma-Aldrich) and 5ng/mL IL-15. Plates were incubated at 37°C, 5% CO2 for 20h and washed 5x with dH2O and PBS-0.05% Tween-20 (PBS-T). 2μg/mL biotinylated IFN-γ (clone 7-B6–1, Mabtech) or 5μg/mL IL-2 (clone MT8G10, Mabtech) diluted in PBS-10% FBS (PBS-F) was added to the respective wells and plates were incubated for 1.5h at RT. Plates were subsequently incubated for 40 minutes at RT in streptavidin-alkaline phosphatase in PBS-F (Jackson ImmunoResearch) was added after washing plates 5x in PBS-T. ELISPOT plates were developed using an Alkaline Phosphatase Conjugate Substrate Kit according to manufacturer’s instructions (Bio-Rad Laboratories, Carlsbad, CA). IFN-γ or IL-2-producing cells were quantified using an ImmunoSpot reader (Cellular Technologies, Ltd., Shaker Heights, OH).
Antibodies and Flow Cytometry
Fresh or frozen PBMCs isolated from the indicated patient groups were stimulated with antigen mixtures as above for 20–22h at 37°C, 5% CO2. For intracellular staining and cytokine detection, the Brefeldin-A Golgi plug (Biolegend) was added at a 1:1000 concentration 2 hours after antigenic stimulation commenced. Cells were washed with PBS-1% BSA after incubation and incubated with the indicated antibodies for surface phenotyping by AIM assay or for intracellular cytokine staining (ICS; antibodies used described in Supplemental Table 1). Cells from each subject were left unstimulated in medium containing 5ng/mL IL-15 (“background”) or stimulated in the presence of the indicated antigens. Fixation and permeabilization was performed using Cytofix/Cytoperm (BD Biosciences). Surface staining was done in the dark at 4°C for 30 minutes, while ICS was done in the dark at RT for 45 minutes. Flow cytometry was conducted on 2–5×105 cells per condition. Data was acquired on a BD FACSymphony Spectral analyzer and analyzed using FlowJo v10 (BD Biosciences) and SPICE-Pestle (83).
Quantification and Statistical Analysis
Statistical tests to determine significance are described in figure legends and conducted largely in Prism (GraphPad). For pie graphs or heatmaps generated using SPICE analysis, statistics were determined by Permutation test following unstimulated background subtraction, with additional thresholding of 0.03% to account for noise, using SPICE-Pestle. P-values lower than 0.05 were considered statistically significant. Quantile stratification was performed within group for Neuro-PASC cohort. Clinical data were collected and managed using REDCap electronic data capture tools hosted at Northwestern University Feinberg School of Medicine (84). REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
Supplementary Material
Acknowledgements
We would like to thank the Flow Cytometry Core Facility at the Robert H. Lurie Comprehensive Cancer Center at Northwestern University supported by Cancer Center Support Grant (NCI CA060553) for their assistance in optimizing antibody panels and help with flow cytometry instrumentation. L.V. was supported by a T32 grant T32AR007611 from the Department of Rheumatology, Northwestern University Feinberg School of Medicine. P.P.M. is supported by a grant from the Emerging and Re-Emerging Pathogens Program (EREPP) at Northwestern University, and a grant from the National Institute on Drug Abuse (NIDA, DP2DA051912).
Footnotes
Declaration of Interests
The authors declare no competing interests.
References
- 1.J. C. R. Center. (Johns Hopkins University of Medicine, Baltimore, MD, 2021), vol. 2021. [Google Scholar]
- 2.Syed, Khan A., Gosai F., Asif A., Dhillon S., Gastrointestinal pathophysiology of SARS-CoV2 - a literature review. J Community Hosp Intern Med Perspect 10, 523–528 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liguori et al. , Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun 88, 11–16 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y. C., Bai W. Z., Hashikawa T., The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol 92, 552–555 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins V., Sohaei D., Diamandis E. P., Prassas I., COVID-19: from an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci, 1–23 (2020). [DOI] [PubMed] [Google Scholar]
- 6.Ladds E. et al. , Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv Res 20, 1144 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vehar S., Boushra M., Ntiamoah P., Biehl M., Post-acute sequelae of SARS-CoV-2 infection: Caring for the ‘long-haulers’. Cleve Clin J Med 88, 267–272 (2021). [DOI] [PubMed] [Google Scholar]
- 8.Halpin S. J. et al. , Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol 93, 1013–1022 (2021). [DOI] [PubMed] [Google Scholar]
- 9.Petersen M. S. et al. , Long COVID in the Faroe Islands - a longitudinal study among non-hospitalized patients. Clin Infect Dis, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed H. et al. , Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J Rehabil Med 52, jrm00063 (2020). [DOI] [PubMed] [Google Scholar]
- 11.Lam M. H. et al. , Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med 169, 2142–2147 (2009). [DOI] [PubMed] [Google Scholar]
- 12.Hampshire, Trender W., Chamberlain SR, Jolly AE, Grant JE, Patrick F, Mazibuko N, Williams S, Barnaby JM, Hellyer H, Mehta MA., Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grifoni et al. , Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181, 1489–1501 e1415 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toor S. M., Saleh R., Sasidharan Nair V., Taha R. Z., Elkord E., T-cell responses and therapies against SARS-CoV-2 infection. Immunology 162, 30–43 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duan Y. Q. et al. , Deficiency of Tfh Cells and Germinal Center in Deceased COVID-19 Patients. Curr Med Sci 40, 618–624 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McMahan K. et al. , Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature 590, 630–634 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graham E. L. et al. , Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers”. Ann Clin Transl Neurol 8, 1073–1085 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tang E. et al. , Validation of the Patient-Reported Outcomes Measurement Information System (PROMIS)-57 and −29 item short forms among kidney transplant recipients. Qual Life Res 28, 815–827 (2019). [DOI] [PubMed] [Google Scholar]
- 19.Weintraub S. et al. , Cognition assessment using the NIH Toolbox. Neurology 80, S54–64 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meckiff J. et al. , Imbalance of Regulatory and Cytotoxic SARS-CoV-2-Reactive CD4(+) T Cells in COVID-19. Cell 183, 1340–1353 e1316 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Havenar-Daughton et al. , Cytokine-Independent Detection of Antigen-Specific Germinal Center T Follicular Helper Cells in Immunized Nonhuman Primates Using a Live Cell Activation-Induced Marker Technique. J Immunol 197, 994–1002 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Elslande J. et al. , Longitudinal follow-up of IgG anti-nucleocapsid antibodies in SARS-CoV-2 infected patients up to eight months after infection. J Clin Virol 136, 104765 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muecksch F. et al. , Longitudinal Serological Analysis and Neutralizing Antibody Levels in Coronavirus Disease 2019 Convalescent Patients. J Infect Dis 223, 389–398 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goubard et al. , Superantigenic Yersinia pseudotuberculosis induces the expression of granzymes and perforin by CD4+ T cells. Infect Immun 83, 2053–2064 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sledzinska et al. , Regulatory T Cells Restrain Interleukin-2- and Blimp-1-Dependent Acquisition of Cytotoxic Function by CD4(+) T Cells. Immunity 52, 151–166 e156 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tian Y. et al. , Unique phenotypes and clonal expansions of human CD4 effector memory T cells re-expressing CD45RA. Nat Commun 8, 1473 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mockus T. E., Ren H. M., Shwetank, Lukacher A. E. To Go or Stay: The Development, Benefit, and Detriment of Tissue-Resident Memory CD8 T Cells during Central Nervous System Viral Infections. Viruses 11, (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen H. et al. , Response of memory CD8+ T cells to severe acute respiratory syndrome (SARS) coronavirus in recovered SARS patients and healthy individuals. J Immunol 175, 591–598 (2005). [DOI] [PubMed] [Google Scholar]
- 29.Krammer F. et al. , Antibody Responses in Seropositive Persons after a Single Dose of SARS-CoV-2 mRNA Vaccine. N Engl J Med 384, 1372–1374 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dangi T. et al. , Cross-protective immunity following coronavirus vaccination and coronavirus infection. J Clin Invest, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahase, Covid-19: What do we know about “long covid”? BMJ 370, m2815 (2020). [DOI] [PubMed] [Google Scholar]
- 32.Hirschtick J. L. et al. , Population-based estimates of post-acute sequelae of SARS-CoV-2 infection (PASC) prevalence and characteristics. Clin Infect Dis, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Havervall S. et al. , Symptoms and Functional Impairment Assessed 8 Months After Mild COVID-19 Among Health Care Workers. JAMA 325, 2015–2016 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weiskopf et al. , Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci Immunol 5, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodda L. B. et al. , Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19. Cell 184, 169–183 e117 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sekine T. et al. , Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19. Cell 183, 158–168 e114 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rasa S. et al. , Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med 16, 268 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klingenstein M. et al. , Evidence of SARS-CoV2 Entry Protein ACE2 in the Human Nose and Olfactory Bulb. Cells Tissues Organs 209, 155–164 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Song et al. , Neuroinvasion of SARS-CoV-2 in human and mouse brain. J Exp Med 218, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dangi T., Class J., Palacio N., Richner J. M., Penaloza MacMaster P., Combining spike- and nucleocapsid-based vaccines improves distal control of SARS-CoV-2. Cell Rep 36, 109664 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kantonen J. et al. , Neuropathologic features of four autopsied COVID-19 patients. Brain Pathol 30, 1012–1016 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heming M. et al. , Neurological Manifestations of COVID-19 Feature T Cell Exhaustion and Dedifferentiated Monocytes in Cerebrospinal Fluid. Immunity 54, 164–175 e166 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Myasoedova E., Crowson C. S., Kremers H. M., Therneau T. M., Gabriel S. E., Is the incidence of rheumatoid arthritis rising?: results from Olmsted County, Minnesota, 1955–2007. Arthritis Rheum 62, 1576–1582 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chakravarty E. F., Bush T. M., Manzi S., Clarke A. E., Ward M. M., Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum 56, 2092–2094 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Aly Z., Xie Y., Bowe B., High-dimensional characterization of post-acute sequelae of COVID-19. Nature 594, 259–264 (2021). [DOI] [PubMed] [Google Scholar]
- 46.Sant J., DiPiazza A. T., Nayak J. L., Rattan A., Richards K. A., CD4 T cells in protection from influenza virus: Viral antigen specificity and functional potential. Immunol Rev 284, 91–105 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tebo E. et al. , Rapid recruitment of virus-specific CD8 T cells restructures immunodominance during protective secondary responses. J Virol 79, 12703–12713 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crowe S. R. et al. , Differential antigen presentation regulates the changing patterns of CD8+ T cell immunodominance in primary and secondary influenza virus infections. J Exp Med 198, 399–410 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Henrickson S. E. et al. , Antigen availability determines CD8(+) T cell-dendritic cell interaction kinetics and memory fate decisions. Immunity 39, 496–507 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alter et al. , Immunogenicity of Ad26.COV2.S vaccine against SARS-CoV-2 variants in humans. Nature, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anthony D. D. et al. , Dissecting the T Cell Response: Proliferation Assays vs. Cytokine Signatures by ELISPOT. Cells 1, 127–140 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Good-Jacobson K. L., Shlomchik M. J., Plasticity and heterogeneity in the generation of memory B cells and long-lived plasma cells: the influence of germinal center interactions and dynamics. J Immunol 185, 3117–3125 (2010). [DOI] [PubMed] [Google Scholar]
- 53.Baumjohann D. et al. , Persistent antigen and germinal center B cells sustain T follicular helper cell responses and phenotype. Immunity 38, 596–605 (2013). [DOI] [PubMed] [Google Scholar]
- 54.Bennasrallah et al. , Three COVID-19 cases with a long-term viral shedding period in Tunisia. Pan Afr Med J 35, 117 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dao T. L., Hoang V. T., Gautret P., Recurrence of SARS-CoV-2 viral RNA in recovered COVID-19 patients: a narrative review. Eur J Clin Microbiol Infect Dis 40, 13–25 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tian Y., Rong L., Nian W., He Y., Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther 51, 843–851 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van Doorn S., Meijer B., Frampton C. M. A., Barclay M. L., de Boer N. K. H., Systematic review with meta-analysis: SARS-CoV-2 stool testing and the potential for faecal-oral transmission. Aliment Pharmacol Ther 52, 1276–1288 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen Y. et al. , The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol 92, 833–840 (2020). [DOI] [PubMed] [Google Scholar]
- 59.Channappanavar R., Zhao J., Perlman S., T cell-mediated immune response to respiratory coronaviruses. Immunol Res 59, 118–128 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mueller S. N., Gebhardt T., Carbone F. R., Heath W. R., Memory T cell subsets, migration patterns, and tissue residence. Annu Rev Immunol 31, 137–161 (2013). [DOI] [PubMed] [Google Scholar]
- 61.Palacio N. et al. , Early type I IFN blockade improves the efficacy of viral vaccines. J Exp Med 217, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wherry E. J., T cell exhaustion. Nat Immunol 12, 492–499 (2011). [DOI] [PubMed] [Google Scholar]
- 63.Shin, Blackburn S. D., Blattman J. N., Wherry E. J., Viral antigen and extensive division maintain virus-specific CD8 T cells during chronic infection. J Exp Med 204, 941–949 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wherry E. J., Barber D. L., Kaech S. M., Blattman J. N., Ahmed R., Antigen-independent memory CD8 T cells do not develop during chronic viral infection. Proc Natl Acad Sci U S A 101, 16004–16009 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tian Y. et al. , Dengue-specific CD8+ T cell subsets display specialized transcriptomic and TCR profiles. J Clin Invest 129, 1727–1741 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Derhovanessian E. et al. , Infection with cytomegalovirus but not herpes simplex virus induces the accumulation of late-differentiated CD4+ and CD8+ T-cells in humans. J Gen Virol 92, 2746–2756 (2011). [DOI] [PubMed] [Google Scholar]
- 67.Toapanta F. R., Bernal P. J., Kotloff K. L., Levine M. M., Sztein M. B., T cell mediated immunity induced by the live-attenuated Shigella flexneri 2a vaccine candidate CVD 1208S in humans. J Transl Med 16, 61 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karki R. et al. , COVID-19 cytokines and the hyperactive immune response: Synergism of TNF-alpha and IFN-gamma in triggering inflammation, tissue damage, and death. bioRxiv, (2020). [Google Scholar]
- 69.Karki R. et al. , Synergism of TNF-alpha and IFN-gamma Triggers Inflammatory Cell Death, Tissue Damage, and Mortality in SARS-CoV-2 Infection and Cytokine Shock Syndromes. Cell 184, 149–168 e117 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pedersen S. F., Ho Y. C., SARS-CoV-2: a storm is raging. J Clin Invest 130, 2202–2205 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Diehl S. et al. , Inhibition of Th1 differentiation by IL-6 is mediated by SOCS1. Immunity 13, 805–815 (2000). [DOI] [PubMed] [Google Scholar]
- 72.Channappanavar R., Perlman S., Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol 39, 529–539 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sorge R. E. et al. , Different immune cells mediate mechanical pain hypersensitivity in male and female mice. Nat Neurosci 18, 1081–1083 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rosen S. F. et al. , Increased pain sensitivity and decreased opioid analgesia in T-cell-deficient mice and implications for sex differences. Pain 160, 358–366 (2019). [DOI] [PubMed] [Google Scholar]
- 75.Addis R., DeBerry J. J., Aggarwal S., Chronic Pain in HIV. Mol Pain 16, 1744806920927276 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kemp I., Corner E., Colvin L. A., Chronic pain after COVID-19: implications for rehabilitation. Br J Anaesth 125, 436–440 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang T. et al. , Transcriptomic profiling of peripheral blood CD4(+) T-cells in asthmatics with and without depression. Gene 565, 282–287 (2015). [DOI] [PubMed] [Google Scholar]
- 78.Miller H., Depression and immunity: a role for T cells? Brain Behav Immun 24, 1–8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Garber et al. , T cells promote microglia-mediated synaptic elimination and cognitive dysfunction during recovery from neuropathogenic flaviviruses. Nat Neurosci 22, 1276–1288 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sahin U. et al. , COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature 586, 594–599 (2020). [DOI] [PubMed] [Google Scholar]
- 81.Oberhardt V. et al. , Rapid and stable mobilization of CD8(+) T cells by SARS-CoV-2 mRNA vaccine. Nature 597, 268–273 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lai S. et al. , How item banks and their application can influence measurement practice in rehabilitation medicine: a PROMIS fatigue item bank example. Arch Phys Med Rehabil 92, S20–27 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roederer M., Nozzi J. L., Nason M. C., SPICE: exploration and analysis of post-cytometric complex multivariate datasets. Cytometry A 79, 167–174 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Harris P. A. et al. , Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42, 377–381 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.