Abstract
Coronavirus disease 2019 (COVID-19) patients typically present with respiratory symptoms; however, cardiac symptoms, such as pericarditis and pericardial effusion, have also been reported. We report a case of acute pericarditis and pericardial effusion as a delayed complication of COVID-19.
Keywords: COVID-19, cytokine storm, pericardial effusion, pericarditis, SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), has infected >120 million people with >2,800,000 deaths worldwide as of April 2021. COVID-19 patients usually present with symptoms of respiratory infection; however, some patients complain of palpitations and chest tightness. COVID-19 patients with acute myocardial injury, acute pericarditis, and left ventricular dysfunction have been reported.1–3 Herein, we present a case of pericarditis with pericardial effusion as a delayed complication of COVID-19.
CASE PRESENTATION
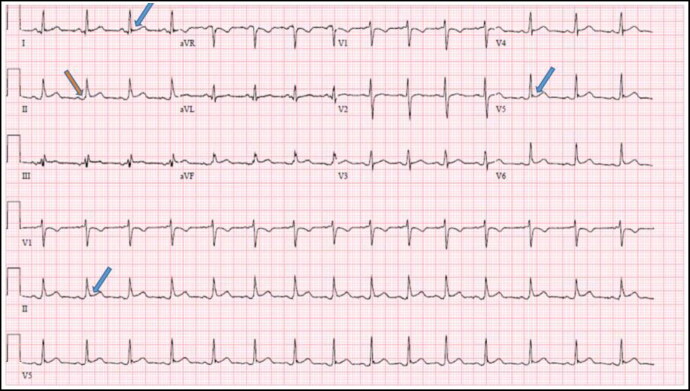
A 30-year-old man presented to our hospital with severe pleuritic chest pain. He had experienced sharp, severe, and progressively worse chest pain for 3 days. The pain worsened with deep inspiration, which produced dyspnea. He had tested positive for COVID-19 6 weeks before presentation, for which he had fever, chills, body aches, cough, and dyspnea. He had self-quarantined for 3 weeks before returning to work. On presentation, he denied fever, chills, and cough, but had dyspnea and chest pain. His vital signs were normal. Electrocardiogram showed normal sinus rhythm with a slight diffuse ST segment elevation (Figure 1). His D-dimer and C-reactive protein levels were elevated at 0.72 μg/mL fibrinogen-equivalent units and 56 mg/L, respectively. The patient was positive for COVID-19 antibodies and COVID-19 positive by polymerase chain reaction. No other coincidental illness or infection was identified. Chest radiograph showed no evidence of acute cardiopulmonary disease. Computed tomographic angiogram of the chest showed moderate pericardial effusion with no pulmonary embolism.
Figure 1.
The patient’s electrocardiogram during admission. Diffuse 1-mm ST-segment elevations (blue arrows) and PR depressions (orange arrow) are suggestive of acute pericarditis.
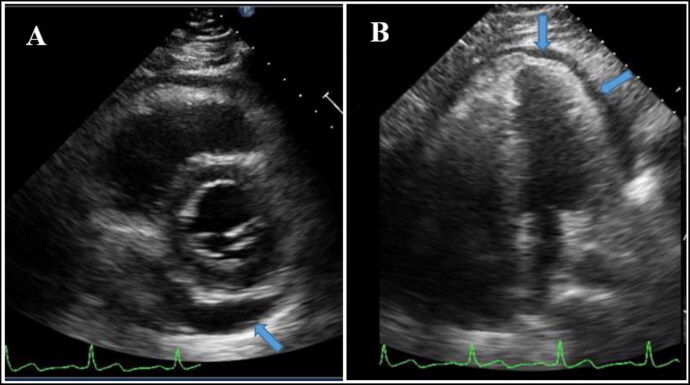
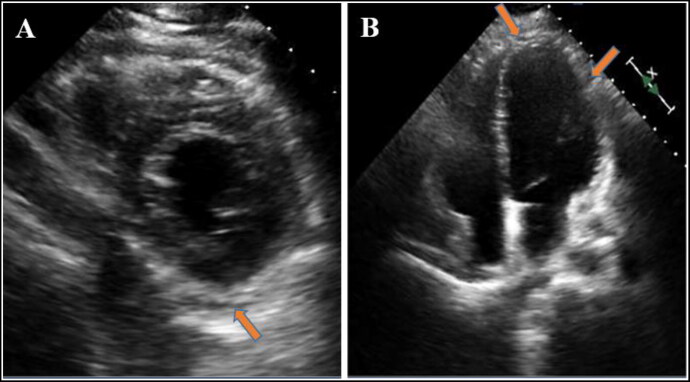
The patient was admitted to the hospital for pericardial effusion and pericarditis. Transthoracic echocardiogram showed a moderate-sized pericardial effusion with no sign of tamponade and a left ventricular ejection fraction of 60% (Figure 2). The patient was treated with colchicine 1 mg twice a day for 1 day as a loading dose and 0.6 mg twice a day for 3 months as a maintenance dose. Within 24 hours, his chest pain resolved. The patient was discharged with instructions to continue taking colchicine 0.6 mg twice a day for 3 months. A repeat transthoracic echocardiogram at 3 weeks showed complete resolution of the pericardial effusion (Figure 3).
Figure 2.
The patient’s echocardiogram during admission in (a) short axis view and (b) four-chamber view showing pericardial effusion (blue arrows).
Figure 3.
The patient’s echocardiogram after treatment with colchicine for 3 weeks in (a) short axis view and (b) four-chamber view showing complete resolution of the pericardial effusion (orange arrows).
DISCUSSION
We described a 30-year-old man who had respiratory symptoms and a positive test for COVID-19 6 weeks before presentation to our hospital for chest pain. We propose that this patient had pericarditis with pericardial effusion as a delayed complication of COVID-19 because he was COVID-19 positive by polymerase chain reaction during admission and no other coincidental illness or infection could have caused his symptoms. There have been reported cases of COVID-19–associated acute pericarditis and pericardial effusion.4–6 In a study of 83 patients with severe and critical COVID-19 infections who underwent a computed tomography scan, 4.8% exhibited pericardial effusion.7 A proposed mechanism by which COVID-19 causes pericarditis and pericardial effusion is inflammation associated with cytokine storm.3,8,9 We suspect that the pericarditis and pericardial effusion observed in this patient was caused by the release of proinflammatory cytokines (e.g., interleukin [IL]-1β, IL-6, IL-8, IL-2 and tumor necrosis factor-α) due to COVID-19. Although we did not capture the level of proinflammatory cytokines, nonspecific markers of inflammation such as D-dimer and C-reactive protein were elevated, suggestive of inflammation.
ACKNOWLEDGMENTS
The authors thank Dr. Leigh Hunter and Anne Murray, PhD, MWC for their editorial help.
References
- 1.Aghagoli G, Gallo Marin B, Soliman LB, Sellke FW.. Cardiac involvement in COVID-19 patients: risk factors, predictors, and complications: a review. J Card Surg. 2020;35(6):1302–1305. doi: 10.1111/jocs.14538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srivastava K.Association between COVID-19 and cardiovascular disease. Int J Cardiol Heart Vasc. 2020;29:100583. doi: 10.1016/j.ijcha.2020.100583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li G, Hu R, Gu X.. A close-up on COVID-19 and cardiovascular diseases. Nutr Metab Cardiovasc Dis. 2020;30(7):1057–1060. doi: 10.1016/j.numecd.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asif T, Kassab K, Iskander F, Alyousef T.. Acute pericarditis and cardiac tamponade in a patient with COVID-19: a therapeutic challenge. Eur J Case Rep Intern Med. 2020;7(6):001701. doi: 10.12890/2020_001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar R, Kumar J, Daly C, Edroos SA.. Acute pericarditis as a primary presentation of COVID-19. BMJ Case Rep. 2020;13(8):e237617. doi: 10.1136/bcr-2020-237617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fox K, Prokup JA, Butson K, Jordan K.. Acute effusive pericarditis: a late complication of COVID-19. Cureus. 2020;12(7):e9074. doi: 10.7759/cureus.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55(6):327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mansouri N, Marjani M, Tabarsi P, von Garnier C, Mansouri D.. Successful treatment of Covid-19 associated cytokine release syndrome with colchicine. A case report and review of literature. Immunol Invest. 2020;1–7. doi: 10.1080/08820139.2020.1789655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang Y, Chen T, Mui D, et al. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020;106(15):1132–1141. doi: 10.1136/heartjnl-2020-317056. [DOI] [PMC free article] [PubMed] [Google Scholar]