Abstract
Skin cancer develops primarily on areas of sun-exposed skin and can typically be treated if caught early. Here, we present a case of a 57-year-old man who presented with an extremely large facial squamous cell carcinoma with resulting perineural invasion and metastasis to parotid lymph nodes because he was unable to obtain timely treatment.
Keywords: Skin cancer, squamous cell carcinoma
Cutaneous squamous cell carcinoma (SCC) is a non-melanoma skin cancer that represents a growing threat to the aging population due to its increasing incidence and metastatic nature. A better understanding of how the disease can progress is important to our understanding of this particular type of skin cancer. This case shows the devastating appearance and effects of facial SCC if left untreated for many years.
CASE DESCRIPTION
A 57-year-old nonsmoking male roofer presented to the emergency department with a progressively enlarging and painful lesion on the right side of the temple that was associated with eye pain, hearing loss, tinnitus, and headache. He first noticed a small plaque in the same area 7 years earlier but didn’t seek treatment. Two days prior to admission, he experienced a syncopal event associated with tunnel vision, lightheadedness, tinnitus, and urinary incontinence. He had taken excessive ibuprofen and smoked marijuana to quell the facial pain and headache prior to the event. Examination revealed a large erythematous and ulcerated lesion with purulent, malodorous discharge and a crusted, irregular border present at the right temple, extending medially toward the lateral canthus (Figure 1). In addition, he had multiple scaly pink macules on the left shoulder, lip, and right ear antihelix. His mental status was intact, visual acuity of the right eye was diminished, and right-sided facial sensation and gross hearing were diminished.
Figure 1.
Erythematous, ulcerated lesion with purulent discharge and an irregular border at the right temple and a right ear antihelix lesion.
Five months earlier, the patient had presented to an outside hospital, at which time biopsy of the lesion revealed moderately differentiated SCC with cystic features involving the dermis. Positron emission tomography/computed tomography (CT) scan at that time showed no regional nodal or distant metastasis. Despite being aware of the diagnosis, the patient was never able to receive treatment due to financial constraints.
Maxillofacial and Neck CT revealed a 4.8 × 4.0 × 1.4 cm lesion that was inseparable from the right lateral orbit rim without underlying bone involvement. There was also an enlarged right submandibular lymph node representing possible metastasis. Magnetic resonance imaging of the brain showed the enhancing right temporal cutaneous lesion with no acute intracranial abnormalities. CT of the chest revealed multiple bilateral pulmonary nodules with no axillary, mediastinal, or hilar lymphadenopathy.
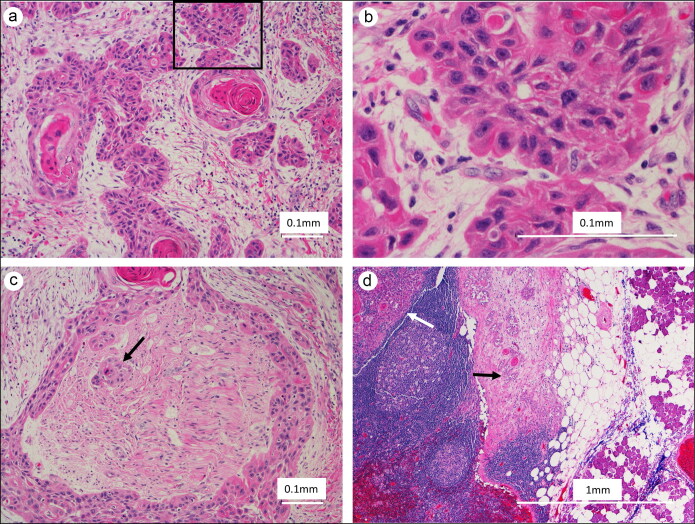
On admission, the patient was started on doxycycline for a potential superimposed infection, as there was purulent discharge. Otolaryngology performed wide local excision of the right temple SCC, right parotidectomy, neck dissection with sacrifice of the frontal branch of the facial nerve, and graft reconstruction of the right lateral canthus. Histopathology results revealed well to moderately differentiated invasive SCC with a depth of invasion of 2.3 cm and presence of perineural invasion (Figure 2). Two of the intraparotid lymph nodes were also positive for metastatic carcinoma (Figure 2). In addition, the right ear antihelix lesion was resected and positive for SCC in situ arising in the background of actinic keratosis. The multidisciplinary tumor board concluded that adjuvant radiation was the next best step in treatment based on the degree of metastasis. The patient recovered well postoperatively and plans to start radiation treatment soon.
Figure 2.
(a) Invasive SCC arranged in irregular nests with keratin pearls in the nest center and stroma that showed desmoplasia. (b) High-power view of the marked field in part a demonstrated the tumor cells with moderate nuclear pleomorphism, hyperchromatic nuclei, occasional prominent nucleoli, dense cytoplasm, and intercellular bridging. (c) The tumor displayed peri- and intraneural invasion involving a larger nerve bundle with an intraneural tumor nest (arrow). (d) There was metastasis into an intraparotid lymph node with tumor nests inside the lymph node (white arrow) and extranodal extension (black arrow). Parotid acini were seen at the right side of the tissue.
DISCUSSION
Cutaneous SCC can be classified as low or high risk.1 High risk features include ≥2 cm in diameter, >2 mm depth of invasion, anatomic location of the face, ear, genitalia, or distal extremities, lack of differentiation, multiple or recurring lesions, perineural invasion, and invasion beyond the subcutaneous fat.1 Our patient, with a history of excessive sun exposure, lesions in multiple sites, moderate differentiation, increased depth of invasion of the tumor, and perineural invasion, was considered high risk. In terms of metastatic SCC, Dacosta Byfield et al found that metastatic disease is more common in men ≥75 years and those who live in the South or Midwest.2 Initially, a lesion may present as a painless plaque, but it can advance to a large, invasive mass.1 The parotid gland, which contains many lymph nodes, is one of the most concerning regions for metastasis.1
Other conditions that can mimic SCC include basal cell carcinoma (BCC), melanoma, and premalignant actinic keratosis. Patients with actinic keratosis are at risk of developing keratinocyte carcinomas (SCC or BCC).3 BCC is the most commonly occurring skin cancer followed by SCC, while melanoma is relatively rare. A comparison of SCC, BCC, and melanoma is shown in Table 1.4,5 Skin biopsy is the gold standard for definitive diagnosis for all types. In our patient, prior biopsy confirmed SCC, with histopathology showing moderately differentiated cystic features involving the dermis. This case is unique in that the patient went many years without treatment and demonstrated the appearance and long-term effects of SCC that ultimately required extensive surgery and postoperative management.
Table 1.
Comparison of non-melanoma and melanoma cancers
| Variable | Keratinocyte (non-melanoma) |
Melanoma | |
|---|---|---|---|
| Squamous cell | Basal cell | ||
| Cell type | Squamous cells | Basal cells | Melanocytes |
| Epidemiology | Elderly men | Elderly men | Aged 20+ men and women |
| Risk factors | UV light exposure, age, lighter skin, immunosuppression, tobacco, albinism, xeroderma pigmentosum | UV light exposure, age, lighter skin, sunburn | UV light exposure, family history, freckles, moles, >5 atypical nevi, age, lighter skin, red hair, tanning bed use |
| Precursor lesion | Actinic keratoses, Bowen's disease (in situ) | De novo | Dysplastic nevi, lentigo maligna |
| Gross appearance | Erythematous, scaly patch or plaque | Pearly nodule or scaly, erythematous, flat lesion | Characterized by ABCDEs (asymmetry, border, color, diameter, evolution), initially horizontal then vertical growth |
| Histopathology | Pleomorphic nuclei, keratinization of the epidermis (in situ) or dermis (invasive) | Basaloid cell nests, peripheral palisading, necrotic keratinocytes, spindle cell stroma | Pathology varies based on subtype |
| Prognosis | Risk of metastasis, mortality > BCC | Low mortality, less likely to metastasize | Most severe, prognosis is proportional to thickness (Breslow's depth) |
| Treatment (depends on metastasis) | Surgery, XRT, chemotherapy | Surgery, cryotherapy, PDT, topicals, chemotherapy | Surgery, XRT, chemotherapy, immunotherapy |
BCC indicates basal cell carcinoma; PDT, photodynamic therapy; UV, ultraviolet; XRT, radiation.
While prognosis is good for small SCC lesions, the prognosis for very large SCC is poor, often due to inoperable metastasis or recurrence of disease. Although SCC is common, treatment depends on the characteristics of the lesion, degree of metastasis, lymph node association, and immunosuppression.1,5 Patients with metastatic SCC who are treated with surgery and radiation have superior outcomes and decreased recurrence compared to those treated with surgery alone.1 This case, with a progressive cutaneous SCC that remained untreated for many years, serves as a reminder of the necessity of treating these lesions early to reduce the potential for metastatic disease and overall mortality.
References
- 1.Burton KA, Ashack KA, Khachemoune A.. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17(5):491–508. doi: 10.1007/s40257-016-0207-3. [DOI] [PubMed] [Google Scholar]
- 2.Dacosta Byfield S, Chen D, Yim YM, Reyes C.. Age distribution of patients with advanced non-melanoma skin cancer in the United States. Arch Dermatol Res. 2013;305(9):845–850. doi: 10.1007/s00403-013-1357-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ehrig T, Cockerell C, Piacquadio D, Dromgoole S.. Actinic keratoses and the incidence of occult squamous cell carcinoma: a clinical-histopathologic correlation. Dermatol Surg. 2006;32(10):1261–1265. doi: 10.1097/00042728-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Diepgen TL, Mahler V.. The epidemiology of skin cancer. Br J Dermatol. 2002; 146(s61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 5.Baldi A, Pasquali P, Spugnini E.. Skin Cancer: A Practical Approach. New York: Springer; 2014: 17–164. [Google Scholar]