Abstract
Proximal pulmonary artery (PA) embolization is a dramatic interventional radiology procedure performed to control recurrent, life-threatening hemoptysis. Distal PA embolization procedures are commonly performed, and preoperative proximal PA embolization procedures have been reported, but to the best of our knowledge there has not been a reported case of a proximal PA embolization to treat hemoptysis. Here, we present a case of a complete proximal PA embolization that effectively resolved recurrent hemoptysis in a patient with a lung tumor following a failed bronchial artery embolization.
Keywords: Embolization, hemoptysis, proximal pulmonary artery
Recurrent hemoptysis occurs in approximately 20% of lung tumor patients, with a 3% incidence of death when hemoptysis is severe.1 Most hemoptysis (>90%) originates from the systemic arteries, with <10% originating from the pulmonary artery (PA).2 The underlying pathology contributing to hemoptysis in lung tumor patients is PA erosion secondary to necrotic tumor processes.3 Currently, bronchial artery embolization is the first-line interventional radiology treatment, with surgical management often used as the definitive treatment in surgical candidates.4 However, in 20% of patients, bleeding will persist after bronchial artery embolization and is associated with high mortality.5 In such cases, PA embolization is indicated to control persistent hemoptysis after bronchial artery embolization5 or in patients with PA erosion.6 Typically, only the segmental or distal branch of the PA contributing to the bleeding is embolized in an attempt to minimize the impact of embolization on pulmonary hemodynamics and maintain perfusion to as much of the lung parenchyma as possible. We present a case of a proximal PA embolization in a lung tumor patient with recurrent hemoptysis after bronchial artery embolization.
CASE PRESENTATION
A 56-year-old Caucasian man with known type 2 diabetes mellitus, mixed hyperlipidemia, and a 55 pack-year smoking history presented to the emergency department with a 2-day history of small-volume hemoptysis, dyspnea, and a 6-month history of an unintentional 10-pound weight loss. He denied previous hemoptysis or dyspnea. The chest radiograph revealed a 15 cm left upper lobe mass suspicious for primary malignancy; computed tomography (CT) angiography with a pulmonary embolism protocol confirmed the mass, showing it encasing the left hilum and narrowing the pulmonary vessels. No signs of metastatic disease were found on CT of the abdomen and pelvis. The patient was treated conservatively, and his hemoptysis spontaneously resolved.
Eight days after discharge, a CT-guided core biopsy of the mass revealed poorly differentiated squamous cell carcinoma of the left upper lobe. The patient was referred to cardiothoracic surgery for a definitive left pneumonectomy. During preoperative workup, coronary CT angiography revealed >80% stenosis of the proximal right coronary artery. The patient was treated with percutaneous intervention and started on 1-month mandatory dual antiplatelet therapy.
Following this, the patient presented to the emergency department five times for recurrent low-volume hemoptysis. His treatments appropriately escalated through an algorithmic approach including iced saline lavage, local epinephrine injection, local thermal ablative therapy, and one targeted fraction of radiation therapy. All of these treatments failed to definitively control his hemoptysis. During his fifth presentation, he developed massive hemoptysis with significant concern for airway compromise. He was emergently intubated in the right mainstem bronchus, dual antiplatelet therapy was paused, and interventional radiology performed embolization of the left lower bronchial artery. However, the patient’s hemoptysis persisted. At this point, a multidisciplinary team determined that a complete left PA embolization was necessary for more definitive control of hemoptysis in anticipation of left pneumonectomy.
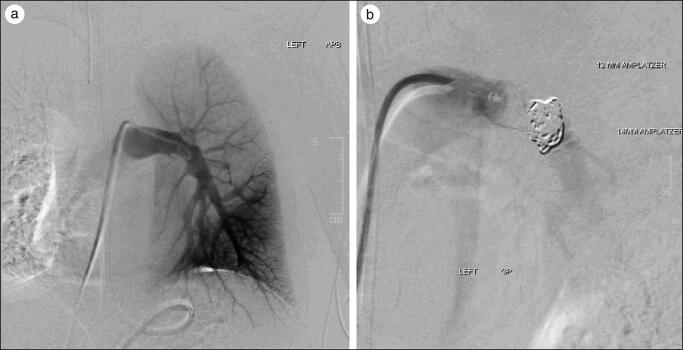
The patient underwent the embolization procedure using one 14 mm and one 12 mm Amplatzer plug followed by four 18 mm × 20 cm Nester coils. His hemoptysis immediately resolved, and postembolization digital subtraction angiogram demonstrated near complete embolization of the proximal left PA with the left PA distal to the embolus significantly decreased in size (4 mm) compared to the same location proximal to embolization (15 mm) (Figure 1).
Figure 1.
Pulmonary artery (PA) digital subtraction angiograms (a) before embolization, showing normal left PA branching anatomy with marked narrowing of the left upper lobe PA just distal to the apical branches secondary to compression from of the large mass, and (b) after embolization, demonstrating embolization of the proximal left PA using a combination of vascular plugs and embolization coils. This image shows some PA opacification distal to the vascular plug; however, the left PA distal to the plug is significantly decreased in size distal to the embolic plug (4 mm) compared to the same location prior to embolization (15 mm) with near complete stasis expected to occur over time.
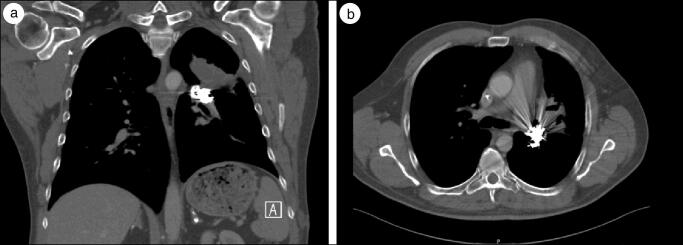
Two weeks later, the patient underwent a left pneumectomy procedure; however, upon initial entry, a pleural mass was identified that was positive for metastatic disease. Due to the confirmed presence of micrometastasis, the patient was no longer deemed a surgical candidate and the pneumonectomy was aborted. However, since the proximal left PA embolization, the patient’s hemoptysis has ceased to return for the entirety of the follow-up period (242 days) (Figure 2).
Figure 2.
CT of the chest 3 months after the pulmonary artery (PA) embolization procedure. (a) Axial image revealing the hyperdense vascular coil plug in the proximal left PA. Also shown are a significant beam hardening artifact from the vascular plug and significantly decreased opacification of the PA system distal to the plug, consistent with near complete embolization. (b) Coronal image with contrast showing the hyperdense coil embolus with significantly decreased opacification of the PA downstream from the plug.
DISCUSSION
The case presented is unique for two reasons. First, the PA supply to the entire left lung was embolized at a proximal location within the left PA, as indicated to control massive life-threatening hemoptysis. This treatment was immediately effective and resolved the hemoptysis for the entirety of the follow-up period without complication (242 days). Second, the patient’s planned pneumectomy was aborted after the proximal PA embolization, and his symptoms resolved without any surgical intervention. Thus, this case demonstrates that in carefully selected conditions, similar to this case, it is feasible and safe to permanently embolize the entire left PA supply to control recurrent hemoptysis without follow-up surgical intervention.
ACKNOWLEDGMENTS
The authors thank Gloria M. Conover, PhD, for providing guidance throughout the writing process.
References
- 1.Gompelmann D, Eberhardt R, Herth FJ.. Advanced malignant lung disease: what the specialist can offer. Respiration. 2011;82(2):111–123. doi: 10.1159/000329703. [DOI] [PubMed] [Google Scholar]
- 2.Khalil A, Fartoukh M, Parrot A, Bazelly B, Marsault C, Carette MF.. Impact of MDCT angiography on the management of patients with hemoptysis. AJR Am J Roentgenol. 2010;195(3):772–778. doi: 10.2214/AJR.09.4161. [DOI] [PubMed] [Google Scholar]
- 3.Khalil A, Parrot A, Fartoukh M, Djibre M, Tassart M, Carette MF.. Pulmonary artery occlusion with ethylene vinyl alcohol copolymer in patients with hemoptysis: initial experience in 12 cases. AJR Am J Roentgenol. 2012;198(1):207–212. doi: 10.2214/AJR.10.5370. [DOI] [PubMed] [Google Scholar]
- 4.Miyano Y, Kanzaki M, Onuki T.. Bronchial artery embolization: first-line option for managing massive hemoptysis. Asian Cardiovasc Thorac Ann. 2017;25(9):618–622. doi: 10.1177/0218492316667231. [DOI] [PubMed] [Google Scholar]
- 5.Marcelin C, Soussan J, Desmots F, et al. Outcomes of pulmonary artery embolization and stent graft placement for the treatment of hemoptysis caused by lung tumors. J Vasc Interv Radiol. 2018;29(7):975–980. doi: 10.1016/j.jvir.2018.01.773. [DOI] [PubMed] [Google Scholar]
- 6.Chun JY, Morgan R, Belli AM.. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010;33(2):240–250. doi: 10.1007/s00270-009-9788-z. [DOI] [PubMed] [Google Scholar]