To the Editor: A 71-year-old male was admitted to the hospital for progressive exertional dyspnea. He had a history of fibrosing mediastinitis (FM)-induced pulmonary vascular stenosis. His right interlobar pulmonary artery had been severely stenosed and implanted with a 6-mm diameter stent (6 mm× 18 mm; PALMAZ®BLUETM, Cordis, Shanghai, China) 6 months before admission, and his left superior pulmonary vein had been implanted with a 9-mm diameter stent (9 mm× 29 mm; ExpressTM Vascular LD, Boston Scientific, Marlborough, MA, USA) 1 month before admission.
After admission, the patient complained of aggravated dyspnea. Physical examinations detected accentuation of the second heart sound at the pulmonary valve auscultation area and right axis deviation. Laboratory tests showed that D-dimer was 0.4 μg/mL, and N-terminal pro B-type natriuretic peptide was 146 pg/mL. Arterial blood gas showed 89.3% of blood oxygen saturation, indicating type I respiratory failure.
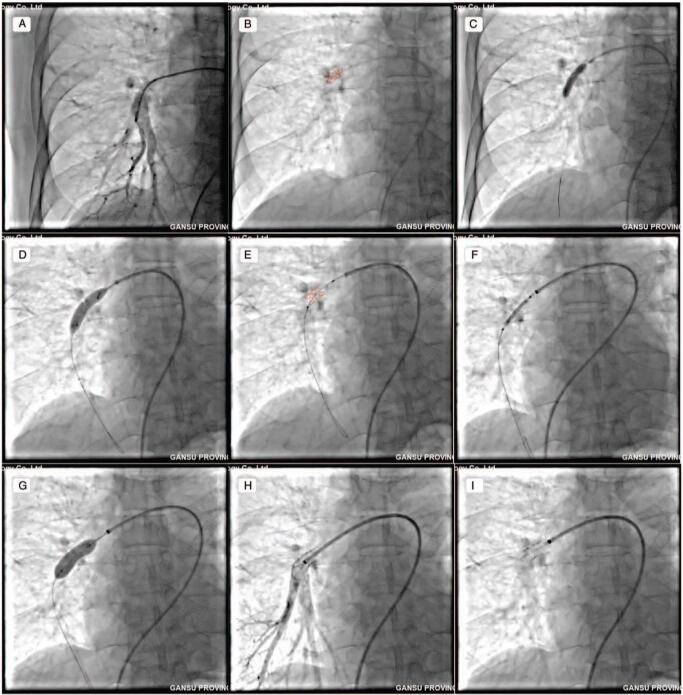
The patient was evaluated as World Health Organization (WHO) functional class III. Computed tomographic pulmonary angiography (CTPA) and selective pulmonary artery/vein angiography revealed intra-stent re-stenosis in the right interlobar pulmonary artery [Figure 1A and 1B]. We consulted with the radiologists in our hospital and analyzed the CTPAs performed before and after the 6-mm diameter stent implantation and then determined that the patient's interlobar pulmonary artery was 10 mm in diameter, and the previously implanted 6-mm diameter stent was under-sized. Subsequently, the 6-mm diameter stent was unzipped using 5 × 30 mm (SterlingTM, Boston Scientific), 7 × 30 mm (SterlingTM, Boston Scientific), and 8 × 30 mm (MUSTANGTM, Boston Scientific) balloons (10–14 atmosphere [atm]) [Figure 1C and 1D]. Pulmonary artery angiography (PAG) showed that the 6-mm diameter stent was completely unzipped [Figure 1E]. Then, a 10 × 25 mm stent (ExpressTM Vascular LD, Boston Scientific) (18 atm) was implanted into the unzipped 6-mm diameter stent [Figure 1F and 1G]. Additional PAG showed that the 10-mm diameter stent was well expanded and that no complications occurred [Figure 1H and 1I].
Figure 1.
PAG and percutaneous transluminal pulmonary angioplasty. (A) Intra-stent re-stenosis in right interlobar pulmonary artery (white arrow). (B) Outline of the 6 mm-diameter stent (red dashed line). (C, D) Unzipping the 6 mm-diameter stent using 5 to 8 mm-diameter balloons. (E) The unzipped stent (red dashed line). (F, G) A 10 mm-diameter stent was implanted. (H, I) The implanted 10 mm-diameter stent was well expanded (white arrow). PAG: Pulmonary artery angiography.
After implantation of the 10-mm diameter stent, the patient's symptoms improved significantly. At 1-year follow-up post-procedure, the patient's functionality improved to WHO functional class I. Six-minute walking distance increased from 272 m upon admission to 365 m at follow-up; mean pulmonary artery pressure, as measured by right heart catheterization, decreased from 41 to 20 mmHg, and tricuspid annular plane systolic excursion increased from 15 to 19 mm during the same time period; CTPA indicated no intra-stent re-stenosis.
FM is a rare fibro-inflammatory disease in the mediastinum.[1] In North America, Histoplasma capsulatum infection is the main cause, whereas tuberculosis infection may be the most prevalent etiology in China.[1] FM often causes symptoms through compressing mediastinal structures. Drug therapy is meant to relieve symptoms but is limited in efficacy.[1] Moreover, the FM-induced mediastinal infiltration of fibrous tissue forms abnormal anatomy, hereby substantially increases the risk of death in surgical treatments.[2] In recent years, percutaneous pulmonary vascular stent implantation has become a new therapeutic modality for FM-induced vascular stenosis.[3] However, implanting a stent appropriate to the diameter of the target vessel is of importance, since an under-sized stent may lead to intra-stent re-stenosis. Unzipping a small-diameter stent has been reported in congenital pulmonary artery stenosis to accommodate body growth in children.[4,5] However, it is not known whether unzipping an under-sized stent in adults under the pathological context of FM-induced pulmonary artery stenosis would be feasible or not, because it is challenging to expand the stenotic pulmonary artery surrounded by fibrous structures. Herein, we report the unzipping of an under-sized stent followed by implantation of another with appropriate size in a senile patient with FM-induced pulmonary artery stenosis, suggesting that unzipping an under-sized stent and implanting a proper-sized one may be safe and feasible to adult patients with FM-induced pulmonary artery stenosis.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (Nos. 81770300, 81860059, 81460072, 82070052), Chinese Academy of Sciences “Light of West China” Program, International Joint Research Program of Gansu Province (No. 18YF1WA046), Innovation and Entrepreneurship Program of Lanzhou City (No. 2018-RC-78), and the Science Foundation of Gansu Provincial Hospital (No. 18GSSY5-4).
Conflicts of interest
None.
Footnotes
How to cite this article: Duan YC, Su HL, Zhu Y, Pan X, Jiang KY, Wang AQ, Qi GM, Zhang Y, Cao YS. Rescue of pulmonary artery intra-stent re-stenosis by unzipping an under-sized stent in an adult patient with fibrosing mediastinitis. Chin Med J 2021;134:1880–1882. doi: 10.1097/CM9.0000000000001493
References
- 1.Cao YS, Duan YC, Su HL. Advances in diagnosis and therapy of pulmonary vascular stenosis induced by fibrosing mediastinitis [in Chinese]. Chin J Cardiol 2020; 48:823–830. doi: 10.3760/cma.j.cn112148-20200214-00081. [DOI] [PubMed] [Google Scholar]
- 2.Mathisen DJ, Grillo HC. Clinical manifestation of mediastinal fibrosis and histoplasmosis. Ann Thorac Surg 1992; 54:1053–1057. doi: 10.1016/0003-4975(92)90069-g. [DOI] [PubMed] [Google Scholar]
- 3.Albers EL, Pugh ME, Hill KD, Wang L, Loyd JE, Doyle TP. Percutaneous vascular stent implantation as treatment for central vascular obstruction due to fibrosing mediastinitis. Circulation 2011; 123:1391–1399. doi: 10.1161/CIRCULATIONAHA.110.949180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sathanandam SK, Kumar TK, Hoskoppal D, Haddad LM, Subramanian S, Sullivan RD, et al. Feasibility and safety of unzipping small diameter stents in the blood vessels of piglets. JACC Cardiovasc Interv 2016; 9:1138–1149. doi: 10.1016/j.jcin.2016.02.035. [DOI] [PubMed] [Google Scholar]
- 5.Morray BH, McElhinney DB, Marshall AC, Porras D. Intentional fracture of maximally dilated balloon-expandable pulmonary artery stents using ultra-high-pressure balloon angioplasty: a preliminary analysis. Circ Cardiovasc Interv 2016; 9:e003281.doi: 10.1161/CIRCINTERVENTIONS.115.003281. [DOI] [PubMed] [Google Scholar]