Background:
To enhance patient safety and prevent medico-legal complaints, we need to understand current trends and impacts. We aimed to characterize Canadian plastic surgery medico-legal patterns in many dimensions.
Method:
This retrospective descriptive analysis of Canadian Medical Protective Association data between January 1, 2013 and December 31, 2017 included closed regulatory body complaints and civil-legal actions involving plastic surgeons. We excluded class action legal cases and hospital complaints. We collected data on patient allegations, procedure types, healthcare-related patient harms, and peer expert criticisms. The primary outcome of interest was physician medico-legal outcome.
Results:
We found 414 cases that met the inclusion criteria: 253 (61.1%) cases involved cosmetic procedures and 161 (38.9%) noncosmetic procedures. The annual incidence among plastic surgeon members of regulatory body complaints and civil-legal actions was 12.1% and 6.7%, for a combined incidence of 18.8%. The most common allegations were deficient clinical assessment, inadequate informed consent, delayed or misdiagnosis, and inadequate monitoring. Leading contributing factors were physician–patient communication breakdown, deficient clinical judgments, and inadequate documentation. The top procedural complications included cosmetic deformity, poor scarring, upper extremity stiffness or deficit, major structural injury, and mental health disorder. Less than half of cases (198/414, 47.8%) had unfavorable medico-legal outcomes for the surgeon. Patients were compensated in 86/198 (43.4%) of civil-legal cases.
Conclusions:
Plastic surgeons experience more medico-legal complaints for cosmetic versus noncosmetic procedures. To minimize medico-legal risks, plastic surgeons should focus on strong physician–patient communication, patient education/consent, thorough clinical assessment, minimizing potentially preventable complications, and maintaining relevant documentation.
INTRODUCTION
Medical malpractice costs more than $55 billion annually to the US healthcare system, about 2.4% of total healthcare spending.1 It is estimated that 75%–99% of US physicians will face medico-legal complaints during their career.2 Although a previous study suggested that Canadian physicians experienced civil-legal actions at a rate of one-fifth as often as their US counterparts,3 recent reports show complaints towards physicians are on the rise in Canada. The Canadian Medical Protective Association (CMPA) reports an 85% increase over the past decade in requests for assistance with medical regulatory body complaints.4,5 Plastic surgery is amongst the top five specialties with the highest medico-legal case incidence.2 Various studies have identified several potential risk factors for medico-legal complaints (eg, inadequate patient selection,6 poor communication, or consent6–8) and unfavorable surgeon medico-legal outcomes (eg, procedure type,7–9 complication profile,1 finding of intraoperative negligence,1 inadequate consent,6–8 incomplete documentation,8 and peer expert criticism8,9).
To enhance quality of care and potentially prevent medico-legal complaints, the current trends of medico-legal complaints and their impact must be described and understood.
Medico-legal complaint data are lacking in the published literature for Canadian plastic surgery.10 It remains unclear if the Canadian medico-legal landscape is similar to its counterparts in the United States and other countries. This study aimed to quantify the incidence of regulatory body complaints and civil-legal actions involving plastic surgeons and describe the reasons for cosmetic and noncosmetic procedure medico-legal complaints.
METHODS
Study Design
University of British Columbia Children’s & Women’s Research Ethics Board (identification number: H19-04052) approval was obtained to conduct this study. The Canadian ethics review panel of the Advarra (formerly Chesapeake) Institutional Review Board (based in Aurora, Ontario and comprising Canadian members) also reviewed and approved the study in compliance with Canada’s Tri-Council Policy Statement on the Ethical Conduct for Research Involving Humans (TCPS 2). A retrospective descriptive analysis of CMPA data between January 1, 2013 and December 31, 2017 was performed. (See appendix, Supplemental Digital Content 1, which displays (A) background on CMPA and the data source (B) definitions. http://links.lww.com/PRSGO/B743.) Closed cases where a plastic surgeon CMPA member contacted the association for assistance with a civil-legal action or a complaint to a regulatory authority (forthwith called College complaints) were eligible for inclusion. (See appendix, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B743.) All cases were closed with the CMPA, where a final medico-legal outcome was determined by the court or regulatory authority, or there was mutual agreement between the parties to resolve the action. Class action legal cases and hospital complaints were excluded to decrease the heterogeneity of the cases reviewed and avoid over-representation of issues.
Variables
We collected data on patient allegations, procedure types, healthcare-related patient harms, and peer expert criticisms. The primary outcome of interest was physician member medico-legal outcomes.
Data Sources
Medical analysts at the CMPA composed of nurses with clinical experience and extensive training in medico-legal research reviewed each case and coded specific clinical details using the Canadian Enhancement to the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada (ICD-10-CA) and the Canadian Classification of Health Interventions (CCI).11 An in-house CMPA coding framework was used to categorize patient safety incidents and the contributing factors (categorized as provider-, team-, or system-related) based on peer expert opinion.12
To reduce the effect of misclassification, regular coding quality assurance reviews were conducted. In addition, severity of patient harm was determined using a modified version of the American Society for Healthcare Risk Management’s Healthcare Associated Preventable Harm Classification.13 We defined patient harm as an outcome that negatively affected the patient’s health and/or quality of life. (See appendix, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B743.) Injury was a specific type of patient harm arising from or associated with plans or actions taken during the provision of healthcare rather than underlying disease or injury.
Statistical Methods
We performed descriptive analyses involving frequencies, proportions, means, SDs, and chi-square test where appropriate. We also performed normality testing on data to determine appropriate statistics to apply. The annual incidence of opened cases was calculated by dividing the case numbers by the number of registered plastic surgeon members. The average annual incidence was then obtained by averaging the incidence across the 5-year study period. Data analyses were conducted with SAS software, version 9.4 (SAS Enterprise Guide software, Version 9.4. Cary, N.C.).
RESULTS
General Medico-legal Trends
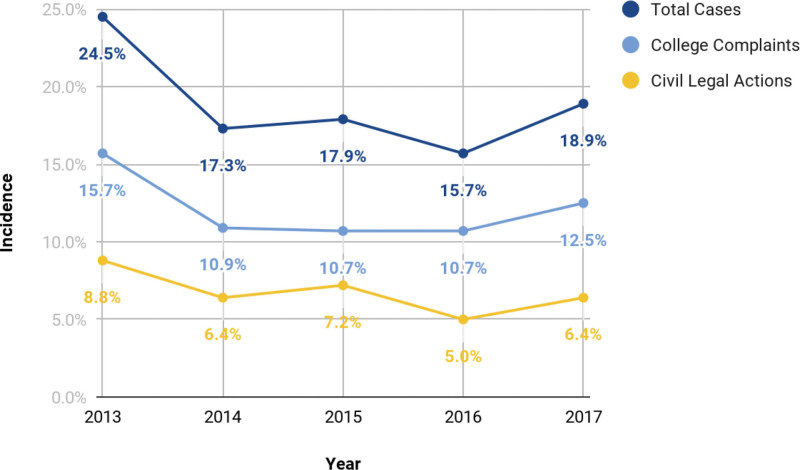
At the end of the study, 582 plastic surgeons were members of the CMPA. In 2020, there were 460 unique plastic surgeon members registered with the Canadian Society of Plastic Surgeons and Canadian Society of Aesthetic Plastic Surgery. This suggests that most actively practicing plastic surgeons were members of the CMPA. Over the 5-year study period, 266 plastic surgeons were involved in medico-legal cases. Break down of the age groups show that 55 (20.7%) were between age 30–39, 81 (30.4%) were between ages 40–49, 78 (29.3%) were between ages 50–59, 38 (14.3%) were between ages 60–69, and 14 (5.3%) were over 70 (Table 1). A total of 414 closed medical-legal cases met the inclusion criteria, comprising 237 (57.2%) civil-legal actions and 177 (42.8%) College complaints. Within the data set of 237 civil-legal action cases, 43 (18.1%) cases proceeded from a College complaint. The average annual incidence for opened civil-legal cases amongst the total number of CMPA plastic surgeon members was 6.7%. The average annual incidence for opened College cases was 12.1%. The overall incidence for open CMPA cases involving plastic surgeons was 18.8% per year. There was a subtle decreasing trend for civil-legal cases and a stable trend for College complaints (Figs. 1, 2). Of all patients involved in closed medico-legal cases, 339 of 414 (81.9%) were female, and the average age was 45 with an SD of 15 years.
Table 1.
Breakdown of Age Ranges of Plastic Surgeons Who Were Involved in a Medico-Legal Case (N = 266)
| Age Range (y) | No. Members |
|---|---|
| 30–39 | 55 (20.7%) |
| 40–49 | 81 (30.4%) |
| 50–59 | 78 (29.3%) |
| 60–69 | 38 (14.3%) |
| 70+ | 14 (5.3%) |
Fig. 1.
Five-year trend of the number of CMPA plastic surgeons, civil-legal action open cases, and College complaint open cases, 2013–2017.
Fig. 2.
Five-year trend of the incidence of CMPA plastic surgeon total open cases, civil-legal action open cases, and College complaint open cases, 2013–2017.
Cosmetic Procedures
Of the included 414 cases, 253 (61.1%) involved cosmetic procedures. The most common procedures were breast augmentation (108/253, 42.7%), abdominoplasty (62/253, 24.5%), and body contouring (55/253, 21.7%). The top three allegations were deficient clinical assessment (92/253, 36.4%), inadequate informed consent process (88/253, 34.7%), and inadequate monitoring or follow-up (32/253, 12.6%). Healthcare-related harm was experienced in 173 of 253 (68.4%) patients. Over half (102/173, 59.0%) of the healthcare-related patient harm was deemed by peer experts to be preventable and 71 of 173 (41.0%) cases were deemed to be an inherent risk of the treatment. The most common reported complications were related to breast deformity or pain (20/127, 5.8%—eg, fat necrosis, mastodynia), poor scarring (19/127, 15.0%—eg, hypertrophic scar), mental health disorders (6/127, 4.7%—eg, adjustment disorder, post-traumatic stress disorder), and eyelid deformity (6/127, 4.7%—eg, ectropion, lagophthalmos). Peer expert opinions were available for 138 of 414 (33.3%) cases. The most common contributing factors identified by peer experts were physician–patient communication breakdown (59/138, 42.8%—eg, inadequate consent process), deficient clinical decision making (51/138, 37.0%), and inadequate documentation (25/138, 14.8%). A total of 127 of 253 (50.2%) cases had unfavorable medico-legal outcomes for the involved surgeon (Table 2).
Table 2.
All Cosmetic Procedure Medico-legal Complaints Compared with Cosmetic Procedures with Unfavorable Medico-legal Outcome for Surgeons
| All Cosmetic Medico-legal Complaints | Cosmetic Medico-legal Complaints with Unfavorable Medico-legal Outcome for Surgeons | ||
|---|---|---|---|
| Top procedures | n = 253 | Top procedures | n = 127 |
| Breast augmentation | 108 (42.7%) | Breast augmentation | 52 (40.9%) |
| Abdominoplasty | 62 (24.5%) | Abdominoplasty | 35 (27.5%) |
| Body contouring | 55 (21.7%) | Body contouring | 22 (17.3%) |
| Top allegations | n = 253 | Top allegations | n = 127 |
| Deficient clinical assessment | 92 (36.4%) | Deficient clinical assessment | 16 (12.6%) |
| Inadequate informed consent | 88 (34.7%) | Inadequate informed consent | 25 (19.7%) |
| Inadequate monitoring | 32 (12.6%) | Inadequate monitoring | <10 |
| Healthcare-related patient harm | n = 253 | Healthcare-related patient harm | n = 127 |
| Any harm | 173 (68.4%) | Any harm | 92 (72.4%) |
| Preventable harm | 102 (40.3%) | Preventable harm | 81 (63.8%) |
| Top contributing factor | n = 138 | Top contributing factor | n = 112 |
| Physician–patient communication | 59 (42.8%) | Physician–patient communication | 52 (46.4%) |
| Deficient clinical decision making | 51 (37.0%) | Deficient clinical decision making | 52 (46.4%) |
| Inadequate documentation | 25 (14.8%) | Inadequate documentation | 18 (16.1%) |
Of the 127 cosmetic cases with unfavorable medico-legal outcomes, the most common procedures were breast augmentation (52/127, 40.9%), abdominoplasty (35/127, 27.5%), and body contouring (22/127, 17.3%). The top allegations were inadequate consent process (25/127, 19.7%) and deficient clinical assessment (16/127, 12.6%). Healthcare-related patient harm was experienced in 92 of 127 (72.4%) patients, 81 of 92 (88.0%) healthcare-related harm cases were deemed preventable, and 11 of 92 (12.0%) were deemed to be an inherent risk of the treatment. Peer expert opinions were available for 112 (88.2%) cases. The most common contributing factors identified were physician–patient communication breakdown (52/112, 46.4%—eg, inadequate consent process), deficient clinical decision making (52/112, 46.4%), and inadequate documentation (18/112, 16.1%) (Table 2).
Amongst cosmetic cases, those with unfavorable medico-legal outcomes for the surgeon had more patient harm that was deemed preventable (81/127, 63.8% versus 102/253, 40.3%) and less cases where poor clinical assessment (16/127, 12.6% versus 92/253, 36.4%) and consent process (25/127, 19.7% versus 88/253, 34.7%) were the reasons for the allegations. The proportion of procedure types, overall harm/complication rate, and types of contributing factors supported by peer expert opinions appeared similar between all cosmetic cases and those with unfavorable medico-legal outcomes for the surgeon (Table 2).
Noncosmetic Procedures
Of the included 414 cases, 161 (38.9%) involved noncosmetic procedures. The most common operations were breast procedures (34/161, 21.1%), hand procedures (26/161, 16.1%), and general reconstructions (16/161, 9.9%). The top three allegations were deficient clinical assessment (55/161, 34.2%), delayed/ missed/ or misdiagnosis (50/161, 31.1%), and inadequate informed consent process (29/161, 18.0%). Healthcare-related harm was experienced in 95 of 161 (59.0%) patients. Almost three-quarters (68/95, 71.6%) of the healthcare-related patient harm was deemed preventable, and 27 of 95 (28.4%) cases were deemed to be an inherent risk of the treatment. The most common reported complications were related to upper extremity stiffness or deformity (9/71, 12.7%—eg, joint stability or arthrosis), injury of major structure (7/71, 9.9%—eg, nerves or bones), malignancy (5/71, 7.0%—eg, melanoma, soft tissue neoplasm). Peer expert opinions were available for 89 (21.5%) cases. The most common contributing factors identified were deficient clinical decision making (37/89, 41.6%), inadequate documentation (27/89, 30.3%), and physician–patient communication breakdown (22/89, 24.7%). In total, 71 of 161 (44.1%) cases had unfavorable medico-legal outcomes for the involved surgeon (Table 3).
Table 3.
All Noncosmetic Procedure Medico-legal Complaints Compared with Noncosmetic Procedures with Unfavorable Medico-legal Outcome for Surgeons
| All Noncosmetic Medico-legal Complaints | Noncosmetic Medico-legal Complaints with Unfavorable Medico-legal Outcome for Surgeons | ||
|---|---|---|---|
| Top procedures | n = 161 | Top procedures | n = 71 |
| Breast | 34 (21.1%) | Breast | 12 (16.9%) |
| Hand | 26 (16.1%) | Hand | 21 (29.6%) |
| General reconstruction | 16 (9.9%) | ||
| Top allegations | n = 161 | Top allegations | n = 71 |
| Deficient clinical assessment | 55 (34.2%) | Deficient clinical assessment | <10 |
| Delayed or misdiagnosis | 50 (31.1%) | Delayed or misdiagnosis | 11(15.5%) |
| Inadequate informed consent | 29 (18.0%) | Inadequate informed consent | <10 |
| Healthcare-related patient harm | n = 161 | Healthcare-related patient harm | n = 71 |
| Any harm | 95 (59.0%) | Any harm | 53 (74.6%) |
| Preventable harm | 68 (42.2%) | Preventable harm | ≥44 (62.0%) |
| Top contributing factor | n = 89 | Top contributing factor | n = 68 |
| Deficient clinical decision making | 37 (41.6%) | Deficient clinical decision making | 27 (39.7%) |
| Inadequate documentation | 27 (30.3%) | Inadequate documentation | 20 (29.4%) |
| Physician–patient communication | 22 (24.7%) | Physician–patient communication | 21 (30.9%) |
Of the 71 noncosmetic cases with unfavorable medico-legal outcomes for the surgeon, the most common procedures were hand procedures (21/71, 29.6%) and breast procedures (12/71, 16.9%). The top allegation was related to diagnostic error (11/71, 15.5%). Healthcare-related harm was experienced in 53 of 71 (74.6%) patients. Most of the healthcare-related patient harm was deemed preventable, and less than 10 cases were deemed to be an inherent risk of the treatment and therefore not included in the classification. Peer expert opinions were available for 68 of 71 (95.8%) cases. The most common contributing factors identified were deficient clinical decision making (27/68, 39.7%—eg, deficient assessment, failure to perform test/intervention), physician–patient communication breakdown (21/68, 30.9%), and inadequate documentation (20/68, 29.4%) (Table 3).
Amongst noncosmetic cases, those with unfavorable medico-legal outcomes for the surgeon occurred more in hand procedures (21/71, 29.6% versus 26/161, 16.1%), had more healthcare-related patient harm/complications (53/71, 74.6% versus 95/161, 59.0%), more healthcare-related patient harm that was deemed preventable (44/71, 62.0% versus 68/161, 42.2%), and less diagnostic error as the reason for allegation (11/71, 15.5% versus 50/161, 31.1%). The proportion of breast procedures and types of contributing factors outlined by peer expert opinions appeared similar between all noncosmetic cases and those with unfavorable medico-legal outcome for the surgeon (Table 3).
Complications in Cases with Unfavorable Medico-legal Outcomes for the Surgeons
The number of complications was insufficient to perform meaningful analysis when separated into unfavorable cosmetic and noncosmetic cases. When combined, a total of 145 patients experienced healthcare-related patient harm. The most common complications in unfavorable medico-legal outcome cases for surgeons among cosmetic and noncosmetic cases were poor scarring (24/145, 16.6%), breast deformity/ pain (23/145, 15.9%), and mental health disorders (10/145, 6.9%). The percentage of cases with poor scarring, breast deformity/ pain, and mental health disorders appeared similar between all medico-legal cases and those with unfavorable medico-legal outcomes for surgeons (Table 4).
Table 4.
All Complications Compared with Those with Unfavorable Medico-legal Outcome for Surgeons
| All Medico-legal Complaints | Medico-legal Complaints with Unfavorable Medico-legal Outcome for Surgeons | ||
|---|---|---|---|
| Complications | n = 268 | Complications | n = 145 |
| Poor scar | 31 (11.5%) | Poor scar | 24 (16.6%) |
| Breast deformity/pain | 30 (11.2%) | Breast deformity/pain | 23 (15.8%) |
| Mental health disorder | 12 (4.5%) | Mental health disorder | 10 (6.9%) |
DISCUSSION
We found medico-legal complaints to be high amongst plastic surgeon CMPA members. The annual incidence of College complaint and civil-legal action was 12% and 7% respectively, and for a total incidence of 19%, implying almost one newly opened case for every five CMPA plastic surgeon members per year. There appears to be a subtle decreasing trend for civil-legal actions and a stable trend for complaints through the regulatory bodies. The majority of involved patients were female and less than 50 years old. The majority of complaints (253/414, 61%) were regarding cosmetic procedures. Given that a lower number of cosmetic procedures are performed annually than noncosmetic procedures,14,15 the actual incidence of medico-legal complaints surrounding cosmetic procedures may be higher.
Cosmetic versus Noncosmetic Procedures
For cosmetic procedures, there was a greater complaint focus on inadequate informed consent process and physician–patient communication breakdown. Mavroforou et al also report reaching a similar conclusion after their review of literature.6 In comparison, noncosmetic cases had a greater focus on delayed or misdiagnosis and deficient clinical decision making. Inadequate documentation was identified to be an important factor for both cosmetic and noncosmetic procedures. The top cosmetic procedure types involved in complaints appeared to be concentrated in breast augmentation (43%), abdominoplasty (25%), and body contouring (22%). In comparison, American Society of Plastic Surgeons data shows that breast augmentation (16%), abdominoplasty (7%), and body contouring (15%) make up a much smaller proportion of total cosmetic procedures performed annually.14 Top complaints for noncosmetic procedures were centered around breast (21%) and hand (16%) procedures. In contrast, the total proportion of annually performed breast (3%) and hand (2%) cases lag behind tumor removal, laceration repair, maxillofacial surgery, and scar revision.15 This concentration of complaints around breast and hand procedures may be attributed to the greater cosmetic expectation, functional demand, and procedure complexity associated with breast and hand operations. Top cosmetic procedure complications were focused around cosmetic deformity, pain, and mental health disorders. Meanwhile top noncosmetic procedure complications were centered around functional impairments—upper extremity stiffness or disability, major structure injury, and delay or misdiagnosis of malignancy.
Cases with Unfavorable Medico-legal Outcomes for Surgeons
Healthcare-related patient harm was identified in the majority of complaints. Occurrence of preventable harm was more frequent among cases of unfavorable medico-legal outcome for the involved surgeon. Kandinov et al reported similar findings in rhytidectomy, where the presence of intraoperative negligence and preventable facial nerve injuries were associated with poorer medico-legal surgeon outcome.1 In our study, procedure type did not differ among varying medico-legal outcomes for cosmetic procedures. However, for noncosmetic procedures, hand related complaints were more frequent among cases with unfavorable medico-legal outcomes for surgeons. This may be related to the greater focus on functional deficit encountered in noncosmetic procedure complications.
International Perspective
Our study found that when the civil-legal cases were contrasted with available data from the United States, Canadian plastic surgeons face lower incidence (7%) when compared with their American colleagues (13%).6 We found that 48% of Canadian plastic surgery civil-legal cases had unfavorable medico-legal outcomes for the surgeon and patients were compensated in 42% of cases. In comparison, Therattil et al and Sarmiento et al reported that 35%–40% of US plastic surgery malpractice litigation cases had unfavorable medico-legal outcomes for involved surgeons.9,16 States with weak tort reform were found to have a greater number of litigation cases.9 Their patient demographics, proportion of surgery types, and complication profile appeared similar to our data.9,16 Similarly for facial rhytidectomy, Kandinov et al reported unfavorable medico-legal outcomes for US plastic surgeons in 40% of cases. A recent survey of UK plastic surgeons revealed that all respondents had experienced either medico-legal claims or were paying increasing indemnity costs over the last 5 years from the time of survey. The vast majority (89%) of claims were settled out of court. Of those that went to court, in nearly all cases, legal fees exceeded the claimant’s settlement fee.17 Review of plastic surgery related medico-legal complaints in Brazil from 2004 to 2008 revealed findings similar to those of our study: the greatest proportion of cases involved cosmetic surgery. In addition, this study described an increasing trend of complaint incidence and expense costs.18 Park et al found Korean aesthetic surgery patients involved in litigation cases had similar demographics compared with that of our patients but reported a greater proportion of facial aesthetic surgeries.7 Given the vast complexity and differences that exist between various countries’ medico-legal system, direct comparisons of outcomes are challenging and should not be interpreted based on numerical values alone (Table 5).
Table 5.
Comparison of Plastic Surgery Medico-legal Trends between Countries
| Canada | United States | Korea | Australia | |
|---|---|---|---|---|
| Incidence (civil-legal) | 6.7% | 13%6 | — | — |
| Patient demographics | Mean age: 39 | Mean age: 4216 | Mean age: 337 | Median age: 4219 |
| Female: 81% | Female: 89%16 | Female: 91%7 | Female: 88% | |
| Cosmetic (%) | 61% | 74%16 | 100%*7 | 100%* |
| Unfavorable outcome | 48% | 40%16 | 91%7 | 42% |
*Only aesthetic procedures were reviewed.
Reducing Risk of Medico-legal Complaint
To minimize medico-legal risk in cosmetic surgery, plastic surgeons should focus on having appropriate patient selection, developing strong physician–patient relationships, and ensuring comprehensive informed consent. Certain cosmetic procedures (breast augmentation, abdominoplasty and body contouring procedures) were associated with higher medico-legal risks when compared with their volumes. For noncosmetic surgeries, plastic surgeons should focus on performing thorough workups and follow-ups where necessary to avoid delay or misdiagnosis. Hand surgery seemed disproportionately represented, and patients may benefit from a more thorough informed consent process and management of expectations. Based on average patient age, sex, and cases that result in unfavorable medico-legal outcomes for the CMPA member, an argument can be made for “lifestyle” related procedures and those associated with improving quality of life both functionally and aesthetically being of higher risk. Finally, detailed documentation, surgeon availability, and appropriate communication should be maintained to further reduce medico-legal risk.
Strengths and Limitations
This is the first known published study reviewing the medico-legal trends in Canadian plastic surgery. At the time of the study, the CMPA represented over 95% of physicians in Canada.3 Given this national sample, our study is a highly representative view of the current plastic surgery medico-legal landscape in Canada. This study is, however, limited by its retrospective design, small overall case volumes as a proportion of overall surgical cases completed, and inclusion of only closed cases. Physicians voluntarily request medico-legal assistance from the CMPA; therefore, the sample likely remains an underrepresentation of all medico-legal cases despite high Canadian physician enrollment in CMPA memberships. While CMPA employed an internally standardized criteria for civil-legal action case outcomes, medico-legal outcome is not standardized within and in between study comparisons. Finally, differences exist between College complaint protection due to regional variations and standards.
CONCLUSIONS
This is the first report describing the medico-legal landscape in Canadian plastic surgery. On average, almost one in five Canadian plastic surgeons faced a newly opened medico-legal case per year. Plastic surgeons experienced more medico-legal complaints related to cosmetic versus noncosmetic procedures. Certain procedures aimed at aesthetic and functional improvements were disproportionately featured in our sample of medico-legal cases. To minimize medico-legal risks, plastic surgeons should focus on strong physician–patient communication, including informed consent, thorough clinical assessments, and maintaining relevant documentation.
Supplementary Material
Footnotes
Published online 13 August 2021.
Presented at the 2021 Canadian Society of Plastic Surgery Annual Meeting [online], June 14, 17, and 21, 2021.
Disclosure: Dr. Calder, Ms. Finestone, and Mr. Liu were employees of the CMPA, a not-for-profit mutual defence organization for physicians, at the time of this study. All the other authors have no financial interest to declare in relation to the content of this manuscript.This study was internally funded by The Canadian Medical Protective Association.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Kandinov A, Mutchnick S, Nangia V, et al. Analysis of factors associated with rhytidectomy malpractice litigation cases. JAMA Facial Plast Surg. 2017;19:255–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeVille K, Goldberg D, Hassler G. Malpractice risk according to physician specialty. N Engl J Med. 2011;365:1939. [DOI] [PubMed] [Google Scholar]
- 3.Coyte PC, Dewees DN, Trebilcock MJ. Medical malpractice—the Canadian experience. N Engl J Med. 1991;324:89–93. [DOI] [PubMed] [Google Scholar]
- 4.Vogel L. Patient complaints about Canadian doctors on the rise. CMAJ. 2018;190:E408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogel L. Growing number of medical trainees named in complaints. CMAJ. 2019;191:E717–E718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mavroforou A, Giannoukas A, Michalodimitrakis E. Medical litigation in cosmetic plastic surgery. Med Law. 2004;23:479–488. [PubMed] [Google Scholar]
- 7.Park BY, Kwon J, Kang SR, et al. Informed consent as a litigation strategy in the field of aesthetic surgery: an analysis based on court precedents. Arch Plast Surg. 2016;43:402–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vila-Nova da Silva DB, Nahas FX, Ferreira LM. Factors influencing judicial decisions on medical disputes in plastic surgery. Aesthet Surg J. 2015;35:477–483. [DOI] [PubMed] [Google Scholar]
- 9.Therattil PJ, Chung S, Sood A, et al. An analysis of malpractice litigation and expert witnesses in plastic surgery. Eplasty. 2017;17:e30. [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Shaqsi S, Hong B, Austin RE, et al. Practice management knowledge amongst plastic surgery residents in Canada: a national survey. Aesthet Surg J Open Forum. 2020;2:ojaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. 5th ed. France: World Health Organization; 2016. [Google Scholar]
- 12.McCleery A, Devenny K, Ogilby C, et al. Using medicolegal data to support safe medical care: a contributing factor coding framework. J Healthc Risk Manag. 2019;38:11–18. [DOI] [PubMed] [Google Scholar]
- 13.Hoppes M, Mitchell JL, Venditti EG, et al. Serious safety events: Getting to Zero. J Healthc Risk Manag. 2013;32:27–45. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Plastic Surgeons. Cosmetic procedure trends. In: Plastic Surgery Statistic Report 2019. Arlington Heights, Ill: American Society of Plastic Surgeons; 2020. Available at https://www.plasticsurgery.org/documents/News/Statistics/2019/cosmetic-procedure-trends-2019.pdf. Accessed August 3, 2020. [Google Scholar]
- 15.American Society of Plastic Surgeons. Reconstructive procedure trends. In: Plastic Surgery Statistic Report 2019. Arlington Heights, Ill: American Society of Plastic Surgeons; 2020. Available at https://www.plasticsurgery.org/documents/News/Statistics/2019/reconstructive-procedure-trends-2019.pdf. Accessed August 3, 2020. [Google Scholar]
- 16.Sarmiento S, Wen C, Cheah MA, et al. Malpractice litigation in plastic surgery: can we identify patterns? Aesthet Surg J. 2020;40:NP394–NP401. [DOI] [PubMed] [Google Scholar]
- 17.Rahman SM, Cooper L, Thomson D, et al. Quantifying the burden of litigation in UK plastic surgery: a national survey. J Plast Reconstr Aesthet Surg. 2019;72:1436–1447. [DOI] [PubMed] [Google Scholar]
- 18.da Silva DB, Nahas FX, Bussolaro RA, et al. The increasing growth of plastic surgery lawsuits in Brazil. Aesthetic Plast Surg. 2010;34:541–542. [DOI] [PubMed] [Google Scholar]
- 19.Bismark MM, Gogos AJ, McCombe D, et al. Legal disputes over informed consent for cosmetic procedures: a descriptive study of negligence claims and complaints in Australia. J Plast Reconstr Aesthet Surg. 2012;65:1506–1512. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.