Abstract
We performed full circumferential imaging of the Schlemm’s canal (SC) of two human eyes using a Fourier domain mode-lock laser (FDML) based 1.66-MHz SS-OCT prototype at 1060 nm. Eight volumes with overlapping margins were acquired around the limbal area with customized raster scanning patterns designed to fully cover the SC while minimizing motion artifacts. The SC was segmented from the volumes using a semi-automated active contour segmentation algorithm, whose mean dice similarity coefficient was 0.76 compared to the manual segmentation results. We also reconstructed three-dimensional (3D) renderings of the 360° SC by stitching the segmented SCs from the volumetric datasets. Quantitative metrics of the full circumferential SC were provided, including the mean and standard deviation (SD) of the cross-sectional area (CSA), the maximum CSA, the minimum and maximum SC opening width, and the number of collector channels (CC) stemming from the SC.
1. Introduction
The accurate assessment of the ocular anterior chamber is an important part of routine clinical evaluation of the eye [1,2]. Imaging structures within the anterior chamber angle is important for accurate anatomical assessment of the aqueous outflow system in glaucoma and the diagnosis of angle closure glaucoma [3,4]. The intraocular pressure (IOP) of an eye is maintained as aqueous humor produced from the ciliary body is drained from the anterior chamber of the eye to the intrascleral and episcleral veins via the Schlemm’s canal (SC), a ring-shaped structure encircling the eye within the anterior chamber angle [5]. Morphological abnormalities of SC, such as narrowing or progressive collapse, have been reported in the presence of elevated IOP [6–10]. In addition, morphological changes in SC were correlated to the onset of primary open angle glaucoma (POAG) [10–13]. Studies have further indicated that the dimensions of SC may vary along the circumferential direction even in normal eyes [9–11,14–17]. Previous in vivo studies have performed the morphological analysis of SC, although the imaging was limited to small sections of the entire canal. A visualization as well as morphological analysis of the entire 360° circumference of SC in three-dimensional (3D) is therefore vital, as it may shed light on its effect on the outflow resistance.
Optical coherence tomography (OCT) is a non-invasive imaging technique that offers high-resolution, 3D visualization of the biological tissue [18]. Studies have reported on in vivo SC imaging using OCT [9,11,15–17,19–22], most of which used the spectral-domain (SD) OCT to measure the cross-sectional dimensions of SC at nasal and/or temporal quadrants. Leung and Weinreb [23] suggested that, compared to the near-infrared (NIR) window at 1300 nm, spectral-domain (SD) OCT systems at shorter NIR wavelength (800 nm ∼ 900 nm) provide better visualization of SC due to higher axial resolution and stronger photon backscattering from the tissue. However, the SC was seen at a various depth from 0.6 mm to 1.1 mm under the limbus in human eyes [11,18–22]. The photons at shorter wavelengths may experience stronger scattering loss when travelling through the tissue, resulting in reduced signal strength at the deep iridocorneal angle recess. It becomes even more challenging in the presence of the intrascleral and episcleral vessels as well as dark pigmentation in the limbus and conjunctiva that may hinder deeper light penetration [24,25]. Without clear delineation of the iridocorneal angle, it increases the difficulty in the identification and segmentation of SC in OCT B-scans [26]. Moreover, SD-OCT systems inevitably suffer from a sensitivity roll-off effect where the signal-to-noise ratio (SNR) gradually reduces along the depth, limiting the imaging depth to 1–2 mm. Although the use of an enhanced depth imaging (EDI) technique in SD-OCT can mediate this roll-off effect, it reduces the overall SNR and cannot overcome the fundamental limitation imposed by the imaging wavelength [27]. Last but not the least, most of commercial SD-OCT systems at 800 nm have limited A-scan speed (in the range of 20–70 kHz). At this speed, the volumetric imaging of SC structures is undermined by motion artifacts. Kagemann et al. [17,20] first attempted 3D rendering of SC in human eyes using two different SD-OCT machines. This was limited to SC segments of 4 mm in length at the nasal and temporal quadrants. More recently, Huang et al. demonstrated the 360° 3D reconstruction of SC in one eye of a healthy volunteer using a commercial SD-OCT instrument with an active eye tracker to compensate motion artifacts [28]. Forty volumes were taken around the limbal area of one eye, with SC in each frame automatically segmented and stitched together. The whole imaging session took two days to complete, making it impractical to implement in regular clinical settings. On the contrary, the swept source (SS) OCT systems can overcome the prolonged scanning duration because of the higher acquisition speed. SS-OCT generally has longer imaging depth (> 2 mm) with a mitigated sensitivity roll-off effect, making it more suitable for deep tissue imaging. The longer wavelength window of SS lasers (1060 nm) allows for deeper light penetration and reduces shadowing artifacts caused by the epi/intra-scleral vessels, both of which are essential for angle delineation and SC imaging. Although the axial resolution of SS-OCT is slightly inferior to its SD-OCT counterpart, and studies have shown good agreement in SC dimension measurements between SS- and SD-OCT [17,21,22].
In this study, we demonstrate a 360° circumferential imaging of SC with SS-OCT in two normal human eyes. A motion-free 3D imaging over a larger extent is possible due to a higher A-line speed enabled by the megahertz sweep rate of SS-OCT systems using a Fourier domain mode-locked (FDML) laser. This ultra-high speed has enabled unprecedented ultra-wide-field retinal imaging with FDML SS-OCT systems without the use of an eye tracker [29,30]. The 1060 nm system offers similar penetration depth but at a higher axial resolution and higher image contrast compared to 1300 nm SS-OCT [23,18]. We also propose an imaging protocol that allows for efficient image acquisition of the 360° SC and develop a semi-automatic active contour segmentation method to delineate SC from the OCT B-scans. 3D reconstruction of the entire SC of both eyes is achieved by stitching the segmented SC from each of the eight positions. The quantitative metrics, including the mean and maximum cross-sectional area (CSA) of SC, the maximum and minimum of SC opening width, and the number of collector channels (CCs) are provided, showing good agreement with previous reports. To our best of our knowledge, this is the first endeavor to incorporate MHz SS-OCT in SC imaging, which may provide a more holistic evaluation of the SC and better evaluate this structure of aqueous outflow in conditions such as glaucoma.
2. Method
2.1. MHz SS-OCT system for Schlemm’s canal imaging
A schematic of the MHz SS-OCT system (Optores, Munich, Germany) is presented in Fig. 1. The details of the system can be found elsewhere [30]. In summary, the source of the system is an FDML laser (Optores, Munich, Germany) operated at 1.66 MHz A-line rate, centered at 1061 nm and sweeping over a bandwidth of 75 nm. The input power is split into three portions: sample arm, reference arm, and recalibration arm. The signal combined from the recalibration and reference arms generates a monotonic interferogram for accurate linear-k resampling, while the sample arm and reference arm create the OCT interferometer for imaging. An electrical shutter was placed in the recalibration arm and was open only during the acquisition of calibration signal. A dual-channel balanced photodetector (WL-BPD1GA, Wieserlabs, Munich, Germany) as well as a PCIe based digitizer (ATS9373, Alazar Technologies Inc., Montreal, Canada) was employed for OCT signal detection and digitization. The prototype system was originally designed for wide-field retinal imaging. An achromatic lens (f = 30 mm, Thorlabs, Newton, NJ, USA) was thus added to the system right after the pivotal point to act as an anterior segment imaging lens allowing for Schlemm’s canal imaging. The focal length was chosen under the constriction posed by the mechanical travel range of the reference arm. The theoretical axial resolution of the system was estimated as 6.5 µm in air. The digitizer worked at 3.68 GS/s, sampling 2304 points for each sweep cycle. The imaging range was 4.2 mm, and the 6-dB fall-off range tested greater than 6 mm. The lateral resolution was measured to be 17.54 µm using a USAF resolution target (Thorlabs, Newton, NJ, USA).
Fig. 1.
Schematic of the MHz SS-OCT. ACL: achromatic lens, FC: fiber coupler, M: mirror, RFM: retroreflector mirror, GS: galvo scanner, SPDM: short-pass dichroic mirror, L: lens. Inset: Illustration of the imaging protocol: volumes taken at the cardinal positions marked as red boxes and those at the intercardinal positions as yellow boxes, and the fast scan directions indicated by arrows. Note that the patient will look sideways during imaging.
2.2. Imaging protocol
Two healthy female volunteers aged between 30 to 40 years with no known ocular and systemic diseases were recruited in this study, and one eye of each subject was randomly chosen to undergo OCT imaging. As shown in the inset of Fig. 1, for each eye, eight volumetric scans were acquired around the limbus, with each located at one of the cardinal (temporal, nasal, superior, inferior) or intercardinal positions (temporosuperior (TS), temporoinferior (TI), nasosuperior (NS), nasoinferior (NI)) to fully cover the SC encircling the cornea. An external fixation target was introduced to ensure normal incidence at the corneal surface above the SC at each of the eight positions.
At each of the four cardinal positions, each volume consisted of 2000 A-scans in the fast scan direction and 600 B-scans in the slow scan direction, covering 9 mm and 4.5 mm, respectively. The fast scan direction at each of the cardinal positions was aligned with the longitudinal direction of the SC, indicated in the inset of Fig. 1 as red arrows. At the other four intercardinal positions, each volume consisted of 1200 A-scans in the fast scan direction and 1200 B-scans in the slow scan direction, covering 9 mm and 5 mm, respectively. The fast scan direction was chosen to be vertical. The scan patterns at the respective scan positions were determined based on (1) the maximal coverage of SC, (2) the additional area of coverage that was required for manual stitching, (3) the minimal scan duration, and (4) the Nyquist sampling theorem. Each volume required around 1 second to acquire, and in total it took less than 30 minutes to complete the full circumferential imaging for one eye. Multiple volumes were taken at each of the positions, and quality check was performed to select the volume with the highest SC visibility for image processing.
2.3. Data preparation, imaging processing, and 3D rendering
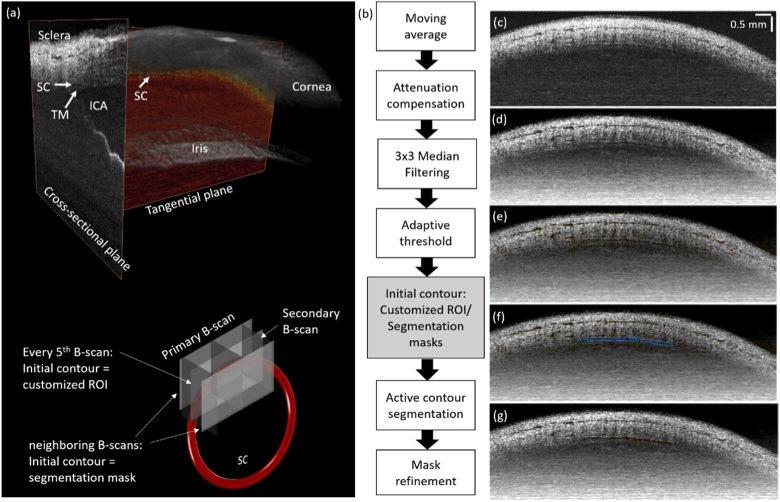
OCT intensity images were generated from the raw data following standard processing steps, including linear-k interpolation, dispersion compensation, inverse Fourier transform, logarithmic scaling and contrast adjustment, using a stand-alone software offered by the prototype manufacturer. The linear-k interpolation was based on the phase extracted from the calibration signal acquired separately before volumetric acquisition. This recalibration signal was taken whenever necessary for accurate linear-k interpolation. The generated OCT intensity images were resampled to isotropic voxel size of 7.5 µm × 7.5 µm × 7.5 µm. A representative OCT volume taken at one of the cardinal positions is presented in Fig. 2(a) (See Visualization 1 (8MB, mp4) ). The primary B-scans under the current protocol are aligned with the tangential plane of SC, while the re-sliced secondary B-scans can be recognized as the conventional cross-sectional SC images. The anatomical landmarks, including SC, sclera, cornea, iris, iridocorneal angle, and trabecular network, are annotated. In the primary B-scans, the SC appears as a continuous tube-like structure proximal to the iris [31]. For volumes taken at the intercardinal positions, however, they were rearranged (rotated and re-sliced) so that the reconstructed primary B-scans were aligned to the tangential plane of the SC, referring to Fig. 2(a). Next, primary B-scans that manifested the presence of SC were manually selected for segmentation. Under this imaging protocol, each volume scan produces around 120 images with clear SC delineation. The data preparation process was done using ImageJ (NIH, Bethesda, MD, USA).
Fig. 2.
(a) Three-dimensional illustration of an OCT volumes taken at the cardinal position, with anatomical landmarks annotated. (See Visualization 1 (8MB, mp4) ) TM: trabecular meshwork; ICA: irido-corneal angle. Bottom: an illustration of the B-scans in an OCT volume with respect to the SC, and the initial contour definition for different primary B-scans. (b) Flowchart of the SC segmentation process. (c) – (g) Images generated from the steps of the flow chart. At every five B-scans in each volume, customized ROI was used for initial contour generation. The segmentation results of these B-scans were then employed for the neighboring B-scans for initial contour generation.
A semi-automatic image segmentation method was developed for delineation of SC from the prepared datasets. The flowchart is presented in Fig. 2(b), and an example of the original OCT B-scan in Fig. 2(c). At first, a three-by-three sliding window was applied across the entire OCT intensity volume for A-line smoothing. An attenuation compensation method [32] was adopted, and the original pixel intensity was converted to
where N is the index of the last pixel. The attenuation corrected B-scans underwent a 3-by-3 median filtering process to reduce the speckle noise (Fig. 2(d)). Next, binarized masks were generated by using a locally adaptive threshold with a sensitivity factor of 0.9 (Fig. 2(e)) [33], and the SC region was segmented by the active contour technique with a pre-defined initial contour and 10 iterations [34]. For every fifth B-scan in the prepared datasets, the initial contour was created by manually refining the binarized masks from thresholding, as shown in Fig. 2(f). For the other B-scans, however, the initial contours were generated based on the SC segmentation results of their closest neighboring B-scans processed by performing morphological dilation using a rectangular kernel of 5 pixels in width and 3 pixels in height. After the active contour segmentation, the resultant masks were eroded by a disk kernel (size = 2 pixels), followed by a 1-pixel morphological closing step (Fig. 2(g)). Finally, the 3D segmentation results were presented in the secondary B-scans, each of which underwent a morphological refinement process to fill the small gaps and remove isolated areas with less than 50 pixels. Segments at the edges of each volume showing low image quality, such as low images sharpness and low contrast, were excluded from the volumes for stitching and quantification. Image processing steps were done by using a customized software written in MATLAB (MathWorks, Natick, MA, USA). Visualization of OCT volumes as well as SC segmentation results was fulfilled using Amira (Thermo Fisher Scientific, Waltham, MA, USA).
After segmentation was completed, the segmented SCs were manually stitched by referring to the episcleral vessels and Palisades of Vogt shown in en face projection of each volume, as well as the common landmarks, such as intra-scleral vascular structures, shown in the secondary B-scans shared by two overlapping volumes. For 3D presentation of the 360° SC, each secondary B-scan as well as the corresponding SC segmentation mask was rotated so that the iris structure was flat. The SC masks were then aligned by using rigid transformation method offered by MATLAB imregister function, and arranged into the ring-shaped structure for visualization.
2.4. Schlemm’s canal quantifications
The semi-automatic segmentation performance was evaluated in one of the volumes by the dice similarity coefficient [35], using fully manual segmentation results as the ground truth for SC. Several measures were selected to serve as quantitative metrics of SC from the 3D segmentation, including the mean and standard deviation (STD) of the cross-sectional area (CSA) as well as the maximum CSA, the maximum and minimum SC opening width, and the number of the CCs stemming from the SC in each of the eight volumes. Specifically, the mean and STD of CSA, the maximum CSA, and the maximum and minimum SC opening width were automatically extracted from the segmentation masks in the secondary B-scans within the central part of the field of view (FOV). This was meant to avoid the higher segmentation error at the periphery of FOV due to lower contrast. The SC opening width, evaluated as the length of the minor axis of an ellipse that has the same central second-order moments as the mask region, was derived by the regionprops function in MATLAB. We used Welch’s t-test to compare the metrics from two different quadrants, and a P-value less than 0.05 was considered statistically significant. We also counted the number of CCs branching from the SC in each OCT intensity volume. The CCs were identified as the well delineated vessel-like structure stemmed from the SC and extended to the aqueous veins close to SC. The physical pixel size (in µm) was converted by dividing the rescaled isotropic digital resolution (7.5 µm) by the refractive index of the tissue (assumed as 1.4). All measurements were done using MATLAB.
3. Result
3.1. Schlemm’s canal imaging and segmentation performance
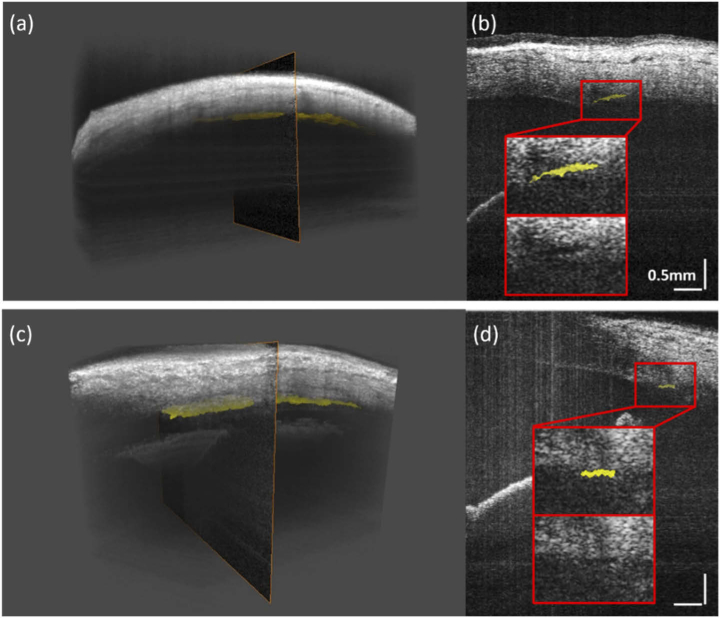
Figure 3(a) and (c) present the representative OCT volumes taken from a cardinal (See Visualization 2 (2.6MB, mp4) ) and an intercardinal position (See Visualization 3 (2.2MB, mp4) ), respectively, with SC color-coded in yellow. The re-sliced secondary B-scans from these volumes are shown in Fig. 3(b) and (d), respectively. The regions where SC resides are marked out by the red boxes, with the 2× zoom-in views shown in the insets. Despite being taken along the slow scan axis, motion artifacts are merely noticeable in these B-scans. Visual assessment of the segmented results compared to the original images suggests that the proposed method may faithfully segment the SC from the OCT volume. The mean dice similarity coefficient was calculated to be 0.76, with the fully manual segmentation of SC in the primary B-scans as the ground truth.
Fig. 3.
Representative 3D renderings and the secondary cross-sectional B-scans of the SC taken at the cardinal and intercardinal positions. (a) OCT volume taken at one of the cardinal positions (See Visualization 2 (2.6MB, mp4) ). (b) Re-sliced secondary B-scan indicated in (a). (c) OCT volume taken at one of the intercardinal positions (See Visualization 3 (2.2MB, mp4) ). (d) Re-sliced secondary B-scan indicated in (c). Insets: The 2× zoom-in views of the regions of interest (ROIs) marked by the red boxes, with the corresponding original images for comparison.
3.2. Full circumferential rendering and quantification of Schlemm’s canal
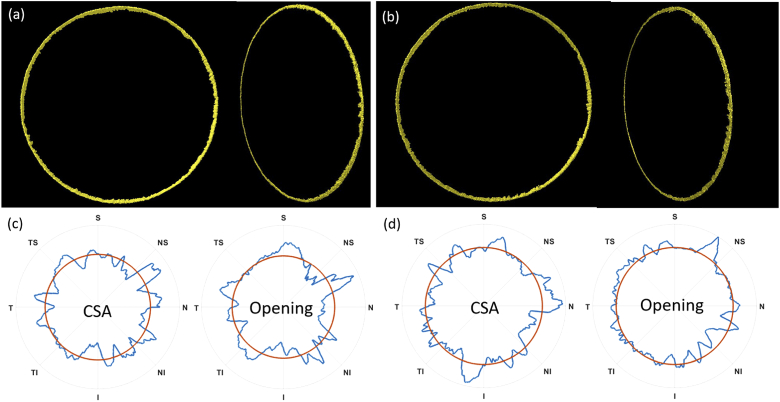
The full circumferential 3D renderings of the SCs in both eyes are presented in Fig. 4(a) and (b), respectively, in both Miyaki-Apple posterior view. The 3D renderings well depict the variability of the SC lumen size around the eye, as well as the conic shape of the SC. The CC branches extended from the SC can also be noticed from the stitched models.
Fig. 4.
The 3D full circumferential SC renderings in the posterior Miyaki-Apple view and side view for two eyes from S1, S2 in (a) and (b), respectively. (c), (d) Normalized CSA and the opening width of SC (opening) in polar plot for S1 and S2, respectively. The metrics was normalized by its global mean, marked as the red circles, and smoothed for visualization purpose.
The full circumferential quantification metrics derived from the SC segmentation results are listed in Table 1. The CSA and opening width of the SC for the two eyes are visualized in 360° in the polar plots in Fig. 4(c) and (d), respectively. The data was distributed equally at each quadrant and smoothed for better visualization. In previous literatures, the mean SC CSA in the nasal side was reported significantly higher than that in the temporal side in the previous literature [14,15,17,19,26,36]. Here we observed the same trend in both eyes with the nasal side showing larger SC CSA compared to the temporal (p < 0.001), which is as well manifested by the polar plots. The CSA measurement results also showed good agreement with the previous reports [9,11,15,21,22]. Nevertheless, we found the SC opening width significantly larger in the temporal quadrant in both subjects. In addition, we also confirmed the previous findings regarding the rapid and drastic change in SC size along the canal [9]. For example, in the eye of Subject 1, the thinnest opening width of the SC was measured to be 20 µm while the thickest was 143 µm.
Table 1. Measured SC metrics at different positions around the eye.a.
| Subject | Metrics | Location | |||||||
|---|---|---|---|---|---|---|---|---|---|
| I | NI | N | NS | S | TS | T | TI | ||
| S1 | Mean CSA [µm2] | 8930* | 10863 | 10983 | 10217 | 9642 | 10478 | 10521 | 9890 |
| STD of CSA [µm2] | 3067 | 3402 | 2663 | 4049 | 3350 | 3486 | 3370 | 3894 | |
| Max. CSA [µm2] | 15928 | 19831 | 19601 | 20233 | 18195 | 18224 | 17305 | 19831 | |
| Max. SC opening [µm] | 88 | 132 | 85 | 143 | 124 | 97 | 111 | 119 | |
| Min. SC opening [µm] | 28 | 29 | 31 | 20* | 39 | 35 | 37 | 29 | |
| # of CCs | 5 | 3 | 4 | 3 | 3 | 2 | 3 | 3 | |
| S2 | Mean CSA [µm2] | 10193 | 9144 | 9993 | 9710 | 9870 | 9587 | 9128* | 9684 |
| STD of CSA [µm2] | 2628 | 2130 | 2683 | 2255 | 2405 | 2282 | 1986 | 2155 | |
| Max. CSA [µm2] | 15210 | 14235 | 15325 | 15010 | 14235 | 14349 | 14263 | 14349 | |
| Max. SC opening [µm] | 85 | 73 | 84 | 99 | 87 | 90 | 83 | 95 | |
| Min. SC opening [µm] | 34 | 28* | 29 | 32 | 37 | 35 | 37 | 35 | |
| # of CCs | 5 | 3 | 5 | 3 | 3 | 3 | 4 | 3 | |
The maximum value is marked as bold; bThe minimum value is marked using *
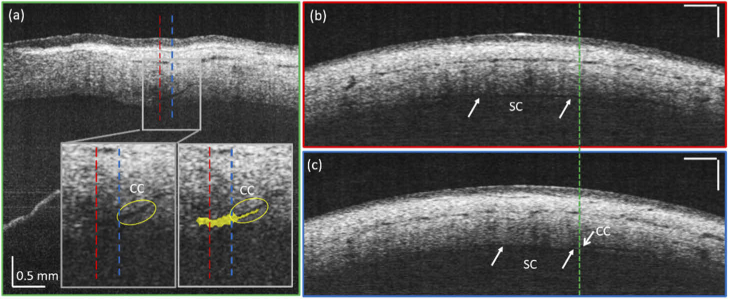
We also counted the number of the SC-CC orifices delineated from the OCT intensity volumes, summarized in Table 1 as well. The CC branches can be identified as structures directly spouting from the SC while extending and merging into the nearby aqueous veins and should be present in both primary and secondary B-scans, as shown in Fig. 5 and Visualization 4 (2.2MB, mp4) . Those obstructed by the shadows of the intrascleral or episcleral vessels were also excluded. We noticed that the CCs were more densely distributed in the nasal quadrant compared to the temporal quadrant, while highest number of CCs was found in the inferior quadrant. The total number of prominent CCs branches was 26 in one subject and 29 in the other, while in normal eyes, it is expected to be around 24 to 36 [28]. Smaller branches were difficult to delineate from the main SC lumen, mainly due to the relatively coarse lateral resolution adopted by the system. We observed an increased number of CCs in the inferior quadrant, which was supported by previous findings on the anatomical distribution of CCs around the eye [37,38].
Fig. 5.
An example of a CC being segmented when running in parallel with SC (See Visualization 4 (2.2MB, mp4) ). (a) The secondary B-scan in the cross-sectional plane showing both SC and CC closely located with each other. Insets: 2× zoom-in view of the ROI marked by the gray box with the corresponding segmentation color-coded in yellow. (b) (c) The primary B-scans taken from the red and blue dotted lines in (a), respectively. The green dotted line indicates the location of the secondary B-scan in (a).
4. Discussion and conclusion
In summary, we demonstrated full circumferential SC imaging and quantification using 1060 nm FDML SS-OCT at 1.66 MHz in human eyes with minimal motion artifacts. To our knowledge, it is the first demonstration of 1060 nm SS-OCT in full circumferential SC imaging. A semi-automatic active contour segmentation algorithm was applied in the B-scans along the longitudinal direction of the SC, which yielded reliable 3D SC segmentation results. This has important clinical applications, as the visualization of the entire SC within the eye provides a more holistic assessment of this aqueous outflow structure, especially in eyes with glaucoma. Furthermore, recent advances in glaucoma drainage surgery to lower IOP have led to devices that target the SC and aim to increase aqueous outflow – thus, imaging the entire SC may guide clinicians on where to implant these devices to achieve maximum effect on aqueous outflow [39].
Thus far, visualization of the aqueous humour outflow (AHO) trace in vivo is generally difficult due to the lack of scatterers such as red blood cells in the drainage system. A recent mouse study demonstrated in vivo visible light OCT angiography (OCT-A) for visualizing SC and limbal vascular network in mouse eyes, where blood reflex was introduced to the AHO to facilitate OCT-A contrast generation via episcleral vein blockage [40]. This practice is, however, not applicable in the clinical settings. To date, OCT remains the only modality that supports 3D non-invasive and contrast-free imaging of SC with high resolution. Segmentation of SC from OCT images is challenging mainly due to the low contrast as well as the inhomogeneous local intensity distribution. A few methods have been tested on automatic SC segmentation from SD-OCT images, including region growing method [41] and fuzzy hidden Markov chain algorithm [28]. However, quantitative segmentation assessment was not reported for these algorithms. The active contour segmentation algorithm has been applied to several medical imaging modalities and showed good performance in face of inhomogeneity and noise [42,43]. Here, we adopted a region-based active contour technique to incorporate a prior knowledge to guide the segmentation. Specifically, manual selection of the ROI was needed to refine the adaptive threshold result to the SC region. In future, novel segmentation algorithms as well as deep learning networks will be explored to fully automate the process.
The proximity of the CCs to the SC can occasionally cause them to be detected as a part of the SC, especially when the CC runs in parallel with the SC as shown in Fig. 5. From the secondary B-scan in Fig. 5(a) alone, it is difficult to notice the presence of CC. It only becomes visible when comparing two primary B-scans in Fig. 5(b) and (c) taken at two different tangential planes, respectively: The CC is spatially offset from the SC in Fig. 5(c) but not in Fig. 5(b). It is conceivable that the CC ostia will be segmented out as a part of the SC and cause segmentation error as manifested in the right inset of Fig. 5(a), where the segmentation result is color-coded in yellow. While the use of shape-based a prior knowledge may help to reduce this kind of segmentation error, in practice it is hard to avoid and may affect the SC quantification metrics derived from the segmentation.
There are several advantages in visualizing SC in the tangential plane along its longitudinal direction with the FDML based SS-OCT. First, it is easier to locate the SC using the proposed protocol. Previously, SC was often visualized cross-sectionally with the iridocorneal angle as guidance, identified as a small opening residing closest to the triangular-shaped trabecular meshwork in cross-sectional OCT image [44], as illustrated in Fig. 2(a). More often, however, there are multiple obstructions that may prevent clear delineation of SC from this viewing plane [11,20]. Using the current imaging protocol, SC structure appears as the first horizontal continuous dark channel in a primary OCT B-scan, most of which was not affected by the obstructions from the intrascleral and episcleral vessels nearby as well as the CCs running in parallel with it (See Visualization 1 (8MB, mp4) ). Secondly, it requires fewer B-scans, and eventually less time, to capture the entire SC section within the FOV, making it more resistant to eye motion artifacts. With the ultra-high speed offered by FDML laser, less than 1 second was required to complete the scan over a 9 mm × 4.8 mm area with a pixel resolution of 7.5 µm. This is significantly improved compared to conventional SD-OCT, which typically requires more than 2 seconds to acquire a 4 mm × 4 mm area with a similar pixel resolution [15,17,28].
It should be noted that the normal incidence at the corneal surface above the SC is crucial for successful delineation of SC with good signal-to-noise ratio (SNR) in OCT. Because of the small NA used to collect the signal, backscattered photons from the SC not at normal incidence to the corneal surface will suffer from greater coupling loss, resulting in a low SNR at the SC sites in the OCT image. Therefore, it is necessary to introduce an external target to shift the fixation of the patient’s eye to ensure normal incidence.
The segmented SCs have little overlapping areas and are in general smaller at the edges than in the central part of the FOV. This is because the surface curvature of the eyeball bends against the field curvature of the AS lens, and areas at the periphery of FOV usually suffer from low SNR and thus higher segmentation error. Efforts have been spent on counteracting the field curvature of the cornea to increase the FOV that can be captured in focus. For example, in full-field (FF) OCT, researchers have introduced a curved reference field to compensate for the field curvature in the sample arm, and they were able to demonstrate the extended FOV of 1.26 mm by 1.26 mm on the cornea, which is still considered limited compared to the entire 16 mm by 16 mm cornea surface [45]. Freeform optics design has also been proposed to inversely bend the field curvature so that it is conformable to the corneal surface for a non-scanning system [46]. However, only theoretical analysis was reported and it will be very challenging to realize such complicated designs in practice. We have previously demonstrated that by balancing the lateral resolution and DOF, it was possible to achieve an optimized lateral FOV (1.06 mm by 1.06 mm) for corneal endothelial cell imaging, similar to the FF-OCT results [47]. In this study, by further sacrificing the lateral resolution, the DOF of the system was extended to 1.8 mm [48], allowing for the SC within each volume to be captured within the DOF if aligned perfectly. Practically, it is nevertheless very challenging to achieve perfect alignment especially when motion is present. It may be necessary to further optimize the imaging protocol and the focusing optics to better capture the SC, which warrants a more detailed investigation.
There are several limitations of our study. First, raster scan patterns may not be optimal for SC imaging. However, in our study, the fast and slow scans were limited to be in either horizontal or vertical directions, and cannot be modified arbitrarily. Therefore, it was not possible to explore scan patterns other than raster scans. Novel scan patterns will be explored in future to improve the efficiency of full circumferential SC imaging. Second, the proposed segmentation method still relied on manual initiation of ROI, which requires one to two minutes for an experienced grader to finish one frame. It may take one or two days for one person to complete the full 3D circumferential SC stitching and quantification. Fully automated segmentation methods, such as deep-learning based segmentation, will be investigated to further accelerate the process. Last but not the least, in this study, we only included two healthy subjects. Further studies will be required to evaluate the proposed method on diseased eyes as well as its clinical viability.
In conclusion, we demonstrated full circumferential SC imaging, segmentation, and quantification in human eyes using 1060 nm FDML SS-OCT. The full circumferential rendering and quantification of SC enabled more sophisticated analysis of SC morphology than from SD-OCT systems. This offers a new method to examine the conventional aqueous outflow pathway, and gain further insights into the role of SC in IOP control and may lead to better management of glaucoma.
Acknowledgements
We would like to thank Ms. Qinglan Hu who helped us with OCT imaging.
Funding
National Medical Research Council10.13039/501100001349 (CG/C010A/2017, OFLCG/004C/2018, TA/MOH-000249-00/2018); Duke-NUS Medical School10.13039/100016017 (Duke-NUS-KP(Coll)/2018/0009A).
Disclosures
The authors declare no conflicts of interest.
Data availability
Data underlying the results presented in this paper are not publicly available at this time but may be obtained from the authors upon reasonable request.
References
- 1.Ang M., Chong W., Tay W. T., Yuen L., Wong T. Y., He M. G., Saw S. M., Aung T., Mehta J. S., “Anterior segment optical coherence tomography study of the cornea and anterior segment in adult ethnic South Asian Indian eyes,” Invest. Ophthalmol. Visual Sci. 53(1), 120–125 (2012). 10.1167/iovs.11-8386 [DOI] [PubMed] [Google Scholar]
- 2.Ang M., Chong W., Huang H., Tay W. T., Wong T. Y., He M. G., Aung T., Mehta J. S., “Comparison of anterior segment optical tomography parameters measured using a semi-automatic software to standard clinical instruments,” PLoS One 8(6), e65559 (2013). 10.1371/journal.pone.0065559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sng C. C. A., Aquino M. C. D., Liao J., Ang M., Zheng C., Loon S. C., Chew P. T. K., “Pretreatment anterior segment imaging during acute primary angle closure: insights into angle closure mechanisms in the acute phase,” Ophthalmology 121(1), 119–125 (2014). 10.1016/j.ophtha.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 4.Sng C. C., Aquino M. C., Liao J., Zheng C., Ang M., Chew P. T., “Anterior segment morphology after acute primary angle closure treatment: a randomised study comparing iridoplasty and medical therapy,” Br. J. Ophthalmol. 100(4), 542–548 (2016). 10.1136/bjophthalmol-2015-307087 [DOI] [PubMed] [Google Scholar]
- 5.Johnson M. C., Kamm R. D., “The role of Schlemm's canal in aqueous outflow from the human eye,” Invest. Ophthalmol. Visual Sci. 24, 320–325 (1983). [PubMed] [Google Scholar]
- 6.Grant W. M., “Clinical measurements of aqueous outflow,” Arch. Ophthalmol. 46(2), 113–131 (1951). 10.1001/archopht.1951.01700020119001 [DOI] [PubMed] [Google Scholar]
- 7.Moses R. A., “The effect of intraocular pressure on resistance to outflow,” Surv. Ophthalmol. 22(2), 88–100 (1977). 10.1016/0039-6257(77)90088-1 [DOI] [PubMed] [Google Scholar]
- 8.Hamanaka T., Matsuda A., Sakurai T., Kumasaka T., “Morphological abnormalities of Schlemm's canal in primary open-angle glaucoma from the aspect of aging,” Invest. Ophthalmol. Visual Sci. 57(2), 692–706 (2016). 10.1167/iovs.15-17127 [DOI] [PubMed] [Google Scholar]
- 9.Francis A. W., Kagemann L., Wollstein G., Ishikawa H., Folz S., Overby D. R., Sigal I. A., Wang B., Schuman J. S., “Morphometric analysis of aqueous humor outflow structures with spectral-domain optical coherence tomography,” Invest. Ophthalmol. Visual Sci. 53(9), 5198–5207 (2012). 10.1167/iovs.11-9229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allingham R. R., de Kater A. W., Ethier R. C., “Schlemm ‘s Canal and Primary Open Angle Glaucoma: Correlation Between Schlemm ‘s Canal Dimensions and Outflow Facility,” Exp. Eye Res. 62(1), 101–110 (1996). 10.1006/exer.1996.0012 [DOI] [PubMed] [Google Scholar]
- 11.Kagemann L., Wollstein G., Ishikawa H., Bilonick R. A., Brennen P. M., Folio L. S., Gabriele M. L., Schuman J. S., “Identification and assessment of Schlemm's canal by spectral-domain optical coherence tomography,” Invest. Ophthalmol. Visual Sci. 51(8), 4054–4059 (2010). 10.1167/iovs.09-4559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yan X., Li M., Chen Z., Zhu Y., Song Y., Zhang H., “Schlemm's canal and trabecular meshwork in eyes with primary open angle glaucoma: a comparative study using high-frequency ultrasound biomicroscopy,” PLoS One 11(1), e0145824 (2016). 10.1371/journal.pone.0145824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hann C. R., Vercnocke A. J., Bentley M. D., Jorgensen S. M., Fautsch M. P., “Anatomic changes in Schlemm's canal and collector channels in normal and primary open-angle glaucoma eyes using low and high perfusion pressures,” Invest. Ophthalmol. Visual Sci. 55(9), 5834–5841 (2014). 10.1167/iovs.14-14128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irshad F. A., Mayfield M. S., Zurakowski D., Ayyala R. S., “Variation in Schlemm's canal diameter and location by ultrasound biomicroscopy,” Ophthalmology 117(5), 916–920 (2010). 10.1016/j.ophtha.2009.09.041 [DOI] [PubMed] [Google Scholar]
- 15.Li P., Butt A., Chien J. L., Ghassibi M. P., Furlanetto R. L., Netto C. F., Liu Y., Kirkland W., Liebmann J. M., Ritch R., Park S. C., “Characteristics and variations of in vivo Schlemm's canal and collector channel microstructures in enhanced-depth imaging optical coherence tomography,” Br. J. Ophthalmol. 101(6), 808–813 (2017). 10.1136/bjophthalmol-2016-309295 [DOI] [PubMed] [Google Scholar]
- 16.Huang A. S., Francis B. A., Weinreb R. N., “Structural and functional imaging of aqueous humour outflow: a review,” Clin. Experiment. Ophthalmol. 46(2), 158–168 (2018). 10.1111/ceo.13064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kagemann L., Nevins J. E., Jan N.-J., Wollstein G., Ishikawa H., Kagemann J., Sigal I. A., Nadler Z., Ling Y., Schuman J. S., “Characterisation of Schlemm's canal cross-sectional area,” Br. J. Ophthalmol. 98(Suppl 2), ii10–ii14 (2014). 10.1136/bjophthalmol-2013-304629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ang M., Baskaran M., Werkmeister R. M., Chua J., Schmidl D., Aranha Dos Santos V., Garhofer G., Mehta J. S., Schmetterer L., “Anterior segment optical coherence tomography,” Prog Retin Eye Res 66, 132–156 (2018). 10.1016/j.preteyeres.2018.04.002 [DOI] [PubMed] [Google Scholar]
- 19.Hong J., Xu J., Wei A., Wen W., Chen J., Yu X., Sun X., “Spectral-domain optical coherence tomographic assessment of schlemm's canal in chinese subjects with primary open-angle glaucoma,” Ophthalmology 120(4), 709–715 (2013). 10.1016/j.ophtha.2012.10.008 [DOI] [PubMed] [Google Scholar]
- 20.Kagemann L., Wollstein G., Ishikawa H., Nadler Z., Sigal I. A., Folio L. S., Schuman J. S., “Visualization of the conventional outflow pathway in the living human eye,” Ophthalmology 119(8), 1563–1568 (2012). 10.1016/j.ophtha.2012.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi G. H., Wang F., Li X. Q., Lu J., Sun X. H., Jiang C. H., Zhang Y. D., “Assessment of Schlemm’s canal in a normal human eye by swept source optical coherence tomography,” Laser Phys. Lett. 10(7), 075602 (2013). 10.1088/1612-2011/10/7/075602 [DOI] [Google Scholar]
- 22.Shi G., Wang F., Li X., Lu J., Ding Z., Sun X., Jiang C., Zhang Y., “Morphometric measurement of Schlemm’s canal in normal human eye using anterior segment swept source optical coherence tomography,” J. Biomed. Opt. 17(1), 016016 (2012). 10.1117/1.JBO.17.1.016016 [DOI] [PubMed] [Google Scholar]
- 23.Leung C. K. S., Weinreb R. N., “Anterior chamber angle imaging with optical coherence tomography,” Eye 25(3), 261–267 (2011). 10.1038/eye.2010.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung C. W., Ang M., Farook M., Strouthidis N. G., Mehta J. S., Mari J. M., Girard M. J., “Enhancement of corneal visibility in optical coherence tomography images with corneal opacification,” Trans. Vis. Sci. Tech. 5(5), 3 (2016). 10.1167/tvst.5.5.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Girard M. J., Ang M., Chung C. W., Farook M., Strouthidis N., Mehta J. S., Mari J. M., “Enhancement of corneal visibility in optical coherence tomography images using corneal adaptive compensation,” Trans. Vis. Sci. Tech. 4(3), 3 (2015). 10.1167/tvst.4.3.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Usui T., Tomidokoro A., Mishima K., Mataki N., Mayama C., Honda N., Amano S., Araie M., “Identification of Schlemm's canal and its surrounding tissues by anterior segment fourier domain optical coherence tomography,” Invest. Ophthalmol. Visual Sci. 52(9), 6934–6939 (2011). 10.1167/iovs.10-7009 [DOI] [PubMed] [Google Scholar]
- 27.Spaide R. F., Koizumi H., Pozonni M. C., “Enhanced depth imaging spectral-domain optical coherence tomography,” Am. J. Ophthalmol. 146(4), 496–500 (2008). 10.1016/j.ajo.2008.05.032 [DOI] [PubMed] [Google Scholar]
- 28.Huang A. S., Belghith A., Dastiridou A., Chopra V., Zangwill L. M., Weinreb R. N., “Automated circumferential construction of first-order aqueous humor outflow pathways using spectral-domain optical coherence tomography,” J. Biomed. Opt. 22(6), 066010 (2017). 10.1117/1.JBO.22.6.066010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klein T., Wieser W., Eigenwillig C. M., Biedermann B. R., Huber R., “Megahertz OCT for ultrawide-field retinal imaging with a 1050 nm Fourier domain mode-locked laser,” Opt. Express 19(4), 3044–3062 (2011). 10.1364/OE.19.003044 [DOI] [PubMed] [Google Scholar]
- 30.Kolb J. P., Klein T., Kufner C. L., Wieser W., Neubauer A. S., Huber R., “Ultra-widefield retinal MHz-OCT imaging with up to 100 degrees viewing angle,” Biomed. Opt. Express 6(5), 1534–1552 (2015). 10.1364/BOE.6.001534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grulkowski I., Liu J. J., Baumann B., Potsaid B., Lu C., Fujimoto J. G., “Imaging limbal and scleral vasculature using swept source optical coherence tomography,” Photonics Lett. Pol. 3(4), 132–134 (2011). 10.4302/plp.2011.4.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Girard M. J. A., Strouthidis N. G., Ethier C. R., Mari J. M., “Shadow removal and contrast enhancement in optical coherence tomography images of the human optic nerve head,” Invest. Ophthalmol. Visual Sci. 52(10), 7738–7748 (2011). 10.1167/iovs.10-6925 [DOI] [PubMed] [Google Scholar]
- 33.Bradley D., Roth G., “Adaptive Thresholding using the Integral Image,” Journal of Graphics Tools 12(2), 13–21 (2007). 10.1080/2151237X.2007.10129236 [DOI] [Google Scholar]
- 34.Chan T. F., Vese L. A., “Active contours without edges,” IEEE Trans. on Image Process. 10(2), 266–277 (2001). 10.1109/83.902291 [DOI] [PubMed] [Google Scholar]
- 35.Zou K. H., Warfield S. K., Bharatha A., Tempany C. M. C., Kaus M. R., Haker S. J., Wells W. M., 3rd, Jolesz F. A., Kikinis R., “Statistical validation of image segmentation quality based on a spatial overlap index,” Acad Radiol 11(2), 178–189 (2004). 10.1016/S1076-6332(03)00671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uji A., Muraoka Y., Yoshimura N., “In vivo identification of the posttrabecular aqueous outflow pathway using swept-source optical coherence tomography,” Invest. Ophthalmol. Visual Sci. 57(10), 4162–4169 (2016). 10.1167/iovs.16-19869 [DOI] [PubMed] [Google Scholar]
- 37.Hann C. R., Fautsch M. P., “Preferential fluid flow in the human trabecular meshwork near collector channels,” Invest. Ophthalmol. Visual Sci. 50(4), 1692–1697 (2009). 10.1167/iovs.08-2375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jablonska J., Lewczuk K., Rękas M., “Schlemm's Canal: The Outflow “Vessel”,” (2016). [DOI] [PMC free article] [PubMed]
- 39.Sng C. C. A., Barton K., “Minimally invasive glaucoma surgery - coming of age,” Br. J. Ophthalmol. 102(10), 1315–1316 (2018). 10.1136/bjophthalmol-2018-313170 [DOI] [PubMed] [Google Scholar]
- 40.Zhang X., Beckmann L., Miller D. A., Shao G., Cai Z., Sun C., Sheibani N., Liu X., Schuman J., Johnson M., Kume T., Zhang H. F., “In vivo imaging of Schlemm's canal and limbal vascular network in mouse using visible-light OCT,” Invest. Ophthalmol. Visual Sci. 61(2), 23 (2020). 10.1167/iovs.61.2.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tom M., Ramakrishnan V., van Oterendorp C., Deserno T., Automated detection of Schlemm's canal in spectral-domain optical coherence tomography (SPIE, 2015). [Google Scholar]
- 42.Kim Y. J., Lee S. H., Park C. M., Kim K. G., “Evaluation of semi-automatic segmentation methods for persistent ground glass nodules on thin-section CT scans,” Healthc Inform Res 22(4), 305–315 (2016). 10.4258/hir.2016.22.4.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang X., Zhai Y., Liu X., Zhu W., Gao J., “Level-set method for image analysis of Schlemm's canal and trabecular meshwork,” Trans. Vis. Sci. Tech. 9(10), 7 (2020). 10.1167/tvst.9.10.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bald M., Li Y., Huang D., “Anterior chamber angle evaluation with fourier-domain optical coherence tomography,” J. Ophthalmol. 2012, 1–5 (2012). 10.1155/2012/103704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mazlin V., Xiao P., Dalimier E., Grieve K., Irsch K., Sahel J.-A., Fink M., Boccara A. C., “In vivo high resolution human corneal imaging using full-field optical coherence tomography,” Biomed. Opt. Express 9(2), 557–568 (2018). 10.1364/BOE.9.000557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nie Y., Gross H., Zhong Y., Duerr F., “Freeform optical design for a nonscanning corneal imaging system with a convexly curved image,” Appl. Opt. 56(20), 5630–5638 (2017). 10.1364/AO.56.005630 [DOI] [PubMed] [Google Scholar]
- 47.Yao X., Devarajan K., Werkmeister R. M., Santos V. A. D., Ang M., Kuo A., Wong D. W. K., Chua J., Tan B., Barathi V. A., Schmetterer L., “In vivo corneal endothelium imaging using ultrahigh resolution OCT,” Biomed. Opt. Express 10(11), 5675–5686 (2019). 10.1364/BOE.10.005675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pircher M., Zawadzki R. J., “Review of adaptive optics OCT (AO-OCT): principles and applications for retinal imaging [Invited],” Biomed. Opt. Express 8(5), 2536–2562 (2017). 10.1364/BOE.8.002536 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data underlying the results presented in this paper are not publicly available at this time but may be obtained from the authors upon reasonable request.