Abstract
We studied whether sustained hemodynamic support (>7 d) with the Impella 5.0 heart pump can be used as a bridge to clinical decisions in patients who present with cardiogenic shock, and whether such support can improve their outcomes.
We retrospectively reviewed cases of patients who had Impella 5.0 support at our hospital from August 2017 through May 2019. Thirty-four patients (23 with cardiogenic shock and 11 with severely decompensated heart failure) underwent sustained support for a mean duration of 11.7 ± 9.3 days (range, ≤48 d). Of 29 patients (85.3%) who survived to next therapy, 15 were weaned from the Impella, 8 underwent durable left ventricular assist device placement, 4 were escalated to venoarterial extracorporeal membrane oxygenation support, and 2 underwent heart transplantation. The 30-day survival rate was 76.5% (26 of 34 patients). Only 2 patients had a major adverse event: one each had an ischemic stroke and flail mitral leaflet. None of the devices malfunctioned.
Sustained hemodynamic support with the Impella 5.0 not only improved outcomes in patients who presented with cardiogenic shock, but also provided time for multidisciplinary evaluation of potential cardiac recovery, or the need for durable left ventricular assist device implantation or heart transplantation. Our study shows the value of using the Impella 5.0 as a bridge to clinical decisions.
Keywords: Equipment safety; heart failure/physiopathology/therapy; heart-assist devices; hemodynamics/physiology; recovery of function; retrospective studies; shock, cardiogenic/complications/mortality/therapy; survival analysis; time factors; treatment outcome
Despite advances in cardiac and critical care, the 30-day mortality rates in patients with cardiogenic shock range from 39.7% to 51.6%,1–3 and 1-year mortality rates, from 50% to 63%.2,4 Early mechanical circulatory support devices provided only modest benefit in these critically ill patients. In the Intra-aortic Balloon Support for Myocardial Infarction with Cardiogenic Shock trial, the 30-day mortality rates in patients who underwent or did not undergo intra-aortic balloon pump (IABP) treatment were similar (39.7% vs 41.3%), as were the 1-year mortality rates (52% vs 51%).5 A meta-analysis of trials on the TandemHeart (CardiacAssist, Inc.) left ventricular assist device (LVAD),6,7 the Impella LP 2.5 IABP (Abiomed, Inc.),8 and the Impella CP IABP (Abiomed)9 revealed no significant difference in 30-day mortality rates between patients undergoing temporary LVAD support and those undergoing IABP support (45% vs 43%10 and 45.5% vs 45.1%11). In other studies, survival to hospital discharge for patients in cardiogenic shock who were treated with venoarterial extracorporeal membrane oxygenation (VA-ECMO) was marginally better (42%–58%).12–15
In contrast, Impella 5.0 (Abiomed) support in a cohort of 16 patients who had cardiogenic shock led to promising survival rates of 94% (30 d) and 75% (1 yr).16 Similarly, in 5 other studies, 67% to 75% of patients presenting with acute decompensated heart failure (HF) and cardiogenic shock were successfully bridged to next therapy after 5 to 17 days of Impella 5.0 support.17–21
The Impella 5.0, a microaxial temporary mechanical circulatory support device, provides up to 5 L/min of forward blood flow from the left ventricle (LV) to the aorta.22 The device is placed through a femoral or axillary artery, carotid cutdown, or sternotomy. Its 21F microaxial pump is mounted on a 9F catheter. Blood is collected through an inflow site within the LV and is propelled through an outlet area in the proximal ascending aorta. The pump completely unloads the LV, decreasing LV myocardial wall tension and oxygen demand, which presumably enables myocardial recovery. Whereas Impella 5.0 treatment has been promising in patients with acute decompensated HF, its effectiveness in patients with cardiogenic shock has not been well studied. Moreover, more studies of using this device for longer than one week are needed.
We report our single-center use of the Impella 5.0 to provide sustained (>7 d) support in patients with cardiogenic shock or end-stage decompensated HF. We wanted to evaluate its potential use as a bridge to clinical decisions including device-weaning, durable mechanical circulatory support, and heart transplantation, as well as to determine whether sustained support substantially improved outcomes.
Patients and Methods
This single-center, retrospective, observational study, conducted at our hospital and medical college, was approved by our institutional review board.
We found 44 patients who were at least 18 years old and had undergone Impella 5.0 support from August 2017 through May 2019. The patients included in the study needed hemodynamic circulatory support to treat cardiogenic shock or acute decompensated HF. Previous use of VA-ECMO support or an IABP was acceptable. We excluded 8 patients who had undergone biventricular assist device support and 2 who had been treated with an Impella 5.0 for high-risk coronary artery bypass grafting (CABG) without shock or acute decompensated HF. Thus, the study included 34 patients: 23 (67.6%) presented with cardiogenic shock, and 11 (32.4%) presented with acutely decompensated HF that necessitated high doses of one or more inotropic agents.
Because early intervention for cardiogenic shock is important, our institution formed a shock team, including emergency department personnel, cardiologists with advanced-HF and interventional treatment expertise, critical care anesthesiologists, and cardiothoracic surgeons. Emergency department providers were prepared to activate the shock protocols early. Consensus for using the Impella 5.0 was reached soon after patients arrived.
The Impella was inserted, with use of a 10-mm graft, through the right axillary artery in 28 patients (82.4%). Some patients showed small axillary arteries or turbulent flow on ultrasonograms, so access was obtained through the right carotid artery in 4 (11.8%) and sternotomy in 2 (5.9%). Femoral artery access and left-sided approaches were not undertaken. Anticoagulation consisted of intravenous unfractionated heparin (0.15–0.3 IU/mL) and thromboelastography with reaction time 1.5 to 2 times that of normal. To prevent hemolysis, the Impella was run at pump performance levels P5 to P7 (plasma free hemoglobin, <12–15 mg/dL, measured daily).
When device explantation was anticipated, the pump speed was lowered to level P3. During a ramp echocardiographic study, pump speed was lowered to level P1. Explantation was then performed only under the following conditions: the patient was not on inotropic support and had a systolic blood pressure >90 mmHg, a cardiac index (CI) >2.2 L/min/m2, and a pulmonary capillary wedge pressure (PCWP) <18 mmHg (Swan-Ganz hemodynamic measurement). Patients who did not meet these criteria underwent evaluation for a durable LVAD or heart transplantation, and those ineligible for further treatment were referred for palliative or hospice care.
Definitions of Presenting Conditions, Complications, and Outcomes
Presenting Conditions. Cardiogenic shock was defined as inadequate tissue perfusion secondary to cardiac dysfunction, leading to elevated filling pressures and hypoperfusion with a systolic blood pressure <90 mmHg and end-organ damage necessitating at least one vasopressor. Cardiac index was not used to define cardiogenic shock because most of the patients in shock were already receiving 2 inotropic agents to augment the CI. Acute decompensated HF was defined as hemodynamic circulatory failure secondary to cardiac dysfunction that necessitated either inotropic or mechanical circulatory support in the absence of pressor needs.
Complications. We defined major bleeding in accordance with the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) criteria: suspected internal or external bleeding resulting in death, reoperation, hospitalization, or ≥4 units of packed red blood cells transfused per 24 hours. Major hemolysis was defined as a plasma free hemoglobin level >20 mg/dL or a serum lactate dehydrogenase level (in U/L) 2.5 times the upper limit of normal 72 hours after implantation, plus associated clinical symptoms or findings of hemolysis (hemoglobinuria, anemia, or hyperbilirubinemia) or abnormal pump function. Hematoma formation was defined as any collection of blood with swelling >5 cm in diameter on ultrasonographic or computed tomographic images or on palpation. Cerebrovascular accident was defined as any new, transient, or permanent focal neurologic deficit on standard neurologic examination with evidence of new infarction or hemorrhage on images. Vascular complications necessitating surgical intervention included vessel dissection, stenosis, thrombosis, perforation, or rupture, and arteriovenous fistula, pseudoaneurysm, acute limb ischemia, and new valvular injury secondary to Impella placement. Valvular injury was defined as new injury to the aortic, mitral, tricuspid, or pulmonic valve when confirmed on Doppler echocardiograms or noted on autopsy. Major infection was defined as clinical infection accompanied by pain, fever, drainage, or leukocytosis, necessitating therapy with antimicrobial agents. Two categories of renal dysfunction were identified according to the INTERMACS definitions of acute and chronic renal dysfunction. Device malfunction included the failure of any device component to operate at designed performance specifications or to perform as intended.
Outcomes. Survival to next therapy was defined as removal of the Impella 5.0 at the time of LVAD implantation, escalation to VA-ECMO support, or heart transplant. For those weaned, survival to next therapy was defined as Impella 5.0 removal after hemodynamic stability was determined by means of an echocardiographic ramp study.
Statistical Analysis
Categorical data, expressed as number and percentage, were compared by using the χ2 test. For data with sample sizes <5, the Fisher exact test was used. Continuous data, expressed as mean ± SD, were compared by using the independent Student t test. A 2-sided P value <0.05 was considered statistically significant. Analysis was performed by using R version 3.3.2 GUI Mavericks build (The R Foundation).
Results
Before Impella 5.0 implantation, all patients had severe LV dysfunction (Table I): mean LV ejection fraction (LVEF), 19.4% ± 8.1%; systolic blood pressure, 105 ± 20.1 mmHg; CI (Fick method), 2.3 ± 0.7 L/min/m2; PCWP, 22.8 ± 7.2 mmHg; and central venous pressure, 13.4 ± 6.2 mmHg. Mean laboratory levels included lactic acid, 2.9 ± 2.8 mmol/L; creatinine, 2.1 ± 1.2 mg/dL; aspartate aminotransferase, 784.5 ± 1,901 IU/L; alanine aminotransferase, 400.7 ± 881.1 IU/L; and mixed venous oxygen saturation, 47% ± 16.9%. The mean number of pressors for the entire cohort was 1.5 ± 1.1. Patients in cardiogenic shock needed an average of 2 pressors before Impella implantation (range, 1–4 pressors).
TABLE I.
Baseline Characteristics of Patients by Weaning Status
| Variable | Total (N=34) | Weaned (n=15) | Not Weaned (n=19) | P Value |
|---|---|---|---|---|
| Age (yr) | 57.6 ± 13.4 | 58 ± 13.2 | 57.2 ± 13.3 | 0.86 |
| Male sex | 23 (67.6) | 9 (60) | 14 (73.7) | 0.47 |
| Transfer from other hospital | 14 (41.2) | 5 (33.3) | 9 (47.4) | 0.5 |
| ICM | 22 (64.7) | 10 (66.7) | 12 (63.2) | 0.99 |
| Hypertension | 23 (67.6) | 12 (80) | 11 (57.9) | 0.27 |
| Renal insufficiency | 12 (35.3) | 7 (46.7) | 5 (26.3) | 0.29 |
| Diabetes | 16 (47.1) | 9 (60) | 7 (36.8) | 0.3 |
| COPD | 10 (29.4) | 3 (20) | 7 (36.8) | 0.45 |
| Cerebrovascular disease | 4 (11.8) | 4 (26.7) | 0 | 0.03 |
| Valvular disease | 9 (26.5) | 2 (13.3) | 7 (36.8) | 0.24 |
| Previous CABG | 4 (11.8) | 2 (13.3) | 2 (10.5) | 0.99 |
| Mechanical ventilation | 33 (97.1) | 15 (100) | 18 (94.7) | 0.99 |
| Mitral regurgitation | 11 (32.4) | 4 (26.7) | 7 (36.8) | 0.72 |
| Cardiopulmonary resuscitation | 10 (29.4) | 4 (26.7) | 6 (31.6) | 0.99 |
| CRRT | 15 (44.1) | 4 (26.7) | 11 (57.9) | 0.09 |
| MELD | 23.1 ± 9 | 19.5 ± 9.4 | 25.6 ± 8.1 | 0.07 |
| Peripheral vascular disease | 5 (14.7) | 4 (26.7) | 1 (5.3) | 0.15 |
| INTERMACS 1 | 20 (58.8) | 7 (46.7) | 13 (68.4) | 0.3 |
| Pressors needed | 1.5 ± 1.1 | 1.3 ± 1 | 1.6 ± 1.3 | 0.35 |
| Vasoactive inotropic score | 23.2 ± 23.8 | 20.4 ± 21.4 | 25.3 ± 25.9 | 0.55 |
| LVEF (%) | 19.4 ± 8.1 | 18.6 ± 6 | 20 ± 9.5 | 0.59 |
| Systolic BP (mmHg) | 105 ± 20.1 | 111.4 ± 20.3 | 99.9 ± 19 | 0.1 |
| Diastolic BP (mmHg) | 65.3 ± 9.7 | 63.7 ± 9.3 | 66.5 ± 10.1 | 0.42 |
| Systolic PAP (mmHg) | 43.3 ± 13.5 | 40.1 ± 15.3 | 45 ± 12.7 | 0.46 |
| Diastolic PAP (mmHg) | 22.8 ± 7.2 | 21.9 ± 5.6 | 23.3 ± 8 | 0.64 |
| PCWP (mmHg) | 22.8 ± 7.2 | 21.9 ± 5.6 | 23.3 ± 8 | 0.64 |
| Central venous pressure (mmHg) | 13.4 ± 6.2 | 11.2 ± 5.3 | 14.9 ± 6.5 | 0.16 |
| Cardiac output (L/min) | 4.5 ± 1.7 | 4.6 ± 1.7 | 4.5 ± 1.7 | 0.93 |
| Cardiac index (L/min/m2) | 2.3 ± 0.7 | 2.4 ± 0.7 | 2.3 ± 0.7 | 0.72 |
| Cardiac power output (W) | 0.8 ± 0.4 | 0.8 ± 0.3 | 0.8 ± 0.4 | 0.93 |
| Sodium (mmol/L) | 135.6 ± 4.4 | 136.1 ± 4.3 | 135.2 ± 4.5 | 0.56 |
| Creatinine (mg/dL) | 2.1 ± 1.2 | 2 ± 1.2 | 2.2 ± 1.1 | 0.68 |
| Alkaline phosphatase (IU/L) | 96.6 ± 73.2 | 80.9 ± 38.9 | 107.4 ± 88.9 | 0.26 |
| AST (IU/L) | 784.5 ± 1,901 | 361.8 ± 868.9 | 1,041.8 ± 2,350 | 0.26 |
| ALT (IU/L) | 400.7 ± 881.1 | 237.4 ± 643.4 | 512.4 ± 1,014.2 | 0.36 |
| Hemoglobin (g/dL) | 11 ± 2.2 | 11 ± 2.8 | 11.1 ± 1.8 | 0.87 |
| Platelet count (×103/μL) | 187.2 ± 88.2 | 183 ± 63 | 190.6 ± 105.6 | 0.8 |
| Albumin (g/dL) | 3.3 ± 0.8 | 3.1 ± 0.9 | 3.5 ± 0.7 | 0.19 |
| Body surface area (m2) | 2.1 ± 0.3 | 2 ± 0.3 | 2.1 ± 0.3 | 0.59 |
| Lactic acid (mmol/L) | 2.9 ± 2.8 | 2.5 ± 2.1 | 3.3 ± 3.4 | 0.47 |
| Time to normal lactic acid level (hr) | 8.7 ± 18.7 | 6.1 ± 10.7 | 10.7 ± 23.3 | 0.45 |
| ACS | 10 (29.4) | 6 (40) | 4 (21.1) | 0.28 |
| STEMI | 5 (14.7) | 2 (13.3) | 3 (15.8) | 0.99 |
| NSTEMI | 5 (14.7) | 4 (26.7) | 1 (5.3) | 0.15 |
| Non-ACS ICM | 12 (54.2) | 4 (26.7) | 8 (42.1) | 0.3 |
| NICM | 12 (35.3) | 5 (33.3) | 7 (36.8) | 0.99 |
| 30-day survival | 26 (76.5) | 13 (86.7) | 13 (68.4) | 0.84 |
| Survival to hospital discharge | 25 (73.5) | 13 (86.7) | 12 (63.2) | 0.74 |
ACS = acute coronary syndrome; ALT = alanine aminotransferase; AST = aspartate aminotransferase; BP = blood pressure; CABG = coronary artery bypass grafting; COPD = chronic obstructive pulmonary disease; CRRT = continuous renal replacement therapy; ICM = ischemic cardiomyopathy; INTERMACS = Interagency Registry for Mechanically Assisted Circulatory Support; LVEF = left ventricular ejection fraction; MELD = model for end-stage liver disease; NICM = nonischemic cardiomyopathy; NSTEMI = non-ST-segment-elevation myocardial infarction; PAP = pulmonary artery pressure; PCWP = pulmonary capillary wedge pressure; STEMI = ST-segment-elevation myocardial infarction
Data are presented as mean ± SD or as number and percentage. P <0.05 was considered statistically significant.
TABLE I.
Baseline Characteristics of Patients by Weaning Status (continued)
| Variable | Total (N=34) | Weaned (n=15) | Not Weaned (n=19) | P Value |
|---|---|---|---|---|
| Age (yr) | 57.6 ± 13.4 | 58 ± 13.2 | 57.2 ± 13.3 | 0.86 |
| Male sex | 23 (67.6) | 9 (60) | 14 (73.7) | 0.47 |
| Transfer from other hospital | 14 (41.2) | 5 (33.3) | 9 (47.4) | 0.5 |
| ICM | 22 (64.7) | 10 (66.7) | 12 (63.2) | 0.99 |
| Hypertension | 23 (67.6) | 12 (80) | 11 (57.9) | 0.27 |
| Renal insufficiency | 12 (35.3) | 7 (46.7) | 5 (26.3) | 0.29 |
| Diabetes | 16 (47.1) | 9 (60) | 7 (36.8) | 0.3 |
| COPD | 10 (29.4) | 3 (20) | 7 (36.8) | 0.45 |
| Cerebrovascular disease | 4 (11.8) | 4 (26.7) | 0 | 0.03 |
| Valvular disease | 9 (26.5) | 2 (13.3) | 7 (36.8) | 0.24 |
| Previous CABG | 4 (11.8) | 2 (13.3) | 2 (10.5) | 0.99 |
| Mechanical ventilation | 33 (97.1) | 15 (100) | 18 (94.7) | 0.99 |
| Mitral regurgitation | 11 (32.4) | 4 (26.7) | 7 (36.8) | 0.72 |
| Cardiopulmonary resuscitation | 10 (29.4) | 4 (26.7) | 6 (31.6) | 0.99 |
| CRRT | 15 (44.1) | 4 (26.7) | 11 (57.9) | 0.09 |
| MELD | 23.1 ± 9 | 19.5 ± 9.4 | 25.6 ± 8.1 | 0.07 |
| Peripheral vascular disease | 5 (14.7) | 4 (26.7) | 1 (5.3) | 0.15 |
| INTERMACS 1 | 20 (58.8) | 7 (46.7) | 13 (68.4) | 0.3 |
| Pressors needed | 1.5 ± 1.1 | 1.3 ± 1 | 1.6 ± 1.3 | 0.35 |
| Vasoactive inotropic score | 23.2 ± 23.8 | 20.4 ± 21.4 | 25.3 ± 25.9 | 0.55 |
| LVEF (%) | 19.4 ± 8.1 | 18.6 ± 6 | 20 ± 9.5 | 0.59 |
| Systolic BP (mmHg) | 105 ± 20.1 | 111.4 ± 20.3 | 99.9 ± 19 | 0.1 |
| Diastolic BP (mmHg) | 65.3 ± 9.7 | 63.7 ± 9.3 | 66.5 ± 10.1 | 0.42 |
| Systolic PAP (mmHg) | 43.3 ± 13.5 | 40.1 ± 15.3 | 45 ± 12.7 | 0.46 |
| Diastolic PAP (mmHg) | 22.8 ± 7.2 | 21.9 ± 5.6 | 23.3 ± 8 | 0.64 |
| PCWP (mmHg) | 22.8 ± 7.2 | 21.9 ± 5.6 | 23.3 ± 8 | 0.64 |
| Central venous pressure (mmHg) | 13.4 ± 6.2 | 11.2 ± 5.3 | 14.9 ± 6.5 | 0.16 |
| Cardiac output (L/min) | 4.5 ± 1.7 | 4.6 ± 1.7 | 4.5 ± 1.7 | 0.93 |
| Cardiac index (L/min/m2) | 2.3 ± 0.7 | 2.4 ± 0.7 | 2.3 ± 0.7 | 0.72 |
| Cardiac power output (W) | 0.8 ± 0.4 | 0.8 ± 0.3 | 0.8 ± 0.4 | 0.93 |
| Sodium (mmol/L) | 135.6 ± 4.4 | 136.1 ± 4.3 | 135.2 ± 4.5 | 0.56 |
| Creatinine (mg/dL) | 2.1 ± 1.2 | 2 ± 1.2 | 2.2 ± 1.1 | 0.68 |
| Alkaline phosphatase (IU/L) | 96.6 ± 73.2 | 80.9 ± 38.9 | 107.4 ± 88.9 | 0.26 |
| AST (IU/L) | 784.5 ± 1,901 | 361.8 ± 868.9 | 1,041.8 ± 2,350 | 0.26 |
| ALT (IU/L) | 400.7 ± 881.1 | 237.4 ± 643.4 | 512.4 ± 1,014.2 | 0.36 |
| Hemoglobin (g/dL) | 11 ± 2.2 | 11 ± 2.8 | 11.1 ± 1.8 | 0.87 |
| Platelet count (×103/μL) | 187.2 ± 88.2 | 183 ± 63 | 190.6 ± 105.6 | 0.8 |
| Albumin (g/dL) | 3.3 ± 0.8 | 3.1 ± 0.9 | 3.5 ± 0.7 | 0.19 |
| Body surface area (m2) | 2.1 ± 0.3 | 2 ± 0.3 | 2.1 ± 0.3 | 0.59 |
| Lactic acid (mmol/L) | 2.9 ± 2.8 | 2.5 ± 2.1 | 3.3 ± 3.4 | 0.47 |
| Time to normal lactic acid level (hr) | 8.7 ± 18.7 | 6.1 ± 10.7 | 10.7 ± 23.3 | 0.45 |
| ACS | 10 (29.4) | 6 (40) | 4 (21.1) | 0.28 |
| STEMI | 5 (14.7) | 2 (13.3) | 3 (15.8) | 0.99 |
| NSTEMI | 5 (14.7) | 4 (26.7) | 1 (5.3) | 0.15 |
| Non-ACS ICM | 12 (54.2) | 4 (26.7) | 8 (42.1) | 0.3 |
| NICM | 12 (35.3) | 5 (33.3) | 7 (36.8) | 0.99 |
| 30-day survival | 26 (76.5) | 13 (86.7) | 13 (68.4) | 0.84 |
| Survival to hospital discharge | 25 (73.5) | 13 (86.7) | 12 (63.2) | 0.74 |
ACS = acute coronary syndrome; ALT = alanine aminotransferase; AST = aspartate aminotransferase; BP = blood pressure; CABG = coronary artery bypass grafting; COPD = chronic obstructive pulmonary disease; CRRT = continuous renal replacement therapy; ICM = ischemic cardiomyopathy; INTERMACS = Interagency Registry for Mechanically Assisted Circulatory Support; LVEF = left ventricular ejection fraction; MELD = model for end-stage liver disease; NICM = nonischemic cardiomyopathy; NSTEMI = non-ST-segment-elevation myocardial infarction; PAP = pulmonary artery pressure; PCWP = pulmonary capillary wedge pressure; STEMI = ST-segment-elevation myocardial infarction
Data are presented as mean ± SD or as number and percentage. P <0.05 was considered statistically significant.
After 24 hours of Impella support, mean cardiac output (CO) increased from 4.5 ± 1.7 to 5.6 ± 1.5 L/min (P=0.035), mean CI improved from 2.3 ± 0.7 to 2.8 ± 0.8 L/min/m2 (P=0.026), and mean PCWP decreased from 22.8 ± 7.2 to 19.5 ± 7.4 mmHg (P=0.02). Lactic acid levels became normal within a mean of 7.8 ± 18.2 hours across the cohort, and patients were weaned from pressors within a mean of 1.7 ± 2.1 days.
The Impella 5.0 served as a bridge to clinical decisions in all patients, including those who died. Because of psychosocial reasons or comorbidities, 5 patients (14.7%) were not suitable for durable LVAD support; they chose palliative treatment or hospice care, and they died shortly after Impella removal. Of the survivors, 15 patients (44.1%) were hemodynamically stabilized and weaned from Impella support: 8 (23.5%) underwent durable LVAD implantation, 4 (11.8%) received escalated VA-ECMO support, and 2 (5.9%) underwent heart transplantation (Fig. 1). Two of the 4 patients who had VA-ECMO support survived.
Fig. 1.
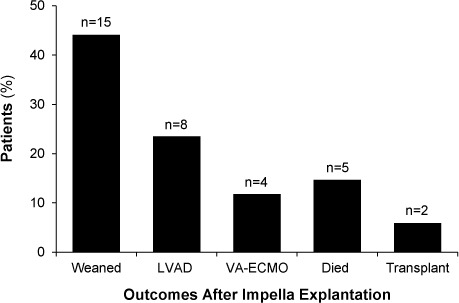
Graph shows outcomes after Impella 5.0 explantation.
LVAD = left ventricular assist device; VA-ECMO = venoarterial extracorporeal membrane oxygenation
The mean duration of Impella support overall was 11.7 ± 9.3 days (range, ≤48 d); in patients who died, it was 13.1 days, and in the patients with LVADs, 15.1 days. Support time was shorter in those who were weaned (10.8 d) and in those who were escalated to VA-ECMO (6.3 d). The causes of death after Impella removal were progressive HF in 4 patients (80%) and multiorgan failure in one (20%). All Impella devices were inspected upon removal, and no thrombi were seen.
The improved outcomes after sustained Impella 5.0 use are highlighted by the overall 30-day survival rate of 76.5% (26 of 34 patients) and survival to hospital discharge of 73.5% (25 of 34) (Table I). Four of the 8 deaths within 30 days were patients who did not qualify for a durable LVAD. Thirteen of the 15 patients weaned from support (86.7%) were alive at 30 days, as were all 8 patients who were given an LVAD (Fig. 2). In one patient, the cause of death was abdominal aortic aneurysm rupture, and in the other, progressive HF in the presence of worsening acute kidney injury.
Fig. 2.
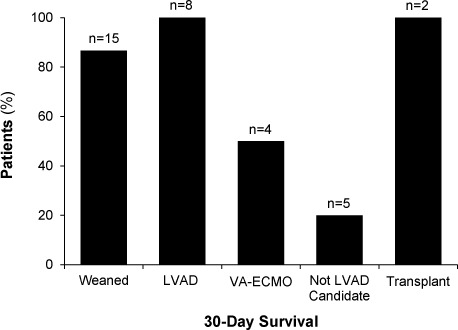
Graph shows 30-day survival rates by outcome.
LVAD = left ventricular assist device; VA-ECMO = venoarterial extracorporeal membrane oxygenation
Of the 15 patients who were weaned, 11 (73.3%) had an improved LVEF (defined as a >5% increase), from a mean of 18.3% ± 6.7% to 41.5% ± 16.2%. The remaining 4 patients recovered their previous level of LVEF. Twelve of the 15 were alive at one year.
Five patients (14.7%) had presented with ST-segment-elevation myocardial infarction (STEMI) and 5 with non-STEMI (NSTEMI). Twelve (35.3%) had gradually progressive ischemic cardiomyopathy, and 12 had nonischemic cardiomyopathy (NICM). The cases of NICM were considered secondary to dilated, stress-induced, or neurocardiogenic cardiomyopathy, or secondary to thyroid storm, troponin T gene mutation, atrial fibrillation, or ventricular fibrillation arrest secondary to hypokalemia. The 30-day survival rate for those with STEMI was 80%; NSTEMI, 80%; ischemic cardiomyopathy, 68.2%; and NICM, 91.7%.
In-hospital complications included major bleeding in 14 patients (41.2%), major hemolysis in 12 (35.3%), major infection in 9 (26.5%), hematoma formation in 6 (17.6%), and hemolysis necessitating device removal in 2 (5.9%). Pneumonia (n=5) and urinary tract infection (n=2) were the most common infections. One patient (2.9%) had an ischemic stroke, transient ischemic attack, flail mitral leaflet secondary to Impella malposition, acute limb ischemia, intermittent complete heart block, cardiac arrest after Impella removal, and seroma formation. The presumed cause of the ischemic stroke was atrial fibrillation. The patient had presented in cardiogenic shock and was eventually weaned from the Impella. One patient died 6 days after Impella removal as a result of abdominal aortic aneurysm rupture. No Impella pump malfunctioned.
Of 12 patients (35.3%) who had chronic kidney disease (CKD) before admission, 10 were undergoing outpatient hemodialysis for end-stage renal disease. Fifteen patients (44.1%) needed continuous renal replacement therapy during hospitalization. The mean serum creatinine level before Impella implantation was 2.1 ± 1.2 mg/dL, compared with 2.2 ± 1.6 mg/dL at hospital discharge. Of the 15 patients without CKD who presented with elevated creatinine levels, 6 (40%) regained normal renal function after pump insertion. Of 3 patients who needed new hemodialysis when discharged, one had CKD III before admission, one had normal renal function before admission, and one had unknown baseline renal function.
Discussion
This single-center study of patients with cardiogenic shock and severely decompensated HF showed that the Impella 5.0 provides hemodynamic stability, improves end-organ perfusion, and enables time for cardiac recovery and clinical decisions. Twenty-nine of 34 patients (85%) survived to next therapy, 76.5% (26 patients) were alive at 30 days, 73.5% (25) were discharged from the hospital, and 44.1% (15) were weaned from the Impella. All are promising results in a cohort with a historical in-hospital survival rate <50%.23,24 Potential explanations for the improved outcomes with Impella 5.0 circulatory support include complete LV unloading (compared with increased afterload associated with VA-ECMO); improved CO and end-organ perfusion; and device insertion through the axillary route, which enables patients to participate in physical therapy for faster recovery.
Early recognition of cardiogenic shock and decompensated HF may also have contributed to the improved outcomes in our cohort. Our shock-team system enabled rapid multidisciplinary consultation and treatment tailored to each patient's hemodynamic instability on admission. Furthermore, our high-volume tertiary care center always has a hybrid room available, thus shortening the time from admission to Impella 5.0 insertion. Finally, our experienced cardiothoracic surgeons inserted Impella devices rapidly and knew how to limit complications.
In early prospective studies of the Impella 5.0, the mean support duration was <7 days,17–19 because the device had been approved for 6 days at most. However, according to the Impella user manual, weaning can be delayed in the presence of ongoing hemodynamic instability,22 so our institution continues Impella support until next therapy can be decided. Therefore, the mean support time in this study was nearly 12 days, and for 48 days in one case. Only 4 of 15 patients (26.7%) were weaned by day 6 (Fig. 3), suggesting that most patients who present in cardiogenic shock or decompensated HF need >6 days for cardiac recovery. Support time should be tailored to the underlying pathophysiology of their shock or decompensation and not be discontinued artificially. Longer support probably improved our patients' cardiac and end-organ recovery, frailty, and functional capacity.
Fig. 3.
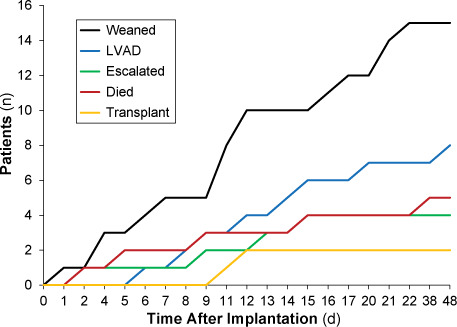
Graph shows the time-to-event curve after Impella 5.0 implantation.
LVAD = left ventricular assist device
Our cohort's better hemodynamic stability may also explain the higher percentage of patients weaned from support than in earlier studies (44.1% vs 10%).17,19 Moreover, the mean CO (4.5 L/min), mean CI (2.3 L/min/m2), and percentage of INTERMACS 1 patients (67.6%) were also higher.17,19,21 The Impella 5.0 probably unloaded the LV, decreasing oxygen demand while improving oxygen supply through decreased LV end-diastolic pressure, thus optimizing cardiac recovery. After 24 hours of support, CO, CI, and PCWP significantly improved.
Determining which patients with cardiogenic shock (INTERMACS 1) or decompensated HF (INTERMACS 2) are candidates for the Impella 5.0 is difficult. After evaluating comorbidities and demographic, hemodynamic, and laboratory data, we found no sound predictors for which patients would be weaned from support and which would need advanced therapy. The only variable significantly associated with weaning was a history of cerebrovascular disease—perhaps a coincidence, because no unweaned patients had that history. We also found that patients with concomitant organ failure were less likely to be weaned successfully.
The 5 patients who died before next therapy were supported for 13.1 ± 2.6 days, during which an average of 2 failed attempts at weaning were made. After 10 to 14 days, multidisciplinary discussions of their cases were held. None was a candidate for a durable LVAD because of socioeconomic barriers or comorbidities, and all chose hospice care over further Impella support. Even though these patients died, Impella support sustained them long enough for sound clinical decisions.
The benefits of Impella 5.0 support far outweigh the risks.17–21,25 In total, 85.3% of our patients were successfully bridged to myocardial recovery (n=15), underwent durable-LVAD implant (8), escalated to VA-ECMO support (4), or underwent a heart transplant (2). Of the 4 patients who had VA-ECMO support, 2 were weaned and survived. As in earlier studies, the main risks of Impella placement were major bleeding (41.2% overall), major hemolysis (35.3%), infection (26.5%), and hematoma formation (17.6%).17–19,21 Our study was the only one to include a patient who had a flail mitral leaflet secondary to device malposition, necessitating urgent mitral valve replacement. Despite the potentially fatal complications such as stroke and mitral flail, the few adverse events and the high bridging rate in our study justify Impella support in this critically ill population. Moreover, in our study, the Impella provided hemodynamic support for ≤48 days with no malfunctions.
Study Limitations. This study was limited by its retrospective design and lack of a control group. Although the cohort was relatively large for a single-center study, the small number of patients made it difficult to find statistical differences between groups. Moreover, no standard protocol with inclusion and exclusion criteria detailed which patients should have been given the Impella or VA-ECMO therapy; Impella implantation was at the discretion of the multidisciplinary shock team.
Conclusions
Our study of Impella 5.0 in patients with cardiogenic shock and decompensated heart failure shows that it can provide hemodynamic stability and improve outcomes. Sustained support can enable cardiac recovery and weaning from device support. In patients who do not improve, device support affords time for multidisciplinary decisions regarding eligibility for durable-LVAD implantation or heart transplant. Patients undergoing support had few adverse events, and there were no instances of device malfunction. A multicenter prospective trial comparing Impella 5.0 support with the standard of care should help to determine the safety and efficacy of the device.
Acknowledgments
We thank Gloria Lin, BS; Emily Neumann, BSN; Barb Alivo, BSN; and Elizabeth Suelzer, MLIS; for their assistance with this manuscript.
Footnotes
Conflict of interest disclosures: Dr. David Joyce serves on the Abiomed, Inc., Surgical Advisory Board. Dr. Lyle Joyce serves on the SynCardia medical advisory board and is a proctor and consultant for Abbott.
References
- 1.Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017;377(25):2419–32. doi: 10.1056/NEJMoa1710261. [DOI] [PubMed] [Google Scholar]
- 2.Aissaoui N, Puymirat E, Tabone X, Charbonnier B, Schiele F, Lefevre T et al. Improved outcome of cardiogenic shock at the acute stage of myocardial infarction: a report from the USIK 1995, USIC 2000, and FAST-MI French nationwide registries. Eur Heart J. 2012;33(20):2535–43. doi: 10.1093/eurheartj/ehs264. [DOI] [PubMed] [Google Scholar]
- 3.Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012;367(14):1287–96. doi: 10.1056/NEJMoa1208410. [DOI] [PubMed] [Google Scholar]
- 4.Thiele H, Akin I, Sandri M, de Waha-Thiele S, Meyer-Saraei R, Fuernau G et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018;379(18):1699–710. doi: 10.1056/NEJMoa1808788. [DOI] [PubMed] [Google Scholar]
- 5.Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J et al. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013;382(9905):1638–45. doi: 10.1016/S0140-6736(13)61783-3. [DOI] [PubMed] [Google Scholar]
- 6.Burkhoff D, Cohen H, Brunckhorst C, O'Neill WW, TandemHeart Investigators Group A randomized multicenter clinical study to evaluate the safety and efficacy of the TandemHeart percutaneous ventricular assist device versus conventional therapy with intraaortic balloon pumping for treatment of cardiogenic shock. Am Heart J. 2006;152(3):469.e1–8. doi: 10.1016/j.ahj.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 7.Thiele H, Sick P, Boudriot E, Diederich KW, Hambrecht R, Niebauer J, Schuler G. Randomized comparison of intra-aortic balloon support with a percutaneous left ventricular assist device in patients with revascularized acute myocardial infarction complicated by cardiogenic shock. Eur Heart J. 2005;26(13):1276–83. doi: 10.1093/eurheartj/ehi161. [DOI] [PubMed] [Google Scholar]
- 8.Seyfarth M, Sibbing D, Bauer I, Frohlich G, Bott-Flugel L, Byrne R et al. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J Am Coll Cardiol. 2008;52(19):1584–8. doi: 10.1016/j.jacc.2008.05.065. [DOI] [PubMed] [Google Scholar]
- 9.Ouweneel DM, Eriksen E, Sjauw KD, van Dongen IM, Hirsch A, Packer EJS et al. Percutaneous mechanical circulatory support versus intra-aortic balloon pump in cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol. 2017;69(3):278–87. doi: 10.1016/j.jacc.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 10.Cheng JM, den Uil CA, Hoeks SE, van der Ent M, Jewbali LSD, van Domburg RT, Serruys PW. Percutaneous left ventricular assist devices vs intra-aortic balloon pump counterpulsation for treatment of cardiogenic shock: a meta-analysis of controlled trials. Eur Heart J. 2009;30(17):2102–8. doi: 10.1093/eurheartj/ehp292. [DOI] [PubMed] [Google Scholar]
- 11.Thiele H, Jobs A, Ouweneel DM, Henriques JPS, Seyfarth M, Desch S et al. Percutaneous short-term active mechanical support devices in cardiogenic shock: a systematic review and collaborative meta-analysis of randomized trials. Eur Heart J. 2017;38(47):3523–31. doi: 10.1093/eurheartj/ehx363. [DOI] [PubMed] [Google Scholar]
- 12.Muller G, Flecher E, Lebreton G, Luyt CE, Trouillet JL, Brechot N et al. The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive Care Med. 2016;42(3):370–8. doi: 10.1007/s00134-016-4223-9. [DOI] [PubMed] [Google Scholar]
- 13.Combes A, Leprince P, Luyt CE, Bonnet N, Trouillet JL, Leger P et al. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med. 2008;36(5):1404–11. doi: 10.1097/CCM.0b013e31816f7cf7. [DOI] [PubMed] [Google Scholar]
- 14.El Sibai R, Bachir R, El Sayed M. ECMO use and mortality in adult patients with cardiogenic shock: a retrospective observational study in U.S. hospitals. BMC Emerg Med. 2018;18(1):20. doi: 10.1186/s12873-018-0171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD et al. Extracorporeal Life Support Organization Registry international report 2016. ASAIO J. 2017;63(1):60–7. doi: 10.1097/MAT.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 16.Griffith BP, Anderson MB, Samuels LE, Pae WE, Jr, Naka Y, Frazier OH. The RECOVER I: a multicenter prospective study of Impella 5.0/LD for postcardiotomy circulatory support. J Thorac Cardiovasc Surg. 2013;145(2):548–54. doi: 10.1016/j.jtcvs.2012.01.067. [DOI] [PubMed] [Google Scholar]
- 17.Lima B, Kale P, Gonzalez-Stawinski GV, Kuiper JJ, Carey S, Hall SA. Effectiveness and safety of the Impella 5.0 as a bridge to cardiac transplantation or durable left ventricular assist device. Am J Cardiol. 2016;117(10):1622–8. doi: 10.1016/j.amjcard.2016.02.038. [DOI] [PubMed] [Google Scholar]
- 18.Lemaire A, Anderson MB, Lee LY, Scholz P, Prendergast T, Goodman A et al. The Impella device for acute mechanical circulatory support in patients in cardiogenic shock. Ann Thorac Surg. 2014;97(1):133–8. doi: 10.1016/j.athoracsur.2013.07.053. [DOI] [PubMed] [Google Scholar]
- 19.Hall SA, Uriel N, Carey SA, Edens M, Gong G, Esposito M et al. Use of a percutaneous temporary circulatory support device as a bridge to decision during acute decompensation of advanced heart failure. J Heart Lung Transplant. 2018;37(1):100–6. doi: 10.1016/j.healun.2017.09.020. [DOI] [PubMed] [Google Scholar]
- 20.Bansal A, Bhama JK, Patel R, Desai S, Mandras SA, Patel H et al. Using the minimally invasive Impella 5.0 via the right subclavian artery cutdown for acute on chronic decompensated heart failure as a bridge to decision. Ochsner J. 2016;16(3):210–6. [PMC free article] [PubMed] [Google Scholar]
- 21.Cheng R, Tank R, Ramzy D, Azarbal B, Chung J, Esmailian F et al. Clinical outcomes of Impella microaxial devices used to salvage cardiogenic shock as a bridge to durable circulatory support or cardiac transplantation. ASAIO J. 2019;65(7):642–8. doi: 10.1097/MAT.0000000000000877. [DOI] [PubMed] [Google Scholar]
- 22.Abiomed, Inc Impella ventricular support systems for use during cardiogenic shock and high-risk PCI: instructions for use and clinical reference manual 2018. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140003S018D.pdf.
- 23.Carroll BJ, Shah RV, Murthy V, McCullough SA, Reza N, Thomas SS et al. Clinical features and outcomes in adults with cardiogenic shock supported by extracorporeal membrane oxygenation. Am J Cardiol. 2015;116(10):1624–30. doi: 10.1016/j.amjcard.2015.08.030. [DOI] [PubMed] [Google Scholar]
- 24.Spinar J, Parenica J, Vitovec J, Widimsky P, Linhart A, Fedorco M et al. Baseline characteristics and hospital mortality in the Acute Heart Failure Database (AHEAD) main registry. Crit Care. 2011;15(6):R291. doi: 10.1186/cc10584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Doersch KM, Tong CW, Gongora E, Konda S, Sareyyupoglu B. Temporary left ventricular assist device through an axillary access is a promising approach to improve outcomes in refractory cardiogenic shock patients. ASAIO J. 2015;61(3):253–8. doi: 10.1097/MAT.0000000000000222. [DOI] [PMC free article] [PubMed] [Google Scholar]


