Abstract
Background.
The rate with which attention deficit/hyperactivity disorder (ADHD) is diagnosed varies widely across countries, suggesting that cultural factors influence the clinical interpretation of child behaviour. This study estimated the point prevalence of severe ADHD among elementary and middle-school Italian children.
Method.
An epidemiological sample of 2016 children attending 2nd–8th grade in the Italian regions of Tuscany and Latium was selected based on census distribution of the school-age population. Teachers completed the Italian version of the ADHD Rating Scale for Teachers (SDAI). For children with at least six inattention symptoms and/or at least six hyperactivity/impulsivity symptoms rated ‘very often’ by the teachers, the parents completed the Italian ADHD Rating Scale for Parents (SDAG). Children with documented ADHD symptoms at both school and home received a complete psychiatric interview with the Kiddie Schedule for Affective Disorders and Schizophrenia-present and lifetime version (K-SADS-PL).
Results.
Of the 1887 assessed children, 4.45% (95% CI 3.58–5.51) met the ADHD cut-off on teacher ratings, 1.43% (0.96–2.12) had ADHD symptoms endorsed by both teacher and parent, and 1.32% (0.87–1.97) were further confirmed by the psychiatric evaluation. The male:female ratio was 7:1. The inattentive type accounted for about half of the ADHD cases.
Conclusions.
When applying stringent criteria for both severity and pervasiveness of symptoms, it is estimated that about 1.3% of the Italian elementary and middle-school children suffer from severe ADHD.
Key words: Attention deficit/hyperactivity disorder, children, Italy, prevalence
Introduction
Attention deficit/hyperactivity disorder (ADHD) is a disorder characterised by developmentally inappropriate and functionally impairing levels of inattention and/or hyperactivity and impulsivity. ADHD becomes typically evident in the first decade of life, and tends to persist through adolescence and adulthood (Swanson et al. 1998). Despite extensive research, there is continuous debate on both the validity and prevalence of ADHD (Singh, 2008). The use of medications to treat ADHD has been rapidly increasing worldwide, a phenomenon that has raised concern about the appropriateness and safety of this practice (Dalsgaard et al. 2013; Thomas et al. 2014). Although neurobiological correlates of ADHD, such as delayed maturation of the brain prefrontal cortex, have been documented (Shaw et al. 2012), there is currently no biological marker that can be used for diagnostic purposes. Thus, ADHD remains a clinical diagnosis that is largely based on the observation of the child's behaviour by parents and teachers.
The prevalence of ADHD is estimated to be about 5% worldwide, but with a large variability that is mainly attributed to differences in diagnostic and ascertainment methods (Polanczyk et al. 2007, 2014). In the USA, rates of 8.7 and 15.5% have been reported (Froehlich et al. 2007; Rowland et al. 2013). Such unexpectedly and increasingly high rates raise concern about the specificity of the assessment methods. Even if the validity of the ADHD construct has been proven regardless of cultural characteristics (Rohde et al. 2005; Buitelaar et al. 2006), the actual application of the diagnosis to community care is strongly influenced by cultural factors (Skounti et al. 2007).
In fact, the presence of the core symptoms of inattention, hyperactivity and/or impulsivity does not per se result in a diagnosis of ADHD, unless these behaviours are deemed by parents and teachers to cause functional impairment. Thus, even if the distribution of objectively measured behaviours relevant to ADHD in the population is consistent across countries and cultures, the critical factor is whether their presence is considered sufficiently extreme and impairing by parents and educators to be considered abnormal.
Over the past 30 years, the more restrictive nosological construct of hyperkinetic disorder of the International Classification of Diseases (ICD) has been largely replaced by the broader criteria of the Diagnostic and Statistical Manual of Mental Disorder (DSM) (Taylor & Sonuga-Barke, 2008). Hyperkinetic disorder can be considered a subset of ADHD, probably accounting for about one-fourth of children clinically treated for ADHD of hyperactive or combined type (Santosh et al. 2005). While the DSM is dominant in the USA, European psychiatry is still influenced, to varying degrees, by the more conservative criteria, thus leading to substantial differences in the rate with which ADHD is diagnosed and managed in clinical practice. The rate of diagnosis is also influenced by differences in the educational systems, as ADHD is considered reason for receiving special education in some countries but not in others (Al-Yagon et al. 2013).
Not surprisingly, differences in diagnostic threshold carry important clinical implications for treatment. There are striking differences worldwide in the use of medications for the treatment of ADHD. In the USA, it was estimated that 3.5% of the population under age 19 received stimulant medications in 2008 (Zuvekas & Vitiello, 2012), and a more recent study has reported that 6.1% of children aged 4–17 years were taking medication for ADHD in 2011 (Visser et al. 2014). In striking contrast, the paediatric use of stimulant medications is <1% in Italy or France (Frauger et al. 2011). Multiple factors probably contribute to these discrepancies, including, among the others, differences in nosology, healthcare and education systems, drug regulatory policy and general attitude of the public towards the use of medications in children (Vitiello, 2008). Among these factors, the interpretation of the child behaviour by parents and teachers as abnormal, and hence in need of treatment, plays a critical role (Moffitt & Melchior, 2007).
Italy is one of the economically developed countries with the lowest use of medications for ADHD. Only a few studies have attempted to evaluate the rate of ADHD in Italian children. A pilot epidemiological study estimated that 3.9% of 4th grade students were ‘likely cases’ of ADHD based only on teacher ratings (Gallucci et al. 1993). In a sample of first graders in Italy, teachers endorsed symptom criteria for ADHD in 7.1% of the children (3.5% with inattentive subtype and 3.6% with hyperactive or combined subtype) (Mugnaini et al. 2006). Parent ratings, however, were not obtained, and, as underscored by the authors of this study, the real prevalence of the disorder is likely to be lower. It is remarkable that an epidemiological study of Italian adolescents (age 10–14 years) found that the overall prevalence of mental disorders (8.2%) was similar to that reported in other European countries, but the prevalence of externalising disorders, which also includes ADHD, was only 1.2% (Frigerio et al. 2009). More recently, in a sample of elementary and middle school population in Syracuse, Italy, the prevalence of ADHD was estimated to be 3%, with most of the cases meeting criteria for the combined or hyperactive type, and about a quarter for the inattentive type (Bianchini et al. 2013).
There is evidence that the population rate of ADHD varies widely based on the diagnostic criteria and the ascertainment methods used (Skounti et al. 2007; Rowland et al. 2013). In particular, the cut-off chosen for symptom endorsement is a key factor. It is conventionally accepted that a manifestation of inattention or hyperactivity that occurs ‘often’ in the eyes of the teacher or the parent qualifies for a symptom of ADHD and therefore counts towards the diagnosis. However, the increasing rate of ADHD reported in epidemiological studies over recent years suggests that the current criteria may be too broad. In particular, concern has been raised that many of the children diagnosed with ADHD in the community have only mild or moderate symptoms, and that some of those diagnosed may not meet the full diagnostic criteria for the disorder (Thomas et al. 2014).
The clinical interpretation of mild symptoms is more likely to be influenced by contextual and cultural factors than that of severe hyperactivity, impulsivity or inattention, which can be more clearly recognised as abnormal. A focus on severe ADHD can help targeting treatment intervention to those most in need while minimising inappropriate exposure to medications. Based on current clinical guidelines, pharmacotherapy is especially indicated for severe ADHD (National Institute for Health and Clinical Excellence, 2013).
The purpose of this study was to assess the prevalence of severe ADHD using an epidemiological sample of Italian school children by adopting extremely stringent criteria for symptom endorsement. The aim was to estimate the proportion of children with unquestionably abnormal levels of inattentive and/or hyperactive and impulsive behaviour, for which treatment would be clearly indicated.
Methods
Sample selection and characteristics
An epidemiological sample of 2016 children was derived from 17 elementary and middle public schools in the Italian regions of Tuscany and Latium. The schools were selected according to the Italian population census, which indicated that 67.02% of children under age 15 lived in municipalities with <50 000 inhabitants, 18.50% in municipalities between 50 000 and 250 000 inhabitants, and 14.46% in municipalities with over 250 000 inhabitants, and that 45.01% of Italian students attended schools with <250 students (Istituto Nazionale di Statistica, 1995; Italian Ministry of Public Education, 2000). Within these schools, a representative sample for grades 2–8 was randomly obtained, reflecting an equal distribution of children attending these grades in the Italian population (Italian Ministry of Public Education, 2000).
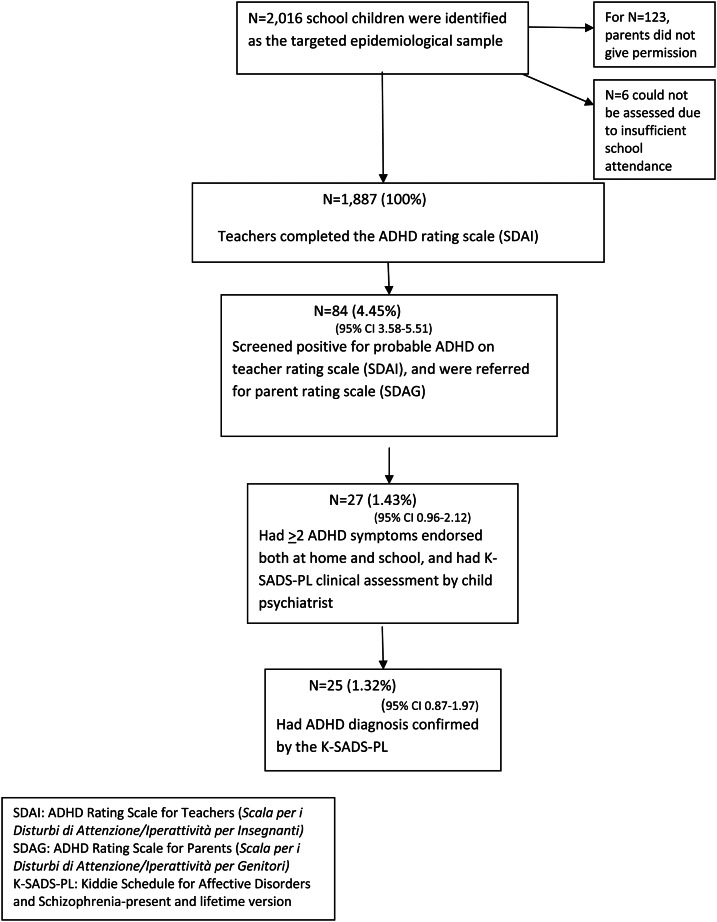
The study was approved by the relevant school districts. Written informed consent was requested from the parents to assess their child in school. Of the 2016 parents contacted, 1893 (93.9%) gave permission. Teachers completed rating scales for 1887 children (Fig. 1 and Table 1). All the data were collected in the school year 2002–2003.
Fig. 1.
Study's steps and subject flow.
Table 1.
Sample characteristics
| N | % | |
|---|---|---|
| Total | 1887 | 100 |
| Males | 924 | 48.97 |
| Females | 963 | 51.03 |
| From municipalities with: | ||
| < 50 000 people | 1,188 | 62.96 |
| 50 000–250 000 people | 415 | 21.99 |
| >250 000 people | 284 | 15.05 |
| School grade:a | ||
| 2 | 256 | 13.57 |
| 3 | 243 | 12.88 |
| 4 | 252 | 13.35 |
| 5 | 271 | 14.36 |
| 6 | 325 | 17.22 |
| 7 | 303 | 16.06 |
| 8 | 237 | 12.56 |
aThe proportion of males within the grades ranged from 46.81 to 54.38%.
Procedures and assessments
At the first step, the teachers of the 1893 children for whom parental permission was granted were asked to complete the Italian version of the ADHD Rating Scale for Teachers (Scala per i Disturbi di Attenzione/Iperattività per Insegnanti or SDAI) (Cornoldi et al. 1996; DuPaul et al. 1997). The SDAI Scale asks the teacher to rate on a 4-point scale the frequency/intensity of the each of the nine symptoms of inattention and the nine symptoms for hyperactivity/impulsivity reported of the Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV; American Psychiatric Association, 1994). Each symptom can be scored as ‘never or rarely’, ‘sometimes’, ‘often’ or ‘very often’. The SDAI has demonstrated excellent inter-rater reliability and test–retest reliability (Marzocchi & Cornoldi, 2000).
At the second step, the parents of the children with at least six inattentive symptoms and/or at least six hyperactivity/impulsivity type scored as present ‘very often’ were asked to complete the parent version of the ADHD rating scale (Scala per i Disturbi di Attenzione/Iperattività per Insegnanti or SDAG) (Cornoldi et al. 1996), which is structured in the same way as the SDAI.
Last, children with at least six inattentive symptoms and/or at least six hyperactivity/impulsivity type scored as present ‘very often’ by the teacher and at least two of these symptoms scored to be present ‘very often’ also by the parent were further assessed with a comprehensive in person psychiatric evaluation. Each child and parent were separately administered the Italian version of the Kiddie Schedule for Affective Disorders and Schizophrenia-present and lifetime version (K-SADS-PL, Kaufman et al. 1997). The K-SADS-PL is a semi-structured psychiatric interview to assess the presence of the most common psychiatric disorders. The K-SADS-PL was administered by an experienced child psychiatrist trained in the use of this diagnostic instrument (RD). Children's intelligence level was measured by Wechsler Intelligence Scale for Children-Revised (WISC-R), and an IQ < 70 was an exclusion criterion from a diagnosis of ADHD. Other exclusion criteria were: a diagnosis of bipolar disorder, major depression, dysthymic disorder, schizophrenia, developmental pervasive disorder or generalised anxiety disorder. Functional impairment was assessed using Children's Global Assessment Scale (CGAS), on a scale from 0 (severe impairment) to 100 (superior functioning), with a score below 70 indicating clinically the significant dysfunction (Shaffer et al. 1983). The Strengths and Difficulties Questionnaire (SDQ) was completed by the teachers and parents (Goodman et al. 2000).
To evaluate the sensitivity of the ascertainment process for ADHD, a sample of 102 children (mean age 8.9 years) and their parents, randomly selected from the children with a negative teacher ADHD rating scale (SDAI) score, were interviewed with the K-SADS PL 1.0. Of them, none met the criteria for ADHD. Inter-rater reliability of the K-SADS-PL interviewers was assessed on a sample of 87 children. The agreement between the interviewers was 89.66%., and the Cohen's kappa coefficient for the diagnosis of ADHD was 0.81.
Data analysis
Descriptive statistics was applied to the data. The number and percentage of children exceeding the set cut-off scores on the SDAI, both SDAI and SDAG and further meeting criteria for ADHD on the K-SADS-PL were computed. Within the subgroup of children with ADHD on the K-SADS-PL, the prevalence of ADHD subtypes and abnormal scores on the parent and teacher SDQ and clinician C-GAS scores were examined.
A conservative approach to missing data was adopted. Of the parents who were requested to complete the SDAG, 5.56% were failed to return the forms, and 8.82% of the parent SDQ forms were similarly missing. In the absence of parent information, a diagnosis of ADHD could not be formulated, and these children were accounted as non-ADHD cases.
Results
Figure 1 and Table 2 summarise the study steps, subject flow and main findings. Of the 2016 children included in the epidemiologically selected sample, 123 children could not be assessed because their parents did not give permission, and other six children could not be assessed because they had been absent from school for extended periods of time. A total of 1887 children (93.6% of the selected sample) were assessed on the ADHD Rating Scale for Teachers (SDAI).
Table 2.
Rate of ADHD by assessment step (N = 1887)
| ADHD | Male/Female | Inattentive type of ADHD | Hyperactive type of ADHD | Combined type of ADHD | 2nd–5th school grade (N = 1022) | 6nd–8th school grade (N = 865) | |
|---|---|---|---|---|---|---|---|
| N (%) (95% CI) | N (ratio) | N (%) (95% CI) | N (%) (95% CI) | N (%) (95% CI) | N (%) (95% CI) | N (%) (95% CI) | |
| Teacher ADHD Rating Scale (SDAI) | 84 (4.45) (3.58–5.51) | 73/11 (7:1) | 51 (2.70) (2.04–3.56) | 18 (0.95) (0.58–1.53) | 15 (0.79) (0.46–1.33) | 65 (6.36) (4.98–8.08) | 19 (2.20) (1.37–3.48) |
| Teacher & Parent Rating Scales (SDAI + SDAG) | 27 (1.43) (0.96–2.12) | 23/4 (7:1) | 19 (1.01) (0.65–1.57) | 4 (0.21) (0.07–0.58) | 4 (0.21) (0.07–0.58) | 21 (2.05) (1.31–3.17) | 6 (0.69) (0.28–1.58) |
| Confirmed by Psychiatric Interview (SDAI + SDAG + K-SADS) | 25 (1.32) (0.87–1.97) | 22/3 (7:1) | 12 (0.64) (0.35–1.15) | 3 (0.16) (0.04–0.51) | 10 (0.53) (0.27–1.01) | 20 (1.96) (1.23–3.07) | 5 (0.58) (0.21–1.43) |
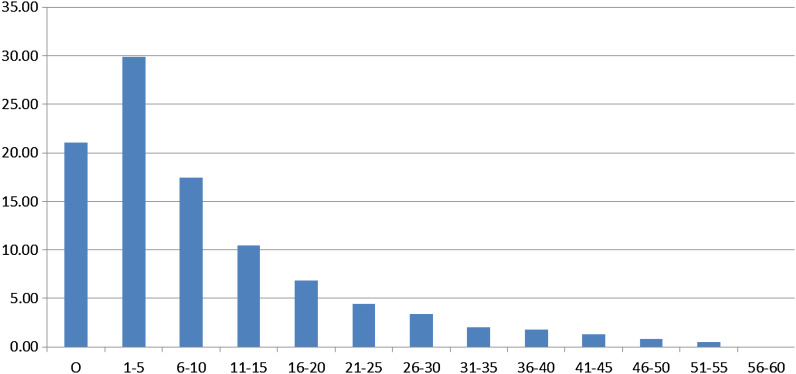
The distribution of the SDAI total score in the sample followed a positively, right skewed distribution (Fig. 2). In total 78% of the children had at least one ADHD-relevant behaviour rated by the teacher to be present ‘sometimes’; 39% had at least one behaviour rated ‘often’; and 6% had at least one behaviour rated ‘very often’.
Fig. 2.
Frequency distribution of total scores of ADHD rating scale for teachers (SDAI) (N = 1887).
Of the 1887 children assessed, 4.45% (95% CI 3.58–5.51) met the number and severity of symptoms for ADHD in the school setting (based on teacher rating); 1.43% (95% CI 0.96–2.12) had also severe symptoms at home (based on both teacher and parent ratings), thus meeting the diagnostic criterion of pervasiveness across more than one setting; and 1.32% (95% CI 0.87–1.97) had their diagnosis of ADHD confirmed by a comprehensive psychiatric evaluation by a child psychiatrist.
Among the children who screened positive on both the teacher and parent ADHD ratings, the psychiatric evaluation did not confirm the diagnosis in three cases: in two cases the symptoms could be better explained by another, non-ADHD, condition, and in one case the full criteria for ADHD were not met because there was no clear-cut evidence of dysfunction.
The prevalence of severe ADHD was 1.96% (95% CI 1.23–3.07) among elementary school children, and 0.58% (95% CI 0.21–1.43) among middle school children. The male/female ratio was 7:1. The demographic and clinical characteristics of the children with severe ADHD are summarised in Table 3. They had C-GAS scores ranging between 40 and 60, which are indicative of clinically significant impairment in global functioning. All had SDQ-teacher abnormal scores, and 19 had SDQ-parent abnormal scores, further documenting functional impairment. ADHD-inattentive type was documented in 12 (48%) of the cases, and ADHD hyperactive or combined type in the other 13 (52%). Sixteen (52%) met the DSM-IV criteria for oppositional defiant disorder and four of these also for conduct disorder.
Table 3.
Characteristics of the identified ADHD samplea
| Total N | 25 (100%) |
| Age (year, mean ± s.d.) | 9.58 ± 1.84 |
| Male (N) | 23 (92%) |
| IQ (mean ± s.d.) | 96.85 ± 15.53 |
| ADHD-inattentive (N) | 12 (48%) |
| ADHD-hyperactive | 3 (12%) |
| ADHD-combined | 10 (40%) |
| With ODDb | 16c (64%) |
aADHD, diagnosed by psychiatric interview based on K-SADS-PL.
bODD, oppositional defiant disorder.
cOf these, 14 were male. Four (all male) also met criteria for conduct disorder.
Discussion
By examining an epidemiological sample of elementary and middle school children in two regions of Italy, and requiring extremely stringent criteria for the endorsement of ADHD-relevant symptoms by both teachers and parents, with final confirmation after a clinical assessment with a child psychiatrist, we estimated that about 1.3% of children suffer from severe ADHD. These children are functionally impaired as documented by CGAS scores in the 40–60 range. This is a conservative estimate because of the requirement that each ADHD symptom be present ‘very often’ based on both teacher and parent report. Not surprisingly, the rate is much lower than reported in other studies that used the DSM-III-R or DSM-IV criteria with the usual cut-off of ‘often’ for presence of ADHD symptoms. By sacrificing diagnostic sensitivity, we have aimed at maximising specificity and therefore avoiding false-positive diagnoses. Focus on severe ADHD can help in planning for more targeted treatment interventions.
Our data confirm that ADHD symptoms are continuously distributed in the population (Fig. 2), so that any cut-off for disorder identification can be considered arbitrary. By selecting ‘very often’ to endorse the presence of each symptom, the likelihood of false positive was minimised. In fact, a score of ‘often’ for at least one item of the ADHD Rating Scale for Teachers (SDAI) was found for 39% of the surveyed children, whereas a score of ‘very often’ for a least one item was found only in 6% of them. By requiring that severe ADHD symptoms may also be present in non-school setting as documented by the ADHD Rating Scale for Parents (SDAG), we ensured the pervasiveness of the condition. Two-thirds of the children meeting the strict criteria by teacher rating did not qualify for pervasiveness of severe ADHD symptoms based on parent rating (Fig. 1).
The 1.3% rate of severe ADHD in this study is similar to the prevalence of hyperkinetic disorder, a nosological construct commonly used before the advent of the DSM criteria of ADHD (Taylor et al. 2004). A diagnosis of hyperkinetic disorder requires the concurrent presence of all three in the core domains of ADHD (i.e., hyperactivity, impulsivity and inattention) and the exclusion of any comorbid condition. The 7:1 male/female ratio for severe ADHD in this study is remarkable. That ADHD is substantially higher in boys and has been consistently documented across studies and countries, but usually with a rate of about 3:1. The data indicate that the male/female ratio increases with the severity of the condition. It should be noted that about half of the children identified with severe ADHD had predominantly inattentive symptoms (Table 3). These data do not obviously rule out that prominent, although not extremely severe, hyperactivity and impulsivity were concomitantly present in these children, but point to the relevance of inattention as a severe cause of impairment in a subset of children. These results also confirm the developmental nature of ADHD, with attenuation of the symptoms as children grow into adolescence.
The study sample was epidemiologically derived and based on the distribution of the school-age population in the targeted geographical area of Tuscany and Latium. Although limited to two regions, the data are likely informative at the Italian national level given the common cultural characteristics and the same educational and health care system across the entire country. Several limitations of the study should be acknowledged. First, the data were collected in 2002–2003 and only recently analysed. Despite the 10-year hiatus, however, it seems unlikely that the rate could have changed during this period as a recent systematic review and meta-regression analyses of data across the past 3 decades have found no evidence of a historical increase in the population prevalence of ADHD when consistent and validated assessment methods are used (Polanczyk et al. 2014). Second, because of funding limitations for this study, a more detailed examination of the sample or inquiry into the use of different symptom cut-offs could not be done.
It should also be noted that there is currently no universally agreed upon definition of severe ADHD (Thomas et al. 2014). Neither the American nor the Australian diagnostic guidelines operationalise the criteria for severity, and the UK National Institute for Health and Clinical Excellence (NICE) guidelines equalise severe ADHD to hyperkinetic disorder (National Institute for Health and Clinical Excellence, 2013).
More than 20 years ago, it was observed that the diagnosis of ADHD ‘is seldom, if ever, made by clinicians in Italy’ and that ‘psychostimulants generally considered to be an important, if not the primary treatment for ADHD, are not available in the Italian pharmacopoeia’ (Gallucci et al. 1993). In fact, no pharmacological treatment of ADHD was available in Italy until 2007, when methylphenidate and atomoxetine were introduced but subjected to strict prescribing regulations through enrolment into a national registry (Arcieri et al. 2012). In the first 3 years (2007–2010), only 1758 were enrolled in the registry vis-à-vis a population of about 7 million children and adolescents aged 6–18 years (Arcieri et al. 2012).
The data from this study indicate that, even if extremely conservative criteria are applied, about 1.3% of school-age children suffer from severe symptoms of ADHD that are pervasive, frequently accompanied by comorbid behavioural disturbance, and associated with clinically significant functional impairment. The impairment is global and not limited to school setting. Given the level of dysfunction, treatment is clearly indicated. While there is no cure for ADHD, symptoms can be successfully managed, and a number of evidence-based treatment modalities are available, including psychosocial and pharmacological interventions.
Financial Support
This study received no specific grant funding, but was supported by resources within the Italian National Health System.
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human research.
References
- Al-Yagon M, Cavendish W, Cornoldi C, Fawcett AJ, Grünke M, Hung LY, Jiménez JE, Karande S, van Kraayenoord CE, Lucangeli D, Margalit M, Montague M, Sholapurwala R, Sideridis G, Tressoldi PE, Vio C (2013). The proposed changes for DSM-5 for SLD and ADHD: international perspectives – Australia, Germany, Greece, India, Israel, Italy, Spain, Taiwan, United Kingdom, and United States. Journal of Learning Disabilities 46, 58–72. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association: Washington, DC. [Google Scholar]
- Arcieri R, Germinario EA, Bonati M, Masi G, Zuddas A, Vella S, Chiarotti F, Panei P, Italian Attention-Deficit/Hyperactivity Disorder Regional Reference Centers (2012). Cardiovascular measures in children and adolescents with attention-deficit/hyperactivity disorder who are new users of methylphenidate and atomoxetine. Journal of Child and Adolescent Psychopharmacology 22, 423–431. [DOI] [PubMed] [Google Scholar]
- Bianchini R, Postorino V, Grasso R, Santoro B, Migliore S, Burlò C, Tata C, Mazzone L (2013). Prevalence of ADHD in a sample of Italian students: a population-based study. Research in Developmental Disabilities 34, 2543–2550. [DOI] [PubMed] [Google Scholar]
- Buitelaar JK, Barton J, Danckaerts M, Friedrichs E, Gillberg C, Hazell PL, Hellemans H, Johnson M, Kalverdijk LJ, Masi G, Michelson D, Revol O, Sebastian JS, Zhang S, Zuddas A (2006). A comparison of North American versus non-North American ADHD study populations. European Child and Adolescent Psychiatry 15, 177–181. [DOI] [PubMed] [Google Scholar]
- Cornoldi C, Gardinale M, Masi A, Petteno L (1996). Impulsività e autocontrollo. Erickson: Trento, Italy. [Google Scholar]
- Dalsgaard S, Nielsen HS, Simonsen M (2013). Five-fold increase in national Prevalence Rates of attention-deficit/hyperactivity disorder medications for children and adolescents with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other psychiatric disorders: a Danish register-based study. Journal of Child and Adolescent Psychopharmacology 23, 432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey KE, Ikeda MJ (1997). Teacher ratings of Attention-Deficit/Hyperactivity Disorder symptoms: factor structure and normative data. Psychological Assessment 9, 436–444. [DOI] [PubMed] [Google Scholar]
- Frauger E, Pauly V, Natali F, Pradel V, Reggio P, Coudert H, Thirion X, Micallef J (2011). Patterns of methylphenidate use and assessment of its abuse and diversion in two French administrative areas using a proxy of deviant behaviour determined from a reimbursement database: main trends from 2005 to 2008. CNS Drugs 25, 415–424. [DOI] [PubMed] [Google Scholar]
- Frigerio A, Rucci P, Goodman R, Ammaniti M, Carlet O, Cavolina P, De Girolamo G, Lenti C, Lucarelli L, Mani E, Martinuzzi A, Micali N, Milone A, Morosini P, Muratori F, Nardocci F, Pastore V, Polidori G, Tullini A, Vanzin L, Villa L, Walder M, Zuddas A, Molteni M (2009). Prevalence and correlates of mental disorders among adolescents in Italy: the PrISMA study. European Child & Adolescent Psychiatry 18, 217–226. [DOI] [PubMed] [Google Scholar]
- Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS (2007). Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Archives of Pediatric and Adolescent Medicine 161, 857–864. [DOI] [PubMed] [Google Scholar]
- Gallucci F, Bird HR, Berardi C, Gallai V, Pfanner P, Weinberg A (1993). Symptoms of attention-deficit hyperactivity disorder in an Italian school sample: findings of a pilot study. Journal of the American Academy of Child and Adolescent Psychiatry 32, 1051–1058. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H (2000). Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. British Journal of Psychiatry 177, 534–539. [DOI] [PubMed] [Google Scholar]
- Istituto Nazionale di Statistica (1995). 13° Censimento Generale della Popolazione e delle Abitazioni – 20 ottobre 1991. Istituto Nazionale di Statistica: Rome, Italy. [Google Scholar]
- Italian Ministry of Public Education (2000). La Scuola Statale: Sintesi dei Dati. Rome, Italy. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Marzocchi GM, Cornoldi C (2000). Una scala di facile uso per la rilevazione dei comportamenti problematici dei bambini con Deficit di Attenzione e Iperattività . Psicologia Clinica dello Sviluppo 4, 43–63. [Google Scholar]
- Moffitt TE, Melchior M (2007). Why does the worldwide prevalence of childhood attention deficit hyperactivity disorder matter? American Journal of Psychiatry 164, 856–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugnaini D, Masi G, Brovedani P, Chelazzi C, Matas M, Romagnoli C, Zuddas A (2006). Teacher reports of ADHD symptoms in Italian children at the end of first grade. European Psychiatry 21, 419–426. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (2013). Attention deficit hyperactivity disorder. Diagnosis and management of ADHD in children, young people, and adults. Issued September 2008; last modified: March 2013. NICE clinical guideline 72. Retrieved 17 July 2014 from http://www.nice.org.uk/guidance/CG72
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American Journal of Psychiatry 164, 942–948. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA (2014). ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis International Journal of Epidemiology 43, 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde LA, Szobot C, Polanczyk G, Schmitz M, Martins S, Tramontina S (2005). Attention-deficit/hyperactivity disorder in a diverse culture: do research and clinical findings support the notion of a cultural construct for the disorder? Biological Psychiatry 57, 1436–1441. [DOI] [PubMed] [Google Scholar]
- Rowland AS, Skipper BJ, Umbach DM, Rabiner DL, Campbell RA, Naftel AJ, Sandler DP (2013). The Prevalence of ADHD in a Population-Based Sample. Journal of Attention Disorders. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santosh PJ, Taylor E, Swanson J, Wigal T, Chuang S, Davies M, Greenhill L, Newcorn J, Arnold LE, Jensen P, Vitiello B, Elliott G, Hinshaw SP, Hechtman L, Abikoff H, Pelham WE, Hoza B, Molina B, Wells K, Epstein J, Posner M (2005). Refining the diagnoses of inattention and overactivity syndromes: a reanalysis of the Multimodal Treatment study of attention deficit hyperactivity disorder (ADHD) based on ICD-10 criteria for hyperkinetic disorder. Clinical Neuroscience Research 5, 307–314. [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S (1983). A children's global assessment scale (CGAS). Archives General Psychiatry 40, 1228–1231. [DOI] [PubMed] [Google Scholar]
- Shaw P, Malek M, Watson B, Sharp W, Evans A, Greenstein D (2012). Development of cortical surface area and gyrification in attention-deficit/hyperactivity disorder. Biological Psychiatry 72, 191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh I (2008). Beyond polemics: science and ethics of ADHD. Nature Review Neuroscience 9, 957–964. [DOI] [PubMed] [Google Scholar]
- Skounti M, Philalithis A, Galanakis E (2007). Variations in prevalence of attention deficit hyperactivity disorder worldwide. European Journal of Pediatrics 166, 117–123. [DOI] [PubMed] [Google Scholar]
- Swanson JM, Sergeant JA, Taylor E, Sonuga-Barke EJ, Jensen PS, Cantwell DP (1998). Attention-deficit hyperactivity disorder and hyperkinetic disorder. Lancet 351, 429–433. [PubMed] [Google Scholar]
- Taylor E, Sonuga-Barke E (2008). Disorders of attention and activity. In Rutter's Child and Adolescent Psychiatry, 5th edn (ed. Rutter M. et al. ), pp. 521–542. Blackwell Publishing: Oxford, UK. [Google Scholar]
- Taylor E, Döpfner M, Sergeant J, Asherson P, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Rothenberger A, Sonuga-Barke E, Steinhausen HC, Zuddas A (2004). European clinical guidelines for hyperkinetic disorder – first upgrade. European Child and Adolescent Psychiatry 13(Suppl. 1), I7–I30. [DOI] [PubMed] [Google Scholar]
- Thomas R, Mitchell GK, Batstra L (2014). Attention-deficit/hyperactivity disorder: are we helping or harming? Brisitsh Medical Journal 347, f6172. [DOI] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child and Adolescent Psychiatry 53, 34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello B (2008). An international perspective on pediatric psychopharmacology. International Review of Psychiatry 20, 121–126. [DOI] [PubMed] [Google Scholar]
- Zuvekas SH, Vitiello B (2012). Stimulant medication use among US children: a twelve-year perspective. American Journal of Psychiatry 169, 160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]