Abstract
Background.
This paper aims to present the Integrated Atlas of Mental Health of Catalonia (2010) focusing on: (a) the importance of using a taxonomy-based coding and standard system of data collection when assessing health services; and (b) its relevance as a tool for evidence-informed policy.
Method.
This study maps all the care-related services for people with mental disorders available in Catalonia in 2010, using the ‘Description and Evaluation of Services and Directories in Europe for long-term care’ (DESDE-LTC). The unit of analysis is the Basic Stable Input of Care (BSIC), which is the minimal organisation unit composed by a set of inputs with temporal stability. We presented data on: (a) availability of BSICs and their capacity; (b) the adequacy of the provision of care, taking into account availability and accessibility; (c) the evolution of BSCIs from 2002 to 2010; and (d) the perceived relevance of Atlas of Mental Health as a tool for evidence-informed policy.
Results.
We identified a total of 639 BSICs. A lack of Health services was detected in highly rural areas, although there was moderate availability of Social Services. Overall, more than 80% of the small mental health areas in Catalonia had an adequate core mental health service. Since 2002 the availability of mental health services has increased. Decision makers found the Atlas a useful and relevant tool for evidence informed policy.
Conclusions.
Policy makers can use Atlases to detect gaps and inequities in the provision of care for people with mental health needs.
Key words: Atlas of health care, evidence-informed policy, integrated care, mental health
Introduction
Evidence-informed policy infers the use of evidence-based approaches, taking into account local factors, to assess a health system challenges and to develop responses to evolving challenges and opportunities (Bosch-Capblanch et al. 2012). Measuring the quality of Mental Health Care is also crucial to reduce the burden of mental disorders (Moran et al. 2013).
Within this context, Atlases of Health are essential tools for decision-making and quality assessment. These Atlases include detailed information on social and demographic characteristics and health-related needs, as well as data on services availability and care capacity. They can also include visualisation tools such as geographic maps and graphics. Atlases of Health have been used since the 1990s, pointing out variations in care and inequities in the provision of treatments. Some examples are the Ontario Atlas of Care (Noble, 1994), the Dartmouth Atlas of Health Care (Cronenwett & Birkmeyer, 2000; Meier & Beresford, 2008) or the Mental Health Atlases produced by the World Health Organization (Saxena et al. 2002, 2006; Almeida, 2003; Berger, 2007; McBain et al. 2012).
Typically, Atlases of Health rely mainly on the lists of services based on official names. The problem of this procedure is that the word ‘service’ is an umbrella term used to describe very different components of the organisation of care. It merges highly structured services, with clinical units, or even programs and interventions. Consequently, these Atlases are not giving an accurate picture of the real availability of services. This lack of a standard classification system of health services also hinders comparisons of ‘like with like’. These are major impediments to the practical use of Atlases for evidence informed policy (Salvador-Carulla et al. 2013a).
Moreover, the current Atlases are generally focused on a traditional vision of health, and mainly take into account medical services. The development of the ‘Person-centred health model’ (Salvador-Carulla & Mezzich, 2012) and the ‘integrated care model’ (Goodwin, 2013) is changing the way health care is assessed and planned. Hence, it is important to have a global picture of all the services available, irrespective of the funding sector (i.e., Health, Social Welfare and Family, Employment, Criminal Justice). This is particularly relevant to Mental Health Care, where scarcity of resources is higher than in other areas (Knapp et al. 2006; Saxena et al. 2007). Holistic service mapping allows policy planners and decision makers to make bridges between the different sectors and to better allocate services (Salvador-Carulla & Mezzich 2012; Salvador-Carulla et al. 2012).
An example of the use of Atlases of Mental Health for Policy and Planning can be found in Catalonia. Since 2001, The Catalan Department of Health has pioneered the use of evidence-informed tools in order to better plan mental health care. Three Atlases of Mental Health have been completed (in 2002, 2006 and 2010), and includes services from the health sector, the social sector and also uses standard assessment systems [the ‘European Service mapping Schedule’ (ESMS) (Johnson et al. 2000) or the ‘Description and Evaluation of Services and Directories in Europe for long-term care’ (DESDE-LTC) (Salvador-Carulla et al. 2013a)]. The Catalan Plan On Mental Health (Available at: http://ec.europa.eu/health/archive/ph_determinants/life_style/mental/docs/ms_rgspain_en.pdf) stated that care for people with mental disorders should be delivered in an integral and coordinated way. Hence, the 2010 Atlas of Mental Health was commissioned to assess all the services providing care for people with mental disorders, irrespective of the funding sector.
This paper aims to present the (Salvador-Carulla et al. 2013b) (The Spanish version of the complete Integrated Atlas of Mental Health can be consulted here: http://www20.gencat.cat/docs/canalsalut/Home%20Canal%20Salut/Professionals/Temes_de_salut/Salut_mental/documents/pdf/memoria_atles_integral_version_castellana.pdf), focusing on: (a) the importance of using a taxonomy-based coding and standard system of data collection when assessing health services; and (b) its relevance as a tool for evidence-informed policy.
Method
Study population
Catalonia is a Spanish region or ‘autonomous community’ with a population over 7.5 million inhabitants. As a consequence of a devolution process started in 1981, the autonomous communities have full governance on health care which is universal and publicly financed (Salvador-Carulla et al. 2006).
This study maps all the care-related services for people with mental disorders, available in Catalonia in December 1st, 2010. These services provided care for all type of mental disorders. There were only two inclusion criteria: (1) at least 20% of the users may had mental disorders; and (2) the services had to be freely provided at the point of use and funded by the Department of Health (community and hospital based) or the Departments of Social Welfare and Family, Education, Employment or Criminal Justice.
Measures
The ‘DESDE-LTC’ (Salvador-Carulla et al. 2013a) is an open-access international instrument for the standardised description and classification of services for long term care (LTC) derived from the ‘ESMS’ (Johnson et al. 2000). It includes a taxonomy tree and coding system that allows the classification of services in a defined catchment area according to its main care structure/activity offered, as well as the level of availability and utilisation.
It is important to note that in services research, there are different units of analysis (i.e., large health maintenance organisations, hospital services, programmes, care packages, etc.). Comparisons must be made across a single ‘unit of analysis’ group. Our analysis, based on DESDE-LTC, is focused on the Basic Stable Inputs of Care (BSICs) (Salvador-Carulla et al. 2013a). BSICs are the minimal organisation units usually composed by a set of inputs with temporal stability arranged for delivering health-related care to a defined population in a care area. It is usually composed of an administrative unit with an organised set of structures and professionals. The typology of care provided by the BSIC is described by a smaller unit of analysis called ‘Main Type of Care’ (MTC). Every single BSIC is described using one or more codes based on the main care structure/activity offered by the service. The definition of the ‘MTCs’ coding used in the Atlas is available at the Supplementary File 1.
Selection of catchment areas
Health Care in Catalonia is organised in three levels. The highest is the Health Region (N = 7), which are divided into ‘health sectors/areas’ (N = 55). These health sectors are formed by Basic Health Areas (BHA) (N = 369). Each citizen, according to the area he/she lives, belongs to a concrete BHA. This zoning is legally defined by the regional Catalan Government. Mental health care in Catalonia is organised territorially in 74 small catchment areas coordinated by a reference Mental Health Community Centre (MHCC). The zoning is not part of the official territorial map of healthcare but is used throughout Spain to provide mental health care for all the catchment area population following the ‘sectorisation’ model of mental healthcare provision (Salvador-Carulla et al. 2010a). Services for persons with mental health disorders that are not run by the Department of Health follow other zoning divisions or are not zoned.
This paper is limited to the distribution of services in two geographical divisions: by the seven Health Regions in Catalonia, and the small mental health catchment areas of the 74 community mental health centres. Other services not funded by the Department of Health have been assigned to different Health Regions following agreement with officers from the Department of Health.
Procedure
A consortium of researchers and decision makers from The Mental Health Director Plan was created to develop the Mental Health Atlas of Catalonia. An additional independent expert panel group (N = 11), which included mental health providers and responsible for mental health from the Social Welfare and Family Department, overviewed the development of the project.
The Director of Mental Health Planning assisted the contact between the researchers and the Mental Health personnel responsible for other Departments. The researchers held face-to-face and/or phone meetings to explain the project and answer any of their questions. Subsequently, each Departmental Officer responsible for mental health provided the researchers with the list of all services delivering care for persons with mental disorders. The departmental officer also sent a letter to all providers to outline the Atlas project and seeking their collaboration. Following this initial contact, the research assistants contacted the services' responsible via e-mail and/or phone and use the DESDE-LTC instrument (Salvador-Carulla et al. 2011, 2013a) to gather data on: (a) type of activities performed by the service; and (2) service data (e.g., opening days and hours, staffing, management, economic information, legal system, user profile, number of users, number of contacts or admissions, number of days in hospital or residential structure, number of available beds or places, links with other services). The researchers used this information to code the services according to DESDE-LTC.
The data were collected between July 2010 and November 2010. The information on some services was checked again in July 2011 and February 2012 following review by the expert advisory group.
Once the Atlas was completed, seven experts from de Catalan Department of Health assessed its relevance and usefulness to support and guide the decision-making process. Scores were allocated from 0 (not relevance/useful) to 10 (highly relevant/useful).
Analysis
We described the key indicators related to social and demographic characteristics. Table 1 shows the definitions of the indicators used. We analysed the availability, placement capacity and workforce capacity of BSIC by MTC. Box 1 defines these concepts (availability and capacity). We calculated the ‘health-related balance of care’. That is, the percentage of the MTC codes directly related to health, provided by services depending of the health sector (Department of Health) and the social sector (including Department of Social Welfare and Family, Education, Employment and Criminal Justice). Supplementary file 1, describes the MTC codes considered to be directly related to health and those that are not (i.e., social care).
Table 1.
Social and demographic indicators
| Catalonia | Barcelona | Catalunya Central | Girona | Lleida | Vall D'Aran i Alt Pirineu | Camp de Tarragona | Terres de l'Ebre | |
|---|---|---|---|---|---|---|---|---|
| Density Index:Population(km2) | 234.10 | 1688.02 | 84.33 | 161.06 | 66.77 | 13.32 | 145.37 | 92.87 |
| Dependency index:(population between 0 and 15 + >64 years old/population 16–64) × 100 | 48.47 | 48.00 | 52.43 | 47.95 | 50.27 | 47.59 | 47.57 | 52.00 |
| Aging index: (population >64 years old/population 0–15) × 100 | 102.12 | 104.11 | 105.80 | 90.98 | 110.87 | 124.71 | 87.92 | 121.02 |
| Immigration rate: (total migrants/total population) × 1000 | 159.5 | 149.1 | 126.4 | 206.1 | 188.2 | 165.6 | 180.5 | 207.0 |
| Non-married rate: (population >15 years old non-married/population >15 years old) × 100 | 37.39 | 39.51 | 35.20 | 32.52 | 34.59 | 37.67 | 32.01 | 32.14 |
| People living alone rate: (number of homes with just one person/total population) × 100 | 7.69 | 7.48 | 6.86 | 9.84 | 7.07 | 11.23 | 7.79 | 6.72 |
| People > 64 years old living alone rate:(number of homes with just one person >64 years n/Population >64 years old) × 100 | 20.36 | 20.66 | 18.25 | 22.51 | 18.02 | 20.66 | 19.93 | 17.66 |
| Single Parent home rate: (number of adult people living alone with children/population >15 years old) × 100 | 1.80 | 1.80 | 1.56 | 1.99 | 1.74 | 2.84 | 1.80 | 1.32 |
| Unemployment rate: (number of unemployed people/population 16–64 years old) × 100 | 11.94 | 11.21 | 14.36 | 12.79 | 16.76 | 8.26 | 11.93 | 12.49 |
Information obtained from the Official Statistics Website of Catalonia (http://www.idescat.cat/en/) for the year 2010.
Box 1.
Definitions of availability and capacity.
Availability: Defined as the presence, location and readiness for use of services or other organisational units in a care organisation or a catchment area at a given time. A service is available when it is operable or usable upon demand to perform its designated or required function. The calculated availability rate of MTC is calculated by 100, 000 inhabitants, by Catalonia and by health region.
Placement Capacity: Maximum number of beds in residential care and of places in day care in a care delivery organisation or a catchment area at a given time. Rates have been calculated by 100, 000 inhabitants, by Catalonia and by health region.
Workforce capacity: Maximum number of staff available in a care delivery organisation or in a catchment area at a given time. Care workforce capacity usually refers to paid staff providing direct care (e.g., it excludes voluntary care providers and administrative staff). It is typically measured in Full Time Equivalents units (FTE), in this case 37.5 h per week. Rates have been calculated by 100, 000 inhabitants, by Catalonia and by health region.
Use of outpatient services: The use of outpatient services is described (treated prevalence per 1, 000 habitants and number of outpatient's visits per 1, 000 habitants), using the Minimum Data Set for Outpatient Mental Health Centres (CMBD-SMA) provided by the Catalonian Department of Health. Patient confidentially was assured using anonymous registers. Data reported in this paper is from 2002, 2006 and 2009 (data from 2010 were not available when elaborating the Atlas 2010).
We presented the percentage of small areas by health region that can be considered as adequately provided. ‘Adequacy of care provision’ was assessed taking into account the availability of core mental health services provided by the Department of Health and their accessibility in the 74 small health areas. Core mental health services are: Adult Acute Hospital (R2), Adult Subacute Care (R4 R5), Adult Medium or Long Term Stay Facilities (R4 R5 R6), Adult Acute Day care (D1), Adult Day Care Centre (D4.1,D3.2, D4.3), Adult Outpatient Care (O8–O10), Child and Adolescent Acute Day Care (D1) and Child and Adolescent (O9–O10). Then a descriptive analysis was made of the evolution of services in Catalonia, linking the results of the 2010 Mental Health Atlas with internal reports carried out in 2002 and 2006. Last, we reported the mean values for usefulness and relevance of the Mental Health Atlas according to different Catalan experts involved in Public Health Planning and Decision Making. Experts were purposively contacted (N = 7).
Results
Describing Catalonia: key indicators
Table 1 shows key demographic indicators. There is a substantial variability in these indicators across the different health regions in Catalonia. Briefly, population density ranged from 13.32 habitants per square kilometre in the highly rural ‘Vall d'Aran i Alt Pirineu’ to 1688.02 habitants per square kilometre in ‘Barcelona’. Highest dependency ratios were found in ‘Catalunya Central’ and ‘Terres de l'Ebre’. The oldest population was found in ‘Vall d'Aran i Alt Pirineu’. In this Health Region, there were higher rates of people living alone and single parent households. The highest per cent of migrants was found in ‘Girona’ followed by ‘Terres de l'Ebre’. ‘Lleida’ had the highest rate of unemployment.
What and how many: identifying and describing services
According to the official listings provided by the different Departments (i.e., the list of the service providers publicly funded), there were a total of 778 services providing care for people with mental health problems. However, it is important to have comparable units of analysis. When these services were evaluated according to DESDE-LTC criteria, the total number of BSICs was 639. These BSICs were coded with 734 codes describing their MTC. Just 12.36% of all the BSICs needed more than one MTC to describe their main activity.
With regard balance of care, 88% of all MTCs provided by the Department of Health, were health-related, whereas only 31% of MTCs provided by other Departments were health-related.
Where: mapping the services, comparing territories
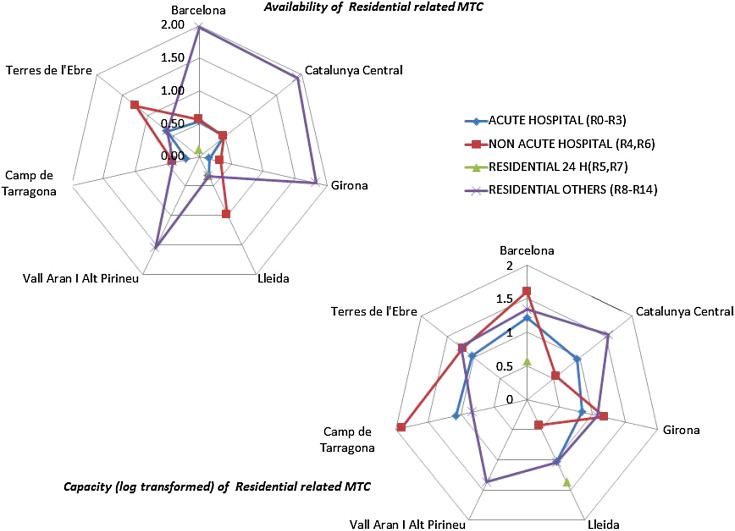
Tables 2 and 3 summarise the availability of services and their capacity (placement and workforce). In the integrated Atlas, the information provided in the tables was visually displayed by maps, graphics and semaphores, to facilitate the understanding of the information by decision or policy makers. Figure 1 shows one example of these visualisation tools (spider graphs with data on adult residential care availability by health region). When policy makers found an inconsistent pattern, they consulted the tables for detailed information.
Table 2.
Availability of MTCs, by health region. Rations per 100 000 inhabitants
| Catalonia | Barcelona | Catalunya Central | Girona | Lleida | Vall d'Aran I Alt Pirieny | Camp de Tarragona | Terres de l'Ebre | |
|---|---|---|---|---|---|---|---|---|
| Population >17 years olds | 6 166 330 | 4 126 001 | 416 261 | 599 473 | 299 391 | 64 639 | 497 611 | 161 224 |
| Population <18 years olds | 1 348 015 | 886 924 | 95 825 | 138 879 | 64 509 | 122 293 | 119 241 | 30 344 |
| ADULTS | ||||||||
| RESIDENTIAL | ||||||||
| Acute Hospital (R0–R3) | 0.37 | 0.53 | 0.48 | 0.17 | 0.33 | 0.00 | 0.20 | 0.62 |
| Non-acute Hospital(R4, R6) | 0.55 | 0.56 | 0.48 | 0.33 | 1.00 | 0.00 | 0.40 | 1.24 |
| Residential 24 H (R5, R7) | 0.08 | 0.10 | 0.00 | 0.00 | 0.33 | 0.00 | 0.00 | 0.00 |
| Residential others (R8–R14) | 1.70 | 1.96 | 1.92 | 1.83 | 0.33 | 1.55 | 0.40 | 0.62 |
| DAY CARE | ||||||||
| Acute day care (D0, D1) | 0.50 | 0.58 | 0.72 | 0.17 | 0.33 | 0.00 | 0.20 | 0.62 |
| Day care related to health (D4–D8) | 0.68 | 0.65 | 0.72 | 0.67 | 1.00 | 1.55 | 0.40 | 1.24 |
| Day care related to employment* | 1.17 | 0.97 | 1.92 | 1.33 | 2.00 | 1.55 | 1.61 | 0.62 |
| Day care (other) | 0.83 | 0.80 | 0.96 | 0.83 | 1.67 | 0.00 | 0.80 | 0.00 |
| OUTPATIENT CARE | ||||||||
| Non-acute movile outpatient care (O5–O7) | 0.26 | 0.29 | 0.24 | 0.17 | 0.67 | 0.00 | 0.00 | 0.00 |
| Non-acute outpatient care (08–010) | 1.46 | 1.41 | 1.20 | 1.33 | 2.00 | 7.77 | 1.00 | 1.86 |
| Emergency care movile (01–02) | 0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.20 | 0.00 |
| Emergency care non-movile (03–04)* | 0.36 | 0.41 | 0.24 | 0.17 | 0.33 | 0.00 | 0.20 | 0.62 |
| Accessibility (A4) (including programs)* | 0.78 | 0.82 | 0.72 | 0.50 | 1.00 | 0.00 | 0.60 | 1.24 |
| CHILD AND ADOLESCENT | ||||||||
| RESIDENTIALL | ||||||||
| ACUTE HOSPITAL (R0–R3)* | 0.82 | 0.68 | 4.80 | 0.72 | 1.55 | 0.00 | 0.84 | 0.00 |
| RESIDENTIAL 24 H (R5, R7) | 0.07 | 0.11 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| DAY CARE | ||||||||
| Acute day care (D0, D1) | 1.71 | 1.92 | 4.80 | 0.72 | 1.55 | 0.00 | 0.84 | 3.30 |
| OUTPATIENT CARE | ||||||||
| Non-acute outpatient care (08–010) | 11.13 | 9.25 | 31.23 | 10.80 | 18.60 | 97.62 | 9.23 | 16.48 |
| Emergency care movile (01–02)* | 0.22 | 0.34 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Emergency care non-movile (03–04)* | 0.07 | 0.11 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
Table 3.
Placement (Cap) and workforce (WF) capacity, by health region. Rates per 100 000 inhabitants
| Catalonia | Barcelona | Catalunya Central | Girona | Lleida | Vall d'Aran I Alt Pirineu | Camp de Tarragona | Terres de L'Ebre | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population >17 years olds | 6 166 330 | 4 126 001 | 416 261 | 599 473 | 299 391 | 64 369 | 497 611 | 161 224 | ||||||||
| Population <18 years olds | 1 348 015 | 886 924 | 95 825 | 138 879 | 64 509 | 12 293 | 119 241 | 30 344 | ||||||||
| ADULTS | ||||||||||||||||
| RESIDENTIAL | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF |
| Acute Hospital (R0–R3) | 14.23 | 10.72 | 16.65 | 12.10 | 9.13 | 6.99 | 7.01 | 1.80 | 10.69 | 9.25 | 0.00 | 0.00 | 12.06 | 13.16 | 11.16 | 17.80 |
| Non-acute Hospital(R4, R6) | 36.06 | 12.65 | 40.74 | 13.77 | 3.60 | 2.37 | 15.35 | 9.22 | 2.67 | 8.03 | 0.00 | 0.00 | 80.38 | 22.58 | 16.75 | 6.55 |
| Residential 24 H (R5, R7) | 3.62 | 2.21 | 3.71 | 2.23 | 0.00 | 0.00 | 0.00 | 0.00 | 23.38 | 14.85 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Residential others (R8–R14) | 19.97 | 4.12 | 21.79 | 4.53 | 35.79 | 5.43 | 12.01 | 1.98 | 11.02 | 3.45 | 23.30 | 8.48 | 6.83 | 3.02 | 17.99 | 0.99 |
| DAY CARE | ||||||||||||||||
| Acute day care (D0, D1) | 10.46 | 2.51 | 12.65 | 2.84 | 10.33 | 3.32 | 4.17 | 1.22 | 6.68 | 2.32 | 0.00 | 0.00 | 4.02 | 1.07 | 9.30 | 2.72 |
| Day care related to health (D4–D8) | 21.07 | 3.31 | 22.81 | 3.83 | 20.42 | 2.40 | 16.35 | 2.19 | 21.71 | 2.47 | 23.30 | 3.23 | 10.05 | 1.48 | 27.91 | 3.82 |
| Day care related to employment* | 12.69 | 0.09 | 12.12 | 1.79 | 15.86 | 3.15 | 8.34 | 1.17 | 23.05 | 3.05 | * | * | 19.49 | 2.25 | * | * |
| Day care (other) | 31.10 | 2.36 | 31.14 | 2.25 | 37.24 | 2.69 | 11.68 | 2.70 | 67.47 | 3.91 | 0.00 | 0.00 | 41.20 | 2.73 | 0.00 | 0.00 |
| OUTPATIENT CARE | ||||||||||||||||
| Non-acute movile outpatient care (05–07) | 3.28 | 0.37 | 3.61 | 0.42 | 6.97 | 0.72 | 2.17 | 0.20 | 3.67 | 0.37 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Non-acute outpatient care (08–010) | na | 11.09 | na | 11.11 | na | 11.41 | na | 10.75 | na | 12.62 | na | 9.04 | na | 10.28 | na | 11.56 |
| Emergency care movile (01–02) | na | * | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | * | na | 0.00 |
| Emergency care non-movile (03–04)* | na | 1.12 | Na | 0.98 | na | * | na | * | na | * | na | 0.00 | na | * | na | 17.80 |
| Accessibility (A4) (including programs)* | 33.68 | 2.57 | 28.94 | 3.03 | 8.65 | 0.23 | 74.40 | 1.19 | 3.34 | 2.13 | 0.00 | 0.00 | 78.37 | 3.83 | * | * |
| CHILD AND ADOLESCENT | ||||||||||||||||
| RESIDENTAL | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF | Cap | WF |
| Acute Hospital (R0–R3)* | 10.09 | 6.87 | 12.52 | 7.58 | 14.41 | 33.03 | 3.60 | * | 6.20 | * | 0.00 | 0.00 | 8.39 | 9.74 | 0.00 | 0.00 |
| Residential 24 H (R5, R7) | 0.89 | 1.41 | 1.35 | 2.15 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| DAY CARE | ||||||||||||||||
| Acute day care (D0, D1) | 34.12 | 9.87 | 41.15 | 12.74 | 48.05 | 9.63 | 0.52 | 5.18 | 23.25 | 4.76 | 0.00 | 0.00 | 12.58 | 4.92 | 65.91 | * |
| OUTPATIENT CARE | ||||||||||||||||
| Non-acute outpatient care (08–010) | na | 87.59 | na | 96.91 | na | 173.42 | na | 83.48 | na | 55.45 | na | 149.60 | na | 51.72 | na | 56.95 |
| Emergency care movile (01–02)* | na | * | na | * | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 |
| Emergency care non-movile (03–04)* | na | * | na | * | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 | na | 0.00 |
*Missing Information; n.a.: not applicable.
Fig. 1.
Availability of residential MTCs. An example of visualisation tools.
Availability and capacity
Residential care
The health region ‘Vall d'Aran i Alt Pirineu’ was largely underprovided. It did not have any acute hospital (R2) in the geographical area. In contrast, residential services (R8–R13), provided by the Department of Social Welfare and Family were highly developed in this region, with a good level of availability. On the other hand, ‘Catalunya Central’ and ‘Girona’ had a lower placement capacity for acute care (the rate of beds was 9.13 and 7.21, respectively, v. 14.23 in overall Catalonia). A low placement capacity was found in non-acute hospital care (R4, R6) in ‘Catalunya Central’ (3.60 v. 36.06 in overall) and ‘Lleida’ (2.67 v. 36.06 in overall). In contrast ‘Lleida’ had the highest availability and capacity rates of non-acute non-hospital residential 24 h care (R5, R7), with a rate of 23.38 beds per 100 000 inhabitants, which highly contrasts with the overall rate of 3.62. On the other hand, ‘Camp de Tarragona’ had the highest rate of non-acute hospital (R4–R6) beds per inhabitants, mainly explained by the presence of a large psychiatric hospital in this area (80.38 v. 36.06 in overall), which also covers other catchment areas. Figure 1 graphically shows this information.
Child and adolescent
There was a lack of residential services for child and adolescents in ‘Vall d'Aran i Alt Pirineu’. ‘Terres de l'Ebre’ also lacked this type of care. Although the lack of long term residential care was not appropriate for child and adolescents, there was a ‘BSIC’ which provides special 24 h residential care (R5). The facility was funded by the Department of Criminal Justice, targeting Child and Adolescents with behavioural disorders related to criminal offences. The service was located in ‘Barcelona’ health region.
Day care
Adult
There was low availability of acute day care (D1), as well as low placement capacity in ‘Girona’, ‘Lleida’ and ‘Tarragona’. Regarding Day care related to health (D4.1), ‘Girona’ and ‘Camp de Tarragona’ had the lowest availability and capacity rates, whereas ‘Vall d'Aran i Alt Pirineu’ had the highest. On the other hand, ‘Catalunya Central’, ‘Tarragona’ and ‘Lleida’ had the highest availability and capacity rates for day care related to employment (D2.2, D3.2).
Child and adolescent
Rates of acute day care availability (D1) for child and adolescent were highly variable, ranging from none in ‘Vall d'Aran i Alt Pirineu’ to 4.80 in ‘Catalonia Central’. ‘Girona’ and ‘Camp de Tarragona’ were also underprovided, both in availability and in placement capacity.
Outpatient care
Adults
Non-acute outpatient care (O8–O10) availability rates ranged from 1.07 in ‘Tarragona’ to 1.84 in ‘Terres de l'Ebre’. In spite of this difference, workforce capacity rates were very similar, around 11 FTE staff per 100 000 inhabitants, with the exception of ‘Vall d'Aran and Alt Pirineu’, which had a higher rate, 12.89 FTE staff per 100 000 inhabitants. The main differences related to the availability of mobile outpatient care (O5–O7), which was not found in ‘Vall d'Aran i Alt Pirineu’, ‘Camp de Tarragona’ and ‘Terres de l'Ebre’. It is important to note that non-mobile emergency care (O3–O4) was usually found together with acute hospital care (R2). That is, one BSIC in combination with two MTC codes (R2 and O3). In this case it was not possible to separately code the shared workforce staff.
Child and adolescent
The availability of outpatient care for child and adolescents was highly variable. The highest availability rate was found in ‘Vall d'Aran i Alt Pirineu’ (97.62 v. 11.13 in overall), mainly explained by the presence of several satellite outpatient clinics in remote areas. There was also a lack of emergency outpatient care (O1–O4). Only one O3 (emergency non-mobile outpatient care) was found in ‘Barcelona’ Health Region, providing care for all Catalonia.
Accessibility
Adults
Care related to accessibility (i.e., case management and care coordination) varied highly across regions, ranging from none in ‘Vall d'Aran i Alt Pirineu’, to 1.23 in ‘Terres de l'Ebre’. This type of care is provided by both the Department of Health and the Department of Social Welfare and Family.
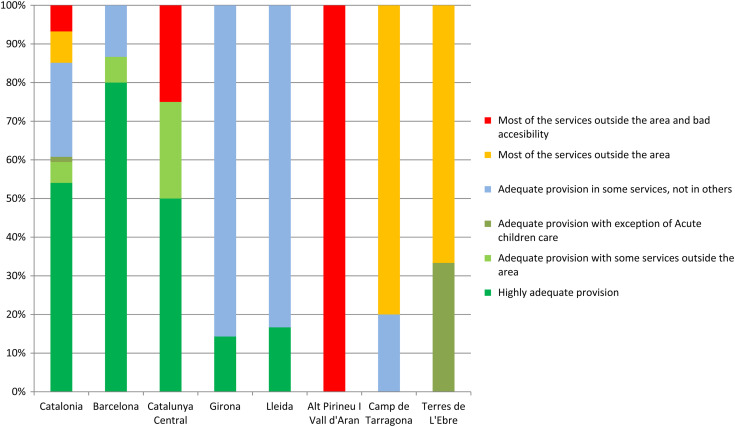
Adequacy of the provision of mental health care
Figure 2 shows the percentage of adequately provided small mental health areas by health region, when only considering the core mental health services provided by the Department of Health. Overall, more than 80% of the small mental health areas in Catalonia had an adequate core mental health service. The regions with the least adequate provision of health care were ‘Vall d'Aran i Alt Pirineu’, followed by ‘Camp de Tarragona’ and ‘Terres de l'Ebre’. In the supplementary file 2, there is a visual representation of the complete analysis of the de-identified 74 small areas.
Fig. 2.
Adequacy of the availability of core mental health main types of care, by health region.
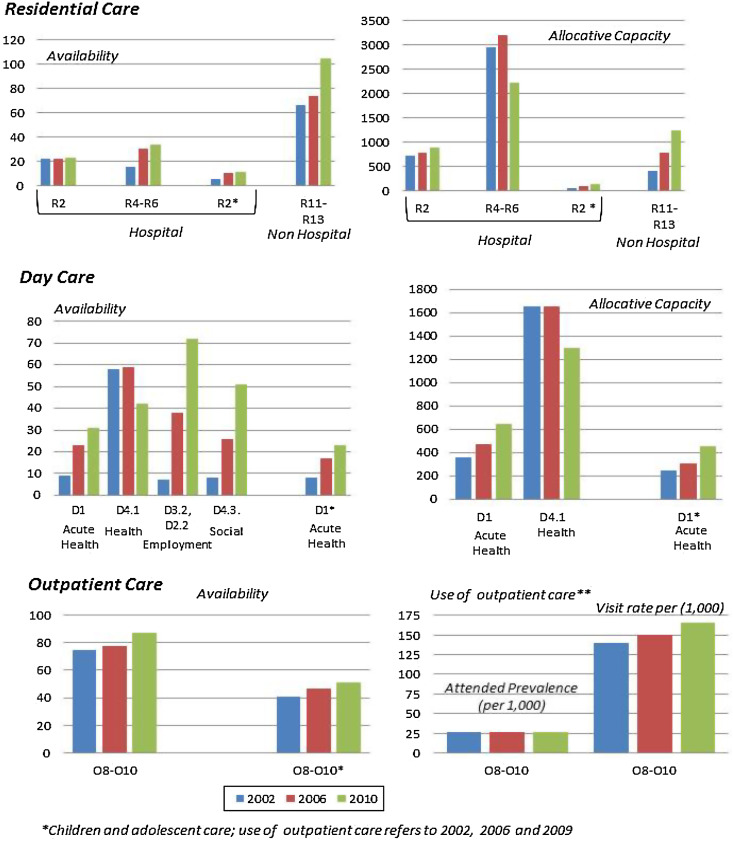
Monitoring the evolution of the system
Figure 3 shows the evolution in the availability and placement capacity of mental health care in Catalonia (2002 to 2010). The availability of services has increased. The exception is ‘day care related to health’ (D4.1), which decreased from 2006 to 2010, while other types of day care increased during the same period. Although the number of official day care health centres has not decreased, some of these services (officially known as ‘Day Centres’) did not meet the criteria to be considered as ‘day care related to health’ (D4.1) when DESDE-LTC criteria were applied. It is also important to note the rise in residential facilities (non-hospital based) and in acute day care. Although the availability of non-acute hospital services has not decreased, the placement capacity of those facilities has reduced. This is related to the de-instituzionalisation process and the consequent development of residential places in the community.
Fig. 3.
Evolution of the Mental Health System in Catalonia: 2002–2006–2010.
Specific Child and Adolescent Mental Health Care has also shown an important development in the last years, particularly with those services related to acute day care.
Evaluating the usefulness and relevance of the Integrated Atlas of Mental Health Care
According to experts in Health Planning and Decision Making from Catalonia, the integrated Atlas Mental Health in Catalonia was useful for their work (average rating 7.78 out of 10, ranging from 6 to 9.5, median value 7) and provided relevant information (average rating 8.28 out of 10, ranging from 7 to 9, median value 9).
Discussion
To the best of our knowledge, this is the first Integrated Atlas of Mental Health Care, which takes into account all the relevant services that receive public funding and specialise in mental health services, following an international standard classification system developed to map services for long-term care.
Practical implications for mental health planning in Catalonia
The Atlas has pointed out a number of problems. First, to provide integrated mental health care, the different Departments involved should agree on which ‘zoning’ use. The continuity of care cannot be guaranteed if sectory boundaries are not aligned. A major achievement would be a shared interoperable mapping/zoning system across agencies. Second, there was a gap between what services were expected to do, and what did happen in reality. In the case of Catalonia, this was identified in relation to the services officially known as ‘day centres/rehabilitation centres’. Decision makers and policy planners may be misinformed on the availability of services, if they base their analysis in the ‘name’ of the services, without taking into account what the services actually do. Care gaps appear when services do not provide the kind of care they are expected to, even when these services are available. That is one of the reasons why having a standardised classification of services is so important. Third, there was a number of ‘official services’ that were not stable enough to be considered a BSIC. This is important for planning as these ‘facilities’ are very vulnerable to economic constraints or crisis, being the first in disappear.
Provision problems were particularly important in the ‘Alt Pirineu-Aran’ region, a highly mountainous and low density rural area, suggesting that a special plan is needed for rural mental health care. Although there was a lack of health services, social services were more developed. Hence, one possible solution is to increase the capability of these social services to provide some health-related care, thereby bridging efforts between health and social sectors. A recent paper from Catalonia also reported a lower use of mental health services in people living in regions with lower density areas (Rocha et al. 2013). ‘Girona’ is another area that was systematically underprovided in comparison with other regions. A lack of services for child and youth mental health care was also detected in ‘Camp de Tarragona’. Efforts are needed in order to develop more services in these areas.
The information on availability and capacity presented in this paper can be linked to information related to health needs, using Geographical Information Systems (GIS). As a part of the Integrated Atlas of Mental Health 2010, there was an analysis of hot-spots and cold-spots (i.e., areas with unusual high or low treated prevalence of mental disorders) (Salinas-Perez et al. 2012). In addition, data on availability and capacity were combined with data on utilisation (i.e., length of stay, visits, attended prevalence) to perform an analysis of technical efficiency (benchmarking) of the 74 small health areas (Garcia-Alonso et al. 2013).
Impact of the Catalan Atlases of mental health in the mental health system
In the case of Catalonia, the Atlases had had a clear impact on the way mental health care was provided. For instance, in the Atlas 2002 it was detected that some of the ‘Day Hospitals (D1)’ did not provide the type of care expected, providing more than ‘Community day centers (D4)’. In consequence, decision makers revised the requirements to be considered as a ‘Day Hospital (D1)’ (official description) and resources were reallocated (new budget). When monitoring the system in 2006, the number of ‘Day Hospitals’ (D1) had dramatically increased. In addition, the Catalan Department of Health incorporated the knowledge provided by the different atlases into their corporative knowledge (de la Puente, 2006) and developed key indicators to monitor the mental health system, based on the mapping system (Salvador-Carulla et al. 2010b). To achieve that, it was important to follow what is known as the ‘exchange model of knowledge transfer’ (Lomas, 2000) or the more recent ‘Interactive System Framework’ (Thigpen et al. 2012). According to both models, to transfer knowledge to action, researchers and stakeholders have to be engaged in a bidirectional model of knowledge exchange from the start. In our case, using an iterative process, policy planners identified their needs, and the researchers helped them to use the knowledge derived from the research. The use of visualisation tools (maps, spider graphics and semaphores) for communicating health information, was also a powerful way to bridge the gap between complex epidemiological presentations of statistics and the varied educational backgrounds of policy makers and other stakeholders (Parrott et al. 2007).
Limitations
There are a number of limitations. First, these results were based on self-reported data given by the different providers. In spite of the extensive checking process followed in this study to validate the data, the information provided by them may have been inaccurate or imprecise. There could be some missing information in placement and workforce capacity, so these results have to be considered with caution. Second, there were some limitations related to the DESDE-LTC instrument itself. The instrument had problems with describing services, which are in transition or when used to codify services provided by macro-organisations with the same professionals working at different services. Third, data on the evolution of the system was not complete. In 2002 the Atlas only included information from the Health Department and partly from the Department of Social Welfare, although the information on social care was inaccurate. In 2006, services from the Department of Employment were also evaluated. In 2010, we evaluated all the services available from every relevant sector. Hence, the increase in the availability of care and in the capacity of the system could be partially conditioned because of incomplete information in 2002 and 2006. Fourth, our definition of adequacy did not include the quality of the services, being just a combination of accessibility and availability. Last, the data on relevance and usefulness of the Integrated Atlas was only based in the experience of 7 experts from the Department of Health.
Conclusion
In conclusion, this paper shows that an integrated Atlases of Mental Health using a standardised classification system, such as the DESDE-LTC, is a powerful tool for evidence informed policy. Policy makers can use Atlases to detect gaps and inequities in the provision of care for people with mental health needs; to ‘fill’ these gaps using local information; and to monitor the system. This paper also illustrates how the collaboration between researchers and policy makers is possible, if objectives are shared and results are communicated in a comprehensive way. Finally, if Atlases of Mental Health are done using common terminology, cross-country comparisons and learning lessons one from each other is possible.
Acknowledgements
We particularly thank the contribution made by representatives from various Departments of the Government of Catalonia who assisted with provider contact: Leandro Tacons, Joana Martinez Matilla, Carme Iniesta i Torres, Rafael Guerrero, Esther Rovira and Gemma Salmeron. The project was overseeing by an Expert Advisory Group. We are grateful to Pere Bonet, Antoni Bulbena, Jordi Cid, Diego Palao, Jose Garcia, Josep Ramos, Lluis Lalucat, Luis Miguel Martinez-Lopez, Enric Aragones, Enric Arques and Joana Martinez Matilla for their valuable comments during the project. The GEOSCAT-SM Research group was a consortium of researchers from PSICOST and Sant Joan De Deu Research Unit bought together to develop the Integrated Atlas of Mental Health in Catalonia. Members of the GEOSCAT-SM group were: Luis Salvador-Carulla, Josep Maria Haro, Antoni Serrano-Blanco, Miriam Poole, Mencia R Gutierrez-Colosia, Ana Fernandez, Teresa Marfull, Carlos Garcia and Jose Alberto Salinas. We thank Javier Garcia-Alvarez and Maria Luisa Rodero for their contribution to the analysis of the Atlas. Finally, we are grateful to the managers of organisations and services of Mental Health Care in Catalonia, who shared their information with us.
Financial Support
This project was funded by competitive tender from the Government of Catalonia.
Conflict of Interest
None.
Ethical Standards
The information provided on service availability and capacity did not required ethical approval as this information did not include data on individual patients. The information on service utilisation was mainly based on publicly available information. Secondary analysis of available datasets was performed following authorisation and ethical approval from the Catalan Department of Health.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796014000511.
click here to view supplementary material
References
- Almeida OP (2003). Atlas: mental health resources in the world 2001. Psychological Medicine 33, 568–568. [Google Scholar]
- Berger EL (2007). Mental Health Atlas 2005. Journal of Nervous and Mental Disease 195, 358–359 [Google Scholar]
- Bosch-Capblanch X, Lavis JN, Lewin S, Atun R, Rottingen JA, Droschel D, Beck L, Abalos E, El-Jardali F, Gilson L, Oliver S, Wyss K, Tugwell P, Kulier R, Pang T, Haines A (2012). Guidance for Evidence-informed policies about health systems: rationale for and challenges of guidance development. Plos Medicine 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronenwett JL, Birkmeyer JD (2000). The Dartmouth Atlas of vascular health care. Cardiovascular Surgery 8, 409–410. [PubMed] [Google Scholar]
- Garcia-Alonso C, Salvador-Carulla L, Alvarez-Galvez J, Salinas-Perez JA, Fernandez A, Serrano-Blanco A, Prat-Pubill B, Jorda-Samprieto E (2013). Modelling the quality and technical efficiency of the mental health system in Catalonia (Spain). Tenth International Conference of the European Network for Mental Health Service Evaluation (ENMESH 2013) Recovery-oriented mental health services: Therapeutic, organisational and economic challenges: Verona.
- Goodwin N (2013). Understanding integrated care: a complex process, a fundamental principle. International Journal of Integrated Care 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S, Kuhlmannr R, the Group Epcat (2000). The European Service Mapping Schedule (ESMS): development of an instrument for the description and classification of mental health services. Acta Psychiatrica Scandinavica 102, 14–23. [PubMed] [Google Scholar]
- Knapp M, Funkm M, Curran C, Prince M, Grigg M, McDaid D (2006). Economic barriers to better mental health practice and policy. Health Policy and Planning 21, 157–170. [DOI] [PubMed] [Google Scholar]
- Lomas J (2000). Using ‘linkage and exchange’ to move research into policy at a Canadian foundation. Health Affairs 19, 236–240. [DOI] [PubMed] [Google Scholar]
- Mcbain R, Salhi C, Morris JE, Salomon JA, Betancourt TS (2012). Disease burden and mental health system capacity: WHO Atlas study of 117 low- and middle-income countries. British Journal of Psychiatry 201, 444–450. [DOI] [PubMed] [Google Scholar]
- Meier DE, Beresford L (2008). Dartmouth Atlas Data can support palliative care development. Journal of Palliative Medicine 11, 960–963. [DOI] [PubMed] [Google Scholar]
- Moran V, O'connor S, Borowitz M (2013). International approaches to measuring the quality of mental health care. Epidemiology and Psychiatric Sciences 22, 3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble M (1994). New Practice Atlas Outlines variations in health-care provided across Ontario. Canadian Medical Association Journal 151, 218–219. [PMC free article] [PubMed] [Google Scholar]
- Parrott R, Hopfer S, Ghetian C, Lengerich E (2007). Mapping as a visual health communication tool: promises and dilemmas. Health Communication 22, 13–24. [DOI] [PubMed] [Google Scholar]
- de la Puente ML (2006). Preface. Acta Psychiatrica Scandinavica 14 (Suppl. 432), 4. [Google Scholar]
- Rocha KB, Rodriguez-Sanz M, Perez K, Obiols JE, Borrell C (2013). Inequalities in the utilization of psychiatric and psychological services in Catalonia: a multilevel approach. Administration and Policy in Mental Health and Mental Health Services Research 40, 355–363. [DOI] [PubMed] [Google Scholar]
- Salinas-Perez JA, Garcia-Alonso CR, Molina-Parrilla C, Jorda-Sampietro E, Salvador-Carulla L (2012). Identification and location of hot and cold spots of treated prevalence of depression in Catalonia (Spain). International Journal of Health Geographics 11, 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador-Carulla L, Mezzich JE (2012). Person-centred medicine and mental health. Epidemiology and Psychiatric Sciences 21, 131–137. [DOI] [PubMed] [Google Scholar]
- Salvador-Carulla L, Garrido M, McDaid D, Haro JM (2006). Financing mental health care in Spain: context and critical issues. European Journal of Psychiatry 20, 29–44. [Google Scholar]
- Salvador-Carulla L, Costa-Font J, Cabases J, McDaid D, Alonso J (2010a). Evaluating Mental Health Care and Policy in Spain. Journal of Mental Health Policy and Economics 13, 73–86. [PubMed] [Google Scholar]
- Salvador-Carulla L, Salinas-Perez JA, Martin M, Grane MS, Gibert K, Roca M, Bulbena A (2010b). A preliminary taxonomy and a standard knowledge base for mental-health system indicators in Spain. International Journal of Mental Health Systems 4, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador-Carulla L, Dimitrov H, Weber G, McDaid D, Venner B, Sprah L, Romero C, Ruiz M, Tibaldi G, Johnson S (2011). DESDE-LTC: Evaluation, and Classification of Services for Long Term Care in Europe. Psicost and Catalunya Caixa: Barcelona. Availabe at: www.edesdeproject.eu/ (last accessed 18 August 2014) [Google Scholar]
- Salvador-Carulla L, Putnam M, Bigby C, Heller T (2012). Advancing a research agenda for bridging ageing and disability. International Journal of Integrated Care 12, e204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador-Carulla L, Alvarez-Galvez J, Romero C, Gutierrez-Colosia MR, Weber G, McDaid D, Dimitrov H, Sprah L, Kalseth B, Tibaldi G, Salinas-Perez JA, Lagares-Franco C, Roma-Ferri MT, Johnson S (2013a). Evaluation of an integrated system for classification, assessment and comparison of services for long-term care in Europe: the eDESDE-LTC study. BMC Health Services Research 13, 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador-Carulla L, Serrano-Blanco A, Garcia-Alonso C, Fernandez A,Salina-Perez JA, Gutierrez-Colosia MR, Marfull-Blanc T, Rodero-Cosano MLPrat-Pubill B, Molina C (2013b). GEOSCAT: Atles integral dels serveis d'atenció a la salut mental de Catalunya, 2010. Pla director de salut mental i addiccions. Direcció General de Planificació i Recursos Sanitaris, Generalitat de Catalunya: Barcelona.
- Saxena S, Maulik PK, O'Connell K, Saraceno B (2002). Editorial: mental health care in primary and community settings: results from Who's project atlas. International Journal of Social Psychiatry 48, 83–85. [DOI] [PubMed] [Google Scholar]
- Saxena S, Sharan P, Cumbrera MG, Saraceno B (2006). World Health Organization's mental health atlas 2005: implications for policy development. World Psychiatry 5, 179–184. [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H (2007). Global Mental Health 2 – resources for mental health: scarcity, inequity, and inefficiency. Lancet 370, 878–889. [DOI] [PubMed] [Google Scholar]
- Thigpen S, Puddy RW, Singer HH, Hall DM (2012). Moving knowledge into action: developing the rapid synthesis and translation process within the interactive systems framework. American Journal of Community Psychology 50, 285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796014000511.
click here to view supplementary material