Abstract
BACKGROUND AND PURPOSE:
Woven EndoBridge (WEB) devices are increasingly used to treat intracranial aneurysms. A1 asymmetry contributes to anterior communicating artery aneurysm formation and to treatment instability after coiling. We sought to evaluate whether A1 asymmetry had an impact on angiographic outcome in anterior communicating artery aneurysms treated with the WEB.
MATERIALS AND METHODS:
Anterior communicating artery aneurysms treated between July 2012 and July 2020 with the WEB from an institutional review board–approved database were reviewed. A1 asymmetry was categorized as the following: absence of the A1 segment on 1 side (unilateral A1) versus bilateral A1. Univariate and multivariable analyses assessed independent predictors of adequate (WEB Occlusion Scale A, B, and C) and complete occlusion (WEB Occlusion Scale A and B).
RESULTS:
Forty-eight individual aneurysms (47 patients) were included in the final analysis, of which 16 (33%) were acutely ruptured. The mean size was 6.5 (SD, 2.2) mm. Adequate and complete occlusion was achieved in 33 (69%) and 30 (63%) cases, respectively. Unilateral A1 was associated with significantly higher rates of adequate (92% versus 60% for bilateral A1; P = .03) and complete occlusion (92% versus 50% for bilateral A1; P < .01). Multivariable logistic regression confirmed unilateral A1 as an independent predictor of both adequate (OR = 10.6; 95% CI, 1.6–220.7; P = .04) and complete occlusion (OR = 9.5, 95% CI, 1.5–190.2; P = .04. A sensitivity analysis comparing unilateral “functional” A1 with bilateral “functional” A1 showed similar results. WEB shape modification was not influenced by the unilateral A1 configuration (P = .70).
CONCLUSIONS:
Anterior communicating artery aneurysms with a unilateral A1 configuration treated with WEB devices are associated with better angiographic outcome than those with bilateral A1. This finding supports the hypothesis that WEB devices are resistant to unilateral flow in the aneurysm as opposed to coils.
The efficacy and safety of the Woven EndoBridge device (WEB; MicroVention) have been widely reported in several observational studies and in prospective trials.1,2 The device is now a reliable option for the treatment of wide-neck aneurysms. Two recent meta-analyses of WEB device use found that overall rates of complete and adequate occlusion were 53% and 80%–83.3%, respectively.3,4
The anterior communicating artery (ACoA) is a preferred site for aneurysms,5 and aneurysms in this location tend to have a higher risk of rupture than aneurysms in other locations.6,7 Because of the wide variety and complexity of the anterior communicating artery anatomy, ACoA aneurysms are usually considered the most complex ones to treat. Several endovascular devices (coils, stent-assisted coiling, and flow diverters) have been specifically reported in this location to overcome this challenge.8-10 Most pointed out the role of A1 asymmetry on the angiographic outcome.8,10 In this situation, the WEB device appears to be an appealing solution: It can be used in wide-neck aneurysms without a stent. However, the influence of the ACoA anatomy on WEB devices is not known.
Here, we aimed to report the angiographic outcomes of ACoA aneurysms treated with the WEB and to determine whether A1 asymmetry has an impact on the treatment outcome.
MATERIALS AND METHODS
Data-Sharing Statement
Study data are available from the corresponding author on reasonable request.
Ethical Statement
The French Ethical Committee for Research in Medical Imaging approved this study (institutional review board number CRM-2101–127). Informed consent was obtained for every patient.
Study Design
In our tertiary care center (Neuri center, Bicêtre Hospital, France), we retrospectively queried the prospectively acquired database of patients with aneurysms treated with WEB devices between July 2012 and July 2020. Consecutive, ruptured or unruptured ACoA aneurysms treated with WEB were included. Patients were excluded under the following circumstances: No follow-up angiograms for at least 3 months after treatment were available; treatment with a WEB was used as a retreatment strategy in a recanalized coiled aneurysm; or the aneurysm was secondary to another vascular malformation (eg, brain arteriovenous malformation).
The primary outcome was adequate angiographic occlusion, defined as a score on the WEB Occlusion Scale (WOS) of A, B or C. The secondary outcome was angiographic complete occlusion (WOS A or B).
A1 Asymmetry Assessment
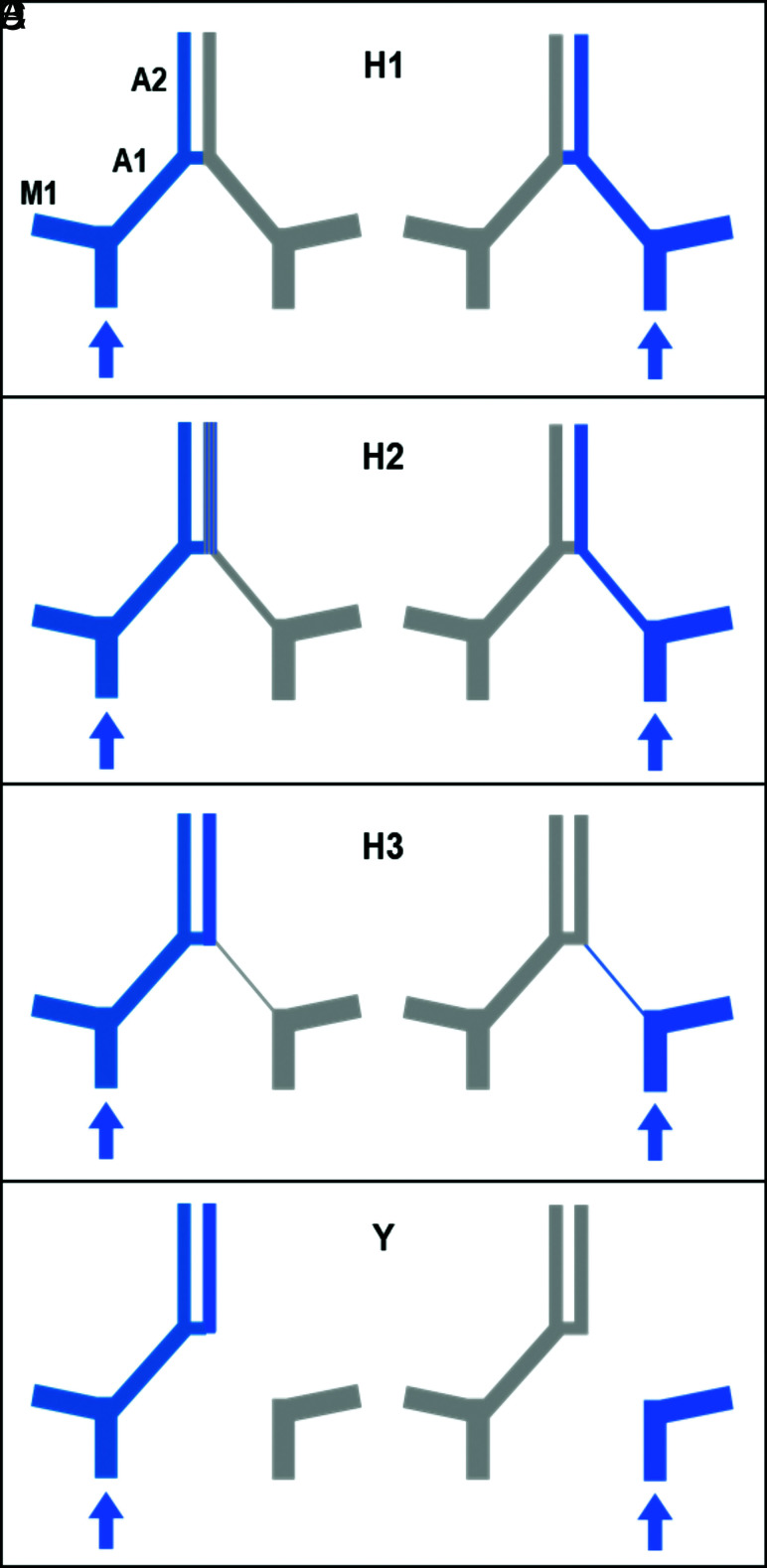
We classified A1 asymmetry using a 4-point grading scale, inspired by previous studies,8,10 on the basis of A1 segment size and functionality (Fig 1) as follows: grade H1, both A1 segments are the same size (ie, symmetric A1s); grade H2, the A1 segment is smaller (hypoplastic) on 1 side but large enough for an opacification of the A2 segment with an ipsilateral injection (ie, asymmetric sizes but both functional A1s); grade H3, the A1 segment is very hypoplastic on 1 side, the A2 segment on that side is not opacified following ipsilateral injection of contrast agent, and both A2 segments are only opacified following injection from the dominant side (ie, asymmetric size and a nonfunctional hypoplastic side); and grade Y, the A1 segment is absent on 1 side (aplastic).
FIG 1.
Grading scale for A1 segments. A, Grade H1: A1 segments are symmetric. B, Grade H2: The A1 segment is smaller on 1 side, but opacification of the A2 segment on that side is observed following ipsilateral injection (ie, asymmetric A1s but both functional). C, Grade H3: The A1 segment is very hypoplastic on 1 side, the A2 segment is not opacified from the ipsilateral injection, and A2 segments are only opacified with injection from the dominant side (ie, asymmetric A1s and a nonfunctional hypoplastic side). D, Grade Y: The A1 segment is absent on 1 side (aplastic). Blue filling represents opacification after injection from the side with the blue arrow. Grade Y corresponds to unilateral A1, and grade H3 + Y, to unilateral functional A1.
A1 segment anatomy was reported as “unilateral A1” (ie, grade Y) or otherwise “bilateral A1” (ie, grade H1 + H2 + H3). For a sensitivity analysis, we also dichotomized A1 segment anatomy using a more functional approach: unilateral “functional” A1 (grade H3 + Y) versus bilateral functional A1 (grade H1 + H2).
Imaging Analysis
Angiographic results were analyzed by 2 expert interventional radiologists (blinded to the clinical data) including 1 working in a different hospital and not involved in the treatment or follow-up. For this study, we used the WOS 4-point grading scale,11 as follows: complete occlusion (WOS A), near-complete occlusion (WOS B), neck remnant (WOS C), and aneurysm remnant (WOS D). Discrepancies were resolved by a third neuroradiologist not involved in the treatment.
We report the following aneurysm characteristics: size (including width/neck ratio and aspect ratio [height/neck]) and shape (rated as regular [smooth aneurysm surface on 3D] versus irregular [in case of a bleb or multilobar shape]).
WEB shape modification (WShM) refers to a loss of device height occurring during the follow-up.12,13 WShM was quantitatively defined as a ratio (percentage) defined as
with “d(initial)” the distance between the WEB proximal and distal markers after detachment, and “d(final)” the distance between the same 2 markers on last follow-up. The distance between the markers of the WEB was measured on cross-sectional images obtained with conebeam CT (VasoCT; Philips Healthcare) performed after WEB detachment and at each follow-up.14
Antiplatelet Regimen
In unruptured cases, patients received aspirin (160 mg per day) and ticagrelor (90 mg twice per day) the day before WEB implantation, and oral treatment was discontinued if not needed (depending on eventual WEB protrusion or use of a stent). In ruptured aneurysms, no antiplatelet regimen was used. For either ruptured or unruptured aneurysms, treatment was performed with the patient under systemic heparinization (50-UI/kg intravenous bolus followed by 20–40 IU/kg/h) that was stopped at the end of the procedure.
WEB Indication and Selection
The decision for WEB treatment of unruptured aneurysms was made by multidisciplinary consensus. For acutely ruptured aneurysms, selection of the treatment strategy was left to the operator. The main indication for using a WEB was a wide-neck bifurcation aneurysm.
In our database, 5 generations of WEB devices were used,15,16 corresponding to the different evolutions of the WEB device. We separated the “previous generation” (ie, generations 1–4), from the “fifth generation” (newest generation available). We also reported WEB devices: Double-Layer (WEB-DL), Single-Layer (WEB-SL), or Single Layer Sphere (WEB-SLS) as chosen by the operator. Devices were delivered through VIA catheters (MicroVention): VIA-17 or 27 depending on the size, or VIA-21–33 for older procedures. The operator used measurements (width, height, and neck of the aneurysm in at least 2 orthogonal projections) from 3D rotational angiograms to select the WEB size and followed the usual guidelines for the sizing: oversizing the width by 1or 2 mm.17
Statistical Analysis
Continuous variables are reported as mean (SD) if normally distributed or as median (interquartile range), while categoric variables are expressed as frequency (percentage). We explored the following: 1) “adequate occlusion” (WOS A, B, and C) versus “aneurysm remnant” (WOS D), and 2) “complete occlusion” (WOS A and B) versus “incomplete occlusion” (WOS C and D). A χ2 or Fisher exact test was used to evaluate qualitative factors as appropriate, and a Student t test or Wilcoxon U test was used to assess quantitative variables as appropriate.
Multivariable logistic regression analysis was performed using all candidate variables (P < .2 in the univariate analysis). For selected variables, ORs with 95% CIs and a P value of the likelihood-ratio test are given. No adjustment for multiple testing was performed, and analyses are regarded as explorative. To further test the impact of A1 asymmetry, we assessed a sensitivity analysis to test unilateral functional A1 (grades H3 + Y) versus bilateral functional A1 (grades H1 + H2). P values < .05 were considered statically significant. All statistical analyses were performed using R statistical and computing software (Version 3.6.1; http://www.r-project.org/).
RESULTS
Patient, Aneurysm, and Anatomic Characteristics
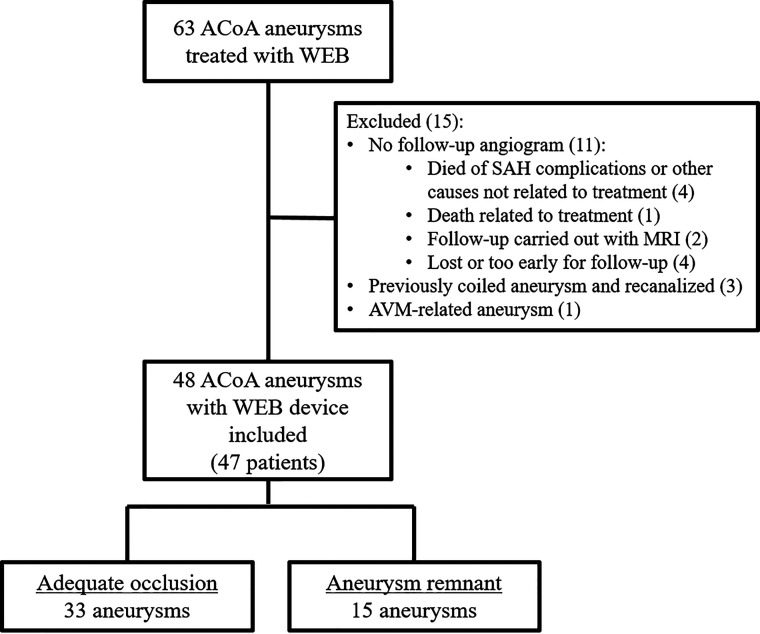
A total of 48 independent ACoA aneurysms treated with WEB devices in 47 patients were included in the analysis (Table 1 and Fig 2, patient flow chart). There were no missing data in the analysis. The mean age was 58.4 (SD, 11.2) years (range, 37–90 years), and 26 patients (54.2%) were women. Sixteen aneurysms (33.3%) were acutely ruptured cases. The mean maximum aneurysm diameter was 6.5 (SD, 2.2) mm (range, 3.1–13.1 mm).
Table 1:
Baseline characteristics and angiographic outcomesa
| Baseline Aneurysm Characteristics | All (n = 48) |
|---|---|
| Age (mean) (yr) | 58.4 (SD, 11.2) |
| Women | 26 (54.2) |
| Cardiovascular risk factor | 25 (52.1) |
| Current smoker | 7 (14.6) |
| Acutely ruptured | 16 (33.3) |
| Irregular aneurysm | 19 (39.6) |
| Maximum diameter (mean) (mm) | 6.5 (SD, 2.2) |
| Aneurysm height (mean) (mm) | 5.0 (SD, 1.8) |
| Aneurysm neck (mean) (mm) | 3.8 (SD, 1.1) |
| Aneurysm width (mean) (mm) | 5.1 (SD, 1.7) |
| Aspect ratio (height/neck) (mean) | 1.27 (SD, 0.39) |
| Width/neck ratio (mean) | 1.28 (SD, 0.27) |
| Unilateral A1 (grade Y) | 13 (27.1) |
| Unilateral functional A1 (grade H3+Y) | 19 (39.6) |
| Baseline treatment characteristics | |
| Type of WEB WEB-DL WEB-SL WEB-SLS |
2 (4.2) 37 (77.1) 9 (18.8) |
| WEB device generation Fifth generation Previous generations |
30 (62.5) 18 (37.5) |
| Additional stent | 2 (4.7) |
| Angiographic outcomes | |
| Adequate occlusion | 33 (68.8) |
| Complete occlusion | 30 (62.5) |
| Aneurysm remnant | 15 (31.2) |
| WShM (median) (IQR) (%) | 31 (11–51) |
Note:—IQR indicates interquartile range.
Data are presented as number (%) unless otherwise indicated.
FIG 2.
Patient flow chart.
A unilateral A1 segment (grade Y) was noted in 13 cases (27.1%), whereas 20 cases (41.7%) had symmetric A1 segments (grade H1). Grades H2 and H3 were noted in 9 (18.8%) and 6 (12.5%) cases, respectively. Both groups, unilateral A1 and bilateral A1, had similar aneurysm sizes: 7.1 (SD, 2.5) mm and 6.0 (SD, 1.9) mm, respectively. The aneurysm was systematically treated from the side with the largest A1 segment. If the sides were symmetric, the side with the more direct angle to the aneurysm was chosen (11 of 20 procedures were from the right side).
Treatment Characteristics and Outcomes
The WEB-SL was used in most cases (37/48, 77.1%), and 30/48 (62.5%) of devices used were fifth generation. Two aneurysms (4.2%) were also stented due to protrusion of the WEB into the parent artery. In both cases, a stent was used as a rescue technique because of WEB protrusion in the parent artery; 1 patient had a grade H1 ACoA configuration, and the other had a grade Y.
The median last follow-up was 12.2 months (range, 3–65 months). Adequate occlusion and complete occlusion were observed in 33/48 (68.8%) and 30/48 (62.5%) cases, respectively. The median WEB shape modification ratio at last follow-up was 31% (interquartile range = 11%–50.8%) and was similar in both adequate occlusion (30%) and aneurysm remnant groups (35%, P = .40). Angiographic outcome was also similar between ruptured and unruptured aneurysms (P = .99).
A1 Asymmetry as a Predictor of Angiographic Outcome
Unilateral A1 was associated with significantly higher rates of adequate (92.3% versus 60.0% for bilateral A1; P = .03) and complete occlusion (92.3% versus 51.4% for bilateral A1; P < .01). Other candidate variables for adequate occlusion were irregular shape (P = .19) and aspect ratio (P = .19), and for complete occlusion, they were irregular shape (P = .08) and age (P = .11). Finally, unilateral A1 was not associated with WEB shape modification (P = .70).
Unilateral A1 was confirmed as an independent predictor for both adequate (OR = 10.6; 95% CI, 1.6–220.7; P = .04) and complete occlusion (OR = 9.5; 95% CI, 1.5–190.2; P = .04). None of the other variables were independent predictive factors of adequate or complete occlusion in this population. Detailed results of univariate and multivariable analyses for adequate and complete occlusion are presented in Table 2 and the Online Supplemental Data, respectively.
Table 2:
Univariate analysis and multivariable logistic regression for angiographic adequate occlusion of ACoA aneurysms treated with WEBa
| Variables | Univariate Analysis |
Multivariable Analysis |
|||
|---|---|---|---|---|---|
| Adequate Occlusion (n = 33) | Aneurysm Remnant (n = 15) | P Value | ORa (95% CI) | P Value | |
| Age (mean) (yr) | 59.1 (SD, 12) | 56.9 (SD, 8) | .45 | ||
| Women | 19 (58) | 8 (53) | .78 | ||
| Cardiovascular risk factors | 17 (52) | 8 (53) | .91 | ||
| Current smoker | 5 (15) | 2 (13) | .87 | ||
| Ruptured aneurysm | 11 (33) | 5 (33) | .99 | ||
| Irregular aneurysm | 11 (33) | 8 (53) | .19 | 0.54 (0.13–2.17) | .38 |
| Aspect ratio (mean) | 1.32 (SD, 0.37) | 1.15 (SD, 0.40) | .19 | 5.98 (0.84–64.79) | .10 |
| Width/neck ratio (mean) | 1.27 (SD, 0.27) | 1.29 (SD, 0.28) | .84 | ||
| Neck (mean) (mm) | 3.77 (SD, 1.13) | 3.79 (SD, 1.20) | .97 | ||
| Unilateral A1 | 12 (36) | 1 (7) | .03 | 10.6 (1.6–220.7) | .04 |
| WEB-SL | 27 (82) | 10 (67) | .39 | ||
| Fifth-generation WEB device | 20 (61) | 10 (67) | .69 | ||
| WShM (median) (IQR) (%) | 30 (11–48) | 35 (19–52) | .40 | ||
Note:—ORa indicates adjusted odds ratio.
Data are presented as number (%) unless otherwise indicated.
A sensitivity analysis comparing unilateral functional A1 (grade H3 + Y) versus bilateral functional A1 (grade H1 + H2) showed similar results. The adequate occlusion rate was 58.6% in grade H1 + H2 versus 84.2% in grade H3 + Y (P = .06), and the complete occlusion rate was 48.3% in grade H1 + H2 versus 84.2% in grade H3 + Y (P = .01), leading to an adjusted OR = 4.2; 95% CI, 1.01–22.87 (P = .06) for adequate occlusion and an adjusted OR = 5.5; 95% CI, 1.31–30.42 (P = .03) for complete occlusion. Table 3 presents the rate of angiographic adequate occlusion at each step of the 4-point grading scale that we used to describe A1 asymmetry.
Table 3:
Angiographic aneurysm occlusion depending on A1 asymmetry grading
| A1 Asymmetry Grading Scale | Adequate Occlusion No. (%) |
|---|---|
| Bilateral functional A1 | 17/29 (59) |
| H1 (n = 20) | 12 (60) |
| H2 (n = 9) | 5 (55) |
| Unilateral functional A1 | 16/19 (84) |
| H3 (n = 6) | 4 (67) |
| Y (n = 13) | 12 (92) |
DISCUSSION
Impact of ACoA Anatomic Configuration on WEB Devices
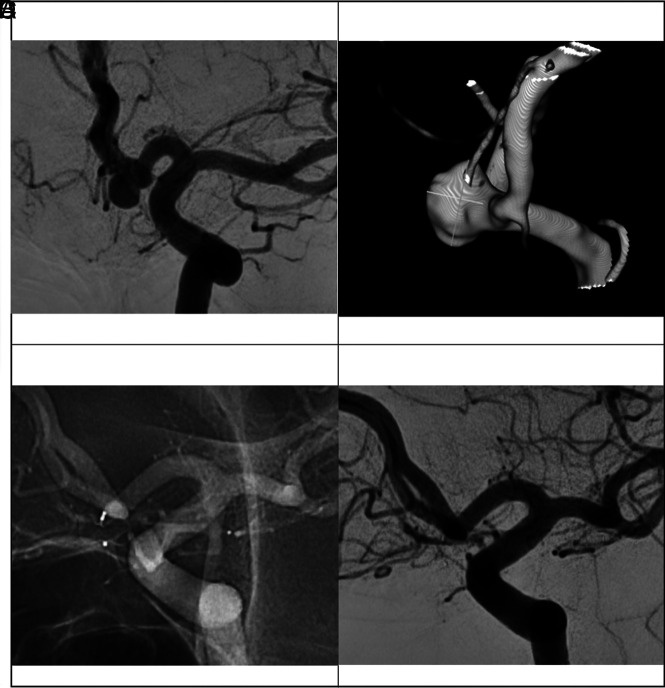
Our study of 48 ACoA aneurysms treated with the WEB device, in which we eliminated potential confounding factors using multivariate analysis, showed that unilateral A1 is a strong independent predictor of both adequate and complete occlusion (Fig 3, illustrative case). When an A1 segment was aplastic on 1 side (grade Y), leading to a unique unilateral blood flow entering the aneurysm, complete occlusion reached 93%. As intended by the sensitivity analysis, it seems that the definition of unilateral A1 could be extended to the absence of a functional A1 segment, which includes grade H3 in the definition.
FIG 3.
Illustrative case of a ACoA aneurysm treated with a WEB device (A and B). The contralateral A1 segment is absent, rendering a Y-shape to the ACoA anatomy. Last control angiogram at 1-year follow-up demonstrates complete occlusion (C and D).
Absence of an A1 segment on one side or the other of the ACoA shifts the anterior communicating complex from an “H-shape” to a “Y-shape.” It is possible that the angle between the aneurysm and the A1 segment on the side used for treatment may also partly explain the better results achieved in the Y-shaped ACoA. Like other termination locations (eg, basilar artery, middle cerebral artery bifurcation), Y-shaped “true bifurcation” aneurysms are more “straightforward,” enabling better positioning of the WEB device and subsequent sealing of the neck, which plays a important role in aneurysm occlusion.18 However, in our experience, complex anatomy with unfavorable angles of approach can be overcome with the balloon-assisted WEB remodeling technique.19
Another interesting result was the absence of significant difference in WEB shape modification between the unilateral A1 and bilateral A1 groups. This supports the hypothesis that this phenomenon is not only correlated to outside arterial flow but is under the influence of multifactorial events like the biologic healing response inside the WEB device.12,20
Comparison with Other Devices
An asymmetric A1 segment of the anterior cerebral arteries, with 1 side dominating the other, is a known risk factor for ACoA aneurysm formation and rupture.21-23 Several hypotheses have been proposed to explain the role of the anterior communicating complex anatomy in the formation of aneurysms, including wall shear stress and arterial blood flow.21,24
In contrast to our findings using WEB devices, Tarulli et al10 demonstrated that an asymmetric A1 was associated with unstable occlusion in coiled aneurysms, leading to higher rates of incomplete occlusion at follow-up. They hypothesized that substantial blood flow in 1 spot at a bifurcation may lead to formation of aneurysms that, after treatment with coils, are predisposed to molding and flattening of coil masses, resulting in an increased incidence of aneurysm remnants. The paradigm shift offered by extra- and intrasaccular flow-diversion devices may be of interest in this situation because it prevents the blood flow from entering the aneurysm. Pagiola et al8 recommended avoiding flow-diverter stents in grade Y ACoA aneurysms because of the risk of thromboembolic complications. Moreover, they also reported higher complication rates and lower rates of aneurysm occlusion when the A1 segments were highly asymmetric (grade H3). Here, our results suggest that the WEB, an intrasaccular flow-diversion device, could prevent the 1-sided blood flow from entering the aneurysm sac, without risking the patency of covered arterial branches.
To summarize, the WEB device could represent the best option for the treatment of a wide-neck ACoA aneurysm with a unilateral A1 configuration (especially if acutely ruptured): 1) It is resistant to unilateral blood flow, so it is more stable than coils across time, and 2) it avoids the deployment of a stent in the parent artery and, thus, the use of antiplatelet therapy.
Other Predictive Factors of Occlusion
In this study focusing on ACoA aneurysms treated with WEB, we observed rates of adequate occlusion similar to those found in a prospective study at midterm follow-up.25 Cagnazzo et al,26 evaluating a series of 86 aneurysms treated with a WEB in any location, found that an irregular shape and wide neck (>4 mm) were independent predictors of aneurysm remnants. Although not statistically significant, our results could suggest a role of the aneurysm irregular shape and aspect ratio (height/neck) on the angiographic outcome. We acknowledge that because the number of included aneurysms was relatively small, it is possible that some variables could not reach statistical significance in the multivariable analysis. However, we present, to date, the largest cohort of ACoA aneurysms treated with WEB.
Limitations
There are other limitations to our analysis. It was a retrospective study performed at a single academic center, and further prospective studies are needed to confirm our results. Also, the follow-up period seems limited (median: 1 year). However, the WEB is considered a stable device across time with most remnant aneurysms detected during the first year.27 Finally, a standardized definition of A1 asymmetry, dominance, and hypoplasia is lacking in the literature, making it difficult to compare studies. To this end, we chose first a consensual definition for the A1 asymmetry (absent or present). Then, we updated a previous grading system by focusing on the functional aspect of the A1 segments, which further confirmed our results.
CONCLUSIONS
A1 asymmetry favors better angiographic outcomes in ACoA aneurysms treated with the WEB device. Here, approximately 70% of ACoA aneurysms were adequately occluded after WEB implantation; however, this reached >92% in the unilateral A1 group, with an adjusted odds ratio of 11. This finding supports the hypothesis that WEB devices are less impacted by unilateral A1 flow, as opposed to other endovascular devices. This could be of interest when planning for a wide-neck ACoA aneurysm with a unilateral A1, particularly if the aneurysm is acutely ruptured. Further prospective studies comparing coils, flow-diverters, and the WEB device in this location are needed.
ABBREVIATIONS:
- ACoA
anterior communicating artery
- WOS
WEB Occlusion Scale
- WShM
WEB shape modification
Footnotes
Disclosures: Jacques Moret—UNRELATED: Consultancy: Medtronic, MicroVention, Stryker, Balt. Laurent Spelle—UNRELATED: Consultancy: MicroVention, Medtronic, Balt; Grants/Grants Pending: hospital grant from Philips Healthcare.
References
- 1.Arthur AS, Molyneux A, Coon AL, et al. The safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal WEB Intrasaccular Therapy (WEB-IT) Study. J Neurointerv Surg 2019;11:924–30 10.1136/neurintsurg-2019-014815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pierot L, Szikora I, Barreau X, et al. Aneurysm treatment with WEB in the cumulative population of two prospective, multicenter series: 3-year follow-up. J Neurointerv Surg 2021;13:363–68 10.1136/neurintsurg-2020-016151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Rooij S, Sprengers ME, Peluso JP, et al. A systematic review and meta-analysis of Woven EndoBridge single layer for treatment of intracranial aneurysms. Interv Neuroradiol 2020;26:455–60 10.1177/1591019920904421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang SM, Liu LX, Ren PW, et al. Effectiveness, safety and risk factors of Woven EndoBridge device in the treatment of wide-neck intracranial aneurysms: systematic review and meta-analysis. World Neurosurg 2020;136:e1–23 10.1016/j.wneu.2019.08.023 [DOI] [PubMed] [Google Scholar]
- 5.Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med 2006;355:928–39 10.1056/NEJMra052760 [DOI] [PubMed] [Google Scholar]
- 6.Bijlenga P, Ebeling C, Jaegersberg M, et al. @neurIST Investigators. Risk of rupture of small anterior communicating artery aneurysms is similar to posterior circulation aneurysms. Stroke 2013;44:3018–26 10.1161/STROKEAHA.113.001667 [DOI] [PubMed] [Google Scholar]
- 7.Suárez Mira JM, De Oliveira Costa FA, Horta BL, et al. Risk of rupture in unruptured anterior communicating artery aneurysms: meta-analysis of natural history studies. Surg Neurol 2006;66:S12–19; discussion S19 10.1016/j.surneu.2006.06.025 [DOI] [PubMed] [Google Scholar]
- 8.Pagiola I, Mihalea C, Caroff J, et al. Flow diversion treatment of aneurysms of the complex region of the anterior communicating artery: which stent placement strategy should “I” use? A single center experience. J Neurointerv Surg 2019;11:1118–22 10.1136/neurintsurg-2019-014858 [DOI] [PubMed] [Google Scholar]
- 9.Huang Q, Xu Y, Hong B, et al. Stent-assisted embolization of wide-neck anterior communicating artery aneurysms: review of 21 consecutive cases. AJNR Am J Neuroradiol 2009;30:1502–06 10.3174/ajnr.A1618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarulli E, Sneade M, Clarke A, et al. Effects of circle of Willis anatomic variations on angiographic and clinical outcomes of coiled anterior communicating artery aneurysms. AJNR Am J Neuroradiol 2014;35:1551–55 10.3174/ajnr.A3991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiorella D, Arthur A, Byrne J, et al. Interobserver variability in the assessment of aneurysm occlusion with the WEB aneurysm embolization system. J Neurointerv Surg 2015;7:591–95 10.1136/neurintsurg-2014-011251 [DOI] [PubMed] [Google Scholar]
- 12.Caroff J, Mihalea C, Da Ros V, et al. A computational fluid dynamics (CFD) study of WEB-treated aneurysms: can CFD predict WEB “compression” during follow-up? J Neuroradiol 2017;44:262–68 10.1016/j.neurad.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 13.Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015;76:522–30; discussion 530 10.1227/NEU.0000000000000669 [DOI] [PubMed] [Google Scholar]
- 14.Caroff J, Mihalea C, Neki H, et al. Role of C-arm VasoCT in the use of endovascular WEB flow disruption in intracranial aneurysm treatment. AJNR Am J Neuroradiol 2014;35:1353–57 10.3174/ajnr.A3860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mihalea C, Caroff J, Pagiola I, et al. Safety and efficiency of the fifth generation Woven EndoBridge device: technical note. J Neurointerv Surg 2019;11:511–15 10.1136/neurintsurg-2018-014343 [DOI] [PubMed] [Google Scholar]
- 16.Caroff J, Mihalea C, Klisch J, et al. Single-Layer WEBs: intrasaccular flow disrupters for aneurysm treatment: feasibility results from a European study. AJNR Am J Neuroradiol 2015;36:1942–46 10.3174/ajnr.A4369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal N, Hoit D, DiNitto J, et al. How to WEB: a practical review of methodology for the use of the Woven EndoBridge. J Neurointerv Surg 2020;12:512–20 10.1136/neurintsurg-2019-015506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vardar Z, King RM, Kraitem A, et al. High-resolution image-guided WEB aneurysm embolization by high-frequency optical coherence tomography. J Neurointerv Surg 2020September28[Epub ahead of print] 10.1136/neurintsurg-2020-016447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mihalea C, Escalard S, Caroff J, et al. Balloon remodeling-assisted Woven EndoBridge technique: description and feasibility for complex bifurcation aneurysms. J Neurointerv Surg 2019;11:386–89 10.1136/neurintsurg-2018-014104 [DOI] [PubMed] [Google Scholar]
- 20.Ding Y, Dai D, Rouchaud A, et al. WEB Device shape changes in elastase-induced aneurysms in rabbits. AJNR Am J Neuroradiol 2021;42:334–39 10.3174/ajnr.A6899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castro MA, Putman CM, Sheridan MJ, et al. Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. AJNR Am J Neuroradiol 2009;30:297–302 10.3174/ajnr.A1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krasny A, Nensa F, Sandalcioglu IE, et al. Association of aneurysms and variation of the A1 segment. J Neurointerv Surg 2014;6:178–83 10.1136/neurintsurg-2013-010669 [DOI] [PubMed] [Google Scholar]
- 23.Tarulli E, Fox AJ. Potent risk factor for aneurysm formation: termination aneurysms of the anterior communicating artery and detection of A1 vessel asymmetry by flow dilution. AJNR Am J Neuroradiol 2010;31:1186–91 10.3174/ajnr.A2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alnaes MS, Isaksen J, Mardal K-A, et al. Computation of hemodynamics in the circle of Willis. Stroke 2007;38:2500–05 10.1161/STROKEAHA.107.482471 [DOI] [PubMed] [Google Scholar]
- 25.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: sesults of the WEBCAST 2 Study. AJNR Am J Neuroradiol 2017;38:1151–55 10.3174/ajnr.A5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cagnazzo F, Ahmed R, Zannoni R, et al. Predicting factors of angiographic aneurysm occlusion after treatment with the Woven EndoBridge Device: a single-center experience with midterm follow-up. AJNR Am J Neuroradiol 2019;40:1773–78 10.3174/ajnr.A6032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fujimoto M, Lylyk I, Bleise C, et al. Long-term outcomes of the WEB device for treatment of wide-neck bifurcation aneurysms. AJNR Am J Neuroradiol 2020;41:1031–36 10.3174/ajnr.A6548 [DOI] [PMC free article] [PubMed] [Google Scholar]