Abstract
Osteomas and cystic mucoceles are well-known benign tumors, affecting the paranasal sinuses. However, the concomitant presence of both lesions represents a rare occurrence, with only a handful of reported cases. We report a case of a frontal sinus osteoma associated with an intracranial mucocele, in a 61-year-old male patient, with a 3-month history of intermittent headaches and subsequent generalized seizures. Post-contrast MRI showed a frontal heterogeneously enhanced lesion with an adjacent non-enhanced cyst. After surgical excision, histopathological examination established the diagnosis of osteoma with mucoid cyst. Mucoceles increase in size progressively and gradually. They are mostly asymptomatic, nevertheless, once they extend intracranially, complications like infections, seizures, or other neurological disturbances, may frequently occur, indicating the necessity for surgical treatment. Imaging modalities, in particular a head MRI is paramount while contemplating the differential diagnosis of a solid and cystic intracranial lesions, owing to its high sensitivity and specificity. The aim of this case report is to underscore the importance of considering intracranial mucoceles in the differential diagnosis of cystic lesions in the anterior cranial fossa when associated with a solid, possibly obstructing mass.
Keywords: Intracranial mucocele, Sinus frontal osteoma, Head MRI
Introduction
Osteomas are benign tumors that stem from the bone tissue and represent the most common tumor of the paranasal sinuses. Hypotheses on their pathogenesis include embryological, genetic, traumatic and infectious theories [1]. However, to date, none of these theories can provide a full picture of the pathological mechanisms that lead to the development of these tumors [1].
Intracranial mucoceles are benign cystic lesions of the paranasal sinuses, filled with mucus and surrounded with an epithelial lining. They are classified as primary and secondary mucoceles, depending on their origin [2]. Primary mucoceles are believed to originate from a minor ductal obstruction of a salivary gland within the sinus tissue [2]. Secondary mucoceles arise from sinus ostium obstruction, due to allergic, inflammatory, traumatic, fibrotic, dysplastic or neoplastic factors, prompting a blockage of the normal sinus drainage and ventilation, resulting in a progressive accumulation of mucous secretions within the sinus cavity [2]. Over time, mucoceles can cause erosion of the adjacent bones, due to pressure changes and chronic inflammation, expanding intracranially in the anterior cranial fossa.
Both lesions frequently affect people in the fourth and fifth decade, with osteomas being more prevalent in men [1,2]. They are benign, expansile lesions that are characterized by a slow and gradual growth, remaining asymptomatic for a long time and often being diagnosed incidentally [1,2]. When symptomatic, common manifestations of intracranial mucoceles include headaches, ophthalmological disturbances, as well as neurological anomalies such as seizures, dementia, and personality changes [3].
They commonly affect the paranasal sinuses as solitary masses, however coexistence of both lesions is quite rare. Diagnosis is established through imaging and histological examinations. In this framework, surgical intervention is greatly advocated due to the high-risk of an intracranial expansion of the mucoceles and related neurological complications [6,7].
Case presentation
A 61-year-old man presented with a 3-month history of intermittent headaches and episodes of generalized seizures 2 weeks prior to presentation, associated with transient motor aphasia, regressive hemiparesis and fluctuating blood pressure values. He was initially admitted to the Neurology Department. There were no focal neurological signs or visual disturbances present in the neurological examination. His cognitive functions appeared normal (GCS = 15 points, NIHSS = 0 points, Karnofsky = 95). He had no history of seizures or sinusitis. The rest of his physical examination was normal. His personal and family medical history was unremarkable. He was subsequently referred to the Radiology Department for a head Magnetic Resonance Imaging (MRI), to investigate the nature of his seizures.
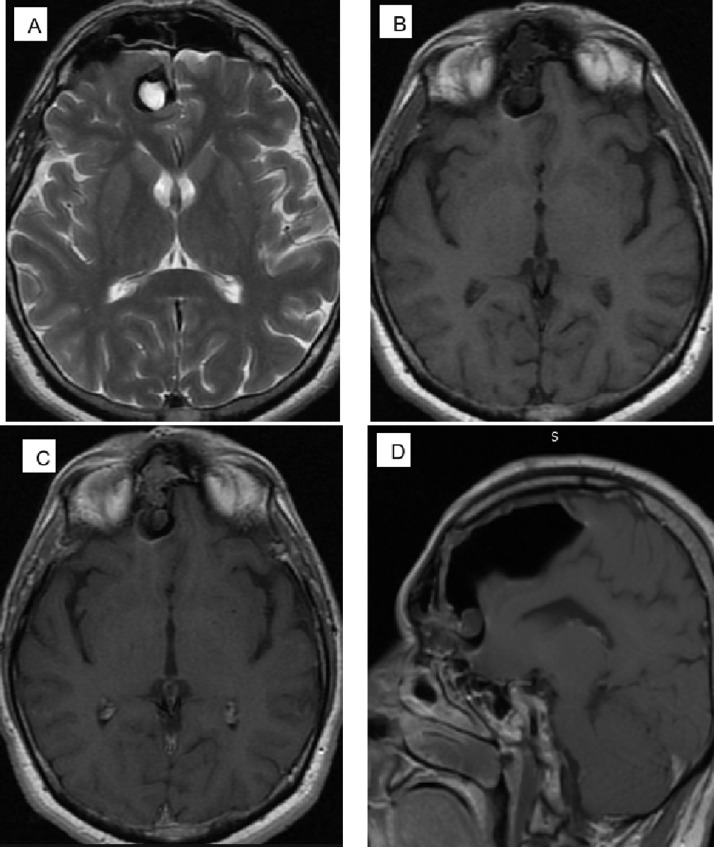
MRI images of the brain were obtained using TSE/T2W sequence in axial and with fat-sat in coronal plane; TSE/T1W sequence in sagittal and axial planes; FLAIR/T2W and HEMO (GRE/T2W) sequence in axial plane. Diffusion weighted and ADC mapping MRI images. Post-ContrastT1W sequence in axial, sagittal and coronal planes. The head MRI revealed a well-defined intracranial, extra-axial cystic expansion immediately posterior and lateral to the osteoma, impressing and displacing the right frontal lobe in addition to the expansion of the osteoma itself.
There was a 75 × 33mm “T2-hypointense” cystic mass involving the anterior basal aspect of the right frontal lobe, with mild peripheral T2-hyperintense gliosis of the adjacent white matter but without any post-contrast enhancement. There was marked susceptibility (blooming) artifact throughout this large intracranial cystic structure.
There was a “T2-hyperintense” mural cystic nodule (20 × 12mm) at the anterior inferior aspect of the described larger cyst, which was in continuation with a lobulated solid component (30 × 19 × 19mm) in the frontal sinus. This solid component showed mild and heterogeneous post-contrast enhancement. There was marked susceptibility (blooming) artifact involving this solid nodular component as well.
Whether the intracranial cystic lesion is an extension of the solid frontal sinus lesion or vice versa is unclear. Given the extensive number of blooming artifacts on HEMO sequence, significant iron deposition is likely within the overall cystic-solid mass (Fig. 1).
Fig. 1.
Case: (A) T2 weighted images in axial plane; (B, C) Axial and sagittal T1-weighted images a well-defined intracranial, extra-axial cystic mass, located behind and lateral to the osteoma, pushing and displacing the right frontal lobe; (D) Axial, (E) Coronal and (F) sagittal contrast-enhanced T1-weighted images.
The patient underwent a complete excision of the calcified mass and the intracerebral mucocele, including obliteration of the sinus and dural repair was performed with right frontal craniotomy. Surgery was successful, with no complications arising in the post-op period. The patient was discharged 5 days after his surgery, fully recovered.
The histopathology showed the cyst contained fibroblastic glial tissue fragments and multilayered mucoproductive cylindrical epithelial fragments. This framework was compatible with that of a mucoid cyst. The solid component contained bone fragments and fibroblastic tissue. Some epithelial elements of the cyst lining were present as well.
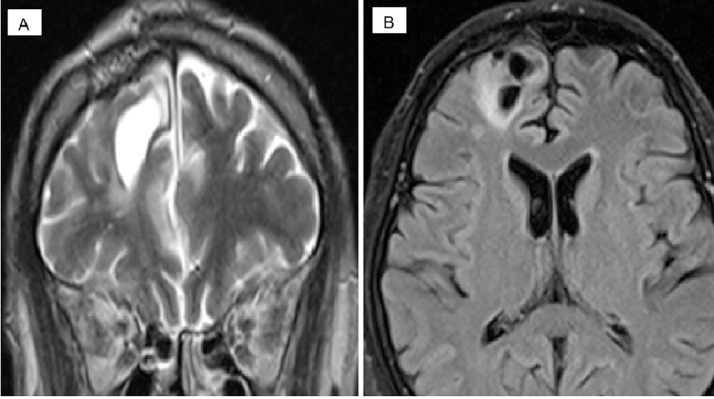
Postoperative MRI revealed a postoperative softening, in the right frontal region, with surrounding gliotic changes, without signs of pathological contrast imbibition (Fig. 2). The patient returned to his normal lifestyle a few months later and is completely asymptomatic to date.
Fig. 2.
Case: Postoperative MRI results: (A) T2 weighted image coronal plane; (B) The FLAIR sequence in the axial plane.
Discussion
Both osteomas and mucoceles represent common, pathological entities of the paranasal sinuses, nevertheless the concomitant presence of both lesions is rare. Existing literature suggests that osteomas precede mucoceles, indeed it is believed they are the source of the sinus ostial obstruction that gives rise to the mucoceles [4–6]. Thus, osteomas are considered the primary tumors and the culprits for the development of mucoceles [4–6]. Additionally, as the lesion cannot extend in the paranasal cavities, due to the obstruction caused by the presence of the osteoma, an intracranial expansion is promoted instead [5–6]. Osteomas associated with mucoceles appear to be more aggressive, with some reports implicating the mucocele component [5].
Other hypothesis on the etiology of osteomas associated with intracranial mucoceles, include the presence of a small ectopic sinus that is not visualized by imaging modalities or during surgery, or the presence of an intracranial communication of the frontal sinus that has disappeared during early childhood [4–6].
The prevalence of secondary mucoceles in patients with osteomas is estimated to be about 50%, with less than 1% of the cases having an intracranial extension [7]. Common clinical manifestations of the intracranial mucoceles occur due to the mass effect or a superimposed infection. Patients present with headaches, ophthalmological disturbances including diplopia and papilledema, as well as neurological anomalies such as abducens palsy, dementia, incontinence, personality changes or seizures [7].
Serious neurological complications include meningitis, encephalitis, epidural, subdural and cerebral abscesses, cerebrospinal fluid rhinorrhea and pneumocephalus [4].
Differential diagnoses to be taken into account when considering a diagnosis of intracranial mucocele, include dermoid and epidermoid cysts, endodermal, ependymal, colloid and Rathke cleft cysts [4].
In our case, the patient presented with generalized seizures precipitated by the intracranial extension of the mucocele. Imaging modalities are of great significance for establishing an accurate diagnosis and clinical management. In the context of a suspected sinus drainage obstruction, intracranial mucocele should be considered in the differential diagnosis of a benign cystic expansion in the anterior cranial fossa. MRI evaluates the distinction between cystic and solid changes and is highly sensitive and specific, representing a golden standard in the differentiation of cystic from neoplastic lesions.
Conclusion
Through this case report, we hope to draw attention to this under recognized pathological entity, in routine neurosurgical practice and emphasize the importance of considering intracranial mucoceles in the differential diagnosis of cystic lesions of the anterior cranial fossa, particularly in the presence of co-existing benign tumors, like an osteoma.
Patient consent
This is to state that I give my full permission for the publication, reproduction, broadcast and other use of photographs, recordings and other audio-visual material of myself and textual material (case histories) in all editions of the above-named product and in any other publication (including books, journals, CD-ROMs, online and inter- net), as well as in any advertising or promotional material for such product or publications. I declare, in consequence of granting this permission, that I have no claim on ground of breach of confidence or any other ground in any legal system against—Kreshnike Dedushi and its agents, publishers, successors, and assigns in respect of such use of the photograph(s) and textual material (case histories). I hereby agree to release and discharge Kreshnike Dedushi and any editors or other contributors and their agents, publishers, successors and assigns from any and all claims, demands or causes of action that I may now have or may hereafter have for libel, defamation, invasion of privacy, copyright or moral rights or violation of any other rights arising out of or relating to any use of my image or case history.
Footnotes
Competing interests: The authors declare that they have no conflict of interest.
Contributor Information
Kreshnike Dedushi, Email: kreshnike.dedushi@uni-pr.edu.
Fjolla Hyseni, Email: fjolla.hyseni@gmail.com.
Juna Musa, Email: musa.juna@gmail.com.
Valon Vokshi, Email: valon.vokshi1@gmail.com.
Atiq Bhatti, Email: arbhattimd@gmail.com.
Ilir Ahmetgjekaj, Email: drilir.a@gmail.com.
Muhammad Tahir, Email: tahirk_tareen@hotmail.com.
Jeton Shatri, Email: jeton.shatri@uni-pr.edu.
References
- 1.Flora Barbara. Paranasal sinus osteoma: case series and a review of the literature. Glob J Oto. 2019;19(4) doi: 10.19080/GJO.2019.19.556017. 2019. [DOI] [Google Scholar]
- 2.Lee Jivianne T. Intracranial mucocele formation in the context of longstanding chronic rhinosinusitis: a clinicopathologic series and literature review. Allergy Rhinol (Providence) 2013;4(3):e166–e175. doi: 10.2500/ar.2013.4.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jurlina Martin. Large intracranial intradural mucocele as a complication of frontal sinus osteoma. J Craniofac Surg. 2010;21(4):1126–1129. doi: 10.1097/SCS.0b013e3181e57228. [DOI] [PubMed] [Google Scholar]
- 4.Nabeshima K. Osteoma of the frontal sinus complicated by intracranial mucocele. Pathol Int. 2003;53(4):227–230. doi: 10.1046/j.1320-5463.2003.01459.x. DOI: 10.1046/j.1320-5463.2003.01459.x. [DOI] [PubMed] [Google Scholar]
- 5.Akay Kamil Melih. Association of paranasal sinus osteoma and intracranial mucocele–two case reports. Neurol Med Chir (Tokyo) 2004;44(4):201–204. doi: 10.2176/nmc.44.201. [DOI] [PubMed] [Google Scholar]
- 6.Sakamoto Hiroki. Frontal sinus mucocele with intracranial extension associated with osteoma in the anterior cranial fossa. Neurol Med Chir (Tokyo) 2011;51(8):600–603. doi: 10.2176/nmc.51.600. [DOI] [PubMed] [Google Scholar]
- 7.Jurlina Martin. Large intracranial intradural mucocele as a complication of frontal sinus osteoma. J Craniofac Surg. 2010;21(4):1126–1129. doi: 10.1097/SCS.0b013e3181e57228. [DOI] [PubMed] [Google Scholar]