Abstract
Originally recognized by Cushing and Bailey, hemangioblastoma is a developmental vascular neoplasm that is predominantly found in the posterior fossa. It is a highly vascularized tumor, with well-differentiated histologic features. Although rare, it remains the most common primary tumor of cerebellum in adults, along with metastases. MRI is the gold standard, allowing a precise characterization of the lesion's features, and its relationship with the surrounding structures. We report the case of a patient with a cerebellar symptomatology, in whom brain MRI raises the diagnosis of hemangioblastoma, which was then confirmed by histopathologic examination.
Keywords: Hemangioblastoma, MRI, Posterior Cerebral Fossa, Histology
Introduction
Hemangioblastoma is a benign vascular neoplasm made up of thin-walled vessels secondary to a developmental disorder. It is usually found in the posterior cerebral fossa and is the most common primary intra-axial and infratentorial tumor in adults. The MRI contribution to the diagnosis is paramount. The spatial resolution and the absence of artefact generated by the petrous pyramid, allow a better tissue characterization and accurate assessment of the surrounding structures. This tumor can present in isolation or as part of a syndromic association with other lesions such as in Von Hippel Lindau disease. A good knowledge of its demographic and especially radiological aspects is essential in order to differentiate from other lesions, to suggest the correct diagnosis, and to carry out further radiological investigations to assess for other anomalies when necessary.
Observation
This is a 54-year-old patient, with no significant past history, who has complained for 2 months of persistent headache associated with vomiting, balance disorder with ataxia, recurrent tremor, as well as nystagmus. The clinical course is marked by worsening of the clinical symptoms, and neurologic examination reveals a cerebellar syndrome. The biological assessment is unremarkable. Faced with this typical clinical presentation, a cerebral MRI was performed. It shows a lesion of the left cerebellar hemisphere, well limited and homogeneous, hypointense in T1 weighted images, before and following injection of Gadolinium, without parietal or intralesional enhancement, and in FLAIR sequences (Fig.1). The lesion is T2 hyperintense (Fig. 2). The diagnosis of a cystic hemangioblastoma is made. The radiological screening concludes with a single brain lesion. The patient undergoes total tumor resection with good postoperative results. Histologic examination concluded with type 1 cerebellar hemangioblastoma.
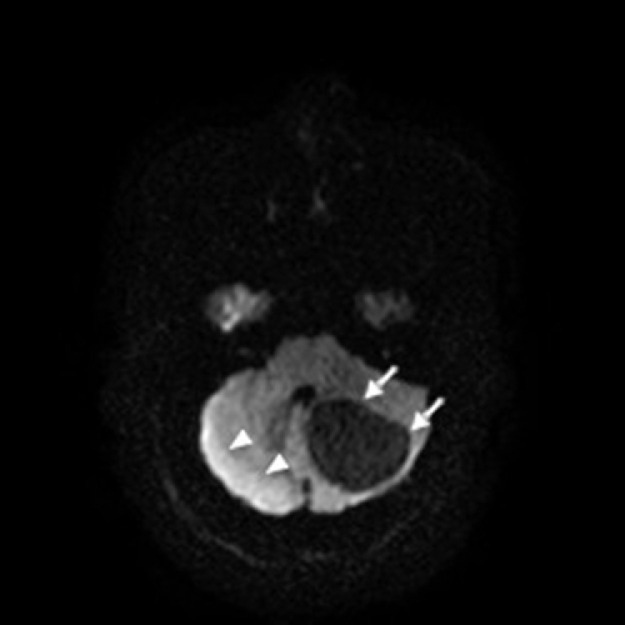
Fig. 3.
Diffusion weighted axial images of a brain MRI. The left cerebellar lesion is hypointense with slight high signal peripherally and in the contralateral cerebellum.
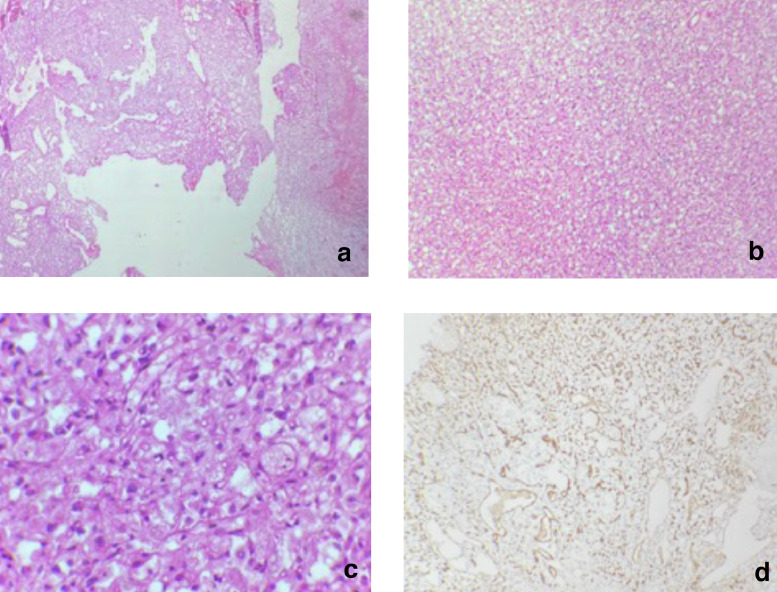
Fig. 4.
Hemangioblastoma histology examination: Compact architectural tumor proliferation (HE, G x 25) (A), made up of stromal cells arranged around many small vessels (HE, Gx 100) (B); Cells have small nuclei that are barely atypical without mitosis (C), and immunohistochemistry detects diffuse expression of the anti-CD34 antibody (HE, Gx 400) (D).
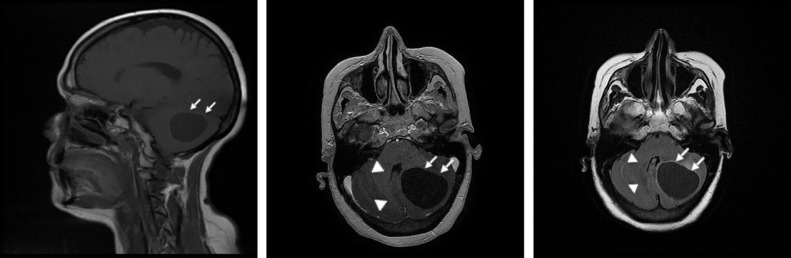
Fig. 1.
Brain MRI sagittal (A) and axial (B,C) T1 weighted images before (A) and following (B) injection of Gadolinium, and FLAIR sequence (C). The left posterior fossa lesion appears well defined, in homogenous low signal without contrast enhancement. There is mass effect upon the adjacent structures (particularly the postero-inferior aspect of the roof of the fourth ventricle).
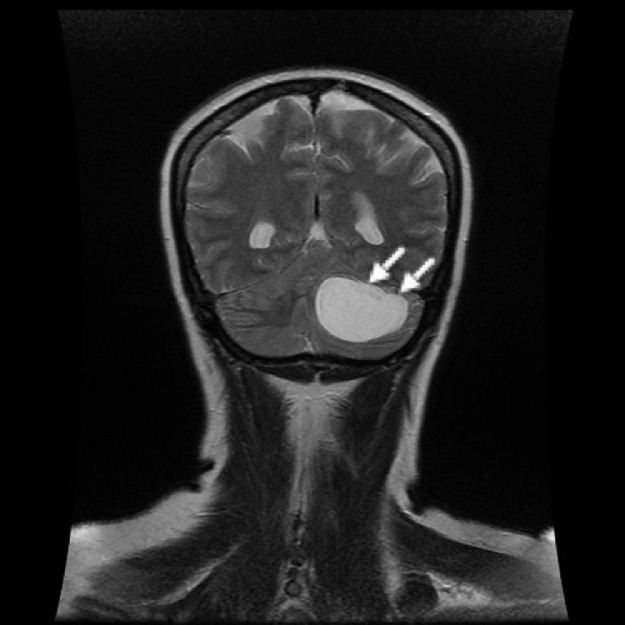
Fig. 2.
Brain MRI coronal image showing a high T2 signal homogenous lesion.
Discussion
Hemangioblastoma is a relatively rare tumor that accounts for 1.5%-2.5% of all brain tumors and 7%-8% of those of the posterior fossa. It is located mainly in the cerebellar hemispheres and thus constitutes 10% of the infratentorial masses in adults [1]. It occurs isolated and sporadically, with a male predominance. However, multiple localizations, in a female patient, and at a younger age can be observed during Von Hippel Lindau's disease [2].
The cerebellar hemispherical location is observed in 72% of cases, followed by vermal (16%) and tonsillar (2%). Four macroscopic aspects (Resche 1971) are described: simple cyst (type I), cyst with a mural nodule (type II), dense tumor (type III), and solid tumor with small internal cysts (type IV). Solid forms followed by cystic ones are the most frequent according to a literature review using 207 articles over 31 years although the opposite idea is more common [2]. This distinction is of clinical and radiological importance. The symptomatology, dominated by cerebellar signs of ataxia, dizziness, headache, especially occipital, and intracranial hypertension, is strongly associated with tumor size and cyst mass effect. This explains that the intracranial hypertension is more frequently encountered in Von Hippel Lindau's (VHL) disease, the result of the cystic form which is the most encountered in VHL disease.
MRI is the gold standard test and demonstrates specific appearances depending on the tumor structure. The cysts appear to be limited, homogeneous in T1 and fluid-attenuated inversion recovery (FLAIR) hypointense, and in T2 hypersignal. The presence of a nodule is revealed by contrast enhancement, usually sitting along the leptomeningeal lining, which does not enhance. The cyst does not have a wall of its own, its margins rather correspond to cerebellar tissue displaced centrifugally by the transudative fluid of the mural nodule. The solid forms have an intermediate T1 signal, with a strong enhancement following Gadolinium injection, a T2 hypersignal and possible areas of signal void, given the hypervascularized nature of the tumor. The enhancement of the cystic wall sometimes indicates tumor extension, as is the case in pilocytic astrocytoma, which represents the main differential diagnosis. However, the younger age of onset, the absence of pial attachment, the rarity of the nodular component and of the association to multiple lesions, and especially the perfusion sequences [3] allow better differentiation before pathologic confirmation. In adults with a single cerebellar nodular lesion, a metastatic origin remains the main concern, The Arterial Spin Labelling sequences are useful to demonstrate the characteristic hypervascular nature of the hemangioblastoma [4].
Immunohistochemical labeling is positive in 80% of cases, mainly for vimentin, vascular endothelial growth factor (VEGF), NSE (Neuron Specific Enolase), and reticulin in decreasing order.
Conclusion
Cerebellar hemangioblastoma is a relatively rare vascular tumor. It is benign in nature but warrants surgical treatment when the mass effect is clinically symptomatic. The multiplicity of tumors, the association with other visceral lesions, the young age of onset and the hereditary nature should prompt to assess for Von Hippel Lindau's disease with the requirement for imaging surveillance.
Footnotes
Competing Interests: None.
References
- 1.Grant LA, Griffin N. 2nd edition. Vol. 1034. Elsevier; 2019. pp. 716–745. (Intracranial tumours. Grainger & Allison's Diagnostic Radiology Essentials: Expert Consult: Online and Print). [Google Scholar]
- 2.Kuharic M, Jankovic D, Splavski B, Boop FA, Arnautovic KI. Hemangioblastomas of the posterior cranial fossa in adults: demographics, clinical, morphologic, pathologic, surgical features, and outcomes. World Neurosurg. 2018;110:e1049–e1062. doi: 10.1016/j.wneu.2017.11.173. [DOI] [PubMed] [Google Scholar]
- 3.Bing F, Kremer S, Lamalle L, Chabardes S, Ashraf A, Pasquier B. Value of perfusion MRI in the study of pilocytic astrocytoma and hemangioblastoma: preliminary findings. J Neuroradiol. 2009;36(2):82–87. doi: 10.1016/j.neurad.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Resche F. Hemangioblastomes. In: Hoerni B, Tubiana M, editors. Tumeurs du système nerveux et de ses enveloppes. editors. Médecine-Sciences-Flammarion; Paris: 1989. pp. 481–495. [Google Scholar]