Highlights
-
•
Improving hypertension control will reduce heart disease and mortality.
-
•
After age 65 years, women are less likely than men to have controlled hypertension.
-
•
Sex differences in hypertension control widen with advancing age.
-
•
Sex differences in hypertension control appear independent of obesity and diabetes.
Keywords: Blood pressure, Hypertension, Hypertension control, Sex, Disparities, Aging, Cardiovascular disease
Abstract
Objective
Determine sex differences in hypertension control by age group in a diverse cohort of adults age 45–84 years at baseline followed for an average of 12 years.
Methods
The Multi-Ethnic Study of Atherosclerosis enrolled 3213 men and 3601 women from six communities in the U.S. during years 2000–2002 with follow-up exams completed approximately every two years. At each exam, resting blood pressure (BP) was measured in triplicate, and the last two values were averaged. Hypertension was defined as a BP ≥ 140/90 mmHg and/or use of antihypertensive medications. Hypertension control was defined as a BP < 140/90 mmHg and in separate analyses as < 130/90 mmHg. Generalized linear mixed effects models with a binomial function were used to calculate the odds of hypertension control by age group (45–64,75–74, 75+) at a given exam and by sex, while accounting for the intra-individual correlation, and adjustment for demographics, co-morbidities, smoking, alcohol use, education and site among participants with hypertension at any of the first five exams.
Results
At baseline, mean age was 64.1 (9.1 [SD]) years, 48.0% were men, and race/ethnicity was Non-Hispanic white in 34.1%, 10.1% Chinese, 35.1% Non-Hispanic Black and 20.7% Hispanic. Average SBP was lower while average DBP was higher among men vs. women at each exam. Adjusted odds ratios of hypertension control defined as BP < 140/90 mmHg among men vs. women was 0.89 (95% CI 0.67, 1.19) for age 45–64 years, 1.37 (95% CI 1.04, 1.81) for age 65–74 years and 2.08 (95% CI 1.43, 3.02) for age 75+ years. When defined as < 130/80 mmHg, adjusted odds of hypertension control among men vs. women was 0.60 (OR 0.60; 95% CI 0.46, 0.79) at age 45–64 years, 1.01 (OR 1.01; 95% CI 0.77, 1.31) at age 65–74 years and 1.71 (95% CI 1.19, 2.45) at age 75+ years.
Conclusion
Sex disparities in hypertension control increase with advancing age and are greatest among adults age 75+ years.
1. Introduction
Cardiovascular disease is the leading cause of mortality and disability-adjusted life years among men and women globally. [1] Over 300,000 women in the U.S. die from heart disease and stroke each year but at least 21,000 of those deaths could be prevented by better hypertension control. [1], [2], [3] Hypertension affects over half of women and men 50 years and older, but after age 65 years, hypertension affects more women (70%) than men (63%). [1, 4] The greater burden of hypertension among older women may be compounded by lower rates of hypertension control compared to men. [4, 5] A recent analysis of the National Health and Nutrition Examination Surveys (NHANES), [4] a population based cross-sectional surveys of non-institutionalized U.S. adults during years 2011-2012 to 2015-2016, showed substantial differences in hypertension control rates by sex and by age. Within the population 65 years and older, rates of hypertension control defined as a systolic and diastolic blood pressure < 140 and < 90 mmHg, respectively, were lower among women (46%) than men (55%). In contrast, hypertension control rates were higher among women than men in the U.S. population age 25–44 years (61% vs. 32%) during this time period. Lower rates of hypertension control among women than men among adults age ≥ 65 years remained consistent across survey years 1999–2000 through 2015–2016. [4]
Studies examining sex disparities in hypertension control among older adults do not account for differences in demographic factors and co-morbidities such as cardiovascular disease (CVD) that could influence blood pressure and hypertension management and control. [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14] We used data from the Multi-Ethnic Study of Atherosclerosis (MESA) to test our hypothesis that hypertension control changes with aging and that these changes differ by sex after controlling for demographics, co-morbidities and education. Identifying sex disparities in hypertension control could inform interventions for improving hypertension management and reducing age-related cardiovascular disease morbidity and mortality.
2. Methods
This longitudinal study utilized data from MESA, an observational cohort designed to study risk factors for subclinical cardiovascular disease. MESA recruited 3213 men and 3601 women, age 45 to 84 years from six communities in the U.S. (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St. Paul, MN) during years 2000–2002 and four subsequent exams occurred every 17 to 20 months through February 2012. A sixth follow-up exam was completed during years 2016–2018. Sampling and recruitment procedures have been described in detail. [15] The Institutional Review Boards at all participating sites approved the study, and all participants gave informed consent.
All participants were free of clinical cardiovascular disease (CVD) and heart failure at baseline per study design. Because the study included CT imaging to measure coronary artery calcium, adults weighing >300 pounds were excluded. This analyses examined systolic blood pressure (SBP), diastolic blood pressure (DBP) and hypertension control by age and sex group among participants with hypertension and among participants on antihypertensive medications at any of the first five exams. Due to the loss of follow-up after the fifth exam (completed in 2012), the main analyses focused on the first five MESA examinations and excluded the 661 participants who died prior to completing the fifth exam. Analyses were repeated with all six exams included and results are shown in Supplemental Tables 5–8. Participants with incomplete blood pressure (BP) data for a given exam were excluded for that exam. Table 1 shows the number of participants with hypertension by sex at each exam after excluding participants with missing BP data and those who died prior to completing the fifth exam. Supplemental Table 1 shows the number of participants who completed each of the six MESA exams by sex.
Table 1.
†Percentage of MESA Participants with Hypertension, and Treated and Controlled Hypertension by Sex and by Exam.
|
% Participants with hypertension (n) |
%Participants on antihypertensive medication (n) |
% Participants on antihypertensive medication with controlled Hypertension (n) |
||||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| Exam1 | 35.9 (1152) | 41.0 (1475) | 75.7 (873) | 77.6 (1144) | +65.8 (575) | 60.9 (697) |
| Exam 2 | 38.2 (1133) | 42.4 (1417) | 81.3 (922) | 82.1 (1263) | *74.5 (687) | 65.2 (758) |
| Exam 3 | *42.0 (1181) | 47.6 (1491) | 86.1 (1017) | 85.5 (1275) | *76.0 (773) | 68.9 (879) |
| Exam 4 | 45.8 (1256) | 49.8 (1530) | 84.1 (1056) | 86.7 (1327) | *78.8 (832) | 71.0 (943) |
| Exam 5 | *60.5 (1332) | 63.1 (1586) | 88.8 (1183) | 87.8 (1393) | *79.2 (938) | 70.6 (984) |
†Excludes MESA participants with missing data on blood pressure and 661 participants who died prior to exam 5; *P < 0.001 compared to women at same exam; +P < 0.05 compared to women at same exam
3. Demographics
MESA participants completed self-administered questionnaires and were interviewed by trained research staff to obtain demographic characteristics, medical history, current medications, and alcohol and tobacco use. These self-administered questionnaires were available in English, Spanish, and Chinese. Participants were asked to report their sex as male or female. Definitions of race and ethnicity were based on responses to queries from the U.S. 2000 census questionnaire. Race and ethnicity were categorized as non-Hispanic (NH) White, NH Black, Chinese or Spanish/Hispanic/Latino.
4. Blood pressure measurement, hypertension and hypertension control
Trained and certified clinic staff obtained BP measurements on all MESA participants during each visit. Each participant's arm circumference was measured at the midpoint from the acromion and olecranon to determine appropriate bladder cuff size. After a 5 min rest, BP was measured three times at 1 min intervals using a Dinamap PRO 100 automated oscillometric device (Critikon, Tampa, FL) with the subject in a seated position with the back and arm supported. BP at each exam was determined by the average of the second and third blood pressure (BP) readings. Participants were asked to bring all current medications to each exam and use of a BP lowering medication was recorded at each exam. Hypertension was defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg and/or use of antihypertensive medications (thiazide diuretics, beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors (ACEI), angiotensin-2 receptor blockers (ARB), and other (-blockers or peripheral vasodilators). Hypertension control was defined as SBP < 140 mm Hg and DBP < 90 mm Hg. Analyses were repeated with hypertension control defined as SBP < 130 mmHg and DBP < 80 mmHg.
5. Covariates
Medical history, and a fasting glucose were collected at baseline at each follow-up exam. Parity and educational status were collected at the baseline exam. Body mass index (BMI) in kg/m2 was calculated from height and weight measured during the examination. Diabetes at each exam was defined by self-reported physician diagnosis, use of insulin or oral hypoglycemic agents), and/or a fasting glucose ≥ 126 mg/dl. Incident cardiovascular disease (CVD) events were assessed by trained personnel who contacted the participants or family members approximately every 6 to 9 months. Reported incident CVD events were adjudicated and classified by the MESA mortality and morbidity review committee. A CVD endpoint included cardiovascular death, resuscitated cardiac arrest, myocardial infarction, angina, stroke, peripheral arterial disease, or congestive heart failure. [16] CVD events that occurred before the fifth MESA exam were included as covariates in the analysis.
6. Statistical analysis
Baseline characteristics of the MESA participants with hypertension and participants on antihypertensive medications were compared by sex for the first five exams. Continuous variables were compared using an unpaired t-test while categorical variables were compared using a chi-square test.
Generalized linear mixed effects models were used to examine the association of sex and age group with SBP and DBP measured at any of the first five exams while generalized linear mixed effects models for the binomial family with logit function were used to examine the association of sex with hypertension control at any of the first five exams. All models accounted for the clustering within sites and intra-individual correlation and adjusted for follow-up time, demographics, smoking and alcohol use status, co-morbidities and education. In all models, age, BMI, smoking status, alcohol use, diabetes and CVD event status were included as time-varying covariates. Fixed effects included race and ethnicity and highest level of education.
In fully adjusted models, an interaction term of sex * age group (45–64, 65–74, 75+ years) was fitted in a mixed effects models and if the sex * age group interaction term reached statistical significance (P < 0.05) then odds of BP control were calculated by sex and by age group and adjusted sex differences in SBP and DBP were calculated by age group. Marginal effects were then used to calculate the adjusted SBP, DBP and probability of hypertension control by sex and by age group. All statistical analyses were performed with Stata v 14.0. Statistical significance was assessed at the alpha 0.05 level.
7. Results
Among the 661 MESA participants (362 men and 299 women) who died prior to exam 5 and were not included in the analyses, overall distribution of age categories and racial/ethnic groups did not differ significantly by sex (Supplemental Table 2). The number of men and women with hypertension, on anti-hypertensive medication and with treated and controlled hypertension at each of the five exams is shown in Table 1. The prevalence of hypertension increased with successive exams and was lower among men than women at all five exams. At baseline, hypertension was present in 35.9% and 40.0% of men and women, respectively. By the fifth exam, the prevalence of hypertension had increased to 60.5% of men and 63.1% of women. No significant differences in antihypertensive medication use were noted between men and women during any of the exams with over 75% of hypertensive men and women treated. Over 60% of all treated hypertension was controlled among men and women. However, at each exam, the prevalence of treated and controlled hypertension was higher among men than women including the baseline exam (65.8% vs. 60.9%; P = 0.02) and the fifth exam (79.2% vs. 70.6%; P < 0.001).
The characteristics of the MESA participants with hypertension (treated and untreated) at a given exam are shown by sex and by exam in Table 2. Among MESA participants with hypertension, mean age did not differ by sex at any of the exams and ranged from 63.9 (Standard Deviation [SD] 9.0) and 64.3 (SD 9.2) years among men and women, respectively, at baseline to 71.8 (SD 9.2) and 72.0 (SD 9.3) years, respectively, at the fifth exam. Although BMI was significantly lower among men than women at each exam, the prevalence of diabetes mellitus was consistently higher among men than women at each exam. Men were also more likely to report current smoking and alcohol use at each exam. With increasing follow-up time, average SBP and DBP declined in both sexes but average SBP was lower while average DBP was higher among men vs. women at each exam. Isolated systolic hypertension defined as a SBP ≥ 140 mmHg and DBP <90 mmHg accounted for 30.4%, 41.5% and 47.8% of hypertension among women at age 45–64 years, 65–74 years and 75+ years, respectively. Among men, isolated systolic hypertension was less prevalent compared to women and accounted for 20.8%, 30.6% and 35.2% of hypertension at age 45–64 years, 65–74 years and 75+ years, respectively.
Table 2.
†Characteristics of MESA participants with hypertension by exam and by sex.
| Exam 1 |
Exam 2 |
Exam 3 |
Exam 4 |
Exam 5 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n) | Men (1152) | Women (1475) | Men (1130) | Women (1406) | Men (1179) | Women (1490) | Men (1249) | Women (1525) | Men (1332) | Women (1586) |
| Age, mean years | 63.9 (±9.0) | 64.3 (±9.2) | 65.3 (±8.9) | 65.7 (±9.3) | 66.7 (±9.0) | 66.7 (±9.4) | 68.3 (±9.1) | 68.3 (±9.2) | 71.8 (±9.2) | 72.0 (±9.3) |
| Age range, years | 45-84 | 45-84 | 47-85 | 47-85 | 49-87 | 48-87 | 50-89 | 50-89 | 55-93 | 54-93 |
| < 65 years, % | 47.2 | 47.9 | 43.0 | 43.1 | 40.1 | 40.7 | 34.5 | 34.8 | 24.9 | 25.4 |
| 65-75 years, % | 39.9 | 37.8 | 40.3 | 37.3 | 38.6 | 36.5 | 38.2 | 37.4 | 33.4 | 32.1 |
| 75+ years, % | 12.9 | 14.4 | 16.7 | 19.6 | 21.3 | 22.8 | 27.4 | 27.9 | 41.7 | 42.5 |
| NH White, % | 36.6++ | 32.1 | 37.0++ | 32.5 | 37.4++ | 34.5 | 38.0++ | 34.2 | 38.5++ | 35.1 |
| Chinese, % | 11.3 | 9.2 | 11.2 | 8.5 | 12.0 | 8.8 | 11.0 | 9.0 | 11.0 | 9.3 |
| NH Black, % | 32.3 | 37.3 | 32.0 | 37.4 | 31.0 | 35.2 | 30.7 | 35.0 | 28.9 | 34.4 |
| Hispanic, % | 19.5 | 21.4 | 19.8 | 21.9 | 19.6 | 21.5 | 20.3 | 21.8 | 21.6 | 21.3 |
| SBP, mmHg | *134.0 (±19.2) | 137.5 (±21.9) | *132.4 (±20.0) | 136.0 (±22.6) | *130.0 (±20.1) | 133.4 (±22.1) | *129.6 (±20.3) | 132.7 (±22.2) | *128.0 (±21.3) | 132.3 (±22.6) |
| DBP, mmHg | *78.6 (±10.1) | 72.7 (±10.4) | *75.9 (±10.5) | 70.6 (±10.5) | *74.7 (±10.4) | 69.5 (±10.2) | *73.9 (±10.7) | 69.0 (±10.1) | *71.0 (±10.8) | 67.7 (±10.2) |
| BMI, kg/m2 | *28.7 (±4.5) | 30.2 (±6.3) | *28.8 (±4.6) | 30.4 (±6.4) | *28.6 (±4.6) | 30.2 (±6.4) | *28.8 (±4.7) | 30.2 (±6.6) | *28.7 (±5.0) | 29.7 (±6.3) |
| DM, % | 19.0 | 16.2 | 22.7 | 19.7 | +23.7 | 20.0 | +25.3 | 21.7 | +28.7 | 24.1 |
| Smokers, % | 11.0 | 9.1 | +9.7 | 6.7 | *10.2 | 7.2 | 9.2 | 7.3 | +8.3 | 6.1 |
| Alcohol use, % | +69.6 | 37.0 | *60.8 | 38.1 | *58.9 | 38.6 | *58.1 | 32.9 | *49.5 | 32.2 |
| < High School education, % | *16.4 | 21.6 | *15.5 | 20.4 | *16.1 | 19.2 | *15.9 | 19.7 | *14.8 | 17.6 |
Data shown as mean (± standard deviation) or frequency; †Excludes MESA participants with missing data on blood pressure and 661 participants who died prior to exam 5; *P < 0.001 compared to women at same exam; +P < 0.05 compared to women at same exam; ++Distribution of race/ethnicity differs significantly between men and women, P < 0.05;
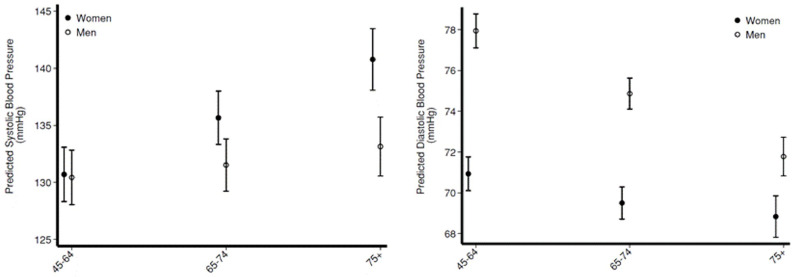
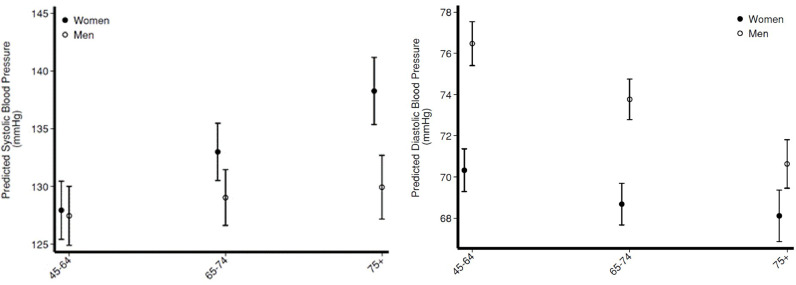
The sex * age group interaction terms were statistically significant in linear mixed effects models when SBP was the dependent variable (Supplemental Table 4) in fully adjusted models that included participants with hypertension at any of the first 5 exams. Table 3 and Fig. 1 shows the adjusted SBP (left panel) and DBP (right panel) in participants with hypertension at any of the first five exams by sex and by age group. No significant differences in adjusted mean SBP were noted in men vs. women in age group 45–64 years (-0.26 mmHg; 95% CI -2.28, 1.76). However, adjusted average SBP was significantly lower among men vs. women at age 65-74 years (-4.14 mmHg; 95% CI -6.04, -2.24) and age 75+ years (-7.63 mmHg; 95% CI -10.17, -4.08). In contrast, after adjustment for covariates, average DBP was significantly higher among men vs. women at age 45-64 years (7.01 mmHg; 95% CI 6.03, 7.99), age 65–74 years (5.36; 95% CI 4.44, 62.8) and age 75+ years (2.94; 95% CI 1.73, 4.16). Similar findings were noted among men and women on antihypertensive medication (Fig. 2).
Table 3.
Adjusted systolic and diastolic blood pressure and proportion with controlled hypertension by sex and age group among MESA participant with hypertension at a given exam. Predicted blood pressure is determined using mixed effects models which accounts for site and the intra-individual correlation and adjusts for follow-up time, race/ethnicity, educational attainment, smoking and alcohol use at the time of the exam, diabetes status and body mass index at the exam and accounts for site. Hypertension defined as use of blood pressure lowering medications and/or a systolic blood pressure ≥ 140 or a diastolic blood pressure ≥ 90 mmHg. Controlled hypertension was defined as a systolic blood pressure < 140 mmHg and a diastolic blood pressure < 90 mmHg or a systolic blood pressure < 130 mmHg and a diastolic blood pressure < 80 mmHg.
| Men | Women | Men | Women | Men | Women | |
|---|---|---|---|---|---|---|
| All Hypertensives 45–64 years 65–75 years 75+ years | ||||||
| Predicted Systolic blood pressure, mmHg (95% CI) | 130.4 (138.0, 132.8) | 130.7 (128.3, 133.1) | 131.5 (129.2, 133.8) | 135.6 (133.3, 138.0) | 133.1 (130.6, 135.7) | 140.8 (138.1, 145.5) |
| Predicted Diastolic blood pressure, mmHg (95% CI) | 77.9 (77.1, 78.8) | 70.9 (70.1, 71.8) | 74.9 (74.1, 75.6) | 69.5 (67.8, 69.8) | 71.8 (70.8, 72.7) | 68.8 (67.8, 69.8) |
| Predicted proportion with controlled hypertension defined as BP < 140/90 mmHg (95% CI) | 0.63 (0.58, 0.67) | 0.65 (0.61, 0.69) | 0.2 (0.58, 0.66) | 0.57 (0.53, 0.61) | 0.60 (0.55, 0.65) | 0.48 (0.42, 0.53) |
| Predicted proportion with controlled hypertension defined as BP < 130/80 mmHg | 34.1 (30.3, 38.0) | 41.8 (37.6, 46.0) | 37.3 (33.4, 41.1) | 37.1 (33.1, 41.2) | 36.3 (31.7, 40.8) | 28.6 (24.1, 33.1) |
| Treated Hypertensives 45-64 years 65-75 years 75+ years | ||||||
| Predicted Systolic blood pressure, mmHg (95% CI) | 127.4 (124.9, 130.0) | 127.9 (125.4, 130.4) | 129.0 (126.6, 131.4) | 133.0 (130.5, 135.5) | 129.9 (127.2, 132.7) | 138.3 (135.4, 141.2) |
| Predicted Diastolic blood pressure, mmHg (95% CI) | 76.5 (75/4. 77/5) | 70.3 (69.3, 71.4) | 738 (72.7, 74.9) | 68.7 (67.7, 69.7) | 70.6 (69.5, 71.8) | 68.1 (66.9, 69.4) |
| Predicted proportion with controlled hypertension defined as BP < 140/90 mmHg (95% CI) | 0.74 (0.70, 0.78) | 0.75 (0.71, 0.78) | 0.71 (0.67, 0.75) | 0.65 (.61, 0.69) | 0.71 (0.66, .76) | 0.56 (0.50, 0.62) |
| Predicted proportion with controlled hypertension defined as BP < 130/80 mmHg | 52.0 (46.7, 57.4) | 55.6 (50.5, 60.8) | 49.8 (44.9, 54.8) | 48.3 (43.1, 53.5) | 47.8 (41.9, 53.8) | 35.2 (29.3, 41.2) |
Fig. 1.
Adjusted systolic blood pressure (left panel) and diastolic blood pressure (right panel) at the age of a given Multi-Ethnic Study of Atherosclerosis follow-up exam for participants with hypertension at the exam. Hypertension was defined as use of blood pressure lowering medications and/or a systolic blood pressure ≥ 140 or a diastolic blood pressure ≥ 90 mmHg. Predicted blood pressure is determined using linear mixed effects models and then marginal effects. Models account for the clustering within sites and the intra-individual correlation and adjusts for race/ethnicity, follow-up time, educational attainment, and time-varying covariates for smoking and alcohol use, diabetes status, body mass index, and incident cardiovascular disease.
Fig. 2.
Adjusted systolic blood pressure (left panel) and diastolic blood pressure (right panel) at the age of a given Multi-Ethnic Study of Atherosclerosis follow-up exam for participants on antihypertensive medication at a given exam. Predicted blood pressure is determined using linear mixed effects models and then marginal effects. Models account for the clustering within sites and the intra-individual correlation and adjusts for race/ethnicity, follow-up time, educational attainment, and time-varying covariates for smoking and alcohol use, diabetes status, body mass index, and incident cardiovascular disease.
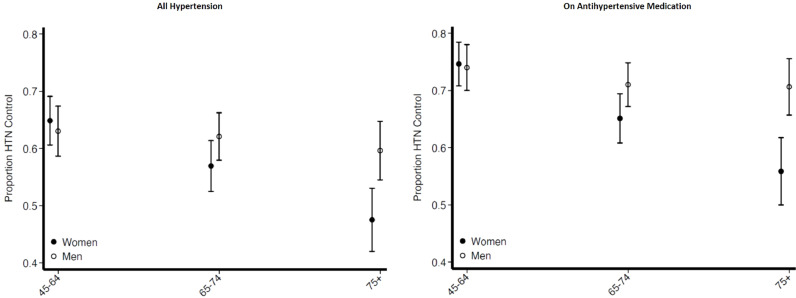
In the fully adjusted model that included participants with hypertension at any of the first five exams and with hypertension control as the dependent variable, the sex * age group interaction terms were significant for age group 65–74 vs. age < 65 years (P < 0.05) and for age group 75+ years vs. age < 65 years (P < 0.001) (Supplemental Table 4). Fig. 3 shows the proportion with hypertension control by sex and by age at a given exam after adjustment for all covariates among all participants with hypertension (left panel). The adjusted proportion of hypertension control among women fell from 64.9% (95% CI 60.6, 69.1) in age group 45–64 years to 57.0% (95% CI 52.5, 61.4) in age group 65–74 years to 47.5% (95% CI 42.0, 53.0) in age group 75+ years (Fig. 3). In contrast, the adjusted proportion of hypertension control was relatively consistent across age groups in men ranging from 63.0% (95% CI 58.7, 67.4) in age group 45–64 years to 59.6% (95% CI 54.5, 64.8) in age group 75+ years. When participants were between age 45-64 years, no significant difference in the adjusted odds of hypertension control was noted between men and women (Odds Ratio [OR] 0.89; 95% CI 0.67, 1.19). However, when participants were age 65–74 years, odds of hypertension control was 1.37 fold (95% CI 1.04, 1.81) higher among men than women. Sex disparities in hypertension control were even larger in the age group 75+ years with a 2.08-fold (95% CI 1.43, 3.02) higher odds of hypertension control among men than women. When the ACC/AHA 2017 hypertension guideline definition for hypertension control of SBP/DBP <130/<80 mmHg was applied, adjusted odds of hypertension control was significantly lower (OR 0.60; 95% CI 0.46, 0.79) among men than women age 45-64 years, and similar among men and women age 65-74 years (OR 1.01; 95% CI 0.77, 1.31) and 1.71 fold (95% CI 1.19, 2.45) higher among men than women age 75+ years.
Fig. 3.
Adjusted proportion of all hypertensive participants (Left Panel) and participants on antihypertensive medication (Right Panel) with controlled hypertension at the age group for a given Multi-Ethnic Study of Atherosclerosis follow-up exam. Hypertension was defined as use of blood pressure lowering medications and/or a systolic blood pressure ≥ 140 or a diastolic blood pressure ≥ 90 mmHg. Controlled hypertension was defined as a systolic blood pressure < 140 mmHg and a diastolic blood pressure < 90 mmHg. Proportion of hypertension control is determined using linear mixed effects models for the binomial family and then marginal effects. Models account for the clustering within sites and the intra-individual correlation and adjusts for race/ethnicity, follow-up time, educational attainment, and time-varying covariates for smoking and alcohol use, diabetes status, body mass index, and incident cardiovascular disease.
The adjusted proportion of hypertension control also declined with advanced age in women but not men on antihypertensive medication at any of the first five MESA exams (Fig. 3 right panel). Adjusted odds of hypertension control in participants on antihypertensive medication were similar in men vs. women in age group 45–64 years (OR 0.96; 95% CI 0.69, 1.32) but higher among men age 65–74 years (OR 1.46; 95% CI 1.08, 1.97) and age 75+ years (OR 2.45; 95% CI 1.62, 3.72). Adjusted odds of hypertension control defined as BP < 130/80 mmHg among participants on antihypertensive medications were not significantly different among men vs. women for age 45-64 years (OR 0.81; 0.59, 1.11), or age 65-74 years (OR 1.09; 95% CI 0.81, 1.48) but were over two-fold higher among men vs. women age 75+ years (OR 2.15; 95% CI 1.42, 3.25).
8. Discussion
In this diverse cohort age 45-84 years at baseline, men were more likely than women to have controlled hypertension at each follow-up exam. After adjustment for demographics and co-morbidities, adjusted odds of hypertension control did not differ by sex for participants age 45-64 years but higher adjusted odds of hypertension control among men vs. women was noted with age 65-74 years. These sex disparities in hypertension control widened with participants age 75+ years and the adjusted odds of hypertension control was approximately two-fold higher in men than women in this age group. Of note, our findings were derived from a cohort that was free of clinical cardiovascular disease at baseline and followed for a mean of 12 years.
Our findings are consistent with a cross-sectional analysis of data from 152,561 patients with incident hypertension from three integrated healthcare systems. Daugherty and colleagues reported that hypertension control rates differed by age group among women. Among women < 49 years, blood pressure was controlled in 49.4% but among women age ≥65 years, hypertension was controlled in 41.5%. In contrast, hypertension control rates were more stable across age groups in men with 41.5% and 42.5% of men age < 49 years and ≥65 years, respectively, with controlled hypertension. Among all adults with incident hypertension who were ≥ 65 years, odds of hypertension control was 11% lower among women than men (95% CI 7%, 14%). [5]
The age-related decline in hypertension control rates among women is also supported by data from the NHANES. [4,17] During survey years 2015–2016, hypertension control was 52.5% among women and 45.7% among men. However, hypertension control fell progressively with advancing age among women with rates declining from 62.6% of women age 18-39 years, to 54.2% at 40-59 years, and 49.2% at 60 years and older. In contrast, hypertension control rose progressively with age in men with rates of 15.5% at 18-39 years to 49.7% at 60 years and older. Data from NHANES periods from 2011–2016 also document sex disparities among adults age 65+ years with hypertension controlled in 46.2% of women compared to 55.1% of men. [4] Observed rates of hypertension control are higher in MESA vs. NHANES because MESA is a selected sample with exclusion of prevalent cardiovascular disease at baseline and with research study participation as an additional selection factor.
The greater increase in prevalent hypertension with aging among women than men is well described and has been attributed in part to differences in height [18] and the decline in estrogen levels with menopause. [4,8,17] However, estrogen replacement does not lower blood pressure or reduce risk of incident hypertension in women. [19] In the MESA cohort, prevalent hypertension was significantly greater among women vs. men at each exam. However, we show that hypertension control rates among those with treated hypertension are lower among women than men and that this disparity is greatest among those 75+ years.
Our findings and previous studies [4,8,17, [20], [21], [22], [23], [24]] of sex disparities in hypertension control rates in older adults is important because hypertension remains the most important and modifiable risk factor for heart disease in women. At least one-third of all cardiovascular disease deaths among women is attributed to poor hypertension control. [1,2] Based on population data, hypertension control alone would prevent over 7% (∼21,000) of heart disease related deaths in women every year. [2,3] Uncontrolled hypertension is also an important yet modifiable risk factor for the development of heart failure, a debilitating disease associated with chronic fatigue, repeated hospitalizations and reduced quality of life. New cases of heart failure among women exceed 500,000 each year and incident heart failure among women is similar if not greater than among men. [25] While the burden of obesity and diabetes among women fuel risk, hypertension is the strongest modifiable risk factor for heart failure among women. [24,25] More than one-quarter of all heart failure (28%) cases among women is attributed to elevated blood pressure compared to approximately one out of eight (13%) heart failure cases among men. [1] In other words, if uncontrolled hypertension was eliminated among women, more than one-quarter of all new heart failure cases could be prevented. Unless hypertension control rates improve over the next decade, the total number of US women living with heart failure will exceed 4 million in 2030, a 50% increase in current prevalence. [1]
The reasons for lower rates of hypertension control among older women have not been fully elucidated but may be partially explained by factors such as poor compliance to treatment and/or provider therapeutic inertia. A previous analysis of the 2005–2011 National Ambulatory Care Survey data showed significantly lower prevalence of medication escalation in women than men with uncontrolled hypertension but the study did not examine whether sex differences varied by age group. [8] In addition, a previous analysis demonstrated that female sex was an independent predictor of apparent treatment resistant hypertension defined as uncontrolled hypertension with use of ≥ 3 blood pressure lowering medications. [26] Other studies suggest that mental health issues and poor communication with healthcare providers are operative. [27] Thus, reasons for lower rates of hypertension control among older women may include both patient and provider level factors. While more studies are needed, clinicians and healthcare systems should consider examining hypertension control rates by both age group and sex in order to elucidate potential sex disparities and consider strategies to improve hypertension control rates in both men and women.
The strengths of this study include the wide age range of the MESA participants at baseline and a twelve-year follow-up period which facilitated the analysis of blood pressure and hypertension control rates with advancing age. MESA also includes four different racial/ethnic groups and blood pressure was measured using standardized methods. The analyses also adjusted for incident CVD events and diabetes mellitus. Multiple factors that can influence hypertension control rates were not addressed such as physical activity, diet and insurance coverage and such factors may change with advancing age and differ by sex. The longitudinal design allowed the examination of changes in blood pressure and hypertension control with aging. To account for survivor bias, we excluded participants who died prior to the fifth exam so not all MESA participants with hypertension were included in the analysis. MESA also excluded persons with clinical cardiovascular disease from enrollment. MESA is also not a representative sample of the US population and so findings may not be generalizable to all older adults.
9. Conclusion
After age 65 years, hypertension control rates are lower among women vs. men and these sex differences widen with advancing age. More research is needed to determine reasons for these age and sex differences in hypertension control. Quality improvement programs for hypertension control should include targeted interventions for older women to reduce their risk for cardiovascular disease and mortality.
Declaration of Competing Interest
Brent Egan, Michael Rakotz, and Gregory Wozniak are employed by Target BP. All other authors have no disclosures to report.
Acknowledgments
Acknowledgements
The authors would like to thank all of the MESA participants for their time and effort in participating in this cohort.
Author Contributions
NO: Conceptualization, writing original draft and revising; RD: Formal analysis, writing-review and editing; TM: Methodology, writing-review and editing; KL: Funding acquisition, methodology, writing-review and editing; EM: Methodology, writing-review and editing; MR: Writing-review and editing; GW:Methodology, writing-review and editing; BE-Writing-review and editing; HK:Supervision, conceptualization, project administration, writing-review and editing.
Source of funding
NIDDK 1R01DK104842-01 and by contracts 75N92020D00001, HHSN268201500003I, N01-HC-95159, 75N92020D00005, N01-HC-95160, 75N92020D00002, N01-HC-95161, 75N92020D00003, N01-HC-95162, 75N92020D00006, N01-HC-95163, 75N92020D00004, N01-HC-95164, 75N92020D00007, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from the National Center for Advancing Translational Sciences (NCATS)
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100230.
Appendix. Supplementary materials
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R. Heart disease and stroke statistics-2017 update: a report from the american heart association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel SA, Winkel M, Ali MK, Narayan KM, Mehta NK. Cardiovascular mortality associated with 5 leading risk factors: national and state preventable fractions estimated from survey data. Ann Intern Med. 2015;163:245–253. doi: 10.7326/M14-1753. [DOI] [PubMed] [Google Scholar]
- 3.Bress AP, Kramer H, Khatib R, Beddhu S, Cheung AK, Hess R. Potential deaths averted and serious adverse events incurred from adoption of the SPRINT (systolic blood pressure intervention trial) intensive blood pressure regimen in the united states: projections from NHANES (national health and nutrition examination survey) Circulation. 2017;135:1617–1628. doi: 10.1161/CIRCULATIONAHA.116.025322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment and control in US Adults: trends in the hypertension control cascade by population subgroup (NHANES 1999-2016) Am J Epidemiol. 2019 doi: 10.1093/aje/kwz177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daugherty SL, Masoudi FA, Ellis JL, Ho PM, Schmittdiel JA, Tavel HM. Age-dependent gender differences in hypertension management. J Hypertens. 2011;29:1005–1011. doi: 10.1097/HJH.0b013e3283449512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chowdhury EK, Owen A, Krum H, Wing LM, Ryan P, Nelson MR. Barriers to achieving blood pressure treatment targets in elderly hypertensive individuals. J Hum Hypertens. 2013;27:545–551. doi: 10.1038/jhh.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 8.Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–1155. doi: 10.1161/HYPERTENSIONAHA.107.107342. [DOI] [PubMed] [Google Scholar]
- 9.Brindel P, Hanon O, Dartigues JF, Ritchie K, Lacombe JM, Ducimetière P. Prevalence, awareness, treatment, and control of hypertension in the elderly: the Three City study. J Hypertens. 2006;24:51–58. doi: 10.1097/01.hjh.0000198028.84353.86. [DOI] [PubMed] [Google Scholar]
- 10.Hennein R, Hwang SJ, Au R, Levy D, Muntner P, Fox CS, Ma J. Barriers to medication adherence and links to cardiovascular disease risk factor control: the Framingham Heart Study. Intern Med J. 2018;48:414–421. doi: 10.1111/imj.13687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Majernick TG, Zacker C, Madden NA, Belletti DA, Arcona S. Correlates of hypertension control in a primary care setting. Am J Hypertens. 2004;17:915–920. doi: 10.1016/j.amjhyper.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 12.Primatesta P, Poulter NR. Hypertension management and control among English adults aged 65 years and older in 2000 and 2001. J Hypertens. 2004;22:1093–1098. doi: 10.1097/00004872-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008-11. J Hum Hypertens. 2015;29:247–253. doi: 10.1038/jhh.2014.82. [DOI] [PubMed] [Google Scholar]
- 14.Van der Niepen P, Dupont AG. Improved blood pressure control in elderly hypertensive patients: results of the PAPY-65 Survey. Drugs Aging. 2010;27:573–588. doi: 10.2165/11537350-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 16.Ito H, Pacold I, Durazo R, Liu K, Shilipak MG, Goff DC. Abstract 8982: the effect of including cystatin C or creatinine in cardiovascular risk model for asymptomatic individuals. The multi-ethnic study of atherosclerosis. Circulation. 2010;122:A8982. doi: 10.1093/aje/kwr185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017;(289):1–8. [PubMed] [Google Scholar]
- 18.Smulyan H, Marchais SJ, Pannier B, Guerin AP, Safar ME, London GM. Influence of body height on pulsatile arterial hemodynamic data. J Am Coll Cardiol. 1998;31:1103–1109. doi: 10.1016/s0735-1097(98)00056-4. [DOI] [PubMed] [Google Scholar]
- 19.Swica Y, Warren MP, Manson JE, Aragaki AK, Bassuk SS, Shimbo D. Effects of oral conjugated equine estrogens with or without medroxyprogesterone acetate on incident hypertension in the Women's Health Initiative hormone therapy trials. Menopause. 2018;25:753–761. doi: 10.1097/GME.0000000000001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gu Q, Burt VL, Paulose-Ram R, Dillon CF. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: data from the national health and nutrition examination survey 1999-2004. Am J Hypertens. 2008;21:789–798. doi: 10.1038/ajh.2008.185. [DOI] [PubMed] [Google Scholar]
- 21.Oparil S. Women and hypertension: what did we learn from the women's health initiative? Cardiol Rev. 2006;14:267–275. doi: 10.1097/01.crd.0000240530.94242.0c. [DOI] [PubMed] [Google Scholar]
- 22.Ramirez LA, Sullivan JC. Sex differences in hypertension: where we have been and where we are going. Am J Hypertens. 2018;31:1247–1254. doi: 10.1093/ajh/hpy148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muiesan ML, Salvetti M, Rosei CA, Paini A. Gender differences in antihypertensive treatment: myths or legends? High Blood Press Cardiovasc Prev. 2016;23:105–113. doi: 10.1007/s40292-016-0148-1. [DOI] [PubMed] [Google Scholar]
- 24.Wenger NK, Arnold A, Bairey Merz CN, Cooper-DeHoff RM, Ferdinand KC, Fleg JL. Hypertension across a woman's life cycle. J Am Coll Cardiol. 2018;71:1797–1813. doi: 10.1016/j.jacc.2018.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holt E, Joyce C, Dornelles A, Morisky D, Webber LS, Muntner P, Krousel-Wood M. Sex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2013;61:558–564. doi: 10.1111/jgs.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.