Abstract
Purpose
The purpose of this study was to systematically review and synthesize factors that influence learners’ perceptions of credibility when feedback is provided by an authority figure in a healthcare environment.
Methods
This study reviewed literature from medicine, psychology, and education using systematic review and qualitative synthesis methods. In a multi-step process, major electronic bibliographic databases were searched for relevant studies until October 2020.
Results
The search identified 9216 articles. A total of 134 abstracts underwent full-text review. Of these, 22 articles met inclusion criteria. The studies were heterogenous and the majority utilized a qualitative design with interviews and focus groups. A few studies employed mixed methodology (n = 2) and two studies used a quantitative design. Four main themes were identified: feedback characteristics, context of feedback, source credibility, and recipient characteristics.
Conclusion
As programs implement major educational change initiatives to create more formative assessment practices, feedback will become even more crucial. The four main themes identified are important factors that contribute to the perception of feedback credibility. While the factors are described independently, they may be viewed as interrelated and the association between these factors and feedback may be driven more by learning culture than each characteristic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40670-020-01167-w.
Keywords: Feedback, Feedback credibility, Assessment, Evaluation, Systematic review, Believability
Introduction
Feedback is integral to learning and improvement [1–4] and, in health professional education, is shown to be linked to patient safety outcomes [5]. Despite a lack of consensus on the definition of feedback [6], high-quality feedback is a well-established and powerful tool in education [7–9]. We describe feedback as the presentation of evaluative information, and the delivery of which is a skill. Despite our best efforts, not all feedback is valuable, and while improvement rarely happens without feedback, one-third of feedback has shown to be detrimental to performance [10].
Despite its widely accepted importance, learners in healthcare settings have reported faculty feedback as infrequent, vague, and ineffective [11], often contrary to the belief held by educators who believe feedback is frequent and plentiful [6, 12]. Though literature focusing on the perspective of the learner is still scarce [5], feedback research is shifting from a teacher-focused model to a learner-centric model [13]. The shift in focus follows the recognition that feedback is no longer a one-way flow of information from the giver to the learner [14] and efforts should be taken to maximize the uptake and effectiveness of feedback by studying the contexts and characteristics of this social transaction.
Feedback is influenced by characteristics of the giver and the receiver and the context in which it is given [14, 15]. Not all feedback is remembered or acted upon by the learner [16]. Once feedback has been relayed, students exhibit a complex behavioral reaction. They recognize the information as feedback, process the information, recognize their potential for change, and decide to act [17]. This process must be completed in full and acted on appropriately for feedback to be useful. Effective feedback is described as specific, credible, timely, and relevant, and is given at a time when the learner is emotionally and cognitively prepared to accept it [17–20].
We chose to review credibility of feedback because it plays a significant role in the decision to engage or disregard feedback [1, 21]. Learners process feedback through credibility filters before ultimately deciding to engage or disregard [22, 23]. In addition, there has yet to be comprehensive examination of factors that influence the believability of feedback in healthcare education. This review directly consolidates our current knowledge of feedback credibility and acceptance, clarifies the roles credibility plays in various aspects of effective feedback, and guides future discourse pertaining to feedback systems in healthcare education.
The purpose of this study is to provide a systematic review on the variables that influence learners’ decision-making around determining credibility of feedback provided by an authority figure. By synthesizing these variables, this paper hopes to further the feedback process.
Methods
This study draws on systematic review and qualitative synthesis methods [24] following PRISMA guidelines [25] to capture major factors that influence learners’ perceptions of credibility when provided feedback from their respective supervisors within educational settings of healthcare disciplines.
Search Strategy
In a multi-step process, PsycINFO, MEDLINE, EMBASE, ERIC, and CINAHL electronic bibliographic databases were searched for relevant studies from each databases’ beginning date until October 2020. In combination with MeSH subject heading terms according to each database (see Appendix I for each search strategy), keywords used in the search strategies included feedback, credibility or credible, and education.
Inclusion and Exclusion Criteria
Published, peer-reviewed, English language studies describing a supervisor-learner dynamic between health professionals within an adult learner population in a healthcare setting were included. All others were excluded. Studies were identified through the literature searches and their abstracts underwent an independent inclusion review process by investigators CD and KB. The research team met frequently to review articles and come to consensus on disagreements and discrepancies in eligibility requirements.
All studies that met inclusion criteria were fully reviewed by CD and KB, and all relevant studies were included in the review (Table 1).
Table 1.
Inclusion and exclusion criteria
| Inclusion | Exclusion |
|---|---|
| • Must be a study that is peer-reviewed and fully published papers | • Systematic review |
| • English language | • Undergraduate student populations not in a healthcare-related profession |
| • Must describe teacher-student or supervisor-trainee relationship between feedback source and recipient | |
| • Participants < 18 years of age | |
| • Healthcare-related educational program, i.e., medicine, nursing, allied health programs |
Data Extraction
From all included articles, investigators (CD and KB) independently reviewed and extracted the objective, study design, analytic approach, sample size, demographic of participants, feedback setting, feedback format, and factors that were identified that influenced feedback credibility. Although many components of effective or valuable feedback were often mentioned, only factors specifically described as influencing feedback credibility in the context of a learner-supervisor relationship were included.
CD and KB then extracted and developed themes to represent the findings of the current review until themes were fully agreed upon and all data could be categorized. To synthesize findings, each investigator thematically coded the extracted data from each article and compared results [26]. Any discrepancies were resolved through critical discussion or a third review author. Articles were coded based on feedback characteristics, the context surrounding the feedback, source of feedback, and findings related to the characteristics of feedback recipients. Team meetings were held to resolve discrepancies and consolidate and refine thematic codes.
Results
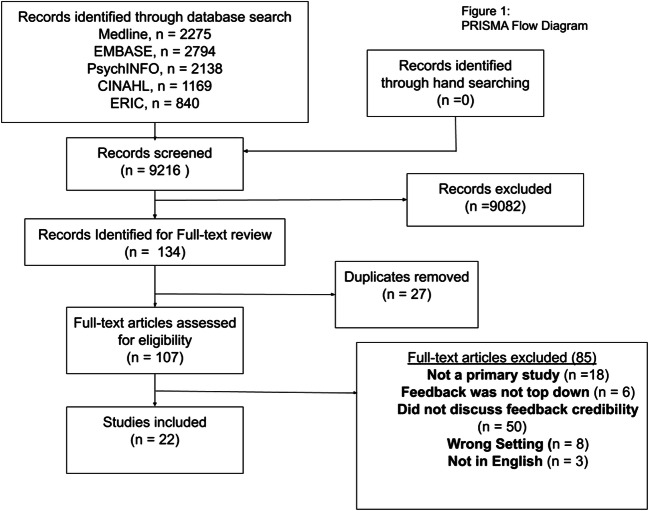
The combined search of electronic databases identified 9216 articles. After initial review and removal of duplicates, 134 abstracts were considered relevant and underwent full-text review (Fig. 1). Of these reviewed articles, 22 met inclusion criteria (Table 2). The studies were heterogenous and most of the included studies utilized a qualitative design using interviews and focus groups (n = 18) and two studies employed mixed methodology. Two studies used a quantitative study design: one used a 2 × 2 factorial design and one analyzed the descriptive statistics of trainees after they rated the credibility of the feedback provider on a 7-point Likert scale.
Fig 1.
PRISMA flow diagram
Table 2.
Summary of results
| Authors and year | Database | Location | Study type | Participants | Influencing factors of credibility |
|---|---|---|---|---|---|
| Duijn et al. (2017) | MEDLINE | Netherlands | Qualitative | Veterinary students; Medical students | • Credible vs trustworthy source who knows the student well |
| • Expertise on subject as well as student’s progress | |||||
| • Relationship over time (length) | |||||
| Ramani, Post et al. (2017) | MEDLINE | USA | Qualitative | Internal medicine residents | • Faculty relationships impact the credibility of feedback |
| • Lack of clear expectations/goal discussions | |||||
| • Direct observation | |||||
| • “Culture of niceness” which lacked the constructive portion of the feedback content | |||||
| Telio et al. (2016) | MEDLINE | Canada | Qualitative | Psychiatry residents | • Trainee judgments of the supervisor’s ability as a clinician (targeted medical knowledge) |
| • Their investment in both the trainees’ identity, and their enthusiasm for teaching. | |||||
| • Perceived feelings of the supervisor towards the learner | |||||
| • Considered supervisor’s motivations in teaching | |||||
| • Engagement in teaching ➔ educational alliance | |||||
| • Lack of trainee interest in receiving feedback - Motivation | |||||
| • Knows about the learner’s personal identity | |||||
| • Learner defensiveness | |||||
| • Education alliance can prompt re-evaluation of FB that was initially met with skepticism overtime | |||||
| Watling et. al (2014) | MEDLINE | Canada | Qualitative |
Physicians; Medical students |
• Longitudinal relationship |
| • Sustained, frequent observation over time | |||||
| • Person has your best intentions at heart | |||||
| • Observing you for long enough | |||||
| • “Oh well, they don’t know me” | |||||
| • Own goals and their teacher were aligned in terms of task | |||||
| • Timeliness—immediacy and during task | |||||
| Manzone et al. (2014) | MEDLINE | Canada | Quantitative | Undergraduate medical students | • Ego-oriented numerical group found FB more credible than task-oriented numerical group |
| Watling et al. (2013) | MEDLINE | Canada | Qualitative |
Undergraduate music students; Medical students; Residents (from a range of specialties); Teacher’s college students |
• Feedback forms supervisors were required to use forced them to comment on aspects of learner performance about which they had insufficient information “obligated to say something when they have nothing to say” |
| • Feedback as a “formality”/mandatory | |||||
| • Feedback cultures shape credibility, i.e., credibility in medical context means clinical skills/expertise | |||||
| • No direct observation of performance decreased credibility ➔ substituting inference for observation | |||||
| Dijksterhuis et al. (2013) | PsychINFO | Netherlands | Qualitative |
Post-graduate trainees in obstetrics and gynecology; Supervisors in obstetrics and gynecology |
• Need for clear standards |
| • Credibility of FB content | |||||
| • Credibility of feedback giver | |||||
| • Direct observation present | |||||
| • The feedback relates to a representative encounter ➔ aligns with self-assessment, trainee must have engaged with task | |||||
| • Supervisor is a role model, well respected, enthusiastic about his chosen specialization, encouraging to trainees | |||||
| Murdoch-Eaton and Sargeant (2012) | MEDLINE | UK | Qualitative and quantitative | Undergraduate medical students | • Maturational differences |
| • Senior students acknowledged the validity of feedback from peers and self-evals. Students in earlier year groups showed a tendency to discount feedback given by anyone other than senior academics | |||||
| • Passive to active learning styles | |||||
| Watling et al. (2012) [10] | MEDLINE | Canada | Qualitative | Faculty members (within 5 years of initial appointment) | • Promotion focus rather than prevention focused (reframing of feedback overtime leads suspicious feedback to become more credible) |
| • Supervisor is respected by peers and learner | |||||
| Watling et al. (2012) [21] | MEDLINE | Canada | Qualitative | Faculty members (within 5 years of initial appointment) | • Credibility of a supervisor facilitates acceptance of feedback |
| • Values not in alignment with learner | |||||
| • Does not align with self-assessment | |||||
| • Learner does not see supervisor as a role model | |||||
| Watling et al. (2008) | MEDLINE | Canada | Qualitative | Residents (from a range of specialties) | • Direct observation |
| • longitudinal relationship | |||||
| • Feedback delivery in person | |||||
| • Specificity ➔ specific example can fail to reflect global performance | |||||
| • Trainees feedback receptivity (motivation/engagement) | |||||
| Stroud et al. (2018) | MEDLINE | Canada | Quantitative | Internal medicine residents | • Expertise/specialty congruency |
| • Gender of supervisor | |||||
| • Gender of trainee—women found feedback more credible overall | |||||
| • Trainee year | |||||
| • No differences in perception of credibility based on how high or low the score was | |||||
| Sargeant et al. (2011) | MEDLINE | UK, USA, Netherlands, and Belgium | Qualitative |
Undergraduate medical students; Post-graduate trainees (specialty not disclosed) |
• Checklist feedback makes it superficial |
| • Objective data lends credibility | |||||
| • Supervisors knowledge about their progress (investment/engagement) | |||||
| Bakke et al. (2020) | MEDLINE | USA | Qualitative | Second-year medical students | • Expertise |
| • Relationship➔ trust and respect | |||||
| • Interest in the individual | |||||
| • Empathetic | |||||
| • Iterative feedback culture | |||||
| • Direct observation over time | |||||
| • Knowledge of student progress | |||||
| Ramani, Konings et al. (2017) | MEDLINE | USA | Qualitative | Internal medicine residents | • Direct observation |
| • Relationship time | |||||
| • Trainee motivation/engagement | |||||
| • Feedback content less emotional and personal | |||||
| • Feedback-seeking attitude | |||||
| Eva et al. (2010) | MEDLINE | Netherlands, Belgium, UK, USA, Canada | Qualitative (data from this study taken from Sargeant (2010)) |
Undergraduate medical students; Post-graduate medical trainees (range of specialties); Midwifery students; Practicing physicians |
• Direct observation enhanced feedback |
| • Strong relationships between learner and teacher | |||||
| • Feedback valence ➔ positive feedback is more credible | |||||
| • Position of beneficence/non- maleficence | |||||
| • Interest in learner | |||||
| • Length/quality of relationship | |||||
| • Learner biased that negative feedback is due to external factors while positive feedback can be attributed to learner | |||||
| Sargeant et al. (2010) | MEDLINE | Netherlands, Belgium, UK, USA, Canada | Qualitative |
Undergraduate medical trainees; Post-graduate medical trainees (range of specialties); Physicians |
• Lack of direct observation |
| • Did not align with self-assessment | |||||
| • No clear standard | |||||
| • “another hoop to jump through” feedback being a chore | |||||
| Moroz et al. (2017) | PsychINFO | USA | Qualitative | Physical medicine and rehabilitation residents | • Motivation affects feedback credibility |
| • Source credibility ➔ positive, long-standing relationship | |||||
| • Culture of the workplace: where feedback has lower priority and is seen as “something to get done” | |||||
| McPhee et al. (2016) | PsychINFO | Australia | Phase 1 quantitative, phase 2 qualitative | Graduated nurses in transition year | • Rostering with many staff across many shifts ➔ learning culture |
| • Checklists devalue feedback | |||||
| • A meeting with the individual for discussion following | |||||
| Poulos and Mahony (2008) | ERIC | Australia | Qualitative | Allied health undergraduate students | • Supervisor biases—diminish credibility of feedback (lack of a clear standard—grades were higher when the students’ held the same viewpoints as the lecturer) |
| • Lecturer’s ability | |||||
| Bing-You and Patterson (1997) | EMBASE | USA | Qualitative | Internal medicine residents | • Not shouting/yelling ➔ intent |
| • Respect for the feedback source | |||||
| • Trust of source | |||||
| • Low level of knowledge or experience | |||||
| • Never observed the learner/did not pay attention | |||||
|
• Feedback given out of obligation is just checking boxes • Seems inattentive towards the learner | |||||
| • They seemed busy, in a hurry, or just going through the motions ➔ interest/culture | |||||
| • Self-assessment does not align with supervisors | |||||
| • Difficulty accepting in a group setting | |||||
| • If it feels like a personal attack/judgmental rather than a critique of performance ➔ intention | |||||
| Fu et al. (2019) | EMBASE | Taiwan | Qualitative | General medicine/internal medicine PGY-1 residents | • Motivation/feedback seeking behavior |
| • Engagement with initial task/importance placed on task | |||||
| • The value that participants placed on feedback—attitude | |||||
| • Initial goals discussion/guidance | |||||
| • Feedback is not specific ➔ “saying something when there’s nothing to say” | |||||
| • Culture of fast rotations and many residents | |||||
| • Timeliness in that delayed FB may call into question the accuracy of events/memory | |||||
| • Repetition of feedback exercise made feedback generic, and redundant |
Populations examined in the literature include allied health undergraduate students (n = 1), undergraduate medical students (n = 8), and resident physicians in internal medicine (n = 5), obstetrics and gynecology (n = 1), and psychiatry (n = 1). Studies were conducted in Canada (n = 10), Australia (n = 2), the Netherlands (n = 5), the USA (n = 7) and the UK (n = 4).
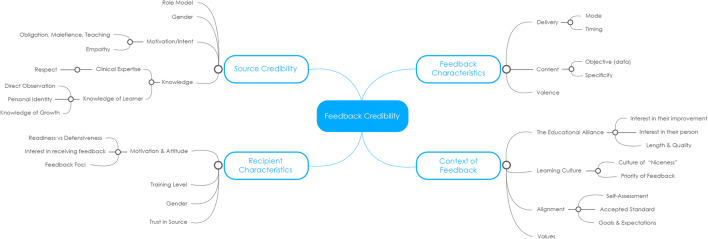
Main themes influencing medical learners’ perceptions of feedback credibility include feedback characteristics, context of feedback, source credibility, and recipient characteristics. Within each theme, a set of sub-themes were identified (Fig. 2) which will be discussed further (Table 3).
Fig 2.
Mind Map Diagram of Themes
Table 3.
Identified themes and sub-themes
| Theme | Sub-theme | Improvements points for the teacher | Improvement points for the learner |
|---|---|---|---|
| Feedback characteristics (9) [15, 27, 29–35] | Delivery | - Delivered individually, and in person. Open a conversation rather than a one-sided delivery | - Ask for feedback during or immediately following tasks |
| - Delivered during or quickly after the task | |||
| Content | - Incorporate objective data | ||
| - Use specific examples that are representative of the learner | |||
| Valence | |||
| Context of feedback (17) [11, 13–15, 21, 27–31, 33–39] | The teacher-learner relationship | - Show interest in the learner’s improvement and person within and outside of the clinical context | |
| Learning culture | - Overcoming a low-priority feedback culture can be difficult, but bidirectional honesty facilitates a stronger educational alliance, leading to more valuable feedback | ||
| Alignment | - Find time to facilitate a goals discussion prior to individual tasks you know you will give feedback for | - Clarify the goals of the task | |
| - Describe what a job well done looks like to you | |||
| Source credibility (20) [10, 11, 13–15, 19, 21, 22, 27, 28, 30–38] | Role model | ||
| Gender | |||
| Motivation and intent | - Feedback given with malicious intent may not only be disregarded but may also be detrimental to the teacher-learner relationship. Feedback that is a personal attack or a projection emotional negativity such as anger, or embarrassment, should be avoided | ||
| - Take formal, mandatory feedback sessions seriously. Show that you have been paying attention and that as a result you have something meaningful to say | |||
| Knowledge and skill | |||
| Personality traits | - Personality traits described as encouraging and empathetic often positively influence the teacher-learner relationship and improve feedback credibility | ||
| Recipient characteristics (12) [10, 13, 14, 17, 22, 27–29, 31, 34–36] | Motivation and attitude | - Seek feedback and work towards an active learning style as opposed to a passive one | |
| Training level | |||
| Gender | |||
| Trust of source | |||
Feedback Characteristics
Nine studies emphasized the importance of feedback characteristics and its influence on feedback credibility [10, 11, 14, 15, 27, 28]. Influencing characteristics of feedback credibility include the delivery, content, and valence of feedback.
Delivery
The mode of delivery as well as timeliness of the delivery affects feedback credibility. When feedback is given in person, individually, it is more credible. The possibility of further discourse about context and details of the feedback lends it credibility [29, 30]. Students described group feedback as generic and less relevant [27]. In terms of timeliness, feedback that is given during the task or soon after is more credible [14, 15]. Timely feedback decreases the possibility and suspicion of memory error, which manifests as generic and vague feedback [31].
Content
Objective, numerical data lends credibility to feedback [32]. However, specificity [29], also a commonly described characteristic of effective feedback [14, 15], does not improve its credibility. In fact, using specific examples may lead the learner to discredit the feedback if the example was not perceived to be representative of the learner’s self-assessment [29]. This may arise when the learner feels they did not truly engage the task, or if they perceived their performance during that task to be an outlier [31, 33]. These concepts are revisited under the recipient characteristic theme.
Valence
Positive feedback was deemed to be generally more credible than negative feedback [34].
Context of Feedback
Seventeen of the 22 studies described context as influencing feedback credibility through 3 main factors: the teacher-learner relationship [14], the learning culture, and the alignment of the feedback.
The Teacher-Learner Relationship
Unsurprisingly, the majority of themes in this review directly affect or are a by-product of the teacher-learner relationship, emphasizing the importance of nurturing and maintaining this relationship.
Described as being an educational alliance by Telio et al. [14], the teacher-learner relationship was alluded to or emphasized in nearly every study. Learners described the length and quality of the relationship to be crucial for feedback to be perceived as credible [14, 15, 28, 34–36]. Learners cited not just a longstanding relationship with the supervisor but also the strength [34] and positive nature [36] of the alliance. Learners described these supervisors as genuinely interested in their improvement and in their person within and outside of the clinical environment [27, 33, 34].
Learning Culture
Articles cited that these relationships tend to be difficult to maintain or establish in the learning culture of medicine, where rotations are short and learners are asked to adapt to a fast turnover of supervisors [30, 31]. The priority of feedback in the learning culture also tempers the credibility of feedback in that the learner may not be aware of its importance, the supervisor may be just “checking the boxes,” or a combination of both [27, 36]. There may also exist a “culture of niceness” where negative feedback is seen to be withheld or subdued out of politeness [11] and so diminishing the credibility of all positive feedback.
Alignment
Feedback that is perceived to be in alignment with the learner’s self-assessment [21, 27, 33, 37], or an accepted standard [33, 37–39] is seen as more credible. This was associated with a lack of knowledge of the learner’s improvement or personal identity, citing that “they don’t know me” [14, 15]. One study found that when students’ objective scores on a task were compared to staff and senior trainee’s scores, the feedback given was more credible than if the students’ scores were shown without the scores of other’s [39], likely because this presented an objective standard for the learner. Having a clear, accepted standard in which feedback could be measured against improved the credibility of the feedback [33, 37, 38]. Prior conversations that align expectations and goals for a task also increase the perceived credibility as this helps create a common goal for the learner to achieve [11, 14, 15, 31, 33]. Another important factor is the alignment of the values of the learner and the supervisor [21] which is associated with source as being a role model and someone who the learner can see themselves wanting to emulate this theme will be further expanded under “Source Credibility.”
Source Credibility
Twenty articles described a characteristic of the feedback giver that affected the feedback credibility. These were gender, motivation/intent, knowledge, certain personality traits, and whether they were role models.
Gender
Male supervisors were generally seen to be more credible than their female counterparts [22].
Role Model
Articles described specialty congruency [22], enthusiasm about their chosen specialty [33], and whether the supervisor was someone who the student aimed to be as an important factor in the credibility of feedback. Students tended to discount feedback, from someone they did not see as a role model even if it was factually accurate [21, 33]. Role models were also described as holding similar values of clinical practice [21], often in a specialty the learner was practicing towards [22].
Knowledge and Skill
Learner’s described the importance of both task-related clinical knowledge [13, 14, 19, 22, 27, 28, 38], and knowledge of the learner [14, 15, 28]. In medical culture, clinical knowledge was associated with respect for the feedback giver [10, 13, 27, 33], which in turn was an important factor that boosted the credibility of the feedback. Knowledge of the learner was further broken down into knowledge of the learner as a person [14, 15], knowledge of their growth as a student [13, 28, 32], and whether or not there was direct observation of the learner’s performance [11, 13–15, 19, 27, 29, 33–35, 37], with many students discounting feedback that came from inference rather than direct observation.
Motivation and Intent
The perception of beneficence and non-maleficence created trust in the educational alliance [34]. The perceived motivation and intentions behind the feedback greatly affect its credibility [14, 15, 27, 31, 33, 34, 36, 37]. Learners thought that feedback with the intention of completing a checklist as less credible than intentions to teach or help the learner [19, 27, 31, 36, 37], describing obligatory, redundant feedback sessions as “something to get done”[36] and “saying something when there’s nothing to say” [31]. The perception of maleficence was noted when the feedback giver would shout or yell, signaling a judgmental attitude or intent of harm [27]. This may be perceived as a personal attack rather than constructive criticism.
Personality Traits
Supervisors who were seen as empathetic and encouraging were cited as being more credible. These supervisors and learners were often in a stronger educational alliance, but the directionality of this correlation is unclear [13, 33].
Recipient Characteristics
Twelve studies showed that recipient characteristics including gender, trust of source, level of training, motivation, and attitude affected the degree in which feedback was taken to be credible.
Motivation and Attitude
Learners who had a feedback-seeking attitude and a more active learning approach found feedback more credible [29, 31, 35, 36]. Alex Moroz et al. [36] found that residents motivated within integrated regulation (external values and goals are integrated into the learner’s self-image and habits as opposed to external regulation in which actions are motivated by anticipated consequences) focused on seeking, accepting, and trusting feedback. Learners who had a defensive mindset towards feedback were more likely to attribute poor performance and negative feedback as a result of external factors such while attributing positive feedback oneself. Watling et al. [10] described how a change in regulatory focus can change initially discredited feedback into credible feedback with time. For example, a learner who had expected praise for his work (promotional focus) was met with constructive criticism, and although he initially felt this to be a “waste of time,” he eventually came to see value in fixing his minor errors (prevention focus), thus lending credibility to the previously discredited feedback.
Level of Training
Studies found that medical residents at higher levels of training tended to find feedback from supervisors less credible than those at lower levels of training as they gain the ability to discern skill and style [22]. Another article found that junior learners would often find only the feedback from senior staff to be credible [17].
Gender
Female learners found feedback to be more credible overall compared to their male counterparts [22].
Trust of Source
Three studies described the importance of perceiving the feedback giver as trustworthy [13, 14, 28]. Although trust and respect were often cited together, respect in medical education was often described in relation to clinical knowledge whereas trust was described as a consequence of the teacher-learner relationship [13].
Discussion
This review examined the available evidence concerning the credibility of feedback provided from supervisor to learner within health professional education settings. While previous reviews have looked at factors contributing to the effectiveness of various types of feedback [40], at the time of writing, no review has explored the factors that make feedback credible to its recipients in a medical education setting.
The four main themes identified (feedback characteristics, context of feedback, source credibility, and recipient characteristics) were presented individually. However, factors presented within these categories can also be viewed as interrelated and the association between these factors and feedback may be driven more by culture than each characteristic independently. Watling et al. [19] state that “professions define credibility and constructiveness in culturally specific ways and create contexts for learning that may either facilitate or constrain the provision of meaningful feedback” [19]. The four themes provide an immediate conduit for the improvement of feedback and feedback culture within medical education. Although it is not easy to change personal characteristics of feedback providers and recipients such as personality or gender, an understanding of feedback receptivity can influence feedback credibility and help educators provide effective feedback for learner self-reflection and growth.
It is often assumed that learners perceive all feedback as credible, and that once feedback has been given, it is the responsibility of the learner to act. However, as identified in this study, several factors influence how learners weigh the credibility of feedback they receive. Feedback providers would benefit from recognizing the recipient’s identity as a learner, particularly where career aspiration may not be related to the educator’s discipline.
While each medical specialty may have its own feedback culture and processes of providing feedback, the results show that an effort to nurture the relationship between the provider and the recipient is crucial. Acting on feedback is an individual activity and when supervisors have or attempt to have an awareness of the goals of the learner, specialty interest, and other recipient factors, feedback is more relevant and meaningful and transcends cultural and specialty differences. Setting expectations before a task and assessing how the learner feels he or she performed after the task can be useful information for formulating feedback. This ensures that the learner completes the task with the same goals as the assessor and that the feedback given after does not differ immensely from the learner’s self-assessment.
The language of feedback is often “us” vs “them” and a strong relationship breaks down this divide and seemingly changes feedback from a battleground to a conversation where the supervisor and the learner are aligned in their intention for growth and improvement [41]. We are discovering that the most effective feedback comes from discourse and not simply one-way communication of information [42]. This sentiment further highlights the importance of the educational alliance. This alignment in focus [10] may be reflected in an alignment in expectation and goals that can improve feedback credibility.
In addition to a strong teacher-learner relationship, direct observation of the entire task is more likely to be perceived by the learner as based on the facts of the observation rather than inferred from another’s. Perspective taking, direct observation, and timing of feedback are key components central to the credibility of feedback and enhance trainee development [14]. Similarly, feedback created from viewing only the result can be perceived as inferring the procession of the task which could understandably decrease the credibility of the feedback. The findings in this review suggest that direct observation was not only desirable by trainees but also necessary for feedback to be appreciated [21, 27, 33].
Limitations
Although this review followed a comprehensive and rigorous review methodology, there a few limitations worth noting. Many studies were limited to one institution in one country with small sample sizes. Studies included also used a variety of questionnaires and data collection tools and so it was impossible to perform a meta-analysis. As well, we were limited to studies in English or translated into English, and so we cannot discount the possibility that some data points were lost or inappropriately included. Some studies were cross-sectional in design which limited our longitudinal insights.
Conclusion
Feedback delivery is vital to undergraduate and post-graduate medical education [7–9]. As the medical culture normalizes an emphasis on feedback, there exists an increased duty for educators to be able to provide meaningful feedback to guide learners. As programs implement major educational change initiatives to create more formative assessment practices, feedback will become more crucial. This paper provides clear factors expressed in the literature that can help shape the feedback process [43]. Further research that builds on this review can promote ideas of lifelong learning and self-development which are fundamental to the growth of health professionals.
Supplementary Information
(DOCX 15 kb)
(DOCX 30 kb)
(DOCX 17 kb)
(DOCX 59 kb)
(DOCX 27 kb)
(DOCX 14 kb)
Authors’ Contributions
CD and SC conceived and planned the study. CD and KB performed the data collection and analysis, and wrote the manuscript. SC supervised the project.
Data Availability
Data available upon request
Compliance with Ethical Standards
Conflict of Interest
The authors declare that there are no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nicol DJ, Macfarlane-Dick D. Formative assessment and self-regulated learning: a model and seven principles of good feedback practice. Stud High Educ. 2006;31(2):199–218. doi: 10.1080/03075070600572090. [DOI] [Google Scholar]
- 2.Ende J. Feedback in clinical medical education. JAMA. 1983;250(6):777–781. doi: 10.1001/jama.1983.03340060055026. [DOI] [PubMed] [Google Scholar]
- 3.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705. doi: 10.1001/jama.1995.03530090032018. [DOI] [PubMed] [Google Scholar]
- 4.Epstein RM. Assessment in medical education. N Engl J Med. 2007;356(4):387–396. doi: 10.1056/NEJMra054784. [DOI] [PubMed] [Google Scholar]
- 5.Paterson C, Paterson N, Jackson W, Work F. What are students’ needs and preferences for academic feedback in higher education? A systematic review. Nurse Educ Today. 2020;85:104236. doi: 10.1016/j.nedt.2019.104236. [DOI] [PubMed] [Google Scholar]
- 6.Van de Ridder JMM, Stokking KM, McGaghie WC, ten Cate OTJ. What is feedback in clinical education? Med Educ. 2008;42(2):189–197. doi: 10.1111/j.1365-2923.2007.02973.x. [DOI] [PubMed] [Google Scholar]
- 7.Norcini J. The power of feedback. Med Educ. 2010;44(1):16–17. doi: 10.1111/j.1365-2923.2009.03542.x. [DOI] [PubMed] [Google Scholar]
- 8.Hattie J, Timperley H. The power of feedback. Rev Educ Res. 2007;77(1):81–112. doi: 10.3102/003465430298487. [DOI] [Google Scholar]
- 9.Veloski J, Boex JR, Grasberger MJ, Evans A, Wolfson DB. Systematic review of the literature on assessment, feedback and physicians’ clinical performance: BEME Guide No. 7. Med Teach. 2006;28(2):117–128. doi: 10.1080/01421590600622665. [DOI] [PubMed] [Google Scholar]
- 10.Watling C, Driessen E, van der Vleuten C, et al. Understanding responses to feedback: the potential and limitations of regulatory focus theory. Med Educ. 2012;46(6):593–603. doi: 10.1111/j.1365-2923.2012.04209.x. [DOI] [PubMed] [Google Scholar]
- 11.Ramani S, Post SE, Konings K, Mann K, Katz JT, van der Vleuten C. “It’s just not the culture”: a qualitative study exploring residents’ perceptions of the impact of institutional culture on feedback. Teach Learn Med. 2017;29(2):153–161. doi: 10.1080/10401334.2016.1244014. [DOI] [PubMed] [Google Scholar]
- 12.Sender-Liberman A, Liberman M, Steinert Y, McLeod P, Meterissian S. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005;27(5):470–472. doi: 10.1080/0142590500129183. [DOI] [PubMed] [Google Scholar]
- 13.Bakke BM, Sheu L, Hauer KE. Fostering a feedback mindset: a qualitative exploration of medical students’ feedback experiences with longitudinal coaches. Academic Medicine. 2019;95(7):1057–1065. doi: 10.1097/acm.0000000000003012. [DOI] [PubMed] [Google Scholar]
- 14.Telio S, Regehr G, Ajjawi R. Feedback and the educational alliance: examining credibility judgements and their consequences. Med Educ. 2016;50(9):933–942. doi: 10.1111/medu.13063. [DOI] [PubMed] [Google Scholar]
- 15.Watling C, Driessen E, Vleuten CPM, Lingard L. Learning culture and feedback: an international study of medical athletes and musicians. Med Educ. 2014;48(7):713–723. doi: 10.1111/medu.12407. [DOI] [PubMed] [Google Scholar]
- 16.Weaver MR. Do students value feedback? Student perceptions of tutors’ written responses. Assess Eval High Educ. 2006;31(3):379–394. doi: 10.1080/02602930500353061. [DOI] [Google Scholar]
- 17.Murdoch-Eaton D, Sargeant J. Maturational differences in undergraduate medical students’ perceptions about feedback. Med Educ. 2012;46(7):711–721. doi: 10.1111/j.1365-2923.2012.04291.x. [DOI] [PubMed] [Google Scholar]
- 18.Lefroy J, Watling C, Teunissen PW, Brand P. Guidelines: the do’s, don’ts and don’t knows of feedback for clinical education. Perspect Med Educ. 2015;4(6):284–299. doi: 10.1007/s40037-015-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watling C, Driessen E, Vleuten CPM, Vanstone M, Lingard L. Beyond individualism: professional culture and its influence on feedback. Med Educ. 2013;47(6):585–594. doi: 10.1111/medu.12150. [DOI] [PubMed] [Google Scholar]
- 20.Sargeant J, Mann K, Sinclair D, Van der Vleuten C, Metsemakers J. Understanding the influence of emotions and reflection upon multi-source feedback acceptance and use. Adv Health Sci Educ Theory Pract. 2008;13(3):275–288. doi: 10.1007/s10459-006-9039-x. [DOI] [PubMed] [Google Scholar]
- 21.Watling C, Driessen E, van der Vleuten CPM, Lingard L. Learning from clinical work: the roles of learning cues and credibility judgements. Med Educ. 2012;46(2):192–200. doi: 10.1111/j.1365-2923.2011.04126.x. [DOI] [PubMed] [Google Scholar]
- 22.Stroud L, Sibbald M, Richardson D, McDonald-Blumer H, Cavalcanti R. Feedback credibility in a formative postgraduate objective structured clinical examination: effects of examiner type. J Grad Med Educ. 10.4300/JGME-D-17-00578.1 Published 2020. Accessed Oct 31, 2020. [DOI] [PMC free article] [PubMed]
- 23.Archer J. State of the science in health professional education: effective feedback. [DOI] [PubMed]
- 24.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 27.Bing-You R, Paterson J. Feedback falling on deaf ears: residents’ receptivity to feedback tempered by sender credibility. Med Teach. 1997;19(1):40. doi: 10.3109/01421599709019346. [DOI] [Google Scholar]
- 28.Duijn CCMA, Welink LS, Mandoki M, ten Cate OTJ, Kremer WDJ, Bok HGJ. Am I ready for it? Students’ perceptions of meaningful feedback on entrustable professional activities. Perspect Med Educ. 2017;6(4):256–264. doi: 10.1007/s40037-017-0361-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Watling CJ, Kenyon CF, Zibrowski EM, Schulz V, Goldszmidt MA, Singh I, Maddocks HL, Lingard L. Rules of engagement: residents’ perceptions of the in-training evaluation process. Acad Med. 2008;83(10 Suppl):S97–100. doi: 10.1097/ACM.0b013e318183e78c. [DOI] [PubMed] [Google Scholar]
- 30.McPhee S, Phillips NM, Ockerby C, Hutchinson AM. Multisource feedback to graduate nurses: a multimethod study. J Clin Nurs. 2017;26(21-22):3442–3456. doi: 10.1111/jocn.13710. [DOI] [PubMed] [Google Scholar]
- 31.Fu RH, Cho YH, Quattri F, Monrouxe LV. ‘I did not check if the teacher gave feedback’: a qualitative analysis of Taiwanese postgraduate year 1 trainees’ talk around e-portfolio feedback-seeking behaviours. BMJ Open. 2019;9(1):e024425. doi: 10.1136/bmjopen-2018-024425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sargeant J, Eva KW, Armson H, Chesluk B, Dornan T, Holmboe E, Lockyer JM, Loney E, Mann KV, van der Vleuten CP. Features of assessment learners use to make informed self-assessments of clinical performance. Med Educ. 2011;45(6):636–647. doi: 10.1111/j.1365-2923.2010.03888.x. [DOI] [PubMed] [Google Scholar]
- 33.Dijksterhuis MGK, Schuwirth LWT, Braat DDM, Teunissen PW, Scheele F. A qualitative study on trainees’ and supervisors’ perceptions of assessment for learning in postgraduate medical education. Med Teach. 2013;35(8). 10.3109/0142159X.2012.756576. [DOI] [PubMed]
- 34.Eva KW, Armson H, Holmboe E, Lockyer J, Loney E, Mann K, Sargeant J. Factors influencing responsiveness to feedback: on the interplay between fear, confidence, and reasoning processes. Adv Health Sci Educ Theory Pract. 2012;17(1):15–26. doi: 10.1007/s10459-011-9290-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramani S, Könings K, Mann KV, van der Vleuten C. Uncovering the unknown: a grounded theory study exploring the impact of self-awareness on the culture of feedback in residency education. Med Teach. 2017;39(10):1065–1073. doi: 10.1080/0142159X.2017.1353071. [DOI] [PubMed] [Google Scholar]
- 36.Moroz A, Horlick M, Mandalaywala N, Stern DT. Faculty feedback that begins with resident self-assessment: motivation is the key to success. Med Educ. 2018;52(3):314–323. doi: 10.1111/medu.13484. [DOI] [PubMed] [Google Scholar]
- 37.Sargeant J, Armson H, Chesluk B, Dornan T, Eva K, Holmboe E, et al. The processes and dimensions of informed self-assessment: a conceptual model. Academic Medicine. 2010;85(7):1212–1220. doi: 10.1097/acm.0b013e3181d85a4e. [DOI] [PubMed] [Google Scholar]
- 38.Poulos A, Mahony MJ. Effectiveness of feedback: the students’ perspective. Assess Eval High Educ. 2008;33(2):143–154. doi: 10.1080/02602930601127869. [DOI] [Google Scholar]
- 39.Manzone J, Tremblay L, You-Ten KE, et al. Task-versus ego-oriented feedback delivered as numbers or comments during intubation training. Med Educ. 2014;48(4):430–440. doi: 10.1111/medu.12397. [DOI] [PubMed] [Google Scholar]
- 40.Ferguson J, Wakeling J, Bowie P. Factors influencing the effectiveness of multisource feedback in improving the professional practice of medical doctors: a systematic review. BMC Med Educ. 2014;14:76. doi: 10.1186/1472-6920-14-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Urquhart LM, Rees CE, Ker JS. Making sense of feedback experiences: a multi-school study of medical students’ narratives. Med Educ. 2014;48(2):189–203. doi: 10.1111/medu.12304. [DOI] [PubMed] [Google Scholar]
- 42.Lizzio A, Wilson K, MacKay L. Managers’ and subordinates’ evaluations of feedback strategies: the critical contribution of voice1. Journal of Applied Social Psychology. 2008;38:919–946. doi: 10.1111/j.1559-1816.2008.00332.x. [DOI] [Google Scholar]
- 43.Lockyer J, Carraccio C, Chan M-K, Hart D, Smee S, Touchie C, Holmboe ES, Frank JR, on behalf of the ICBME Collaborators Core principles of assessment in competency-based medical education. Med Teach. 2017;39(6):609–616. doi: 10.1080/0142159X.2017.1315082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15 kb)
(DOCX 30 kb)
(DOCX 17 kb)
(DOCX 59 kb)
(DOCX 27 kb)
(DOCX 14 kb)
Data Availability Statement
Data available upon request