Abstract
Introduction
It is broadly agreed that physicians must be self-directed learners, and many studies measuring medical student readiness and capacity for self-directed learning (SDL) have been reported. However, less attention has been paid to faculty tasked with guiding students to develop SDL skills. In an effort to determine whether faculty feel equipped to foster SDL, a needs assessment was developed.
Methods
The faculty needs assessment for fostering SDL (FNA-fSDL) was constructed and distributed nationally to medical educators. Faculty perceptions of the value of SDL, administration support, and faculty development were queried. Items also measured faculty recognition of cognitive, affective, and metacognitive strategies shown to cultivate SDL. Descriptive statistical analysis and frequency comparison tests to identify potential group differences related to work responsibility, classroom/clinical setting, and level of learner served were performed.
Results
Among the 359 respondents representing diverse areas of medical education, there was overwhelming agreement that physicians in training should be self-directed learners and that faculty require training in educational approaches promoting SDL. Faculty were more likely to recognize strategies supporting development of metacognitive skills and least likely to identify those related to cognitive aspects of learning. Fewer than half of faculty had received training in fostering SDL at their home institutions or at conferences.
Discussion
While there is strong support for the development of SDL among learners, these results suggest most faculty do not feel sufficiently trained to accomplish this goal. The FNA-fSDL can be used by institutions to assess their own faculty.
Keywords: Self-directed learning, Faculty development, Learning-oriented teaching
Introduction
Within an ever-changing healthcare landscape, it is essential that physicians meet their societal obligation to maintain and advance knowledge and skills throughout their professional lives [1]. Successful clinicians are self-motivated and able to identify knowledge gaps, create learning goals, and take responsibility for them, as well as assess self-efficacy in accomplishing their learning needs. In other words, physicians must be capable of self-directed learning (SDL) as first defined by Knowles [2]. The importance of SDL is recognized in undergraduate medical education (UME) and graduate medical education (GME) as articulated in required elements outlined by the Liaison Commission on Medical Education (LCME) [3] and the Accreditation Council for Graduate Medical Education (ACGME) [4], respectively. It is therefore not surprising that medical education literature is replete with studies focusing on learner readiness [5, 6] and capacity for SDL [7–9].
Educational programs intentionally designed to promote SDL involve the deliberate incorporation of approaches to help students develop self-regulated learning (SRL) skills [10]. Whereas SDL is an overall approach to learning, SRL describes specific activities the learner uses in a cycle of planning, execution, and evaluation [11]. There is a broad literature describing specific educational strategies adopted by primary and secondary school educators to help equip learners to become self-directed learners [12–15]. These strategies are also described in higher education literature [16, 17] and are often termed process-oriented instruction. Process-oriented instruction aims to integrate content-specific knowledge with explicit thinking and learning strategies [18] thereby providing teachers with tangible skills and instructional approaches they can use to help students develop self-regulation with the goal of improving academic performance [19, 20] and fostering lifelong SDL [21]. In 2004, ten Cate partnered with Vermunt and colleagues to propose medical educators adopt learning-oriented teaching, a model similar to process-oriented teaching [22].
Learning-oriented teaching strategies fall into three domains: (1) cognitive: building content knowledge/cognitive development, (2) affective: emotional and motivational support, and (3) metacognitive development [22]. In building cognition, the goal of the instructor is to make knowledge more accessible to learners not only by presenting and clarifying information but also by coaching learners in the analysis and application of information and skills. Emotional and motivational elements of teaching recognize that learning can be demanding and uncomfortable. Strategies that communicate that learning is nonetheless worthwhile, for example, modeling and actionable feedback can help learners develop SRL skills. In supporting the acquisition of metacognitive skills, instructors apply strategies that demonstrate how to plan study activities, evaluate study skills, and assess progress.
To date, there has been limited information about the degree to which medical educators as a community promote SDL by providing students with SRL strategies. Therefore, the goal of the present study was to survey medical educators at the national level to gain understanding of community perception of the value of SDL for their learners, to gauge the support faculty discern from their administration, and assess exposure to faculty development in promoting SDL. To evaluate familiarity with learning approaches that promote SRL, we measured the ability of faculty to recognize educational strategies reported to promote the development of self-regulated learning. Additionally, a portion of the survey was distributed to students to gauge their recognition of and experience with these educational strategies. Finally, we examined whether faculty teaching responsibility, principle educational setting (e.g., classroom, clinic), and level of medical student taught influenced teachers’ promotion of SDL and use of SDL strategies. In this way, this work begins to address the question of faculty perception of SDL while assessing the need for faculty development to improve delivery of medical education curricula that promotes its development.
Materials and Methods
Participants
The target audience for the survey was medical educators providing instruction to undergraduate medical students. The online survey described below was sent in June 2019 via e-mail to members of a listserv developed to include one individual (i.e., associate dean, preclinical director, or program director) identified as being knowledgeable about their curriculum at each of 155 accredited U.S. medical schools. Additional invitations were sent to members of the International Association of Medical Science Educators Listserv, DR-ED Listserv, and program directors from 1004 ACGME accredited residency programs. A portion of the survey was also distributed to all Zucker School of Medicine at Hofstra/Northwell (Zucker SOM) students (n = 361).
Survey
The survey was developed in three stages. First, 10 educators (both preclinical and clinical instructors; MDs, DOs, and PhDs) from the Zucker SOM and 10 from the Geisel School of Medicine at Dartmouth (Geisel SOM) were asked to complete a small-scale survey and provide both written and verbal feedback. In the second phase of development, a revised pilot survey was distributed to 925 Zucker SOM faculty who were not involved in earlier instrument development. The survey was accessible as an anonymous Qualtrics (Provo, UT) survey link. These included clinical, research, and full-time education faculty across UME and GME. The response rate for this phase of instrument development was 15.6% (n = 145). The next, final version of the survey excluded Zucker SOM faculty.
Responses to the pilot study informed the development of the final survey, which was developed based upon the learning-oriented teaching model of ten Cate et al. [22]. It consisted of five sections. (1) The first gathered the demographic data summarized in Table 1. (2) The next section presented a list benefits of SDL reported in the literature (Fig. 1) [7, 23]. Respondents were asked to select all items they perceived to be valuable (a binary choice of yes/no). (3) The following section included a series of questions designed to discern whether faculty felt supported by their administration and if they were receptive to faculty development in techniques to promote SDL (Fig. 2). (4) Next, respondents were queried about how such faculty development has been, or might best be, delivered (Fig. 3). Responses in both sections three and four were anchored in a Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). (5) The last section listed 18 different teaching/curricular strategies that have been documented as a means to promote self-regulated or self-directed learning [12, 13, 20]. Respondents were asked to identify whether strategies might promote SDL by indicating “yes,” “no,” or “unsure.” The term SDL rather than SRL was used to avoid confusion as it is unclear if the difference between SDL and SRL is widely understood [11]. Each strategy belonged to one of the three domains described by ten Cate [22]: (1) cognitive, (2) affective, or (3) metacognitive, with six strategies per domain (Table 2). Domains were not labeled on the survey to avoid influencing responses. This section of the survey was also sent to students at Zucker School of Medicine, where a curriculum that stresses self-directed learning is practiced [24]. Students were prompted to indicate if they thought each strategy promoted SDL (yes/no). Students were also asked if they could recall experiencing the use of each strategy during their medical education.
Table 1.
Demographic distribution of respondents. Number (%) of responses to each demographic category
| Demographic categories | BA/BS (n = 1) | MS/MA (n = 13) | *MD/DO, or MBBS (n = 107) | *Ph.D. or EdD (n = 155) | MD/Ph.D. (n = 59) | |
|---|---|---|---|---|---|---|
| Age (n = 335) | 25–35 | 0 | 1 (0.3) | 7 (2.1) | 7 (2.1) | 5 (1.5) |
| 36–45 | 0 | 5 (1.5) | 35 (10.4) | 40 (11.9) | 19 (5.7) | |
| 46–55 | 1 (0.3) | 2 (0.6) | 29 (8.7) | 32 (9.6) | 13 (3.9) | |
| 56–65 | 0 | 5 (1.5) | 28 (8.4) | 52 (15.5) | 14 (4.2) | |
| 66–75 | 0 | 0 | 6 (1.8) | 13 (3.9) | 7 (2.1) | |
| 75 < | 0 | 0 | 2 (0.6) | 11 (3.9) | 1 (0.3) | |
| Gender (n = 335) | Male | 1 (0.3) | 4 (1.2) | 42 (12.5) | 63 (18.8) | 34 (10.1) |
| Female | 0 | 8 (2.4) | 65 (19.4) | 91 (27.2) | 24 (7.2) | |
| Others | 0 | 1 (0.3) | 0 | 1 (0.3) | 1 (0.3) | |
| Responsibility (n = 335) | Education | 1 (0.3) | 7 (2.1) | 60 (17.9) | 115 (34.3) | 38(11.3) |
| Clinical | 0 | 0 | 32 (9.6) | 0 | 13 (3.9) | |
| Research | 0 | 0 | 2 (0.6) | 6 (1.8) | 3 (0.9) | |
| Admin | 0 | 4 (1.2) | 10 (3.0) | 26 (7.8) | 4 (1.2) | |
| Others | 0 | 2 (0.6) | 3 (0.9) | 8 (2.4) | 1 (0.3) | |
| Teaching type (n = 324) | One to one | 1 (0.3) | 4 (1.2) | 90 (27.8) | 76 (23.5) | 33 (10.2) |
| Small group | 1 (0.3) | 7 (2.2) | 103 (31.8) | 130 (40.1) | 48 (14.8) | |
| Lecture | 1 (0.3) | 4 (1.2) | 85 (26.2) | 125 (38.6) | 40 (12.3) | |
| Faculty rank (n = 317) | Instructor | 0 | 4 (1.3) | 2 (0.6) | 4 (1.3) | 1 (0.3) |
| Assistant prof | 1 (0.3) | 1 (0.3) | 33 (10.4) | 41 (12.9) | 20 (6.3) | |
| Associate prof | 0 | 0 | 46 (14.5) | 47 (14.8) | 19 (6.0) | |
| Prof | 0 | 0 | 24 (7.6) | 55 (17.4) | 19 (6.0) | |
| Interaction with students (n = 331) | Years 1 and 2 | 1 (0.3) | 5 (1.5) | 21 (6.3) | 130 (39.3) | 25 (7.6) |
| Years 3 and 4 | 0 | 1 (0.3) | 50 (15.1) | 6 (1.8) | 16 (4.8) | |
| All 4 years | 0 | 6 (1.8) | 37 (11.2) | 15 (4.5) | 18 (5.4) | |
| Experience (n = 336) | 1–5 years | 1 (0.3) | 7 (2.1) | 12 (3.6) | 23 (6.8) | 8 (2.4) |
| 6–10 years | 0 | 4 (1.2) | 26 (7.7) | 36 (10.7) | 11 (3.3) | |
| 11–15 years | 0 | 1 (0.3) | 25 (7.4) | 17 (5.1) | 7 (2.1) | |
| <16 years | 0 | 1 (0.3) | 45 (13.4) | 79 (23.5) | 33 (9.8) | |
*For MD/DO or MBBS vs. Ph.D. or EdD comparison tests, those groups were included.
Fig. 1.
Perceived benefits of self-directed learning (n = 339)
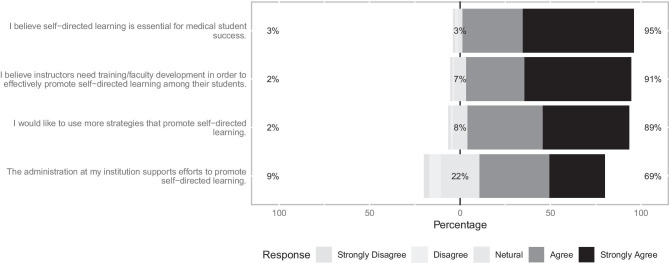
Fig. 2.
Perception of support for faculty development
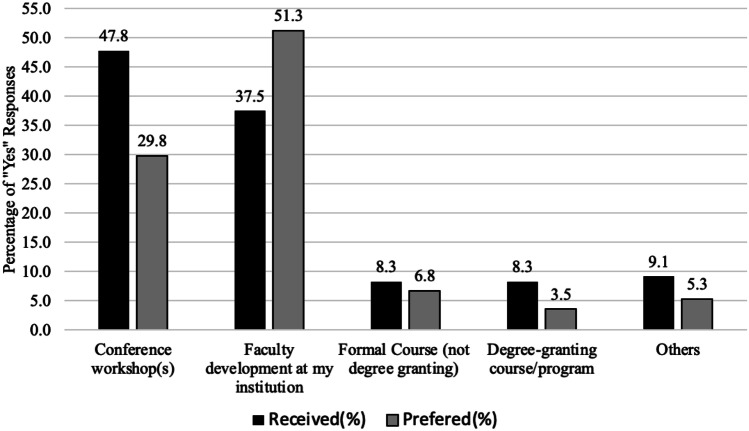
Fig. 3.
Survey of formats of faculty development (N = 339)
Table 2.
Percentage of recognition of SDL strategies
| Instructional l domain | Faculty (N = 339) | Students (N = 77) | |||
|---|---|---|---|---|---|
| Promote SDL | Do not know | Not promote SDL | Promote SDL | Experienced | |
| Building content knowledge/cognitive | |||||
| Explaining relationships between new and old concepts | 28.1 | 44.7 | 21.3 | 46.4 | 58.9 |
| Providing analogies between new topics or concepts and familiar, everyday topics or concepts | 36.0 | 39.9 | 18.5 | 44.6 | 52.7 |
| Asking students to compare and contrast information | 67.1 | 17.4 | 9.6 | 50.9 | 53.6 |
| Step-by-step explanations of complex skill processes (e.g., performing an abdominal exam)* | 12.6 | 68.8 | 12.9 | 26.8 | 58.0 |
| Asking students questions that require critical thinking | 74.4 | 11.8 | 7.6 | 54.5 | 60.7 |
| Asking students to apply a concept to a new or similar situation | 72.8 | 13.5 | 8.1 | 51.8 | 53.6 |
| Mean | 48.6 | 32.7 | 13.0 | 45.8 | 56.3 |
| SD | 26.3 | 22.5 | 5.7 | 10.0 | 3.4 |
| Emotional and motivational/affective | |||||
| Giving students specific feedback about their understanding of content | 55.9 | 21.6 | 16.6 | 46.4 | 49.1 |
| Giving students specific feedback about their clinical skills performance | 51.1 | 23.3 | 19.9 | 42.0 | 57.1 |
| Providing time during the day without curricular activities for students to learn conceptual content on their own | 76.4 | 4.5 | 13.5 | 56.3 | 53.6 |
| Providing time during the day without curricular activities for students to consolidate conceptual content on their own | 71.6 | 7.0 | 15.4 | 57.1 | 45.5 |
| Encouraging students to set learning goals | 85.4 | 3.7 | 5.3 | 50.0 | 47.3 |
| Demonstrating how course material is relevant to medicine | 29.8 | 43.8 | 20.2 | 43.8 | 50.9 |
| Mean | 61.7 | 17.3 | 15.2 | 49.3 | 50.6 |
| SD | 20.2 | 15.6 | 5.5 | 6.4 | 4.3 |
| Promoting student regulation of learning/metacognition | |||||
| Directing students to specific resources* | 41.3 | 33.7 | 19.1 | 38.4 | 52.7 |
| Discussing study skills with students who seek extra help with content | 65.7 | 15.2 | 13.2 | 47.3 | 34.8 |
| Eliciting student self-evaluation of understanding of content | 75.6 | 7.3 | 11.0 | 45.5 | 46.4 |
| Eliciting student self-evaluation of skill performance | 71.3 | 8.7 | 13.8 | 43.8 | 50.9 |
| Facilitating student self-evaluation of their learning process and study strategies | 77.8 | 4.5 | 11.5 | 43.8 | 44.6 |
| Encouraging students to evaluate and utilize their prior knowledge | 74.2 | 8.4 | 10.4 | 50.9 | 49.1 |
| Mean | 64.0 | 13.0 | 13.2 | 45.0 | 46.4 |
| SD | 13.6 | 10.7 | 3.2 | 4.2 | 6.4 |
*Negatively scored
Data Analysis
Percentages for all individual questions and average percentage (with SD) for individual instructional domains were calculated. We conducted separate chi-square analyses on the 18 educational strategies to determine if faculty work responsibility (education, clinical, research, administration), classroom setting (one-to-one instruction, small group, lecture), and level of student most frequently taught (medical school students in years 1 and 2, years 3 and 4, or throughout all 4 years) impacted responses. Finally, we conducted chi-square analyses on all questions by faculty’s demographic categories listed in Table 1 to test possible group differences. Only statistically significant differences are reported in this study.
Results
A total of 339 faculty responses were collected through national electronic distribution across 155 LCME accredited medical schools and 1004 ACGME accredited residency programs. This would yield a response rate of 29% if one individual at each institution or program responded. However, the uncertainty regarding number of respondents per institution combined with the indeterminate number of respondents contacted via listservs makes it impossible to calculate the exact response rate. The majority of respondents possessed terminal degrees: MD/DO/MBBS (107; 30.0%), Ph.D. (155; 43.5%) degrees, or MD/Ph.D. (59; 16.6%), (Table 1). About two-thirds (221; 62.1%) cited education as their primary responsibility with a fairly even distribution across faculty rank from assistant to full professor. Respondents were asked to identify the educational level of student for whom they were primarily responsible. The majority (330, 97%) of respondents taught medical students, although not necessarily exclusively at the UME level. Slightly more than half reported teaching in years 1 and 2 (183; 54.0%), followed by throughout 4 years (77; 27.7%) and years 3 and 4 (73; 21.5%). Only three respondents did not teach at the UME level. Those with a Ph.D. were more likely to instruct students in the first and second years of medical school while clinicians more frequently interacted with third and fourth year students as well as students throughout the 4-year educational continuum. Respondents frequently taught in small group (289; 85.3%) and large lecture (256; 75.5%) settings. The response rate from students was 31% (112 responses).
Faculty overwhelming reported that SDL is essential for medical student success (320; 94.4%: Fig. 2). Slightly more MDs (106; 99.1%) than Ph.D.s (141; 91.0%, P = 0.01) believed this to be the case. Faculty perceived SDL to be beneficial to their learners for a variety of reasons (Fig. 1). The vast majority (331; 97.6%) indicated that they believe SDL fosters life-long learning skills. At least three-quarters of respondents identified the following as benefits of SDL: promoting self-reflection about learning (292; 86.1%), increasing learner curiosity (281; 82.9%), fostering internal motivation (279; 82.3%), better physician preparation (276; 81.4%), and promoting goal setting by learners (268; 79.1%). A plurality of respondents felt that SDL encourages students to be prepared for class activities (208; 61.4%), facilitates team and peer teaching skills (193; 56.9%), and prepares learners for clinical responsibilities (189; 55.8%). Those items only a minority of respondents believed were linked to SDL were its capacity to improve academic performance (170; 50.1%) and to improve learners’ communication skills (118; 34.8%).
The positive view most faculty have with regard to SDL was evident with 89% (n = 302) of respondents indicating that they would like to use more instructional strategies to promote their students’ SDL (Fig. 2). Ninety-one percent (n = 308) of respondents believed, “instructors need training in order to effectively promote self-directed learning among their students.” Such training typically requires institutional support and although about two-thirds (69.0%, n = 234) of faculty respondents reported their administration supports efforts to promote SDL (Fig. 2), only about a third (37.5%, n = 127) indicated having received in-house faculty development that enhanced their ability to guide learners to become self-directed (Fig. 3). The source most frequently indicated was conferences or workshops (162; 47.8%). Only a small number of faculty had participated in a formal course (28; 8.3%) or a degree-granting course/program (28; 8.3%). It is notable that the most frequently selected preferred source for future training was faculty development provided by their institution (174; 51.3%), followed by conferences or workshops (101; 29.8%).
The capacity of faculty to identify strategies that promote SDL is mixed (Table 2). These data reveal that faculty were able to identify some of the strategies in all skill domains as those that promote SDL. They were more likely to recognize metacognitive and affective approaches, with averages of 67.7%, (SD = 13.6) and 61.7% (SD = 20.2), respectively, than items in the cognitive domain, which had an average 48.5% (SD = 26.3). Interestingly, while 67.3% (n = 70) of MDs indicated the affective domain promotes SDL, fewer Ph.D.s (53.8%, n = 82) indicated this skill domain promoted SDL (P = 0.001). There was no difference between MDs and Ph.D.s within the cognitive and metacognitive domains. In examining other demographic data, no differences in the capacity to recognize SDL strategies were observed by classroom setting or level of medical student taught.
The identical teaching strategies were presented to undergraduate medical students at the Zucker School of Medicine where SDL promoting instruction is stressed (Table 2) [24]. Students indicated that some items in the three skill domains can promote their ability to become self-directed but were not overwhelmingly positive about any particular strategy or domain, with similar average frequencies of recognition in each domain of 45.8% (cognition), 49.3% (affective), and 45.0% (metacognitive). Students and faculty identified cognitive strategies with roughly the same frequency (45.8% vs 48.5%, P = 0.79), but faculty identified affective and metacognitive strategies more frequently than students (61.7% vs 49.3%, P = 0.00 and 67.7% vs 45.0%, P = 0.00, respectively).
Discussion
The importance of self-directed learning is a dominant theme in twenty-first century medical education literature and has been adopted as an achievable goal for medical students [3] and residents [4]. Process- and learning-oriented teaching models are founded on the principles of SDL and the practices of SRL. They provide tangible instructional activities designed to help students develop SRL skills [13, 14, 20, 22]. These include strategies such as encouraging students to set goals (motivational domain), stimulating critical thinking (content building domain), and encouraging students to assess their knowledge and skill (metacognitive domain). SRL skills are thus prerequisite to becoming a life-long learner [10]. The implementation of learning-oriented teaching therefore requires deliberate consideration of the role of teachers, students, learning materials, and the educational culture [19, 20, 22].
Medical education literature appears to have thoroughly probed learners, as well as pedagogies such as problem-based learning [25], and the learning environment [26] for evidence that learners are becoming self-directed. By contrast, reports of faculty perceptions and preparation have been underrepresented in medical education literature. This article describes the development and deployment of an instrument designed to answer the following questions: Do faculty who deliver curricula believe SDL is of value? Do faculty know how to integrate strategies that foster SDL into their teaching? Do they feel supported by their administrators? Are they receiving sufficient faculty development?
Do faculty who deliver curricula believe SDL is of value? The effective integration of SDL in educational programs requires instructors who understand and are convinced of the value of SDL [6, 20]. SDL has been widely regarded as important for the acquisition of medical knowledge, skills, and attitudes during formal medical training [7] as well as for the development of physicians who are life-long learners [26]. Our national survey of over 300 medical educators shows faculty overwhelmingly believe that SDL is “essential for medical student success” and “fosters the development of life-long learning skills.”
Do faculty know how to integrate strategies that foster SDL into their teaching? Our survey assessed the capacity of faculty to promote SDL by asking respondents to identify a selection of teaching strategies, distributed over three domains (Table 2) that have been reported to foster proficiency in self-regulated learning [12, 13, 20]. Using recognition of instructional activities as a proxy for actual capacity to execute teaching that promotes SDL is admittedly imperfect. However, our intention was not the assessment of individual medical educators, but rather to paint a picture of the medical educator community.
We found that despite an overwhelming belief that SDL was essential, this did not translate to the capacity to recognize the means by which to foster its development. Faculty were most likely to view activities that promote metacognition as worthwhile and least likely to recognize strategies within the cognitive domain as important in fostering SDL. Metacognition may be most familiar to faculty since the practice of formative self-assessment has become common in UME and GME [27]. However, it is interesting to note that self-assessment—an integrated judgment of one’s ability in a particular domain—is not the same as the metacognitive act of self-monitoring, which entails real-time awareness of one’s skill or knowledge level in a specific situation. Self-monitoring is positively correlated with performance [28].
By contrast, within the cognitive domain, fewer than half of surveyed faculty recognized three of the six activities listed. For example, only about a quarter (28.1%) of respondents identified item 1 (explaining relationships between new and old concepts), which fosters knowledge scaffolding. Scaffolding involves relating new content to prior knowledge and has been shown to facilitate the transition from teacher to student regulation of the learning process [20].
Grow [12] argues persuasively that teachers can actively equip learners to become more self-directed. His staged SDL model asserts that learners and instructors must be matched in their readiness and ability to develop (learners) and coach (instructors) SDL. We queried students to determine if their recognition of teaching/learning strategies designed to promote SDL was congruent with that of faculty. There was a clear discordance between faculty and students in identifying educational strategies within the affective and metacognitive domains. The ability of faculty to more frequently recognize strategies within these domains suggests that faculty may have misaligned their expectations of students relative to the students’ understanding of an educational strategy.
Do faculty feel supported by their administrators? The importance of administrative support should not be underestimated as many of the strategies needed to promote the development of self-directed learners veer from traditional instructional models and therefore require buy-in from stakeholders at all levels. About two-thirds of faculty respondents in our study felt supported by their administration. This may reflect the broad endorsement SDL has received in medical education literature and, perhaps more importantly, by the LCME [3] and ACGME [4]. Despite this sense of support, only about a third of respondents had received in-house faculty development to accomplish this goal.
Are faculty receiving sufficient faculty development? The need to adequately prepare instructors for a successful implementation of SDL is widely recognized by educational experts [14, 20, 22] as well as by the faculty queried here. Just as we cannot assume all learners are equally equipped with the capacity to hone self-regulated learning skills, so too faculty differ in their understanding of how to guide students in this process [12]. Faculty recognize that learning-oriented teaching is not an innate talent as we found broad consensus that “instructors need training/faculty development in order to effectively promote SDL” and that faculty would “like to use more strategies that promote self-directed learning.” The finding that only about a third of faculty receive such training within their institutions suggests this is an unmet need.
Limitations
This study is not without limitations, which reduce the generalizability of our findings. First, despite efforts to achieve broad, national input from medical educators, our response rate was low, with only 339 respondents. Furthermore, we could not determine the survey response rate because the online survey was distributed via listservs. It may also be that those who responded represent a self-selected group of educators with an interest in SDL. Finally, surveying students at a single medical school where students are familiar with the principles of SDL limits the impact and generalizability of the student input.
Conclusion
Medical educators are keen to deliver curricula that produce physicians who are self-directed. Faculty recognize that they must be knowledgeable about pedagogies specifically designed to foster these skills. Likewise, learners understand the importance of external guidance in the development of SDL [23]. Thus, it is important that faculty receive the training and support needed to produce physicians who are life-long learners. We must recognize that it is unfair to demand that students acquire self-regulated learning skills if SDL is treated simply as an assumption embedded in the curriculum. Faculty development is key to ensuring that instructors have the tools to help learners meet the expectations of self-directed learning. Our instrument provides a means to evaluate the extent to which faculty members need assistance in becoming medical educators capable of guiding learners to become self-directed.
Acknowledgements
The authors would like to thank Lynn Foster-Johnson, Ph.D., for critically reading the manuscript and providing valuable insight, Saori Herman, MLIS, AHIP, for her assistance with references, and David Orner, MPH, for help with survey distribution.
Funding
This study was supported by an Educational Scholarship grant from the International Association of Medical Science Educators.
Declarations
Ethical approval
This study was deemed exempt by the Hofstra University Internal Review Board.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Artino AR, Jr, Brydges R, Gruppen LD. Self-regulated learning in healthcare profession education: theoretical perspectives and research methods. In: Cleland J, Brydges R, Gruppen LD, editors. Researching Medical Education. Hoboken, NJ: John Wiley & Sons; 2015. pp. 155–166. [Google Scholar]
- 2.Knowles MS. Self-directed learning : a guide for learners and teachers. New York, NY: Association Press; 1975. [Google Scholar]
- 3.Liaison Committee on Medical Education. Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. Association of American Medical Colleges; American Medical Association; 2020. Accessed September 9, 2019. https://lcme.org/wp-content/uploads/filebase/standards/2021-22_Functions-and-Structure_2020-03-31.docx2021-22_Functions-and-Structure_2020-03-31.docx.
- 4.Burke AE, Benson B, Englander R, Carraccio C, Hicks PJ. Domain of competence: practice-based learning and improvement. Acad Pediatr. 2014;14(2 Suppl):S38–54. doi: 10.1016/j.acap.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 5.Harvey BJ, Rothman AI, Frecker RC. Effect of an undergraduate medical curriculum on students' self-directed learning. Acad Med. 2003;78(12):1259–1265. doi: 10.1097/00001888-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Premkumar K, Pahwa P, Banerjee A, Baptiste K, Bhatt H, Lim HJ. Does medical training promote or deter self-directed learning? A longitudinal mixed-methods study. Acad Med. 2013;88(11):1754–1764. doi: 10.1097/ACM.0b013e3182a9262d. [DOI] [PubMed] [Google Scholar]
- 7.Murad MH, Coto-Yglesias F, Varkey P, Prokop LJ, Murad AL. The effectiveness of self-directed learning in health professions education: a systematic review. Med Educ. 2010;44(11):1057–1068. doi: 10.1111/j.1365-2923.2010.03750.x. [DOI] [PubMed] [Google Scholar]
- 8.Stegers-Jager KM, Cohen-Schotanus J, Themmen AP. Motivation, learning strategies, participation and medical school performance. Med Educ. 2012;46(7):678–688. doi: 10.1111/j.1365-2923.2012.04284.x. [DOI] [PubMed] [Google Scholar]
- 9.Kassab SE, Al-Shafei AI, Salem AH, Otoom S. Relationships between the quality of blended learning experience, self-regulated learning, and academic achievement of medical students: a path analysis. Adv Med Educ Pract. 2015;6:27–34. doi: 10.2147/amep.S75830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandars J, Cleary TJ. Self-regulation theory: applications to medical education: AMEE Guide No. 58. Med Teach. 2011;33(11):875-886. 10.3109/0142159x.2011.595434. [DOI] [PubMed]
- 11.Gandomkar R, Sandars J. Clearing the confusion about self-directed learning and self-regulated learning. Med Teach. 2018;40(8):862–863. doi: 10.1080/0142159x.2018.1425382. [DOI] [PubMed] [Google Scholar]
- 12.Grow GO. Teaching learners to be self-directed. Adult Educ Q (Am Assoc Adult Contin Educ). 1991;41(3):125–149. doi: 10.1177/0001848191041003001. [DOI] [Google Scholar]
- 13.Vermunt JD, Verloop N. Congruence and friction between learning and teaching. Learn Instr. 1999;9(3):257–280. doi: 10.1016/S0959-4752(98)00028-0. [DOI] [Google Scholar]
- 14.Bolhuis S. Towards process-oriented teaching for self-directed lifelong learning: a multidimensional perspective. Learn Instr. 2003;13(3):327–347. doi: 10.1016/S0959-4752(02)00008-7. [DOI] [Google Scholar]
- 15.Pilling-Cormick J, Garrison D. Self-directed and self-regulated learning: conceptual links. Can J Univ Contin Educ. 2013;33. 10.21225/D5S01M.
- 16.Hanson D. Instructor’s guide to process oriented guided inquiry learning. Hampton, NH: Pacific Crest; 2013. [Google Scholar]
- 17.Brown SD. A process-oriented guided inquiry approach to teaching medicinal chemistry. Am J Pharm Educ. 2010;74(7):121. doi: 10.5688/aj7407121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vermunt JD. Process-oriented instruction in learning and thinking strategies. Eur J Psychol Educ. 1995;10(4):325. doi: 10.1007/BF03172925. [DOI] [Google Scholar]
- 19.Vermunt JD, Vermetten YJ. Patterns in student learning: relationships between learning strategies, conceptions of learning, and learning orientations. Educ Psychol Rev. 2004;16(4):359–384. doi: 10.1007/s10648-004-0005-y. [DOI] [Google Scholar]
- 20.Vrieling E, Bastiaens T, Stijnen S. Process-oriented design principles for promoting self-regulated learning in primary teacher education. Int J Educ Res. 2010;49:141–150. doi: 10.1016/j.ijer.2011.01.001. [DOI] [Google Scholar]
- 21.Schunk DH, Zimmerman BJ, editors. Self-regulated learning: from teaching to self-reflective practice. New York, NY: Guilford Publications; 1998. [Google Scholar]
- 22.ten Cate O, Snell L, Mann K, Vermunt J. Orienting teaching toward the learning process. Acad Med. 2004;79(3):219–228. doi: 10.1097/00001888-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Sawatsky AP, Ratelle JT, Bonnes SL, Egginton JS, Beckman TJ. Faculty support for self-directed learning in internal medicine residency: a qualitative study using grounded theory. Acad Med. 2018;93(6). 10.1097/ACM.0000000000002077. [DOI] [PubMed]
- 24.Ginzburg S, Brenner J, Willey J. Integration: a strategy for turning knowledge into action. Med Sci Educ. 2015;25(4):533–543. doi: 10.1007/s40670-015-0174-y. [DOI] [Google Scholar]
- 25.Evensen DH, Salisbury-Glennon JD, Glenn J. A qualitative study of six medical students in a problem-based curriculum: toward a situated model of self-regulation. J Educ Psychol. 2001;93(4):659–676. doi: 10.1037/0022-0663.93.4.659. [DOI] [Google Scholar]
- 26.Artino AR, Jr, Dong T, DeZee KJ, et al. Achievement goal structures and self-regulated learning: relationships and changes in medical school. Acad Med. 2012;87(10):1375–1381. doi: 10.1097/ACM.0b013e3182676b55. [DOI] [PubMed] [Google Scholar]
- 27.Blanch-Hartigan D. Medical students’ self-assessment of performance: results from three meta-analyses. Patient Educ Couns. 2011;84(1):3–9. doi: 10.1016/j.pec.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 28.Eva KW, Regehr G. Exploring the divergence between self-assessment and self-monitoring. Adv Health Sci Educ Theory Pract. 2011;16(3):311–329. doi: 10.1007/s10459-010-9263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]