Abstract
Objective
This study compares data from two medical student cohorts early in their training from New Zealand and Hong Kong and then makes further comparisons with a non-medical group.
Methods
Questionnaires obtained information regarding educational site (universities situated in New Zealand, Hong Kong, and USA), gender, age, motivational beliefs, quality of life, and competitiveness. The study was split into two phases. The first phase focused on measuring and comparing the learning and wellbeing variables of two medical student cohorts. The second phase focussed on making further comparisons with non-medical student groups.
Results
Responses were elicited from 353 students in medically oriented courses and 688 students with a non-medical orientation. For phase 1, the results indicated differences between the two medical student groups on measures of self-efficacy, intrinsic value, enjoyment of competition, and physical quality of life. For phase 2, differences between the medical and non-medical student groups were noted for self-efficacy, intrinsic value, enjoyment of competition, contentiousness, and physical and social quality of life.
Conclusions
The results provide insights into medical and non-medical students’ learning and wellbeing experiences from multi-national, multi-discipline perspectives. The results suggest that wellbeing issues of students are likely context-specific and moderated by region, curriculum, gender, and culture.
Keywords: Medical and biomedical students, Social science students, Quality of life, Motivation beliefs, Competitiveness
Introduction
Considerable research has investigated the wellbeing of medical students [1–5]; however, fewer studies have explored how well these students fare in relation to their non-medical peers [6, 7]. Medical students in their first year of study are typically considered at risk of psychological morbidity and experience stress, which may increase as the year unfolds [8].
In one example, the Biomedical Common Year or Overlapping Year in a New Zealand university [9] is a set of Year 1 courses that academically prepares students for a conditional entry into courses such as Year 2 medicine. Entry into Year 2 medicine requires a high level of academic attainment in the Biomedical Common Year or Overlapping Year [10]. In New Zealand, it is estimated that about 50% of these Year 1 students indicate a preference for studying medicine [11], suggesting that about 700 students are vying for less than 270 allocated places in Year 2 [12]. Consequently, Year 1 of study likely creates a highly competitive learning environment, which makes it challenging to maintain a healthy lifestyle.
The principal objective, in this paper, was to gather information on quality of life (QOL), competitiveness, and motivational beliefs from several student groups, namely those studying in New Zealand, USA, and Hong Kong. The underlying focus of the paper was to examine how medical students early in their training, from New Zealand and Hong Kong, respond to these questionnaires to appraise their level of wellbeing and aspects of learning. The first phase of the investigation was to compare two regionally different medical student groups, at Year 1 of their training, to assess whether medical students across global boundaries respond similarly. In addition, to explore whether medical students are different from other student groups, we compared their responses with two non-medical student groups, also at Year 1 of their training, from New Zealand and USA. In this manner, we aimed to assess whether regional difference was more significant than discipline difference, or whether in fact all groups respond similarly.
Theoretical Background
There are strong theoretical arguments suggesting a connection between QOL, motivation to learn, and competitiveness. For example, ecological [13] and expectancy-value [14, 15] models of human behaviour emphasise the holistic nature of learning. Further, Konu and Rimpelä [16] developed a wellbeing model synthesising the facets of teaching and education with learning and wellbeing. According to this model, wellbeing is improved when optimising learning conditions, social relationships within the learning environment, developing a sense of self-fulfilment, and optimising health conditions.
Students early in their tertiary education are often seen as high-risk students when compared with those studying in later years [17]. There have been strong links established between student academic success, their motivation to succeed, and level of satisfaction. In higher education establishments, students’ perceptions of their QOL have been well reported and it has been stated that students in their early years of study experience undue stress, which has an impact on study perseverance [18, 19]. Additionally, medical students experience physical and psychological wellbeing issues in their first year of study, and their responses indicated that these issues decline over the course of the year [20].
With reference to medical students, there are reports suggesting they are at high risk of diminished QOL [2, 3, 21, 22], with some papers suggesting the need for coping strategies and interventions to deal with the stressors associated with the intense medical learning environment [6, 23]. It has been further suggested that biomedical students in New Zealand (potentially Year 1 medicine) students’ levels of quality of life are linked to motivational beliefs and levels of competitiveness [24]. More specifically, higher levels of QOL were found to be associated with higher levels of self-efficacy, intrinsic value, enjoyment of competition, and lower levels of test anxiety. Additionally, Mitchell [25] reported that medical students, in general, view themselves as both intrinsically motivated and anxious, and these variables were able to contribute to a model predicting academic achievement. In their review of the literature, Kusurkar et al. [26] found that medical students’ feelings of wellbeing enhanced motivation culminating in a sense of thriving within the clinical learning environment.
Furthermore, Lonka et al. [27] investigated links between medical students’ perceptions of their wellbeing, motivation, and learning. They reported correlations between dysfunctional orientations to learning and negative views of the learning environment. Dysfunctional orientation to learning was also correlated with disengagement, reports of a high workload, and anxiety. In a systematic review, Dyrbye, Thomas, Shanafelt [3] reported that psychological distress was evident amongst female medical students, although it was suggested that there is a dearth of data linking medical student distress with academic performance, dropout rates, and professional development. Similar gender differences have been noted elsewhere [24, 28, 29].
Bugaj et al. [6] stated that medical students are considered to be more stressed when compared with age-matched peers and medical students appear to be more at risk of psychological issues, such as depression, anxiety, and depression. Dyrbye, Thomas, and Shanafelt [3] reported evidence that there is a high prevalence of depression and anxiety amongst medical students, and that psychological distress amongst medical students is consistently higher than in the general population and age-matched peers. In a recent systematic review and meta-analysis, Rotenstein et al. [30] found that a high prevalence of depressive symptoms appears to be still a major issue amongst medical students and higher than in the general population. Nonetheless, Henning et al. [7] reported that when compared with the general population norms, both medical and non-medical students expressed concerns related to QOL, although no evidence was reported to indicate that medical students were worse off than their non-medical peers.
Several assumptions need to be considered in a comparative multi-national study. The first assumption is that different cultural groups have different experiences of wellbeing and learning. With respect to the operational variables used in this study, we found no studies comparing New Zealand and Hong Kong medical students. However, Chan [31] showed that Chinese medical students were found to report higher level of depression compared with their US medical peers, although no difference was found when compared with a non-medical Chinese student group.
The second assumption is that different learning environments may engender different student responses to wellbeing and learning. There are studies that have attempted to compare wellbeing experiences across regional boundaries [32]. We were unable to find any literature comparing wellbeing and learning variables of medical students across international boundaries. Some studies in the general education literature attempted to investigate this phenomenon. Stankov [33] proposed that students who can be identified as ‘Confucian Asian’ are often more driven than European students towards academic attainment; specifically, they had less tolerance for underachievement, which suggests a higher level of competitiveness. Stankov also reported that the Confucian Asian students appeared to apply more effort, be more persistent, and exhibited relatively higher levels of anxiety and self-doubt when compared with their European peers.
In summary, we have shown that there is a theoretical rationale underlying this investigation and evidence to suggest that first-year students are often greatly challenged and hence a high priority for research. Second, we have provided evidence above to show that medical students experience QOL challenges and these are often linked with learning experiences. Third, we have indicated that medical students have more QOL challenges than their non-medical peers and, finally, students studying in different regions are likely to have different experiences of QOL and learning. With this context in mind, we explore two research questions:
Do medical students, early in their training, across two different medical schools, situated in New Zealand and Hong Kong, respond similarly to questions on wellbeing and learning factors?
When compared with their non-medical student peers, do these medical students respond similarly to questions on wellbeing and learning factors?
Methods
Participants
Students from four universities were invited to participate in this study. At the University of Auckland, all students (N = 1036) studying in a population health course in 2014 within the Biomedical Common Year or Overlapping Year [9] were invited to participate in this survey. At Auckland University of Technology, students enrolled in various general health courses in years 1 and 2 were invited (N = 386). At West Chester University, undergraduate students (various majors) enrolled in two sections of a general education psychology course were invited to participate as an option in fulfilling their course research requirement (N = 429). At the University of Hong Kong, all students studying first-year medicine were invited and present during a whole class lecture (n = 192 from a total student population of N = 210).
Each of the five groups will be abbreviated (see italics below) from hereon in:
UoAMed: students intending to study medicine within the Biomedical Common Year or Overlapping Year [9] at the University of Auckland
UoAnon-Med: students not intending to study medicine within the Biomedical Common Year or Overlapping Year [9] at the University of Auckland
AUT: health science courses in years 1 and 2 at Auckland University of Technology [34]
WCU: a first-year general education psychology course at West Chester University [35]
HKU: first-year medicine at the University of Hong Kong [36]
Procedure
Ethics approval for the collection and use of data was obtained from all universities. The UoA students (medical and non-medical) were sent an email with a link to an online survey and invited to respond to the survey. The AUT students were introduced to the research study by one of the researchers at a face-to-face lecture, and paper versions of the questionnaire were handed out during a lecture break. Completed paper questionnaires could be handed back to a return box in the lecture theatre or a locked box at the faculty reception. The WCU participants responded to an online survey via Qualtrics software. The HKU participants responded to a paper-based survey.
Measures
Demographic and Background Details
Age and gender measures were obtained.
Motivated Strategies for Learning Questionnaire [37]
The motivational beliefs scale used by Pintrich, De Groot [37] was adapted for this study. Three scales measured aspects of self-efficacy (9 items), intrinsic value (9 items), and test anxiety (4 items). Students were instructed to respond to the items on a 5-point Likert scale (1 = never true to 5 = always true) in reference to their perceptions of their motivational behaviour.
World Health Organisation QOL Questionnaire (BREF) [38]
The four domains cited in this instrument were used, namely physical QOL (7 items), psychological QOL (10 items), social relationships (3 items), and environmental conditions (8 items). All items are presented on a 5-point Likert scale with varying anchors. Three items (items 3, 4, and 26) had to be reversed so that high scores represent higher levels of QOL and lower scores the converse.
Revised Competitiveness Index [39]
This 14-item instrument utilises two scales that measure students’ levels of competitiveness within the learning environment. These include enjoyment of competition (9 items) and contentiousness or avoidance of conflict situations (5 items). All items are presented on a 5-point Likert scale (1 = never true to 5 = always true) with 9 items reversed scored.
Data Analysis
First, the response rates (n/N) for each university were calculated as a percentage measure. Second, statistics were presented that described the demographic and background details of the participants. Preliminary statistics were conducted to ensure the domains within the instruments yielded acceptable Cronbach’s alpha coefficients [40].
The first inferential analysis concentrated on identifying differences and similarities between the two medical student groups, early in their training, across two different medical schools, situated in New Zealand and Hong Kong. We utilised the IBM SPSS statistics version 24 package [41], and incorporated a multiple analysis of covariance (MANCOVA) [42] to analyse the effect of the measures cited above in reference to the two medical student groups. Using these same data analysis methods, the second inferential analysis concentrated on identifying differences and similarities between the medical and non-medical student groups. Given there were nine measures, a Bonferroni correction was implemented to reduce the potential for type-1 errors related to multiple comparisons, which set the required cutoff value to p < .006 [43].
Results
Response Rate and Participant Data
The sample characteristics and response rates (n/N) are shown in Table 1. The age differences amongst cohorts and gender proportional differences suggest the need to include these variables in the multi-variate model. The response rates were high for WCU and HKU but modest for AUT and UoA cohorts [44, 45].
Table 1.
Demographic characteristics (age and gender) for each for each of the cohorts
| Characteristics | Cohort | |||||
|---|---|---|---|---|---|---|
| AUT (n = 139) | HKU (n = 165) | UoAMed (n = 188) | UoAnon-Med (n = 151) | WCU (n = 399) | ||
| Age | Mean | 22.45 | 18.33 | 18.88 | 19.01 | 19.17 |
| SD | 6.4 | 0.53 | 2.18 | 3.42 | 2.2 | |
| Gender | Female | 114 | 85 | 53 | 33 | 265 |
| Male | 25 | 80 | 135 | 118 | 134 | |
| Response rates | 36% | 86% | 33% | 93% | ||
Subsequent differences in values are due to incomplete responses by some participants
Descriptive Measures for Instruments
The means and standard deviations for the measures of QOL, motivational beliefs, and competiveness for all groups were compared with other studies, and no anomalies were noted [7, 39, 46, 47]. The internal consistency measures ranged from 0.71 to 0.92 across all nine domains suggesting that all measures were within satisfactory requirements [42].
A preliminary analysis (using a MANCOVA) showed that gender and age were influential. Hence, the gender and age variables were added into the final MANCOVA model with gender as an independent variable and age as a covariate. The main analysis focused on examining the students’ group responses amongst four university contexts (phase 1 between the two medical student cohorts and phase 2 the medical versus non-medical cohorts).
Findings from the MANCOVA Model
Medical Student Groups
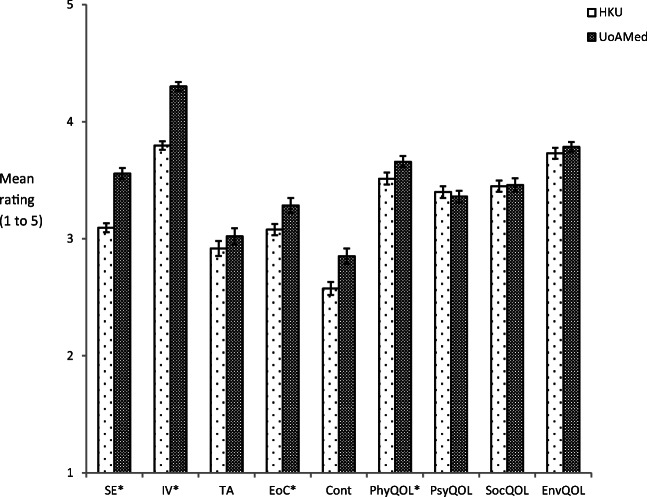
A multi-variate effect was noted for the medical student cohort, Wilks’ Lambda = 0.72, F(9, 339) = 14.00, p < .001. A series of univariate comparisons identified four measurement main effect differences, namely for self-efficacy, intrinsic value, enjoyment of competition, and physical QOL (p < .006) between the two medical students groups (as illustrated in Fig. 1). More specifically:
A significant difference between the HKU ratings for self-efficacy (M = 3.09, SD = .50) and UoAMed ratings (M = 3.56, SD = 0.65); F(1, 347) = 67.93, p < .006
A significant difference between the HKU ratings for intrinsic value (M = 3.80, SD = 0.47) and UoAMed ratings (M = 4.30, SD = 0.52); F(1, 347) = 71.71, p < .006
A significant difference between the HKU ratings for enjoyment of competition (M = 3.08, SD = 0.63) and UoAMed ratings (M = 3.29, SD = 0.88); F(1, 347) = 13.64, p < .006
A significant difference between the HKU ratings for physical QOL (M = 3.51, SD = .65) and UoAMed ratings (M = 3.66, SD = 0.66); F(1, 347) = 9.41, p < .006
Fig. 1.
Bar chart showing the mean ratings (with standard error bars) for each measure across the two medical cohorts. * signifies significant differences between medical cohorts (p < .006); SE self-efficacy, IV intrinsic value, TA test anxiety, EoC enjoyment of competition, Cont contentiousness, PhysQOL physical QOL, PsyQOL psychological QOL, SocQOL social QOL, and EnvQOL environmental QOL). Mean rating (1 to 5)
One significant interaction effect for cohort by gender was noted (Table 2). More specifically, the interaction effect was associated with for test anxiety with the HKU ratings (Mfemale = 2.89, SDfemale = 0.80; Mmale = 2.95, SDmale = 0.84) compared with UoAMed ratings (Mfemale = 2.50, SDfemale = 0.72; Mmale = 3.23, SDmale = 0.97); F(1, 347) = 16.45, p < .006. See Table 4 in Appendix for full MANCOVA details.
Table 2.
Means and standards deviations (SD) for each measure across gender by medical cohorts with significant interactions indicated
| Measures | Medical cohorts | ||||||
|---|---|---|---|---|---|---|---|
| HKU (n = 164) | UoAMed (n = 188) | ||||||
| Male | Female | All | Male | Female | All | ||
| Self-efficacy | Mean | 3.17 | 3.03 | 3.09 | 3.84 | 3.45 | 3.56 |
| SD | 0.52 | 0.47 | 0.50 | 0.53 | 0.67 | 0.65 | |
| Intrinsic value | Mean | 3.74 | 3.85 | 3.80 | 4.25 | 4.32 | 4.30 |
| SD | 0.50 | 0.44 | 0.47 | 0.53 | 0.51 | 0.52 | |
| Test anxiety* | Mean | 2.95 | 2.89 | 2.92 | 2.50 | 3.23 | 3.02 |
| SD | 0.84 | 0.80 | 0.82 | 0.72 | 0.97 | 0.96 | |
| Enjoyment of competition | Mean | 3.17 | 2.99 | 3.08 | 3.63 | 3.15 | 3.29 |
| SD | 0.64 | 0.60 | 0.63 | 0.76 | 0.89 | 0.88 | |
| Contentiousness | Mean | 2.64 | 2.52 | 2.57 | 2.81 | 2.87 | 2.85 |
| SD | 0.77 | 0.66 | 0.72 | 0.90 | 0.94 | 0.93 | |
| Physical QOL | Mean | 3.52 | 3.51 | 3.51 | 3.88 | 3.57 | 3.66 |
| SD | 0.65 | 0.65 | 0.65 | 0.64 | 0.65 | 0.66 | |
| Psychological QOL | Mean | 3.43 | 3.37 | 3.40 | 3.60 | 3.27 | 3.36 |
| SD | 0.63 | 0.65 | 0.64 | 0.64 | 0.67 | 0.68 | |
| Social QOL | Mean | 3.36 | 3.53 | 3.45 | 3.38 | 3.49 | 3.46 |
| SD | 0.67 | 0.57 | 0.62 | 0.72 | 0.81 | 0.78 | |
| Environmental QOL | Mean | 3.64 | 3.81 | 3.73 | 3.88 | 3.75 | 3.79 |
| SD | 0.68 | 0.50 | 0.60 | 0.57 | 0.58 | 0.57 | |
*Significant interactions (p < .006) for medical cohorts by gender
Table 4.
Summary of the tests of between-subjects effects for the MANCOVA involving gender by medical cohorts with covariate results for age omitted
| Source | df | SS | F | |
|---|---|---|---|---|
| Medical cohorts | Self-efficacy | 1 | 22.20 | 67.93✝ |
| Intrinsic value | 1 | 17.51 | 71.71✝ | |
| Test anxiety | 1 | 0.63 | 0.84 | |
| Enjoyment of competition | 1 | 7.83 | 13.64✝ | |
| Contentiousness | 1 | 4.63 | 6.61* | |
| Physical QOL | 1 | 3.94 | 9.41** | |
| Psychological QOL | 1 | 0.05 | 0.11 | |
| Social QOL | 1 | 0.01 | 0.01 | |
| Environmental QOL | 1 | 0.77 | 2.26 | |
| Gender | Self-efficacy | 1 | 5.59 | 17.10✝ |
| Intrinsic value | 1 | 0.61 | 2.49 | |
| Test anxiety | 1 | 8.36 | 11.19** | |
| Enjoyment of competition | 1 | 8.41 | 14.65✝ | |
| Contentiousness | 1 | 0.06 | 0.09 | |
| Physical QOL | 1 | 1.86 | 4.44* | |
| Psychological QOL | 1 | 3.18 | 7.50** | |
| Social QOL | 1 | 1.42 | 2.80 | |
| Environmental QOL | 1 | 0.04 | 0.14 | |
| Medical cohorts *gender | Self-efficacy | 1 | 1.21 | 3.69 |
| Intrinsic value | 1 | 0.03 | 0.10 | |
| Test anxiety | 1 | 12.30 | 16.45✝ | |
| Enjoyment of competition | 1 | 1.67 | 2.91 | |
| Contentiousness | 1 | 0.59 | 0.85 | |
| Physical QOL | 1 | 1.70 | 4.07 | |
| Psychological QOL | 1 | 1.52 | 3.57 | |
| Social QOL | 1 | 0.06 | 0.13 | |
| Environmental QOL | 1 | 1.68 | 4.96 | |
*p < .05, **p < .01, ✝+++p < .001
Medical Versus Non-medical Student Groups
A multi-variate effect was noted for the medical student cohort, Wilks’ Lambda = 0.72, F(9, 1017) = 23.98, p < .001. A series of univariate comparisons identified six measurement main effect differences for self-efficacy, intrinsic value, enjoyment of competition, contentiousness, physical QOL, and social QOL (p < .006) between the two students groups (as illustrated in Fig. 2). More specifically:
A significant difference between the medical student group ratings for self-efficacy (M = 3.34, SD = .63) and non-medical student ratings (M = 3.51, SD = 0.67); F(1, 1025) = 13.88, p < .006
A significant difference between the medical student ratings for intrinsic value (M = 4.07, SD = 0.56) and non-medical student ratings (M = 3.78, SD = 0.59); F(1, 1025) = 65.60, p < .006
A significant difference between the medical student ratings for enjoyment of competition (M = 3.19, SD = 0.78) and non-medical student ratings (M = 3.37, SD = 0.99); F(1, 1025) = 22.44, p < .006
A significant difference between the medical student ratings for contentiousness (M = 2.72, SD = .84) and non-medical student ratings (M = 2.84, SD = 0.87); F(1, 1025) = 11.85, p < .006
A significant difference between the medical student ratings for physical QOL (M = 3.59, SD = .66) and non-medical student ratings (M = 3.79, SD = 0.60); F(1, 1025) = 23.45, p < .006
A significant difference between the medical student ratings for social QOL (M = 3.45, SD = 0.71) and non-medical student ratings (M = 3.61, SD = 0.83); F(1, 1025) = 7.60, p < .006
Fig. 2.
Bar chart showing the mean ratings (with standard error bars) for each measure across the medical and non-medical cohorts. * signifies significant differences between medical cohorts (p < .006); SE self-efficacy, IV intrinsic value, TA test anxiety, EoC enjoyment of competition, Cont contentiousness, PhysQOL physical QOL, PsyQOL psychological QOL, SocQOL social QOL, and EnvQOL environmental QOL). Mean rating (1 to 5)
Two significant interaction effects for cohort by gender were noted (Table 3). The first interaction effect was associated with for enjoyment of competition with the medical students ratings (Mfemale = 3.09, SDfemale = 0.80; Mmale = 3.35, SDmale = 0.73) compared with non-medical student ratings (Mfemale = 3.19, SDfemale = 0.96; Mmale = 3.81, SDmale = 0.91); F(1, 1025) = 8.17, p < .006. The second interaction effect was associated with contentiousness with the medical student ratings (Mfemale = 2.74, SDfemale = 0.86; Mmale = 2.70, SDmale = 0.83) compared with non-medical student ratings (Mfemale = 2.74, SDfemale = 0.88; Mmale = 3.11, SDmale = 0.82); F(1, 1025) = 10.99, p < .006. See Table 5 in Appendix for full MANCOVA details.
Table 3.
Means and standards deviations (SD) for each measure across gender by medical and non-medical cohorts with significant interactions indicated
| Measures | Medical and non-medical cohorts | ||||||
|---|---|---|---|---|---|---|---|
| Medical (n = 353) | Non-medical (n = 688) | ||||||
| Male | Female | All | Male | Female | All | ||
| Self-efficacy | Mean | 3.43 | 3.29 | 3.34 | 3.56 | 3.50 | 3.51 |
| SD | 0.62 | 0.63 | 0.63 | 0.56 | 0.70 | 0.67 | |
| Intrinsic value | Mean | 3.94 | 4.14 | 4.07 | 3.62 | 3.84 | 3.78 |
| SD | 0.57 | 0.54 | 0.56 | 0.59 | 0.57 | 0.59 | |
| Test anxiety | Mean | 2.77 | 3.09 | 2.97 | 2.78 | 3.11 | 3.02 |
| SD | 0.82 | 0.92 | 0.90 | 0.90 | 0.96 | 0.95 | |
| Enjoyment of competition* | Mean | 3.35 | 3.09 | 3.19 | 3.81 | 3.19 | 3.37 |
| SD | 0.73 | 0.79 | 0.78 | 0.91 | 0.96 | 0.99 | |
| Contentiousness* | Mean | 2.70 | 2.73 | 2.72 | 3.10 | 2.74 | 2.84 |
| SD | 0.83 | 0.86 | 0.84 | 0.82 | 0.88 | 0.87 | |
| Physical QOL | Mean | 3.66 | 3.55 | 3.59 | 3.86 | 3.77 | 3.79 |
| SD | 0.67 | 0.65 | 0.66 | 0.58 | 0.60 | 0.60 | |
| Psychological QOL | Mean | 3.50 | 3.31 | 3.38 | 3.58 | 3.44 | 3.48 |
| SD | 0.64 | 0.66 | 0.66 | 0.68 | 0.73 | 0.72 | |
| Social QOL | Mean | 3.37 | 3.51 | 3.45 | 3.55 | 3.64 | 3.61 |
| SD | 0.69 | 0.72 | 0.71 | 0.86 | 0.82 | 0.83 | |
| Environmental QOL | Mean | 3.74 | 3.77 | 3.76 | 3.68 | 3.70 | 3.69 |
| SD | 0.64 | 0.55 | 0.58 | 0.59 | 0.59 | 0.59 | |
*Significant interactions (p < .006) for medical and non-medical cohorts by gender
Table 5.
Summary of the tests of between-subjects effects for the MANCOVA involving gender by medical versus non-medical cohorts with covariate results for age omitted
| Source | df | SS | F | |
|---|---|---|---|---|
| Medical versus non-medical cohorts | Self-efficacy | 1 | 5.95 | 13.88✝ |
| Intrinsic value | 1 | 20.93 | 65.60✝ | |
| Test anxiety | 1 | 0.00 | 0.00 | |
| Enjoyment of competition | 1 | 17.68 | 22.44✝ | |
| Contentiousness | 1 | 8.70 | 11.85** | |
| Physical QOL | 1 | 8.85 | 23.45✝ | |
| Psychological QOL | 1 | 2.48 | 5.14* | |
| Social QOL | 1 | 4.76 | 7.60** | |
| Environmental QOL | 1 | 0.70 | 2.04 | |
| Gender | Self-efficacy | 1 | 2.32 | 5.43* |
| Intrinsic value | 1 | 8.98 | 28.14✝ | |
| Test anxiety | 1 | 21.69 | 25.45✝ | |
| Enjoyment of competition | 1 | 39.22 | 49.78✝ | |
| Contentiousness | 1 | 5.62 | 7.65** | |
| Physical QOL | 1 | 2.30 | 6.10 | |
| Psychological QOL | 1 | 5.66 | 11.73** | |
| Social QOL | 1 | 2.61 | 4.16* | |
| Environmental QOL | 1 | 0.15 | 0.45 | |
| Medical versus non-medical cohorts *gender | Self-efficacy | 1 | 0.33 | 0.78 |
| Intrinsic value | 1 | 0.04 | 0.13 | |
| Test anxiety | 1 | 0.00 | 0.00 | |
| Enjoyment of Competition | 1 | 6.44 | 8.17** | |
| Contentiousness | 1 | 8.07 | 10.99** | |
| Physical QOL | 1 | 0.01 | 0.02 | |
| Psychological QOL | 1 | 0.15 | 0.30 | |
| Social QOL | 1 | 0.07 | 0.12 | |
| Environmental QOL | 1 | 0.03 | 0.08 | |
*p < .05, **p < .01, ✝p < .001
Discussion
The aim of the current paper was to compare the perceived levels of QOL and learning variables between medical students in two regions and then compare these medical student responses with non-medical students. Given the complexity of the analysis, we have split the analysis into two distinct parts with a focus on medical students.
In the first analysis, we explored how the two medical student groups (New Zealand and Hong Kong) responded to the questionnaires to gauge regional and curricula influences. In New Zealand, the Biomedical Common Year or Overlapping Year is essentially a Year 1 course for medicine as it is for other health science courses; hence, even though the New Zealand medical students designated in this study could be considered intending medical students, they are in fact in their first year of medicine and will progress to Year 2 if they achieve the necessary entry criteria. The main perceived differences between these New Zealand medical students and those studying in Hong Kong are regional and endorsement.
In the second analysis, we explored how medical students (New Zealand and Hong Kong) compared with non-medical student responses (two groups from New Zealand and one from the USA). One internal control group came from the same course as the medical student group, but these students did not intend to apply for medicine. The second non-medical group comprised New Zealand health science students studying in the same city as the New Zealand medical group but at a different university. The last non-medical student comprised general education psychology students studying in a US university. This created a rich comparison group of non-medical students (internal, regional, and international controls).
Medical Cohort Comparisons: Regional Differences
The findings clearly show four differences between the two medical student cohorts, situated in New Zealand and Hong Kong. Students studying in UoAMed responded higher on self-efficacy, intrinsic value, enjoyment of competition, and physical QOL than their HKU peers. All significant differences were noted in favour of the UoAMed group. The differences are likely due to two reasons.
First, the UoAMed group are not yet fully confirmed as medical students (with about 40% likely to be accepted) and are in a crucial year that decides whether or not they will be admitted into medicine [11]. Hence, this year is their high stakes year for entry into the formalised Year 2 medical programme. In contrast, the HKU group are already selected into their Year 1 medical programme. Therefore, it is of no surprise that facets that measure self-efficacy, intrinsic-value, competition, and physical QOL (given they likely need to be physically robust) are higher for the UoAMed group. Lee, Lee, and Bong [48] found that both self-efficacy and interest could influence grade attainment in both English and Korean learning environments. Self-efficacy had a direct effect on grade outcome, whilst interest (or intrinsic value) had an indirect effect via self-regulation. In both cases, higher levels of self-efficacy and intrinsic value resulted in high grade achievement. In addition, possessing high levels of self-efficacy is critical to survival and success in a highly competitive learning environment [49]. The impact of grade attainment is also likely a feedback mechanism that influences both self-efficacy and enjoyment of competition, suggesting that achieving high levels of academic attainment will reinforce or dampen these two states. Lastly, to thrive in a medicine course, a student needs to be both physically and psychologically robust, and this is likely accentuated, and of great importance, when the year is high stakes. [50]
Second, the differences may be explained in terms of response bias [51], suggesting that there is a cultural difference in terms of responding. Chen, Lee, and Stevenson [51] conducted a study on self-reporting styles between three cultural groups, namely students from Japan, US, and Taiwan. In their study, the questionnaire provided items that focused on the effect of daily events and school life. The findings indicated that US students responded in a more extreme manner than the other two groups, with the US participants favouring extreme values whilst the Japanese and Taiwanese groups preferred mid-point options. In a further study, Harzing [52] reported major differences in response styles between 26 countries and these differences were not only between countries but also between cultural groupings within countries. In addition, Harzing suggested that differences between extreme and middle response styles are likely linked to both cultural and language differences. Hence, even though it is likely that the HKU group had a very high standard of English language, their use of the English language and understanding of concepts will likely differ from those of the UoAMed students, leading to differential responses patterns to equivalent scale anchors. To assist in making meaningful comparative interpretations, the cultural preference for mid-point versus extreme values is scope for further research amongst these cohorts.
Lastly, as shown in Table 4, only one interaction effect with gender was noted for test anxiety. This result indicates that gender, with the exception of test anxiety, does not appear to have an influential effect on the differences noted between the two cohorts. The gender and medical cohort effect result for test anxiety indicates that it is the UoAMed that contribute to this outcome, with male students scoring lower than female students. This disparity is not an uncommon finding in the international literature investigating the wellbeing of medical students, with one review stating that female students are more at risk of burnout and emotional exhaustion whilst male students are more risk of depersonalisation [50]. It is also not uncommon to be reported in the New Zealand literature [47]. This interaction may also indicate that this high-stakes year of study at UoAMed has a more anxiety-provoking impact on female students than their male counterparts.
Medical Students Versus Non-medical Students
When combined, the two medical student cohorts were different to the combined non-medical student cohorts on six of the nine measures. Medical students rated the intrinsic value measure higher than the non-medical peers, but the non-medical students rated the self-efficacy, enjoyment of competition, contentiousness, physical QOL, and social QOL higher than the medical student counterparts. No differences were noted for test anxiety, psychological QOL, and environment QOL.
First, the difference in intrinsic value is highly significant (F-ratio = 65.60), suggesting that this is an important distinction between the two groups and this is likely to be attributed to the course intention effect. In Table 3, we note that the mean for the non-medical group is 3.78 and the mean for the HKU group is 3.74, but the mean for the UoAMed group is 4.25. This indicates that those students intending to study medicine, but not yet ratified as medical students, are more engaged with their studies than other students. This level of engagement is understandable given their high-stakes investment in the course of study. Another potential difference could be associated with the effect of an autonomy-supported approach in which students are encouraged to make their own choices regarding their preferred career path they wish to aim for. If students act in an autonomous manner, they are more likely to cultivate feelings of volition, willingness, and choice, which fit well with a self-determination perspective [53].
Second, the high scores on intrinsic value are in contrast with the relative low scores on self-efficacy, enjoyment of competition, contentiousness, physical QOL, and social QOL. The overall self-efficacy score for the non-medical group is 3.51, whilst the overall score for the UoAMed group is 3.56, suggesting that the difference is potentially influenced by a curricula, cultural, and/or regional difference, which is consistent with the literature on middle to extreme differences in responding [51]. The differences on levels of both enjoyment of competition and contentiousness being in favour of the non-medical students are somewhat counterintuitive given that medical students are operating in a highly competitive learning environment [54]. However, it may also suggest that coping in a competitive environment is different from enjoyment of competition. In addition, the differential scores for contentiousness may suggest that the medical students (early in their training) are more confronting than their non-medical peers, although it is likely to have a moderating effect of culture given that the HKU mean is 2.57 and UoAMed mean is 2.85, which is similar to the non-medical overall mean of 2.84. Lastly, the lower mean scores for medical students on two of the four QOL measures, physical and social QOL, are consistent with the literature suggesting medical students have greater issues with wellbeing than other students [50].
The null effects for two of the QOL measures, psychological and environmental QOL, are not consistent with the literature [5, 50]. In particular, issues such as depression, anxiety, and burnout are considered more prevalent amongst medical students [5, 50]. In addition, one study reported that medical students scored consistently higher in environmental QOL than other students [7].
Lastly, two group and gender interaction effects were noted, specifically for enjoyment of competition and contentiousness. The results suggest that male medical students scored lower than their non-medical student peers but female students appear to be more similar across both groups. Hence, the notion of competitive difference between the medical and non-medical groups, discussed above, is likely moderated by cultural, curricula, regional, and/or gender. Furthermore, the differences between the gender scores within the medical student groups are less marked than those observed in the non-medical group suggesting that non-medical male students enjoy competition and are more confronting than their female peers and both male and female medical students. It is acknowledged and clearly evident in Tables 4 and 5 (Appendix) that gender differences are common place in the university environment and this appears to be prevalent in both the medical and non-medical learning environments, and in particular these findings show that the critical areas are likely to be related to anxiety, psychological wellbeing, and competitiveness. Gender disparities are common place with respect to wellbeing and are well recorded in the medical education literature and clearly scope for ongoing research [50, 54]. This may also have implications for speciality selection and perseverance in the programs of study.
Ameliorative Actions to Promote Students’ Quality of Life
There are options that could be employed to enhance students’ learning experiences and quality of life. At the institutional level, a consistent audit of selection processes, curriculum planning and development, and ensuring students are well supported is essential [23]. To ensure there is an optimal fit between courses and students, selection criteria need to consider not only cognitive capability but also the professional and social skills required to apply these cognitive skills to the wider communities that these students will serve. [55] Curriculum planning and development is often a difficult balancing act between ensuring graduate competencies are maximised through delivery of relevant content using effective and efficient pedagogical strategies [56]. Nevertheless, the curriculum needs to be aware of the environmental and learning variables that influence students’ wellbeing and their motivation to learn. Therefore, implementation of resilience strategies such as the university endorsed Computer-Assisted Learning for the Mind website [57] are useful to assist students not only whilst training but also when they graduate and become professionals contributing to the communities they serve. Lastly, it is important that students know of the support services available at their institution as well as a developing a culture that endorses help seeking behaviour, such as when coping with mental health issues [58].
Students also have a responsibility for engaging in self-care activities so that they can cope with the demands of university level study and better prepare themselves for future workplace stressors. Some coping strategies that could be employed include seeking support from friends and family support, and engaging in regular exercise and leisure activities [59], in addition, being willing and able to seek more professional help when life becomes unmanageable, such as financial assistance, counselling, learning advice, health services, and supervision/mentoring [59, 60]. Other self-care strategies include choosing eating healthily, engaging in constructive interpersonal relations, being responsible about one’s health, engaging in physical activity, being open to spiritual growth options, and implementing other stress management techniques [61].
Limitations and Strengths of the Study
There are limitations to the present study design. First, a relatively low response rate was attainment for the UoA and AUT cohorts but the response rates from the other two centres were high. Even so, the response rates for the UoA and AUT groups are comparable with those cited elsewhere and a review of response rates suggests that they fall within acceptable limits for representativeness of this type of survey [44, 45, 62]. Second, a social desirability measure to control for response bias could have been included. It has long been accepted that respondents can fake their responses to questionnaires and can recognise the intentions of the measurement strategies behind the items [63]. In addition, combining the medical (UoAMed and HKU) and non-medical cohorts (UoAnonMed, AUT WCU) for analysis purposes may mask the probable disparities between and within these subgroups. Nonetheless, we argue that combining the medical and non-medical groups for the purpose of analysis has the advantage of making the comparisons potentially more meaningful by including participants from a range of courses as well as including students from a range of universities in New Zealand, Hong Kong, and USA. One further potential limitation of the study relates to the confirmation of medical students. In New Zealand, context confirmation occurs after Year 1 whilst in Hong Kong, this context occurs prior to Year 1. We feel this analysis adds to the richness of discussion related to creating a confirmation track or not prior to studying at university. The current findings suggest that the high intensity environment may not adversely affect motivation, enjoyment of competition, or physical health. It could, thus, be argued that exposing students to this learning environment may best prepare them for the demands of later medical training. This is an area of great interest and potential for further research, given the high intensity learning environments associated with medical training.
The strength of the study is the multi-national comparative design feature and the relatively large sample sizes. We have not found any similar study that compares medical and non-medical students, early in their training across four different sites. Furthermore, the global context of the study enables further light to be shone on a complex issue. Clearly, there are regional and cultural influences that affect the students’ response patterns to measures of QOL and learning. To understand these contextual influences further, such as in the context of medical curricula, the impact of high-stakes exams, and recruitment strategies, more comparative research is suggested.
Appendix
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Initial approval was granted by the University of Auckland Human Participants Ethics Committee on 20 Nov 2013 Reference Number 010641. Subsequent approval was obtained from the three remaining centres.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ablard K, Lipschultz R. Self-regulated learning in high-achieving students: relations to advanced reasoning, achievement goals, and gender. J Educ Psychol. 1998;90(1):94–101. doi: 10.1037/0022-0663.90.1.94. [DOI] [Google Scholar]
- 2.Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, Shanafelt TD. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006;81:374–384. doi: 10.1097/00001888-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. 2006;81(4):354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Salamonson Y, Everett B, Koch J, Wilson I, Davidson PM. Learning strategies of first year nursing and medical students: a comparative study. Int J Nurs Stud. 2009;46(12):1541–1547. doi: 10.1016/j.ijnurstu.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Samaranayake CB, Fernando AT. Satisfaction with life and depression among medical students in Auckland, New Zealand. N Z Med J. 2011;124(1341):12–17. [PubMed] [Google Scholar]
- 6.Bugaj T, Cranz A, Junne F, Erschens R, Herzog W, Nikendei C. Psychosocial burden in medical students and specific prevention strategies. Mental Health Prev. 2016;4(1):24–30. doi: 10.1016/j.mhp.2015.12.003. [DOI] [Google Scholar]
- 7.Henning MA, Krägeloh C, Hawken SJ, Zhao Y, Doherty I. The quality of life of medical students studying in New Zealand: a comparison with non-medical students and a general population reference group. Teach Learn Med. 2012;24(4):334–340. doi: 10.1080/10401334.2012.715261. [DOI] [PubMed] [Google Scholar]
- 8.Moffat KJ, McConnachie A, Ross S, Morrison JM. First year medical student stress and coping in a problem-based learning medical curriculum. Med Educ. 2004;38(5):482–491. doi: 10.1046/j.1365-2929.2004.01814.x. [DOI] [PubMed] [Google Scholar]
- 9.The University of Auckland. Biomedical Common Year or Overlapping Year. 2015; http://www.science.auckland.ac.nz/en/about/our-programmes/op-biomed-common-year.html. Accessed 13 Feb 2015.
- 10.The University of Auckland. Entry requirements for Bachelor of Medicine and Bachelor of Surgery (MBChB). 2015; https://www.fmhs.auckland.ac.nz/en/faculty/for/future-undergraduates/undergraduate-study-options/mbchb/entry.html#6a24d5a2b8307836303d44e054d0adb1. Accessed 3 Jan 2016.
- 11.Henning MA, Krägeloh CU, Booth R, Hill EM, Chen J, Webster CS. Profiling potential medical students and exploring determinants of career choice. The Asia-Pacific Scholar. 2017;2(1):7–15. doi: 10.29060/TAPS.2017-2-1/OA1019. [DOI] [Google Scholar]
- 12.Health Workforce New Zealand. An assessment of the utility of graduate-entry medical education programmes for New Zealand. 2011; http://www.nzdoctor.co.nz/media/930253/graduate%20medical%20entry%20programme%20report%20final%203%20june.pdf. Accessed 24 Jan 2015.
- 13.Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 14.Wigfield A, Eccles JS. Expectancy–value theory of achievement motivation. Contemp Educ Psychol. 2000;25(1):68–81. doi: 10.1006/ceps.1999.1015. [DOI] [PubMed] [Google Scholar]
- 15.Wigfield A, Tonks S, Klauda SL. Expectancy-value theory. In: Wentzel K, Wigfield A, Miele D, editors. Handbook of motivation at school. 2. New York: Routledge; 2012. pp. 55–74. [Google Scholar]
- 16.Konu A, Rimpelä M. Well-being in schools: a conceptual model. Health Promot Int. 2002;17(1):79–87. doi: 10.1093/heapro/17.1.79. [DOI] [PubMed] [Google Scholar]
- 17.Baik C, Naylor R, Arkoudis S, Dabrowski A. Examining the experiences of first-year students with low tertiary admission scores in Australian universities. Stud High Educ. 2017:1–13.
- 18.Chester A, Burton LJ, Xenos S, Elgar K. Peer mentoring: supporting successful transition for first year undergraduate psychology students. Aust J Psychol. 2013;65(1):30–37. doi: 10.1111/ajpy.12006. [DOI] [Google Scholar]
- 19.Friedlander LJ, Reid GJ, Shupak N, Cribbie R. Social support, self-esteem, and stress as predictors of adjustment to university among first-year undergraduates. J Coll Stud Dev. 2007;48(3):259–274. doi: 10.1353/csd.2007.0024. [DOI] [Google Scholar]
- 20.Park CL, Adler NE. Coping style as a predictor of health and well-being across the first year of medical school. Health Psychol. 2003;22(6):627–631. doi: 10.1037/0278-6133.22.6.627. [DOI] [PubMed] [Google Scholar]
- 21.Aktekin M, Karaman T, Senol Y, Erdem S, Erengin H, Akaydin M. Anxiety, depression and stressful life events among medical students: a prospective study in Antalya, Turkey. Med Educ. 2001;35(1):12–17. doi: 10.1046/j.1365-2923.2001.00726.x. [DOI] [PubMed] [Google Scholar]
- 22.Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Acad Psychiatry. 2012;36(3):177–182. doi: 10.1176/appi.ap.11040079. [DOI] [PubMed] [Google Scholar]
- 23.Henning MA, Hawken SJ, Hill AG. The quality of life of New Zealand doctors and medical students: what can be done to avoid burnout? New Zealand Med J. 2009;122(1307):102–110. [PubMed] [Google Scholar]
- 24.Henning MA, Krägeloh CU, Booth R, Hill EM, Chen J, Webster CS. Biomedical students in their first year of study: factors explaining performance in a high stakes examination. Med Sci Educ. 2017;27(4):633–643. doi: 10.1007/s40670-017-0444-y. [DOI] [Google Scholar]
- 25.Mitchell C. Motivation changes in medical students during two years of the preclinical curriculum. Auckland, New Zealand: Faculty of Education, University of Auckland; 2015. [Google Scholar]
- 26.Kusurkar R, Ten Cate TJ, Van Asperen M, Croiset G. Motivation as an independent and a dependent variable in medical education: a review of the literature. Med Teach. 2011;33(5):e242–e262. doi: 10.3109/0142159X.2011.558539. [DOI] [PubMed] [Google Scholar]
- 27.Lonka K, Sharafi P, Karlgren K, Masiello I, Nieminen J, BirgegÅrd G, Josephson A. MED NORD-A tool for measuring medical students' well-being and study orientations. Med Teach. 2008;30(1):72–79. doi: 10.1080/01421590701769555. [DOI] [PubMed] [Google Scholar]
- 28.Niemi P, Vainiomäki P. Medical students' distress-quality, continuity and gender differences during a six-year medical programme. Med Teach. 2006;28(2):136–141. doi: 10.1080/01421590600607088. [DOI] [PubMed] [Google Scholar]
- 29.Henning MA, Krägeloh C, Hawken SJ, Doherty I, Zhao Y, Shulruf B. Motivation to learn, quality of life and estimated academic achievement: medical students studying in New Zealand. Med Sci Educ. 2011;21(2):142–150. doi: 10.1007/BF03341611. [DOI] [Google Scholar]
- 30.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. Jama. 2016;316(21):2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan DW. Depressive symptoms and depressed mood among Chinese medical students in Hong Kong. Compr Psychiatry. 1991;32(2):170–180. doi: 10.1016/0010-440X(91)90010-A. [DOI] [PubMed] [Google Scholar]
- 32.Diener E, Diener M, Diener C. Factors predicting the subjective well-being of nations. J Pers Soc Psychol. 1995;69(5):851–864. doi: 10.1037/0022-3514.69.5.851. [DOI] [PubMed] [Google Scholar]
- 33.Stankov L. Unforgiving Confucian culture: a breeding ground for high academic achievement, test anxiety and self-doubt? Learn Individ Differ. 2010;20(6):555–563. doi: 10.1016/j.lindif.2010.05.003. [DOI] [Google Scholar]
- 34.Auckland University of Technology. Psychology Major - Bachelor of Health Science 2018; http://www.aut.ac.nz/study-at-aut/study-areas/health-sciences/undergraduate-courses/bachelor-of-health-science-psychology. Accessed 1 Jun 2018.
- 35.West Chester University of Pennsylvania. Psychology (PSY): College of the Sciences and Mathematics 2018; http://catalog.wcupa.edu/general-information/index-course-prefix-guide/course-index/undergraduate/psy/. Accessed 1 Jun 2018.
- 36.The University of Hong Kong. Undergraduates Studies 2018; https://www.med.hku.hk/programme/mbbs-6yr. Accessed 1 Jun 2018.
- 37.Pintrich PR, De Groot EV. Motivational and self-regulated learning components of classroom academic performance. J Educ Psychol. 1990;82(1):33–40. doi: 10.1037/0022-0663.82.1.33. [DOI] [Google Scholar]
- 38.The WHOQOL Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi: 10.1017/S0033291798006667. [DOI] [PubMed] [Google Scholar]
- 39.Houston J, Harris P, McIntire S, Francis D. Revising the competitiveness index using factor analysis. Psychol Rep. 2002;90(1):31–34. doi: 10.2466/pr0.2002.90.1.31. [DOI] [PubMed] [Google Scholar]
- 40.Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.IBM SPSS Statistics. Release notes - IBM SPSS Statistics 24.0. 2015; https://www-304.ibm.com/support/docview.wss?uid=swg27047057. Accessed 1 Jun 2018.
- 42.Field AP. Discovering statistics using SPSS : and sex, drugs and rock’n’roll. 2. London: SAGE; 2005. [Google Scholar]
- 43.Goldman M. Statistics for bioinformatics. 2008. https://www.stat.berkeley.edu/~mgoldman/Section0402.pdf. Accessed 1 Jun 2018.
- 44.Nulty DD. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval High Educ. 2008;33(3):301–314. doi: 10.1080/02602930701293231. [DOI] [Google Scholar]
- 45.Sax LJ, Gilmartin SK, Bryant AN. Assessing response rates and nonresponse bias in web and paper surveys. Res High Educ. 2003;44(4):409–432. doi: 10.1023/A:1024232915870. [DOI] [Google Scholar]
- 46.Harris PB, Houston JM. A reliability analysis of the revised competitiveness index. Psychol Rep. 2010;106(3):870–874. doi: 10.2466/pr0.106.3.870-874. [DOI] [PubMed] [Google Scholar]
- 47.Henning MA, Krägeloh CU, Manalo E, Doherty I, Lamdin R, Hawken SJ. Medical students in early clinical training and achievement motivation: variations according to gender, enrolment status, and age. Med Sci Educ. 2013;23(1):6–15. doi: 10.1007/BF03341798. [DOI] [Google Scholar]
- 48.Lee W, Lee M-J, Bong M. Testing interest and self-efficacy as predictors of academic self-regulation and achievement. Contemp Educ Psychol. 2014;39(2):86–99. doi: 10.1016/j.cedpsych.2014.02.002. [DOI] [Google Scholar]
- 49.Træen B, Westerberg AC, Njøten MO, Røysamb E. Predictors of self-efficacy in Norwegian competition riders. J Equine Vet Sci. 2015;35(10):807–814. doi: 10.1016/j.jevs.2015.07.021. [DOI] [Google Scholar]
- 50.Dyrbye LN, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–149. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 51.Chen C, Lee S-Y, Stevenson HW. Response style and cross-cultural comparisons of rating scales among east Asian and north American students. Psychol Sci. 1995;6(3):170–175. doi: 10.1111/j.1467-9280.1995.tb00327.x. [DOI] [Google Scholar]
- 52.Harzing A-W. Response styles in cross-national survey research: a 26-country study. Int J Cross-cult Manag. 2006;6(2):243–266. doi: 10.1177/1470595806066332. [DOI] [Google Scholar]
- 53.Williams GC, Deci EL. The importance of supporting autonomy in medical education. Ann Intern Med. 1998;129(4):303–308. doi: 10.7326/0003-4819-129-4-199808150-00007. [DOI] [PubMed] [Google Scholar]
- 54.Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39(6):594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 55.Powis D. Improving the selection of medical students. In: British Medical Journal Publishing Group; 2010
- 56.Khan MA, Law LS. An integrative approach to curriculum development in higher education in the USA: a theoretical framework. Int Educ Stud. 2015;8(3):66–76. doi: 10.5539/ies.v8n3p66. [DOI] [Google Scholar]
- 57.Moir F, Fernando AT, III, Kumar S, Henning M, Moyes SA, Elley CR. Computer assisted learning for the mind (CALM): the mental health of medical students and their use of a self-help website. New Zealand Med J (Online) 2015;128(1411):51. [PubMed] [Google Scholar]
- 58.Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Med Care. 2007;45(7):594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- 59.El-Ghoroury NH, Galper DI, Sawaqdeh A, Bufka LF. Stress, coping, and barriers to wellness among psychology graduate students. Train Educ Prof Psychol. 2012;6(2):122–134. [Google Scholar]
- 60.Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress, burnout and coping strategies in preclinical medical students. N Am J Med Sci. 2016;8(2):75–81. doi: 10.4103/1947-2714.177299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ayala EE, Winseman JS, Johnsen RD, Mason HR. US medical students who engage in self-care report less stress and higher quality of life. BMC Med Educ. 2018;18(1):189. doi: 10.1186/s12909-018-1296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baruch Y. Response rate in academic studies-a comparative analysis. Hum Relat. 1999;52(4):421–438. [Google Scholar]
- 63.Furnham A. Response bias, social desirability and dissimulation. Personal Individ Differ. 1986;7(3):385–400. doi: 10.1016/0191-8869(86)90014-0. [DOI] [Google Scholar]