Abstract
Introduction
Ultrasound (US) imaging has rapidly increased its application in almost every medical field. Many universities worldwide provide teaching of US for undergraduates in their curricula. Emerging evidence is supporting the use of ultrasonography to improve also non-US skills and knowledge of medical students.
Objectives
The purpose of this review is to understand if the integration of US lessons into medical students’ curriculum improves their learning of physical examination and enhances their skills when performing it.
Methods
We performed a systematic review of literature by searching three electronic medical databases. We included studies of any level of evidence published in peer-reviewed journals. Evaluated data were extracted using the PICO framework and critically analyzed. PRISMA guidelines were applied; we excluded all the articles evaluated with serious risk of bias and/or low methodological quality.
Results
We included 15 articles, accounting for more than 1643 medical students involved from five different countries and 14 various academical institutions. Eight out of nine studies (88.9%) reported an improvement of practical physical examination scores by students exposed to ultrasound lectures. Eleven out of eleven studies (100%), which administered self-assessment questionnaires, reported strong agreement among students that ultrasound lectures helped them learning and understanding the physical exam and improved their confidence and skills.
Conclusions
Increasing evidence shows that incorporating ultrasound in medical students’ curriculum might improve their ability and confidence when learning and performing a physical exam. This significant tendency needs to be corroborated at a deeper level by further studies.
Electronic supplementary material
The online version of this article (10.1007/s40670-020-00921-4) contains supplementary material, which is available to authorized users.
Keywords: medical education, Undergraduates, Physical exam, ultrasound
Introduction
Since its first diffusion, ultrasound imaging has rapidly increased its application in almost every medical field [1, 2]. Its contribution to the improvement of diagnosis’ efficiency radically changed medical practice, due to its affordability, reliability, and practicality [1, 2]. Thanks to these characteristics, ultrasonography has been used as a diagnostic and interventional tool over the past 20 years [2], handily executed and interpreted by clinicians at the bedside, with and even without the intervention of a radiologist [2]. This practice, called point-of-care ultrasonography [2], has been deeply introduced into physical examination routine, and most authors claim that physicians shortly will consider ultrasound as an “extension of their senses,” like the stethoscope [3].
Despite its possible even wider diffusion, ultrasound imaging today is part of the everyday clinician job. Thus, it needs a significant implementation of its teaching in undergraduate medical education [3, 4]. Moreover, one of the critical aspects of ultrasound is that it mostly relies on user skills, which underlines why it is a primary need to train future doctors to manage this tool effectively [3]. Many medical schools worldwide implemented teaching of ultrasound for medical students [5–7]; nevertheless, there is still no agreement on when and how this should be inserted into the course of study [8].
Different instructional methods have been used [4], including traditional teaching, featured by lessons, videos, and web-based lectures [9], combined with a practical session through the scanning of peers [10], patients [9, 11] or the use of simulators [11]. Also, whereas a curriculum implementation is still relatively uncommon, most medical schools have introduced ultrasonography education as an elective course, mostly related to the teaching of anatomy [12–14]. Among all this heterogeneity, emerging evidence supports a focus on practice-based learning to improve technical skills [15, 16].
Since the use of ultrasound has spread so much both in the clinical setting and, slowly, also in medical students’ curricula [17], it is interesting to analyze the actual influence of ultrasound on the students’ clinical skills.
Beside its integration, many studies already investigated the improvement of physical examination in students who had learned and mastered ultrasonography at a university [17, 18], underlining the fulfillment of undergraduate students who took part in those programs [19]. Ultrasound has also been used as a guidance of procedures, and it has been enhanced improved practicality among medical students who used point-of-care ultrasound guidance in the placement of intravenous catheters [20, 21].
Emerging evidence is supporting the use of ultrasounds to improve not only US abilities but also non-US skills such as anatomy knowledge and physical examination proficiency of medical students [17]. This method resulted, on medical students’ performance, as effective as cadaver dissections or endoscopy [17, 22, 23], and the same achievement was reached when the lessons were taken by either anatomists or near-peer educators like residents of fourth-year [24].
The literature up to now already highlighted how the use of ultrasonography helped students to be more accurate in the comprehension of human anatomy and more confident in performing precise physical examinations. Moreover, it suggested that preparing medical students for this procedure could result in a better health care offer. Therefore, the benefits are both into the improvement of the student’s knowledge about visiting the patient and into the possibility to have always more professionals able to perform a bedside procedure at the best of their capacity, regardless of their specialty. Nonetheless, a recent systematic review underlined the absence of actual evidence to support a deeper integration of ultrasound in a university’s curricula [25].
Our systematic review aims to report the most up-to-date evidence on the effects of ultrasonography implementation on physical examination skills in medical education.
Methods
Literature Search Strategy
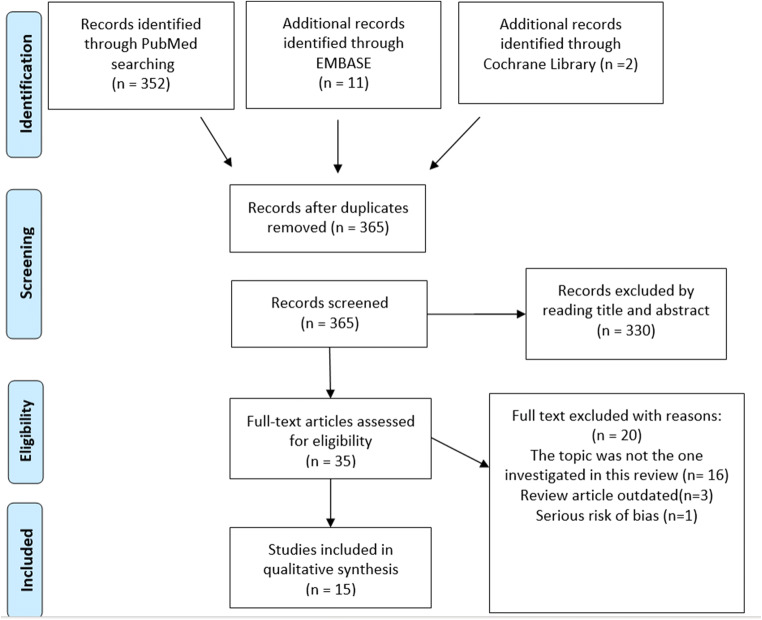
We conducted this systematic review according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [26]. A comprehensive search was performed on three electronic medical databases (PubMed, Embase, and Cochrane Library) by two independent authors (V.O. and M.F.) from their inception on the 10th of July 2019. Our main aims were: (1) to understand ultrasound lessons influence on clinical examination skills learning and development, (2) to identify how this can be implemented in a medical school curriculum, and (3) to evaluate the self-reported perception of medical students involved. To achieve the maximum sensitivity of the search strategy, we combined these terms: (ultrasonography or sonography) and (Education, Medical, Undergraduate) or (medical students) and (Physical Examination) or (physical exam) as either keywords or mesh terms. The reference lists of all included articles, previous literature reviews on the topic and top hits from Google Scholar were reviewed for further identification of potentially relevant studies. To avoid overlapping with other ongoing reviews, we first searched on PROSPERO site for any similar review (Fig. 1).
Fig. 1.
Prisma flowchart of the included studies
Selection Criteria
Eligible studies for our systematic review included those investigating the effects of ultrasonography training sessions on physical examination skills and confidence of undergraduates. Primary screening of the titles and abstracts was performed by adding studies of any level of evidence published in peer-reviewed journals written in English. The use of US not only for training but also during the physical exam practical assessment was our exclusion criteria. Additionally, we excluded studies in which data were not accessible, missing, without an available full text, or not well reported. Duplicates, abstracts, case reports, conference presentations, reviews, editorials, and expert opinions were excluded. Two authors (V.O. and F.M.) performed the search and evaluated the articles independently. An experienced researcher in systematic reviews (E.C.) solved cases of doubt. At the beginning of the procedure, each investigator reads the abstracts of all the articles, selected the relevant ones according to both inclusion and exclusion criteria, and then compared the results with the other investigators. After 4 weeks, the same studies were reread to establish the agreement of the investigators about articles’ selection. No disagreement was observed among the investigators. One investigator extracted the data from the full-text articles to Excel spreadsheet structured tables to analyze each study descriptively. Another investigator independently double-checked the extraction of primary data from all the articles. Doubts and inconsistencies were grouped and solved.
Data Extraction and Criteria Appraisal
All data were extracted from article text, tables, and figures. Data were extracted using the Population, Intervention, Comparison, Outcome (PICO) framework and included title, year of publication, study design, sample size, study population, students’ characteristics, intervention and comparator (where applicable), outcomes, funding, and conclusions. Two investigators independently reviewed each article (V.O. and F.M.). Discrepancies between the two reviewers were resolved by discussion and consensus. The final results were reviewed by the senior investigator (E.C.).
Risk of Bias Assessment
Risk of bias assessment of full-text of all the studies selected was performed according to the ROBINS risk of bias tool [27] for non-randomized trials and the Cochrane Collaboration’s risk of bias tool [27] for randomized trials. This assessment used the following judgment keys: “low” indicated a low risk of bias, “moderate” suggested that the risk of bias was moderate, and “high” showed a high risk of bias. Two authors performed the assessment (F.O. and G.G.) independently. Inter-rater agreement was 92%. Any discrepancy was discussed and solved with the senior investigator (E.C.). Table 1S in online resource 1 outlines the risk of bias assessment.
Table 1.
Main characteristics of the included studies
| Author (Year) |
Country of origin | Number of subjects |
Control group |
Questionnaire | Physical exam involved |
Findings |
|---|---|---|---|---|---|---|
|
Afonso et al. (2010) |
US |
307 (II year) |
no | yes | Generic physical examination | Physical exam. Skills↑ |
|
Ahn et al. (2015) |
US |
150 (II year) |
yes | yes | Palpation of the femoral pulse and estimation of the location of the femoral vein |
US > notUS Self-confidence↑ |
|
Barloon et al. (1998) |
US |
46 (II year) |
yes | no | Measurement of liver span | US > notUS |
|
Butter et al. (2007) |
US |
170 (I year) |
yes | yes |
Abdominal examination Liver measurement |
DelayedUS > immediateUS Physical exam. Confidence↑ DelayedUS ≈ immediateUS |
|
Dinh et al. (2015) |
US |
301 (I year) |
yes | yes | OSCE assessment |
US > notUS Physical exam. Skills↑ |
|
Fodor et al. (2012) |
Romania |
104 (III year) |
yes | yes |
Thyroid palpation Lung percussion and liver size estimation by palpation-percussion. |
US ≈ notUS US > notUS Physical exam. Skills↑/≈a |
|
Hoppmann et al. (2011) |
US |
not declared (I, II, III, IV year) |
no | yes | Generic physical examination | Physical exam. Skills↑ |
|
Hoppmann et al. (2015) |
US |
not declared (I, II, III, IV year) |
no | yes | Generic physical examination | Physical exam. Skills↑ |
|
Jamniczky et al. (2015) |
Canada |
137 (I year) |
no | yes | Generic physical examination | Physical exam. Skills↑ |
|
Legget et al. (2018) |
New Zealand |
8 (V, VI year) |
yes | no | Auscultation of heart murmurs | US ≈/> notUS |
|
Liu et al. (2019) |
US |
68 (I, II year) |
yes | yes | OSCE assessment |
US > notUS Physical exam. Confidence↑ |
|
Parikh et al. (2018) |
US |
93 (II year) |
no | yes | Female pelvic examination and testicular examination | Physical exam skills↑ |
|
Rempell et al. (2016) |
US |
38 (II year) |
no | yes | Generic physical examination | Physical exam skills↑ |
|
Sweetman et al. (2013) |
Australia |
194 (I, II year) |
yes | no | Gastro-intestinal tract examination | US < notUS |
|
Walrod et al. (2018) |
US |
27 (I year) |
yes | no | Palpation of knee and shoulder | US ≈ notUS |
US - Ultrasound training; Exam. – Examination; ↑ - Improvement; > − Better results than; < − Worst results than; ≈ − Similar results
a- depends on the physical exam involved: self-reported confidence in clinical skills showed a statistically significant increase in the US group only for thyroid palpation and liver size estimation
Study Quality Assessment
The research methodology quality assessment was completed as a “yes/no” response to eight questions focusing on study objectives, study design, randomization, reporting of participant characteristics, and description of the intervention. The reporting quality assessment included six items: description of underpinning theoretical models, description of the assessment process, the educational context, psychometric details, provision of materials allowing replication, and the strength of the conclusions drawn. The first five of these items were scored on a three-point Likert scale, with the last item strength of findings, scored against a five-point Likert scale. The impacts of the interventions were classified following Kirkpatrick’s adapted hierarchy [28], in line with guidance provided by BEME [29]. A descriptive synthesis of all included studies was completed, summarizing key findings, with an assessment of quality indicators as listed above. Data were extracted, for each study, into a piloted, non-standardized data-table for accuracy and completeness. Extraction included subheadings from the Best Evidence Medical Education (BEME) Quality, Utility, Extent, Strength, Target, Setting of evidence (QUESTS) acronym [19]. The strength of the retrieved evidence was graded using the power of evidence for BEME [20].
•Grade 1; No definite conclusions can be drawn. Not significant.
•Grade 2; Results ambiguous, but there appears to be a trend.
•Grade 3; Conclusions can probably be based on the results.
•Grade 4; Results are precise and very likely to be true.
•Grade 5; Results are unequivocal.
The assessment was performed by two authors (F.O. and G.G.) independently. Inter-rater agreement was 94%. Any discrepancy was discussed and solved with the senior investigator (E.C.). Table 2S in online resource 1 outlines the quality assessment.
Results
Study Characteristics
We identified 15 studies [9, 30–43], which evaluated the impact of ultrasound lectures and hands-on sessions on physical examination skills and confidence of medical students. They account for a total of more than 1643 participants, medical students attending 14 different institutions of five different countries, of which the most represented are the USA.
Several studies focused their outcomes on the physical examination of a particular human system, or an organ within cardiovascular system [35, 37, 39], endocrine system [31], digestive system [30, 31, 39–41], musculoskeletal system [36], reproductive system [32], and respiratory system [31]. Other studies used a more comprehensive outcome, like the OSCE assessment [33, 38], whereas some other studies generically investigated physical exam [9, 34, 42, 43] through surveys. Overall the studies evaluated many of the various aspects of necessary physical examination.
In only four studies [9, 36, 39, 42], the students involved had prior ultrasound exposure on the subject evaluated.
Long-term interventions, such as integration of a longitudinal ultrasound module in traditional curricula, were evaluated by seven studies [9, 33, 34, 38, 39, 42, 43]. Short-term interventions, like workshops or intensive lectures, were assessed by eight studies [30–32, 35–37, 40, 41].
Nine studies [30, 31, 33, 35–38, 40, 41] used a control group, and the assignment of students to intervention or control group was randomized except for one study [30]. The remaining were post-intervention survey studies.
The studies included were categorized by the type of outcome reported. In five studies [32, 34, 39, 42, 43], the results were extracted exclusively from self-assessment surveys. Three studies [36, 37, 41] used only practical evaluation. Five studies [31, 33, 35, 38, 40] got the results from both questionnaire and practical examination.
A summary of the study characteristics is available in Table 1.
Ultrasound Training and Improvement in Palpation Skills
Three studies [31, 35, 36] focused their outcomes on the effects of ultrasonography lessons on the palpation skills of students.
Ahn et al. [35] reported that 71 students, who underwent a short-term US training, were more accurate in recognizing the femoral pulse when compared to the 79 students of the control group (distance from the femoral artery in cm, mean 0.46 ± 0.71, CON 1.26 ± 2.06, P = .02).
In the paper by Fodor et al. [31], no statistically significant differences (P > .05) were found between two groups of 52 students, of which one underwent short-term ultrasound lessons, in measuring thyroid diameters using palpation. These two studies were evaluated as high quality and low risk of bias.
Walrod et al. [36] randomized 27 students in two groups, receiving short-term, hands-on ultrasound sessions respectively on knee and shoulder anatomy, and each one serving as a control group for the other. The shoulder group performed significantly better in the palpation of the shoulder (performance assessment in %, mean 63.0 ± 21.5, CON 40.2 ± 28.3, P = .03), especially in the palpation of the long head of the biceps tendon (performance assessment in %, mean 63.5 ± 28.7, CON 28.8 ± 35.8, P = .01), and in the overall evaluation for both joints (performance assessment in %, mean 71.6 ± 13.0, CON 56.1 ± 13.1, P = .01). This study was evaluated as medium quality and moderate risk of bias.
Overall, also considering their quality and risk of bias, these three studies tend to demonstrate that ultrasound training could have positive implications for the palpation skills of undergraduates, but the degree of improvement could be different or also non-statistically significant concerning the human system investigated through the physical exam.
US Influence on Abdominal/Gastrointestinal Tract Examination
Two studies [30, 40] analyzed how the competence of students in conducting a complete abdominal/GI tract examination was affected by short-term, hands-on ultrasound lessons.
Butter et al. [40] measured the students’ skills with a clinical skills assessment (CSA) checklist at two different times. They randomized 176 students in two groups: one received US training before the first CSA, the other received US training after the first CSA. At CSA-1, no statistically significant differences between the scores of the two groups were noted. At CSA-2, the group who received the delayed US training outperformed the other group scores and showed a higher degree of improvement from CSA-1 (CSA scores, immediate vs. delayed US, mean 7.28 ± 0.88, CON 7.66 ± 0.68, P = .0001). This study was assessed as high quality and low risk of bias.
Sweetman et al. [30] used multiple station assessment task (MSAT) scores, a type of clinical assessment similar to OSCE, and confronted the scores of a cohort of 98 students instructed with US with a retrospective control group of 96 students that did not receive US training. The performance of the US group compared to the non-US group was slightly inferior but statistically significant (MSAT scores, mean 1.02 ± 0.144, CON 1.07 ± 0.099, P = 0.004). This study was evaluated as medium quality, whereas the risk of bias was not clear due to some missing information.
Overall the two studies showed conflicting results, but considering its high quality and low risk of bias, the findings of the first study presented could have more importance than the second one, indicating that US could improve the abdominal examination skills of medical students.
US Training Effects on Students’ OSCE Scores
The use of US in medical education has also been studied as an implementation of the students’ ability in physical examination through the objective structured clinical examination (OSCE) assessment [33, 38].
Dinh et al. [33], which compared the skills of 163 students with previous US training with those of 138 students of the previous year with no US exposure, showed a statistically significant difference (P < .05) between the post-US and the pre-US group OSCE scores: in the first one, a major number of students obtained the higher ratings, while very few students received a negative evaluation. That difference was emphatic in the following items: blood pressure examination, abdominal examination, and professionalism. This study was evaluated as a moderate risk of bias and high quality.
Liu et al. [38] selected two groups of 34 students each: one receiving additional US lessons and tutoring, one following the standard program, and working as a control group.
The comparison, which analyzed both short and long-term improvement of the students’ abilities, showed significantly (P < .05) higher OSCE scores in the study group than the control group. This study showed high quality and low risk of bias.
Overall, also considering the quality and risk of bias of the studies analyzed, US training seems to have a great positive influence on OSCE scores of students.
US Enhancement of Liver Size Estimation
Three studies were interested in liver size estimation [40, 41, 44]. Butter et al. [40] examined the accuracy of 170 students in assessing the liver size after attending US training (n = 82) or not (n = 88). The results showed no significant differences in the accuracy of estimations between the two groups.
Barloon et al. [41] randomized 46 students into a control group who received only lecture and practice sessions (n = 27), and a study group who also received sonography training of liver examination (n = 19). The results showed a significant superiority of the sonography group in liver span measurements, consistently closer to the reference standard (p < .001).
In the last study, by Fodor et al. [44], the intervention group received US training, in addition to traditional instructions in palpation and percussion of the liver (n = 52),while the control group received only general instructions (n = 52). The authors found no significant differences between the two groups in liver superior limit identification. However, the inferior liver limit has been correctly identified consistently more often in the US group (p < .0001). Also, more students of the US group correctly identified both liver limits (p < .00001).
Regarding the quality of the studies, they have been assessed as low risk of bias, except the second one, which has been evaluated as moderate, and they have been all assessed as high quality. Considering the quality of the studies and the findings reported, it is shown that US training can be beneficial to upgrade the students’ ability in liver size estimation; little differences or non-statistically significant results could be revealed considering the part of the liver examined and the timing of introduction of the US training concerning the traditional lessons schedule.
Effects of US on Heart Auscultation and Lung Percussion
Legget et al. [37] analyzed the combined use of US and a digital stethoscope in order to find an improvement in the students’ cardiac auscultation skills. The study involved eight students, randomly divided into a control group, who received training with a standard acoustic stethoscope, and an intervention group, who received US and digital stethoscope training. The results only showed a significant mean score improvement between two sequential assessment in the intervention group (p = .027).
Fodor et al. [44] focused on lung percussion to assess the students’ skills in identifying the inferior limit of the lung. The identification has been performed by percussion along three lines: parasternal, mid-clavicular, and anterior axillary. A higher percentage of students from the group who received US training correctly identified the 3 points considered, compared with the group who did not received the training (p = .0028 along the anterior axillary lines; p = .0237 along the parasternal and the anterior axillary lines; p = .0374 along the mid-clavicular and the anterior axillary lines).
The first study has been assessed as a moderate risk of bias and high quality, while the second one has been evaluated as low risk of bias and high quality.
Overall, pondering both the results and the quality of the two studies, US could be a favorable tool to enhance the students’ lung percussion skills, whereas its effect on heart auscultation is still unclear.
Evidence and Students’ Perceptions from Self-Assessment Questionnaires
In ten studies [9, 31–35, 38–40, 42, 43], a questionnaire was administered to students who underwent US training to collect and analyze their opinions about the influence of the US lessons on their physical examination skills and confidence.
From the survey by Liu et al. [38] emerged that 34 students indicated that the POCUS pilot curriculum provided them more comfort when performing physical examination and an earlier clinical exposure.
Ahn et al. [35] showed that the students’ self-confidence in identifying the femoral artery and vein increased in a statistically significant way after their exposure to US lessons (P < .001 for the artery and P = .01 for the vein, n = 50).
For 163 students in the study by Dinh et al. [33], US exposure through a long-term curriculum integration improved their physical examination, considering it as a valuable tool important for their medical education, and that can benefit their future practice.
Fodor et al. [31] also found that students had different perceptions about the utility of US lessons in regard to the physical exam involved: the % of students who considered that US lessons improved their physical examination skills was 96% (n = 52) for thyroid palpation, 60% (n = 52) for lung percussion, and 81% (n = 52) for liver size estimation; self-reported confidence in clinical skills showed statistically significant increase in favor of the US group only for thyroid palpation and liver size estimation.
Butter et al. [40] demonstrated that, after exposure to US hands-on sessions, all students (n = 176) showed increased confidence in performing abdominal examination (P = .0001).
The studies mentioned above were all evaluated as high quality and low [31, 35, 38, 40] or moderate [33] risk of bias.
Hoppmann et al. [9, 42] showed that at both 4 and 9 years since the introduction of an integrated US curriculum in medical school, over 90% of the students (response rate over 90%) said that the US curriculum implementation improved their understanding of anatomy and physical exam, with tangible benefit to their their professional education.
In the study by Parikh et al. [32], the evaluation of 93 students after US demonstrations showed a statistically significant increase of confidence in their ability to palpate the ovary, uterus and, epididymis and a statistically significant decrease in the anxiety about conducting a testicular and bimanual pelvic examination; all of the students highly agreed that US lessons improved their understanding and skills of reproductive system examination.
The 88% of 38 students in the study by Rempell et al. [43] agreed or strongly agreed that the integration of US lectures and hands-on sessions in their medical school curriculum allowed them to learn the physical examination more effectively and that this integration enhanced their confidence in physical examination skills.
After US lessons and hands-on sessions, it was reported by Afonso et al. [39] that 78% of 307 students valued the US as an essential part of the physical diagnosis course.
Jamniczky et al. [34] found that 137 students considered US useful for learning physical examination skills (mean 4.4 ± 0.8, where one = very useless and 5 = very useful); furthermore, cognitive load imposed by “knobology” was inversely associated with perceived utility for learning physical examination (P = .03).
The studies above mentioned were assessed as medium quality and low [39] or moderate [9, 32, 34, 42, 43] risk of bias.
Overall, bearing in mind the quality and risk of bias of the studies, it strongly emerged from the surveys that ultrasound integration during medical school is highly appreciated by students, who felt that US training enhanced their physical examination skills and confidence. Some significant differences could affect the degree of appreciation concerning the type of physical examination involved and to the cognitive load imposed by the knowledge of basic ultrasound technique.
Discussion
From the analysis of the 15 studies included in our systematic review, we identified a concord trend, common to almost all the studies: US integration into medical undergraduates’ curriculum, either in a short or long-term intervention, seems to improve their physical examination skills and their confidence when performing a physical exam. We discovered that US exposure is highly satisfying among students, and it is associated with concrete learning and practical benefits concerning physical examination abilities. A possible explanation to this findings might be given by the immediate feedback that the US image provides to the student, who can match the position of internal organs on the body surface in real-time and know if he/she is examining the patient in the right manner, improving his/her physical examination accuracy and understanding, especially for palpation and percussion [30, 32, 34, 38, 41, 44]. Only one study out of 15 reported a slightly negative outcome of US training on physical examination skills of students, justified by the authors with the too short length of the US training, that could have provided the students with over-confidence without increasing their real abilities. This finding was suspected by the other two studies [40, 44]. This result stresses an important point that needs to be highlighted by future research: if the best way to introduce medical students to US is either a short or long-term intervention, providing a better understanding of the pros and cons of both kinds of intervention.
Another issue pointed out by Butter et al. [40] and confirmed by Fodor et al. [44] was that students’ exposure to US training before they had traditional practical physical examination training was unsuccessful, by contrast, the same exposure after the traditional practical training significantly improved their skills; these data suggest that a student must reach a minimum level of competence in practical physical examination to benefit from a US training on the subject and upgrade his/her skills. Future investigations, comparing the performances of the students’ groups that received US training before or after traditional physical examination lessons, are required to establish this evidence.
We also discovered that US effectiveness, proved by practical assessments or perceived by students, varies with the type of physical exam involved and the cognitive load imposed by US technique. As regards to the palpation of the thyroid [44], the authors addressed the non-statistically significance of the differences between the two groups studied to the competitive mood that the experiment created and that led both groups to perform the test with more attention. The musculoskeletal physical exam, [36] revealed that US could have little benefit for palpation of bony landmarks [36], probably because they are just easy to identify with basic anatomy knowledge, whereas it could have a role on the palpation of soft tissues [36]. Further work is needed to confirm that US training has different outcomes depending on the anatomy involved; some discriminant factors might be: the superficiality and the consistency of the organ/tissue examined, the easiness to explore the organ/tissue with traditional physical examination instructions only, the better visualization of some organ/tissue with US, and the relative difficulty of US technique depending on the organ/tissue examined. Jamniczky et al. [34] found that the cognitive load imposed by basic ultrasound knobology (the functionality of US machines controls) negatively affected students’ perceptions on the utility of US for learning physical examination but not for learning anatomy. This could mean that if we want to use US to enhance physical examination skills of students, which, in comparison to anatomy learning, are dynamic tasks that demands a different cognitive load; we should first instruct the students based on US knobology to avoid an excessive cognitive amount that would impede the students to process correctly the new information learned through the lecture. Further researches are required to assess these components of the learning scenario.
State of the Art on the Subject
Our research topic was mentioned by other two past systematic reviews [25, 45] as part of a more comprehensive analysis on various outcomes of US on medical education. Their results reported an inconclusive role for US due to limited evidence. Accordingly to these findings, we discovered that the evidence for every single type of physical inspection of the various human systems or organs is still inadequate and relies on a limited number of studies; on the other hand, all these studies, collected together, showed a mild trend, demonstrating that US has a positive influence on physical examination skills of medical students. We highly encourage further randomized trial with a focus on specific anatomic district in order to clarify the US role. Our systematic review corroborates the positive results of other past reviews [8, 17, 46, 47] about non-US related outcomes such as physical examination improved skills or anatomy improved learning.
Implications and Possible Practical Applications
Point-of-care US is used to confirm or refuse a focused question made by the physician in real-time, and, despite comprehensive screening scans, it may promote critical and clinical thinking because its application is based on assumptions made by the traditional clinical skills of the physician [33].
US is not an essential medical skill today, and probably it will not be even in the future. However, it can be a useful tool in everyday practice and also in the experience of a medical student. Bearing in mind its possible wider future implementation in the medical curriculum [39], we underline how, based on available evidence, physical examination teaching may not need US enhancement to reach high quality, even though we recognize its several benefits.
If someone thinks that US implementation may negatively affect critical thinking and tactile skills of students, relying too much on technology, it is to bear in mind that US is not intended to replace physical examination or anatomy teaching, but as an adjuvant to enhance the traditional way of teaching and learning through a synergic strategy to build a well-rounded curriculum [35].
The integration of US into medical school faces some challenges [43]. Costs, teachers’ availability, and time needed are the more significant obstacles. Nonetheless, some authors demonstrated that a curriculum could be improved feasibly and with minimal resources [33, 38, 43, 48]; a lot can also be learned from pilot US long-term integrations [9, 42].
US is a technique that requires time to be learned and mastered: early exposure during medical years might allow students to practice, being prepared, and advantaged during residency [33] and for their future work as physicians.
Given the results of this and other reviews and articles on US utility to strengthen US related and non-US related skills of students, US appears to be a viable tool for medical education because, with a single intervention, students can achieve multiple favorable outcomes. Learn the basics of medical US, accordingly to the increasing use of US in almost every medical field [49] and reaching the necessary milestones [6] of US learning can have future benefit that go over the follow up of the studies described and should be pursued. [33].
Strengths and Limitations
One limitation to our study is that four out of the 15 included studies [9, 36, 39, 42]; the students involved had previous US exposure on the subject evaluated by the study. Of these only one appraised the effectiveness of US on physical examination skills of students with a practical assessment before the intervention. An additional limitation is that, except for the study by Legget et al. [37], the students practiced and improved their physical examination skills on normal anatomy; further studies are needed to assess this evidence also on pathological scenarios.
Our review conformed to the PRISMA guidelines, and all studies included were assessed for their quality and risk of bias; moreover, to our knowledge, this is the first systematic review focused exclusively on this particular topic with the highest number of studies evaluated.
Conclusions and Significance of this Work
Although the real and full value of US teaching during medical school still needs clarification, great benefits emerge from an increasing number of literature studies on various utilities that US can have for medical education. We noticed that US training could be useful to improve medical students’ physical examination skills, confidence, and competence. Big decisions like that of integrating US in the medical students’ curriculum need to be supported by a large volume of substantial evidence, and this review wants to shine a light on a little piece of this bigger picture. Supplementary studies are needed to clarify the unsettled points that emerged within our review and to determine the combination of teaching strategies that optimizes learning.
Electronic supplementary material
(DOCX 19 kb)
Acknowledgments
We thank the contribution of the Medical Student Research Academy (MSRA) in supporting this project with lessons about research methodology and manuscript preparation. Without its network and support, this project would not have seen the end.
Funding
No funding was used for this study.
Compliance with Ethical Standards
Conflict of Interest
All the authors have nothing to disclose for this study.
Ethical Approval
N/A
Informed Consent
N/A
Footnotes
Author Contribution
Emanuele Chisari: Study concept and design, Analysis and interpretation of the data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Administrative, technical, or material support, Study supervision
Vittorio Oteri: Study concept and design, Analysis and interpretation of the data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Administrative, technical, or material support, Study supervision
Federica Occhipinti: Study concept and design, Acquisition of the data, Analysis and interpretation of the data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content
Giorgia Gribaudo: Acquisition of the data, Analysis and interpretation of the data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content
Francesco Marastoni: Acquisition of the data, Analysis and interpretation of the data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoppmann R, Blaivas M, Elbarbary M. Better medical education and health care through point-of-care ultrasound. Acad Med. 2012;87:134. doi: 10.1097/ACM.0b013e31823f0e8f. [DOI] [PubMed] [Google Scholar]
- 2.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 3.Solomon SD, Saldana F. Point-of-care ultrasound in medical education — stop listening and look. N Engl J Med. 2014;370:1083–1085. doi: 10.1056/NEJMp1311944. [DOI] [PubMed] [Google Scholar]
- 4.Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. Ultrasound curricula in undergraduate medical education: A scoping review. J Ultrasound Med. 2018;37:69–82. doi: 10.1002/jum.14333. [DOI] [PubMed] [Google Scholar]
- 5.Dinh VA, Fu JY, Lu S, Chiem A, Fox JC, Blaivas M. Integration of ultrasound in medical education at United States medical schools: A national survey of directors’ experiences. J Ultrasound Med. American Institute of Ultrasound in Medicine. 2016;35:413–419. doi: 10.7863/ultra.15.05073. [DOI] [PubMed] [Google Scholar]
- 6.Dinh VA, Lakoff D, Hess J, Bahner DP, Hoppmann R, Blaivas M, et al. Medical student core clinical ultrasound milestones: A consensus among directors in the United States. J Ultrasound Med [Internet]. 2016 [cited 2019 Aug 11];35:421–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26782162. [DOI] [PubMed]
- 7.Lane N, Lahham S, Joseph L, Bahner DP, Fox JC. Ultrasound in medical education: listening to the echoes of the past to shape a vision for the future. Eur J Trauma Emerg Surg. 2015;41:461–467. doi: 10.1007/s00068-015-0535-7. [DOI] [PubMed] [Google Scholar]
- 8.Patel SG, Benninger B, Mirjalili SA. Integrating ultrasound into modern medical curricula [Internet]. Clin. Anat. 2017 [cited 2019 Aug 11]. p. 452–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28247975. [DOI] [PubMed]
- 9.Hoppmann RA, Rao V V, Poston MB, Howe DB, Hunt PS, Fowler SD, et al. An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience [Internet]. Crit. Ultrasound J. springer; 2011 [cited 2019 Jun 7]. p. 1–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21516137. [DOI] [PMC free article] [PubMed]
- 10.Knobe M, Münker R, Sellei RM, Holschen M, Mooij SC, Schmidt-Rohlfing B, et al. Peer teaching: A randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44:148–55. [DOI] [PubMed]
- 11.Cawthorn TR, Nickel C, O’Reilly M, Kafka H, Tam JW, Jackson LC, et al. Development and evaluation of methodologies for teaching focused cardiac ultrasound skills to medical students. J Am Soc Echocardiogr. 2014;27:302–309. doi: 10.1016/j.echo.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Wittich CM, Montgomery SC, Neben MA, Palmer BA, Callahan MJ, Seward JB, et al. Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. JAMA. 2002;288:1062–3. [DOI] [PubMed]
- 13.Brown B, Adhikari S, Marx J, Lander L, Todd GL. Introduction of ultrasound into gross anatomy curriculum: perceptions of medical students. J Emerg Med. 2012;43:1098–1102. doi: 10.1016/j.jemermed.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 14.Prats MI, Royall NA, Panchal AR, Way DP, Bahner DP. Outcomes of an advanced ultrasound elective: preparing medical students for residency and practice. J Ultrasound Med. 2016;35:975–982. doi: 10.7863/ultra.15.06060. [DOI] [PubMed] [Google Scholar]
- 15.Florescu CC, Mullen JA, Nguyen VM, Sanders BE, Vu PQP. Evaluating didactic methods for training medical students in the use of bedside ultrasound for clinical practice at a faculty of medicine in Romania. J Ultrasound Med. 2015. p. 1873–82. [DOI] [PubMed]
- 16.Cuca C, Scheiermann P, Hempel D, Via G, Seibel A, Barth M, et al. Assessment of a new E-learning system on thorax, trachea, and lung Ultrasound. Emerg Med Int. 2013;2013:1–10. doi: 10.1155/2013/145361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis [Internet]. Anat. Sci. Educ. 2017 [cited 2019 Aug 11]. p. 176–89. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27286419. [DOI] [PubMed]
- 18.Dinh VA, Dukes WS, Prigge J, Avila M. Ultrasound integration in undergraduate medical education: comparison of ultrasound proficiency between trained and untrained medical students. J Ultrasound Med. 2015;34:1819–1824. doi: 10.7863/ultra.14.12045. [DOI] [PubMed] [Google Scholar]
- 19.Dickerson J, Paul K, Vila P, Whiticar R. The role for peer-assisted ultrasound teaching in medical school. Clin Teach. 2017;14:170–174. doi: 10.1111/tct.12541. [DOI] [PubMed] [Google Scholar]
- 20.Griswold-Theodorson S, Hannan H, Handly N, Pugh B, Fojtik J, Saks M, et al. Improving patient safety with ultrasonography guidance during internal jugular central venous catheter placement by novice practitioners. Simul Healthc. 2009;4:212–216. doi: 10.1097/SIH.0b013e3181b1b837. [DOI] [PubMed] [Google Scholar]
- 21.Osborn SR, Borhart J, Antonis MS. Medical students benefit from the use of ultrasound when learning peripheral IV techniques. Crit Ultrasound J. 2012;4:2. doi: 10.1186/2036-7902-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLachlan JC. New path for teaching anatomy: Living anatomy and medical imaging vs. dissection. Anat. Rec. - Part B New Anat. 2004. p. 4–5. [DOI] [PubMed]
- 23.Knobe M, Carow JB, Ruesseler M, Leu BM, Simon M, Beckers SK, et al. Arthroscopy or ultrasound in undergraduate anatomy education: A randomized cross-over controlled trial. BMC Med Educ. 2012;12:85. doi: 10.1186/1472-6920-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeppesen KM, Bahner DP. Teaching bedside sonography using peer mentoring: A prospective randomized trial. J Ultrasound Med. 2012;31:455–459. doi: 10.7863/jum.2012.31.3.455. [DOI] [PubMed] [Google Scholar]
- 25.Feilchenfeld Z, Dornan T, Whitehead C, Kuper A. Ultrasound in undergraduate medical education: a systematic and critical review. Med Educ. 2017. [DOI] [PubMed]
- 26.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700–0. [DOI] [PMC free article] [PubMed]
- 27.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. British Medical Journal Publishing Group; 2016;355:i4919. [DOI] [PMC free article] [PubMed]
- 28.Bates, Reid. A critical analysis of evaluation practice: the Kirkpatrick model and the principle of beneficence. Eval Program Plann [Internet]. Elsevier; 2004 [cited 2019 Sep 30];27:341–7. Available from: https://ideas.repec.org/a/eee/epplan/v27y2004i3p341-347.html
- 29.Hammick M, Dornan T, Steinert Y. Conducting a best evidence systematic review. Part 1: From idea to data coding. BEME Guide No. 13. Med Teach [Internet]. 2010 [cited 2019 Sep 30];32:3–15. Available from: 10.3109/01421590903414245 [DOI] [PubMed]
- 30.Sweetman GM, Crawford G, Hird K, Fear MW. The benefits and limitations of using ultrasonography to supplement anatomical understanding. Anat Sci Educ [Internet]. 2013 [cited 2019 Jun 7];6:141–8. Available from: 10.1002/ase.1327 [DOI] [PubMed]
- 31.Daniela Fodor, Radu Badea, Laura Poanta, Dan Lucian Dumitraşcu, Anca Dana Buzoianu P-AM. The use of ultrasonography in learning clinical examination– a pilot study involving third year medical students [Internet]. 2012. Available from: http://www.medultrason.ro/assets/Magazines/Medultrason-2012-vol14-no3/02Fodor.pdf.pdf [DOI] [PubMed]
- 32.Parikh T, Czuzak M, Bui N, Wildner C, Koch B, Leko E, et al. Novel use of ultrasound to teach reproductive system physical examination skills and pelvic anatomy. J Ultrasound Med [Internet]. 2018 [cited 2019 Jun 4];37:709–15. Available from: 10.1002/jum.14408 [DOI] [PubMed]
- 33.Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L. Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med [Internet]. 2015 [cited 2019 Jun 5]. p. 43–50. Available from: 10.7863/ultra.34.1.43 [DOI] [PubMed]
- 34.Jamniczky HA, Mclaughlin K, Kaminska ME, Raman M, Somayaji R, Wright B, et al. Cognitive load imposed by knobology may adversely affect learners’ perception of utility in using ultrasonography to learn physical examination skills, but not anatomy. Anat Sci Educ [Internet]. 2015 [cited 2019 Jun 5];8:197–204. Available from: 10.1002/ase.1467 [DOI] [PubMed]
- 35.Ahn JS, French AJ, Thiessen MEW, Browne V, Deutchman M, Guiton G, et al. Using ultrasound to enhance medical students’ femoral vascular physical examination skills. J Ultrasound Med [Internet]. 2015 [cited 2019 Jun 5];34:1771–6. Available from: 10.7863/ultra.15.14.11014 [DOI] [PubMed]
- 36.Walrod BJ, Schroeder A, Conroy MJ, Boucher LC, Bockbrader M, Way DP, et al. Does ultrasound-enhanced instruction of musculoskeletal anatomy improve physical examination skills of first-year medical students? J Ultrasound Med [Internet]. 2018 [cited 2019 Jun 4];37:225–32. Available from: 10.1002/jum.14322 [DOI] [PubMed]
- 37.Legget ME, Toh MY, Meintjes A, Fitzsimons S, Gamble G, Doughty RN. Digital devices for teaching cardiac auscultation - a randomized pilot study. Med Educ Online [Internet]. Taylor & Francis; 2018 [cited 2019 Jun 4];23:1524688. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30499380. [DOI] [PMC free article] [PubMed]
- 38.Liu RB, Suwondo DN, Donroe JH, Encandela JA, Weisenthal KS, Moore CL. Point-of-care ultrasound: Does it affect scores on standardized assessment tests used within the preclinical curriculum? J Ultrasound Med [Internet]. 2019 [cited 2019 Jun 4];38:433–40. Available from: 10.1002/jum.14709 [DOI] [PubMed]
- 39.Afonso N, Amponsah D, Yang J, Mendez J, Bridge P, Hays G, et al. Adding new tools to the black bag-Introduction of ultrasound into the physical diagnosis course. J Gen Intern Med [Internet]. Springer; 2010 [cited 2019 Jun 7];25:1248–52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20697974. [DOI] [PMC free article] [PubMed]
- 40.Butter J, Grant TH, Egan M, Kaye M, Wayne DB, Carrión-Carire V, et al. Does ultrasound training boost Year 1 medical student competence and confidence when learning abdominal examination? Med Educ [Internet]. 2007 [cited 2019 Jun 5];41:843–8. Available from: 10.1111/j.1365-2923.2007.02848.x [DOI] [PubMed]
- 41.Barloon TJ, Brown BP, Abu-Yousef MM, Ferguson KJ, Schweiger GD, Erkonen WE, et al. Teaching physical examination of the adult liver with use or real-time sonography. Acad Radiol [Internet]. 1998 [cited 2019 Jun 5];5:101–3. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1076633298801293 [DOI] [PubMed]
- 42.Hoppmann RA, Rao V V., Bell F, Poston MB, Howe DB, Riffle S, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J [Internet]. Springer; 2015 [cited 2019 Jun 7];7:1–15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26589313. [DOI] [PMC free article] [PubMed]
- 43.Rempell J, Saldana F, DiSalvo D, Kumar N, Stone M, Chan W, et al. Pilot point-of-care ultrasound curriculum at harvard medical school: early experience. West J Emerg Med [Internet]. California Chapter of the American Academy of Emergency Medicine (Cal/AAEM); 2016 [cited 2019 Jun 5];17:734–40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27833681. [DOI] [PMC free article] [PubMed]
- 44.Fodor D, Badea R, Poanta L, Dumitrascu DL, Buzoianu AD, Mircea PA. The use of ultrasonography in learning clinical examination- a pilot study involving third year medical students. Med Ultrason. 2012;14:177–181. doi: 10.11152/mu.2013.2066.143.df177. [DOI] [PubMed] [Google Scholar]
- 45.Davis JJ, Wessner CE, Potts J, Au AK, Pohl CA, Fields JM. Ultrasonography in undergraduate medical education: A systematic review. J Ultrasound Med [Internet]. 2018 [cited 2019 Aug 10];37:2667–79. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29708268. [DOI] [PubMed]
- 46.Mircea PA, Badea R, Fodor D, Buzoianu AD. Using ultrasonography as a teaching support tool in undergraduate medical education - time to reach a decision [Internet]. Med. Ultrason. 2012 [cited 2019 Aug 11]. p. 211–6. Available from: http://www.medultrason.ro/assets/Magazines/Medultrason-2012-vol14-no3/08Mircea.pdf [PubMed]
- 47.Grignon B, Oldrini G, Walter F. Teaching medical anatomy: what is the role of imaging today? Surg Radiol Anat [Internet]. 2016 [cited 2019 Aug 11];38:253–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26298830. [DOI] [PubMed]
- 48.Mullen A, Kim B, Puglisi J, Mason NL. An economical strategy for early medical education in ultrasound. BMC Med Educ [Internet]. 2018 [cited 2019 Aug 11];18:169. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30021562. [DOI] [PMC free article] [PubMed]
- 49.Mollenkopf M, Tait N. Is it time to include point-of-care ultrasound in general surgery training? A review to stimulate discussion. ANZ J Surg [Internet]. 2013 [cited 2019 Aug 11];83:908–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23980756. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)