Abstract
Background
The medical literature reports that many medical trainees experience burnout. The primary goal of this study was to determine how the prevalence of burnout and other forms of emotional distress among the University of Kansas School of Medicine (KUSM) medical students compared to the previously published data.
Methods
We conducted a cross-sectional survey of 379 medical students. Between July and September 2018, we surveyed 872 KUSM medical students on the three campuses (Kansas City, Salina, and Wichita) of KUSM. The survey included items on demographic information, burnout, symptoms of depression, fatigue, quality of life, and self-reported general health. The authors used standard descriptive summary statistics, Kruskal-Wallis test/one-way analysis of variance, chi-square test, correlation, and multivariate logistic regression model to analyze the data.
Results
The overall response rate was 43.5% with 48% of the students reporting manifestations of burnout. Burnout, depression, and fatigue were lowest during the first year of training and increased as year in training progressed. In multivariate models, only year in training was associated with increased odds of burnout, symptoms of depression, and fatigue. Nearly 46% of the students screened positive for depression, and 44.6% reported high levels of fatigue in the past week.
Conclusion
Even though KUSM students have a lower prevalence of burnout than the national rate (48% vs. 55.9%), this prevalence is high enough to warrant new interventions. Because burnout and other emotional distress increase over the course of medical school no matter what campus the students attend, interventions should be both longitudinal and global across all campuses.
Keywords: Medical students, Burnout, Depression, Fatigue, Quality of life, Self-reported general health
Introduction
The medical literature reports that many medical trainees experience burnout in response to chronic job stressors [1, 2]. Manifestations of burnout are characterized in three dimensions: overwhelming exhaustion, depersonalization and detachment from the job, and a sense of ineffectiveness and lack of accomplishment [3]. As explained by Maslach and Leiter, exhaustion is the physical and emotional component of burnout, and is a state of physical and mental fatigue. A person experiencing emotional exhaustion feels overextended and has surpassed their coping limits without any source of replenishment and recovery. Depersonalization is the interpersonal component of burnout and manifests as cynicism, emotional detachment, and disengagement from the job. Finally, the self-evaluation component of burnout presents as a sense of ineffectiveness and lack of accomplishment. It is a decreased sense of pride in one’s work. A person with low sense of accomplishment is characterized by feelings of incompetence and lack of achievement and productivity.
Burnout is a serious problem among medical professionals that appears to be getting worse. Not only is burnout more common than in other professions, but current data show a 6% increase in burnout manifestations among US medical students over a 6-year period, from 49.6% in 2008 [4] to 55.9% in 2014 [5]. A 2014 study found that 56% of US medical students experienced at least one manifestation of burnout, 58% screened positive for depression, and 9% reported suicidal ideation in the last 12 months [5]. Burnout among medical professionals is associated with a number of negative sequelae, including poor quality of patient care [6, 7], self-reported medical errors [8, 9], increased risk of suicidal ideation [4, 5, 10], and substance use disorder [11]. Due to the high rates of burnout and other forms of emotional distress among medical students, the Liaison Committee on Medical Education requires that each medical school “has in place an effective system of personal counseling for its medical students that includes programs to promote their wellbeing and to facilitate their adjustment to the physical and emotional demands of medical education” (pg. 20) [12].
The primary goal of this study was to determine how the prevalence of burnout and other forms of emotional distress (depression and fatigue) among the University of Kansas School of Medicine (KUSM) medical students compares to the previously published data [4, 5]. A second goal was to assess trends across all 4 years of the curriculum and across all three campuses to give insight for targeted interventions. To our knowledge, these trending data have not been previously published for US medical students. Finally, we sought trends related to a new curriculum being implemented at KUSM over 4 years, beginning in July 2017.
The KUSM has three campuses (Kansas City, Salina, and Wichita). The Kansas City campus is a traditional urban, academic medical center with student classes of 175 in each of the first 2 years, and 125 in each of the third and fourth years. The Wichita campus is an urban/suburban, community-based campus with student classes of 28 in each of the first 2 years and 78 in each of the third and fourth years (50 students complete years 1 and 2 in Kansas City then transfer to Wichita for years 3 and 4). The Salina campus is in a town of 48,000 and has eight students per class. Each campus offers different clinical experiences and educational attributes, and often attracts students with different clinical interests. For example, the Wichita and Salina campuses have a high rate of students matching into primary care. Though the curricular goals and objectives as well as assessment methods are the same for all campuses, the student experience varies. Thus, any differences or similarities between campuses could inform intervention decisions.
Prior to 2017, KUSM had a traditional curriculum that included 15 h of lecture per week in years 1 and 2, most of which emanated from Kansas City to Salina and Wichita via interactive television video conferencing. The new ACE (for Active, Competency-based, and Excellence-driven) curriculum overhauled the entire 4 years, especially years 1 and 2, with interventions based on adult learning theory and methods to encourage professional development, teamwork, and life-long learning. We anticipated improvements in student wellbeing as an outcome of the curriculum reform and wanted to measure whether that occurred. To address our study goals, we sought a survey method that would compare closely with published national data [4, 5] yet be simple and quick enough to encourage completion by medical students.
Methods
Study Design and Participants
The study was a cross-sectional survey of 872 medical students on the three campuses of KUSM from July through September 2018. Each student received an email invitation to participate in the study along with a link to a 10-item survey. Participation was voluntary and responses were anonymous. A sample size of 350 was calculated as necessary for adequate power (> 0.85) to detect significant relationships among the variables with 2 degrees of freedom, P < 0.05, and 0.21 effect size [13, 14]. The KUSM Institutional Review Board granted exemption for the study.
Study Measures
The survey included items on demographic information (age, sex, year in training, and campus location), burnout, symptoms of depression, fatigue, quality of life, and self-reported general health.
Burnout
To make the length of the survey short and reduce the amount of time to complete the survey, manifestations of burnout among the medical students were assessed using two single-item measures of overwhelming exhaustion and depersonalization adapted from the full Maslach Burnout Inventory (MBI-22), which has been previously validated [15]. The overwhelming exhaustion item (“I feel burnout from my work/education”) and depersonalization item (“I’ve become more callous toward people since I became a medical student”) have been shown to be useful screening questions for burnout [16, 17]. These two items have shown the highest factor loading [15, 18, 19] and strong correlation [16, 20] with their respective emotional exhaustion and depersonalization domains in the MBI-22 [16]. The two single items have been used in previous studies to measure manifestations of burnout among medical students [4, 5].
The medical students recorded the degree to which each item applied to them on a 7-point Likert scale (0 = Never, 6 = Every day). The scores of each domain were grouped into low, moderate, and high burnout categories using established cutoffs [2–5, 15]. Higher scores on exhaustion and depersonalization domains are indicative of greater exhaustion and depersonalization, and greater burnout. Consistent with convention [2–5, 15], we considered students who scored high on exhaustion and/or depersonalization domains as having at least one manifestation of professional burnout.
Symptoms of Depression and Fatigue
We screened for symptoms of depression using a 2-item Primary Care Evaluation of Mental Disorders Patient Health depression-screening questionnaire (PHQ-2). The questions asked the participants about their feelings of being down, depressed, or hopeless and if they have been bothered by little interest or pleasure in usual activities during the past month. The 2-question screen has a reported sensitivity of 96% and specificity of 57% [21, 22].
We measured the students’ levels of fatigue over the past week using a standardized linear analog scale (0 = as bad as it can be to 10 = as good as it can be) similar to what is described by West and colleagues [23]. Participants who scored five or less on the scale were considered to have higher levels of fatigue [5].
Quality of Life and General Health
The overall quality of life was assessed using a single global item from the World Health Organization Quality of Life (WHOQOL)-BREF [23]. This single item has been validated for use with medical students [24]. The participants rated their overall quality of life on a 5-point Likert scale (1 = Very poor, 5 = Very good).
For the medical students’ general health, we used the question, “How satisfied are you with your health?” This question was adapted from the World Health Organization Quality of Life (WHOQOL)-BREF [25]. Participants rated their general health satisfaction on a 5-point Likert scale (1 = Very dissatisfied, 5 = Very satisfied).
Statistical Analysis
Standard descriptive statistics were used to create a demographic profile and describe the prevalence of burnout symptoms among the medical students. Kruskal-Wallis test/one-way analysis of variance (for continuous variables), chi-square test (for categorical variables), and correlation were used to evaluate association between the variables. We performed multivariate logistic regression analysis to identify characteristics associated with manifestations of burnout, symptoms of depression, and fatigue. Year in training, age, sex, and location of campus were used in the modeling process. All analyses were 2-sided with alpha of 0.05. The IBM SPSS (Statistical Package for the Social Sciences), version 23 was used for these analyses.
Results
On average, the students spent approximately 2 min to complete the survey. The response rates were 43.5% (379/872) for all the KUSM medical students, 40.5% (259/639) for the Kansas City students, 48.8% (98/201) for the Wichita students, and 28.1% (9/32) for the Salina students. As shown in Table 1, 197 (52%) of the respondents were females; 322 (89.4%) were younger than 30 years; and plurality were in second and third years of training. Analysis of the study sample compared demographically to the overall KUSM medical students’ population showed a statistical difference between the groups on only gender and age. There was a 3.79% margin of error at a 95% confidence level between the study sample and the overall KUSM medical students’ population, demonstrating that our sample represented the overall KUSM medical student population [26, 27].
Table 1.
Demographic characteristics of responding medical students compared to all KUSM medical students
| Characteristics | Responders (N = 379) | All KUSM medical students (N = 872) | P value |
|---|---|---|---|
| Gender, no. (%) | 0.024 | ||
| Male | 166 (43.8) | 460 (52.8) | |
| Female | 197 (52.0) | 412 (47.2) | |
| Other | 2 (0.5) | – | |
| Missing | 14 (3.7) | – | |
| Age, years | < 0.001 | ||
| Median | 25.0 | 23.0 | |
| Age group, no. (%) | (n = 360) | ||
| 20–24 | 140 (36.9) | 648 (71.3) | |
| 25–29 | 182 (48.0) | 169 (19.4) | |
| 30–34 | 28 (7.4) | 37 (4.2) | |
| 35–39 | 5 (1.3) | 13 (1.5) | |
| 40–44 | 5 (1.3) | 5 (0.6) | |
| Year in training, no. (%) | 0.997 | ||
| First-year medical student | 91 (24.0) | 213 (24.4) | |
| Second-year medical student | 96 (25.3) | 223 (25.6) | |
| Third-year medical student | 96 (25.3) | 230 (26.4) | |
| Fourth-year medical student | 86 (22.7) | 206 (23.6) | |
| Missing | 10 (2.6) | – | |
| Campus of location | 0.241 | ||
| Kansas City | 259 (68.3) | 639 (73.3) | |
| Wichita | 98 (25.9) | 201 (23.1) | |
| Salina | 9 (2.4) | 32 (3.7) | |
| Missing | 13 (3.4) | – | |
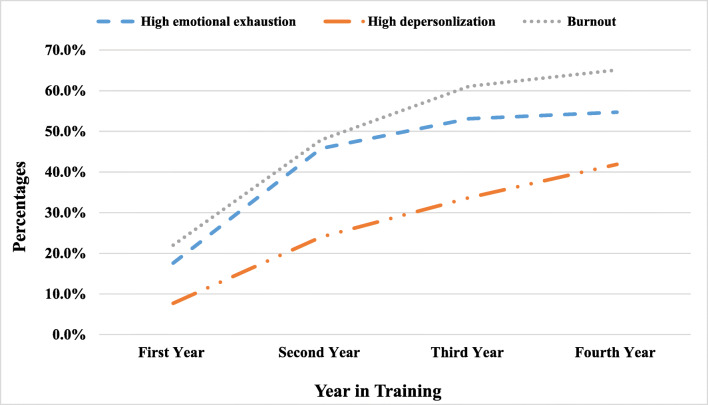
Table 2 summarizes the prevalence of burnout, depression, and fatigue along with overall quality of life and satisfaction with general health. In aggregate, 48% (182 of 379) of the medical student respondents reported manifestations of burnout. Manifestations of burnout increased with seniority (see Fig. 1).
Table 2.
Burnout, depression, fatigue, quality of life, and general health among KUSM medical students
| Characteristics | All participants (N = 379) | First-year students (n = 91) | Second-year students (n = 96) | Third-year students (n = 96) | Fourth-year students (n = 86) | P value |
|---|---|---|---|---|---|---|
| Burnout index, no. (%)a | ||||||
| Emotional exhaustion: high score | 160 (42.7) | 16 (17.6) | 44 (45.8) | 51 (53.1) | 47 (54.7) | < .001 |
| Depersonalization: high score | 99 (26.5) | 7 (7.7) | 23 (24.0) | 32 (33.7) | 36 (41.9) | < .001 |
| Burnoutb | 182 (48.0) | 20 (22.0) | 46 (47.9) | 58 (61.1) | 56 (65.1) | < .001 |
| Depression, no. (%) | ||||||
| Screened positive for depression | 174 (45.9) | 28 (30.8) | 43 (44.8) | 48 (50.0) | 48 (55.8) | < .01 |
| Missing | 1 (0.3) | – | – | – | 1 (1.2) | |
| Fatigue | ||||||
| Mean (standard deviation [SD])C | 5.9 (2.1) | 7.3 (1.4) | 5.8 (1.9) | 5.5 (2.2) | 5.0 (2.1) | < .001 |
| Level of fatigue in the past week, No. (%) | ||||||
| Low | 205 (54.1) | 74 (81.3) | 51 (53.1) | 46 (47.9) | 32 (37.2) | |
| High | 169 (44.6) | 17 (18.7) | 45 (46.9) | 50 (52.1) | 53 (61.6) | |
| Missing | 5 (1.3) | – | – | – | 1 (1.2) | |
| Quality of life | ||||||
| Mean (SD) | 4.0 (0.8) | 4.5 (0.5) | 4.0 (0.7) | 3.8 (0.9) | 3.9 (0.9) | < .001 |
| Overall quality of life, No. (%) | ||||||
| Very poor | 3 (0.8) | – | – | 2 (2.1) | 1 (1.2) | |
| Poor | 23 (6.1) | – | 4 (4.2) | 9 (9.4) | 10 (11.6) | |
| Neither poor nor good | 37 (9.8) | 1 (1.1) | 12 (12.5) | 12 (12.5) | 9 (10.5) | |
| Good | 208 (54.9) | 42 (46.2) | 59 (61.5) | 55 (57.3) | 46 (53.5) | |
| Very good | 107 (28.2) | 48 (52.7) | 21 (21.9) | 18 (18.8) | 19 (22.1) | |
| Missing | 1 (0.3) | – | – | – | 1 (1.2) | |
| General health | ||||||
| Mean (SD) | 3.7 (1.0) | 4.1 (0.6) | 3.6 (1.0) | 3.5 (1.1) | 3.4 (1.1) | < .001 |
| General health satisfaction, No. (%) | ||||||
| Very dissatisfied | 6 (1.6) | – | – | 3 (3.1) | 3 (3.5) | |
| Dissatisfied | 68 (17.9) | 2 (2.2) | 23 (24.0) | 22 (22.9) | 18 (20.9) | |
| Neither dissatisfied nor satisfied | 46 (12.1) | 8 (8.8) | 12 (12.5) | 11 (11.5) | 13 (15.1) | |
| Satisfied | 192 (50.7) | 58 (63.7) | 45 (46.9) | 44 (45.8) | 41 (47.7) | |
| Very satisfied | 66 (17.4) | 23 (25.3) | 16 (16.7) | 16 (16.7) | 10 (11.6) | |
| Missing | 1 (0.3) | – | – | – | 1 (1.2) | |
aWe assessed burnout using the single-item measures for emotional exhaustion and depersonalization adapted from the full Maslach Burnout Inventory
bHigh score on emotional exhaustion and/or depersonalization subscale of the Maslach Burnout Inventory
cScores ranged from 0 to 10, low mean fatigue score suggests higher/worsened fatigue
Fig. 1.
Manifestations of burnout, emotional exhaustion scores, and depersonalization scores by year in training
As shown in Table 3, the medical students who reported manifestations of burnout were 2.53 (72.1 vs 28.5, P < .001) times more likely to screen positive for depression, and 2.09 (68.0 vs 32.5, P < .001) times more likely to report excessive fatigue. In a multivariate logistic regression model, only year in training was independently associated with higher odds of experiencing burnout (Table 4).
Table 3.
Relationship of depression and fatigue with burnout among the medical students
| Burnout | ||||||
|---|---|---|---|---|---|---|
| Measures | Present | Not present | Total | χ2 | P value | Phi |
| Depression, no. (%) | 70.34 | < .001 | 0.44 | |||
| Screened positive for depression | 124 (72.1) | 48 (27.9) | 172 (100.0) | |||
| Screened negative for depression | 57 (28.5) | 143 (71.5) | 200 (100.0) | |||
| Total | 181 (48.7) | 191 (51.3) | 372 (100.0) | |||
| Level of fatigue, no. (%) | 46.62 | < .001 | 0.35 | |||
| High degree | 115 (62.0) | 54 (32.0) | 169 (100.0) | |||
| Low degree | 66 (32.5) | 137 (67.5) | 203 (100.0) | |||
| Total | 181 (48.7) | 191 (51.3) | 372 (100.0) | |||
Table 4.
Results of multivariable analysis of factors independently associated with burnout, depression, and fatigue among the medical students
| Dependent variables | Independent variables | Odds ratio (95% confidence interval)* | P value |
|---|---|---|---|
| Burnout manifestations | Year in training | < .001 | |
| Fourth year | 6.1 (2.98 to 12.46) | < .001 | |
| Third year | 5.1 (2.63 to 10.11) | < .001 | |
| Second year | 3.2 (1.67 to 6.14) | < .001 | |
| First year | 1.0 (Reference) | − | |
| Age (for each additional year older) | 1.02 (0.95 to 1.10) | 0.51 | |
| Male (versus female) | 0.76 (0.48 to 1.18) | 0.22 | |
| Campus location | 0.79 | ||
| Kansas City | 1.14 (0.25 to 5.09) | 0.87 | |
| Wichita | 0.96 (.204 to 4.48 | 0.95 | |
| Salina | 1.0 (Reference) | – | |
| Screened positive for depression | Year in training | 0.006 | |
| Fourth year | 3.36 (1.71 to 6.61) | < .001 | |
| Third year | 2.22 (1.18 to 4.17) | 0.013 | |
| Second year | 1.85 (1.00 to 3.42) | < .05 | |
| First year | 1.0 (Reference) | – | |
| Age (for each additional year older | 0.98 (.91 to 1.05) | 0.51 | |
| Male (versus female) | 0.80 (.52 to 1.23) | 0.31 | |
| Campus location | 0.84 | ||
| Kansas City | 0.73 (.17 to 3.02) | 0.66 | |
| Wichita | 0.68 (.17 to 2.69) | 0.58 | |
| Salina | 1.0 (Reference) | – | |
| Low degree of fatigue | Year in training | < .001 | |
| Fourth year | 0.13 (.06 to .28) | < .001 | |
| Third year | 0.23 (.11 to .45) | < .001 | |
| Second year | 0.26 (.13 to .50) | < .001 | |
| First year | 1.0 (Reference) | – | |
| Age (for each additional year older | 1.01 (.94 to 1.08) | 0.87 | |
| Male (versus female) | 1.57 (1.00 to 2.47) | 0.51 | |
| Campus location | 0.76 | ||
| Kansas City | 1.10 (.23 to 5.0) | 0.94 | |
| Wichita | 1.26 (.28 to 5.69) | 0.76 | |
| Salina | 1.0 (Reference) | – | |
*Higher odd ratio is more desirable. Odd ratio represents increased risk of burnout, depression, or fatigue in the categorical group relative to the reference group
Overall, 174 (45.9%) of the medical students screened positive for depression during the prior month (Table 2). Symptoms of depression were least prevalent among the first-year medical students and most prevalent among the fourth-year medical students. In the multivariate model, only year in training was independently associated with higher odds of experiencing symptoms of depression (Table 4).
One hundred sixty-nine (44.6%) of all the medical student respondents complained of excessive fatigue during the prior week. The level of fatigue worsened as training year progressed (Table 2). In the multivariate model, year in training was independently associated with higher odds of experiencing fatigue over the prior week (Table 4).
Three hundred and fifteen (83.1%) of the participating students rated their overall quality of life as good/very good, and 258 (68.1%) were satisfied/very satisfied with their self-reported general health (Table 2). The overall quality of life negatively correlated with manifestations of burnout (r[372] = − .45, P < .001), negatively correlated with symptoms of depression (r[377] = − .49, P < .001), negatively correlated with fatigue (r[373] = − .46, P < .001), and positively correlated with general health (r[372] = .43, P < .001).
Discussion
Our multivariate analysis demonstrated that high exhaustion, high depersonalization, manifestations of burnout, depressive symptoms, and high fatigue increased with year in training at KUSM and that the findings were consistent across all three campuses. We did not find significant associations of any of these features with student age, gender, or location of campus. Compared nationally, 48% of the KUSM students reported burnout versus 55.9% of the US medical students. However, the 61.1–65.1% rates among the KUSM medical students in their clinical years are higher than the nationally reported findings of 49.9–55.9% overall [4, 5].
Students experiencing burnout were more likely to have symptoms of depression and fatigue. The definitions for these variables overlap. Our findings support studies that have found an association between medical student burnout and risk of depression [5, 28, 29], and high degree of fatigue [5]. Personal and medical education-related factors have been associated with medical student emotional distress [30]. Different aspects of medical training may have an impact on burnout due to different types of stress. Clinical years in medical school may be associated with longer hours, potentially stressful patient care experiences such as death and dying, and social isolation [31–33].
The high rates of burnout and emotional distress displayed by students as their training progresses could be due to the cumulative effect of medical training. Interestingly, the level of exhaustion among the KUSM medical students plateaued during the clinical years while depersonalization continued to progress. The plateau in exhaustion could be explained by the typical relaxation of work hours in year four as compared to year three. Progression of depersonalization could be due to the cumulative effect of medical education or medical culturalization.
As the majority of students experienced burnout by the end of training, an opportunity exists to promote wellness and prevent burnout. Interventions can be considered from both the individual student perspective and from the curriculum perspective. Effective strategies directed toward individual students include skills training to recognize distress, self-recognition of when to seek help, and development of strategies that promote personal wellbeing. Fostering supportive relationships with faculty mentors has also been suggested as a strategy to reduce emotional distress and promote wellbeing among students [34, 35]. Peer support “buddy-programs,” pairing a senior student with a junior student as a mentor, have been associated with decreased stress among medical students [29, 36]. Peer discussions (e.g., Balint groups) are another opportunity to provide support and prevent burnout [37, 38]. Importantly, medical schools can intensify their commitment to providing support to students with emotional distress either through institutional support systems or outside resources. Also, medical schools can encourage medical students to adopt strategies to reduce the risk of emotional distress. For example, medical trainee participation in activities that promote wellness (such as regular physical activities, healthier eating, adequate sleep, mindfulness activities, emotional decompression, and work-life balance) has been suggested as a strategy to combat emotional distress [30, 39]. Establishing and maintaining meaningful personal and social relationships with family and friends have been associated with a reduction in burnout and other distress among medical students [40, 41].
In the ACE curriculum, KUSM has implemented several of these strategies at all three campuses. The ACE curriculum was in its second year at the time of the study, so the ACE strategies had not been applied to students who were in their clinical years. Follow-up surveys should help us determine which strategies are most successful over time.
In addition, medical schools should consider reforming their curriculum to encourage collaborative learning, which has been suggested to create a positive learning environment that promotes wellbeing [42]. The ACE curriculum at KUSM was designed to expressly address this theme through the use of methods such as case-based collaborative learning [43].
Despite the high rates of distress among the KUSM medical students, the majority (83.1%) of the students rated their overall quality of life as good/very good. 68.1% were satisfied/very satisfied with their general health. The apparent discrepancy between these percentages could be due to the way the students interpreted the survey item. They might have interpreted the quality of life as physical health rather than a multidimensional construct that includes domains of physical health, psychological wellbeing, social relationships, and economic satisfaction [43–47].
A strength of this study was the creation of a single-survey tool to measure burnout and other emotional distress among medical students. The study has brought together constructs from several validated inventories/instruments to create a survey tool that may be useful to others interested in comparing their students to national norms and following trends over time and through curriculum revisions.
Our study has limitations. First, although similar to other studies with medical students [4, 5, 11], the 43.5% overall response rate limits the generalizability of the findings. Emotionally distressed medical students may be less motivated to respond to the survey, or more likely to participate because the topic may be relevant to them. Second, respondents were older and more likely to be female than non-respondents, a confounder of uncertain significance. Third, as the results are limited to the KUSM medical students, the findings may not be generalizable to other medical schools. Though this is the case, the consistency of the findings across three different campus types suggests important generalities in student experience. Finally, the study was done at the beginning of the academic year which could impact the way the findings are reported. First-year students may report low levels of burnout as they have just started medical training, while students in the fourth year have just completed their third year. Thus, higher burnout rates reported by the fourth-year students may be related to the students’ experiences in the third year rather than the fourth year.
Conclusion
In conclusion, even though KUSM students have a lower prevalence of burnout than the national rate (48% vs. 55.9%), this prevalence is high enough to warrant new interventions. Because burnout and other emotional distress increase over the course of medical school no matter what campus the students attend, interventions should be both longitudinal and global across all campuses. Future studies may address causes for the progression of burnout over the course of medical school and the impact of interventions to prevent it earlier. Addressing medical student wellbeing has the potential to not only benefit students, but patients, the public, health care delivery, the medical profession, and medical career.
Acknowledgments
The authors thank Mark Meyer, MD of the University of Kansas School of Medicine for the support on the manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The University of Kansas School of Medicine Institutional Review Board granted exemption for the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.IsHak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160–163. doi: 10.1080/0142159X.2016.1248918. [DOI] [PubMed] [Google Scholar]
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. In: Fiske ST, Schachter DL, Zahn-Waxer, editors, Annual Review of Psychology. 2001;53, pp. 397–422. [DOI] [PubMed]
- 4.Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, Durning S, Moutier C, Szydlo DW, Novotny PJ, Sloan JA, Shanafelt TD. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 5.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 6.Weigl M, Schneider A, Hoffmann F, Angerer P. Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. Eur J Pediatr. 2015;174:1237–1246. doi: 10.1007/s00431-015-2529-1. [DOI] [PubMed] [Google Scholar]
- 7.Shirom A, Nirel N, Vinokur AD. Overload, autonomy, and burnout as predictors of physicians’ quality of care. J Occup Health Psychol. 2006;11:328–342. doi: 10.1037/1076-8998.11.4.328. [DOI] [PubMed] [Google Scholar]
- 8.Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic Proceedings. (In Press). 10.1016/j.mayocp.2018.05.014. 2018. [DOI] [PMC free article] [PubMed]
- 9.Hayashino Y, Utsugi-Ozaki M, Feldman MD, Fukuhara S. Hope modified the association between distress and incidence of self-perceived medical errors among practicing physicians: prospective cohort study. PLoS One. 2012;7:e35585. doi: 10.1371/journal.pone.0035585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ofei-Dodoo S, Kellerman R, Gilchrist K, Casey EM. Burnout and quality of life among active member physicians of the Medical Society of Sedgwick County. Kans J Med. 2019;12(2):33–39. doi: 10.17161/kjm.v12i2.11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyrbye LN, Massie FS, Eacker A, Harper W, Power D, Durning SJ, Thomas MR, Moutier C, Satele D, Sloan J, Shanafelt TD. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304(11):1173–1180. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 12.Liaison Committee on Medical Education. Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. 2016. https://med.virginia.edu/ume-curriculum/wp-content/uploads/sites/216/2016/07/2017-18_Functions-and-Structure_2016-03-24.pdf. Accessed 21 May 2019.
- 13.Australia and New Zealand Melanoma Trials Group Statistical Decision Tree Power calculator for Chi-Square Test https://www.anzmtg.org/stats/PowerCalculator/PowerChiSquare. Accessed 15 Oct 2018.
- 14.Kim H-Y. Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017;42(2):152–155. doi: 10.5395/rde.2017.42.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3. Palo Alto: Consulting Psychologists Press; 1996. [Google Scholar]
- 16.West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24:1318–1321. doi: 10.1007/s11606-009-1129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rafferty JP, Lemkau JP, Purdy RR, Rudisill JR. Validity of the Maslach Burnout Inventory for family practice physicians. J Clin Psychol. 1986;42:488–492. doi: 10.1002/1097-4679(198605)42:3<488::AID-JCLP2270420315>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 18.Kanste O, Miettunen J, Kyngas H. Factor structure of the Maslach Burnout Inventory among Finnish nursing staff. Nurs Health Sci. 2006;8:201–207. doi: 10.1111/j.1442-2018.2006.00283.x. [DOI] [PubMed] [Google Scholar]
- 19.Vanheule S, Rosseel Y, Vlerick P. The factorial validity and measurement invariance of the Maslach Burnout Inventory for human services. Stress Health. 2007;23:87–91. doi: 10.1002/smi.1124. [DOI] [Google Scholar]
- 20.West CP, Dyrbye LN, Satele DV, Slon JA, Shanafelt TD. Concurrent validity of single item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445–1452. doi: 10.1007/s11606-012-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spitzer RL, Williams JB, Kroenke K, Linzer M, de Gruy FV, 3rd, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. doi: 10.1001/jama.1994.03520220043029. [DOI] [PubMed] [Google Scholar]
- 23.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 24.Krägeloh CU, Henning MA, Hawken SJ, Zhao Y, Shepherd D, et al. Validation of the WHOQOL-BREF quality of life questionnaire for use with medical students. Qual Life Res. 2013;22(6):1451–1457. doi: 10.1007/s11136-012-0265-9. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization . Programme on Mental Health. WHOQOL-BREF: introduction, administration, scoring, and generic version of the assessment. Geneva: WHO; 1996. [Google Scholar]
- 26.Data Star, Inc. What Every Researcher Should Know About Statistical Significance. 2008. http://www.surveystar.com/startips/oct2008.pdf. Accessed 29 Oct 2018.
- 27.CheckMarket. Calculate Representative Sample Size. https://www.checkmarket.com/sample-size-calculator/. Accessed 29 Oct 2018.
- 28.Prinz P, Hertrich K, Hirschfelder U, de Zwaan M. Burnout, depression and depersonalization--psychological factors and coping strategies in dental and medical students. GMS Z Med Ausbild. 2012;29(1). [DOI] [PMC free article] [PubMed]
- 29.Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress, burnout and coping strategies in preclinical medical students. N Am J Med Sci. 2016;8(2):75–81. doi: 10.4103/1947-2714.177299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dyrbye LL, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–1622. doi: 10.4065/80.12.1613. [DOI] [PubMed] [Google Scholar]
- 31.MacLeod RD, Parkin C, Pullon S, Robertson G. Early clinical exposure to people who are dying: learning to care at the end of life. Med Educ. 2003;37(1):51–58. doi: 10.1046/j.1365-2923.2003.01412.x. [DOI] [PubMed] [Google Scholar]
- 32.Billings ME, Engelberg R, Curtis JR, Block S, Sullivan AM. Determinants of medical students’ perceived preparation to perform end-of-life care, quality of end-of-life care education, and attitudes toward end-of-life care. J Palliat Med. 2010;13(3):319–326. doi: 10.1089/jpm.2009.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003;18(9):685–695. doi: 10.1046/j.1525-1497.2003.21215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students – a review of the PubMed literature 2000-2008. BMC Med Educ. 2010;10:32. doi: 10.1186/1472-6920-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murdoch-Eaton DG, Levene MI. Formal appraisal of undergraduate medical students: is it worth the effort? Med Teach. 2004;26(1):28–32. doi: 10.1080/0142159032000150502. [DOI] [PubMed] [Google Scholar]
- 36.Mouret GM. Stress in a graduate medical degree. Med J Aust. 2002;177:S10–S11. doi: 10.5694/j.1326-5377.2002.tb04652.x. [DOI] [PubMed] [Google Scholar]
- 37.Benson J, Magraith K. Compassion fatigue and burnout: the role of Balint groups. Aust Fam Physician. 2005;34(6):497–498. [PubMed] [Google Scholar]
- 38.Kjeldmand D, Holmström I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med. 2008;6(2):138–145. doi: 10.1370/afm.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ofei-Dodoo S, Callaway P, Engels K. Prevalence and etiology of burnout in a community-based graduate medical education system: a mixed method study. Fam Med. 2019; in press. [DOI] [PubMed]
- 40.McLuckie A, T Matheson KM, Landers AL, Landine J, Novick J, Barette T, Dimitropoulos G. The relationship between psychological distress and perception of emotional support in medical students and residents and implications for educational institutions. Acad Psychiatry. 2018;42(1):41–47. doi: 10.1007/s40596-017-0800-7. [DOI] [PubMed] [Google Scholar]
- 41.Yiu V. Supporting the well-being of medical students. CMAJ. 2005;172(7):889–890. doi: 10.1503/cmaj.050126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Noori S, Blood A, Meleca J, Kennedy V, Sengupta D. Current directions in medical student wellbeing: a primer for students. Association of American Medical Colleges: https://www.aamc.org/download/450164/data/medstudentwellbeing.pdf. Accessed 4 Jan 2019.
- 43.Krupat E, Richards JB, Sullivan AM, Fleenor TJ, Schwartzstein RM. Assessing the effectiveness of case-based collaborative learning via randomized controlled trial. Acad Med. 2016;91(5):723–729. doi: 10.1097/ACM.0000000000001004. [DOI] [PubMed] [Google Scholar]
- 44.The WHOQOL Group The World Health Organization Quality of Life Assessment (WHOQOL). Development and psychometric properties. Soc Sci Med. 1998;46:1569–1585. doi: 10.1016/S0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention . Measuring healthy days: Population assessment of health-related quality of life. Atlanta: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 46.Gandek B, Sinclair SJ, Kosinski M, Ware JE., Jr Psychometric evaluation of the SF-36 health survey in Medicare managed care. Health Care Financ Rev. 2004;25(4):5–25. [PMC free article] [PubMed] [Google Scholar]
- 47.McHorney CA. Health status assessment methods for adults: past accomplishments and future directions. Annu Rev Public Health. 1999;20:309–335. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]