Abstract
Anatomy is a foundational science mainstay of undergraduate medical school education, particularly in the pre-clerkship curriculum. During the post-clerkship curriculum, students closer to graduate medical education may benefit from a focused concentration on human anatomy related to their specific clinical interests. Here, we describe a course for post-clerkship students that uniquely incorporates a multimodal approach of dissection, didactics, and clinical correlation to radiologic imaging, with the opportunity to personalize student learning on a specialty-specific anatomic region. The course increased students’ confidence of anatomical knowledge and its clinical relevance. Other institutions may benefit from establishing a similar multimodal integrated post-clerkship anatomy curriculum.
Electronic supplementary material
The online version of this article (10.1007/s40670-019-00833-y) contains supplementary material, which is available to authorized users.
Keywords: Anatomy, Radiology, Integrated curriculum, Medical education, Post-clerkship, Personalized learning
Introduction
Anatomy is an essential foundational science that is often limited to the pre-clerkship medical curriculum. Multiple studies have documented a significant decline in anatomy education throughout medical schools [1–3]. Traditionally taught through dissection and didactics, anatomy education has changed with advancements in digital technology. In the era of medical school curriculum revision, schools are incorporating new methods of anatomical teaching, resulting in reduced time allotted to dissection and fewer dedicated anatomy instructors in favor of virtual animation or web-based teaching modules [4–6]. This change decreases the time for students to interact with anatomical structures in the context of the entire human body, removes the opportunity to develop three-dimensional tactile and spatial reasoning skills, and prevents the sense of teamwork that anatomical dissection fosters among students and dissection groups [7–9]. With fewer total hours in gross anatomy and little formal teaching of anatomy in the post-clerkship curriculum, students in later phases of their training may begin to lose their anatomical foundational knowledge.
As part of the changing landscape of anatomical education, basic science educators from the Carnegie Foundation for the Advance of Teaching published a call to reform medical education by encouraging integration and individualization of the learning process, in order to best contribute to students’ professional development [10]. Multiple studies have called for a multimodal approach to contextualize anatomical science into a clinical setting and integrate it with competency-based milestones [11–13]. This shift in thinking is a promising step forward, as integrated curricula with basic science and clinical context promote better retention of information for learners [14]. However, integration of anatomy is a slow process. In a survey of 170 allopathic and osteopathic schools about their anatomy curriculum, 55 institutions still use body donors in a primarily laboratory-based setting, but less than half of that are part of an integrated curriculum [15].
Curriculum 2.0
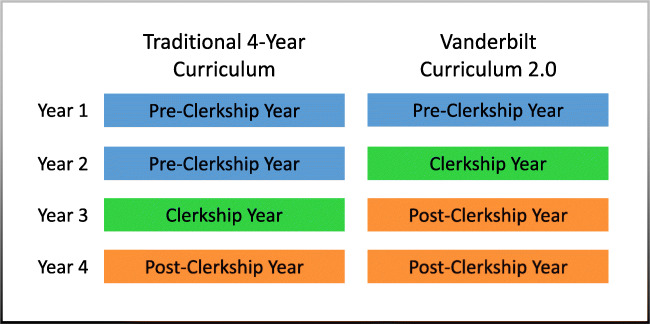
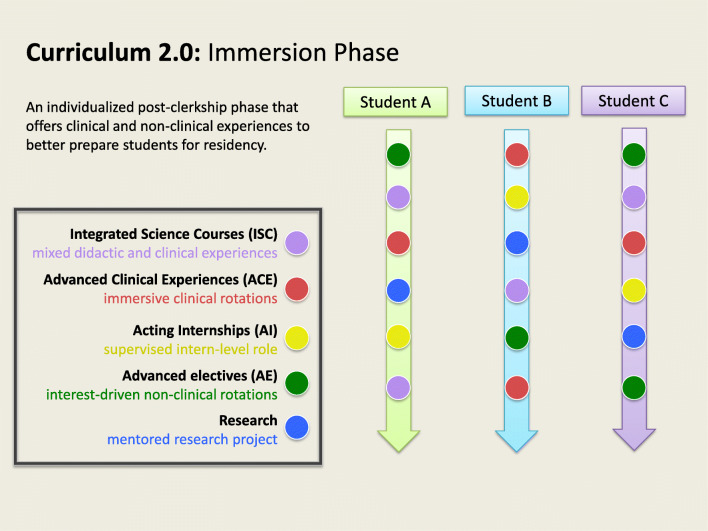
In 2013, Vanderbilt University School of Medicine (VUSM) transitioned to a new undergraduate medical education program, titled Curriculum 2.0 [16]. Curriculum 2.0 is an innovative competency-based curriculum that focuses on individualized learning plans and performance-based medical student advancement, while fitting into the traditional 4 years of medical school. In the first year of the curriculum, students build a strong foundation of medical knowledge through structured case-based and team-based learning, as well as a formal longitudinal anatomy, histology, and pathology curriculum. In the second year of Curriculum 2.0, students build upon their conceptual understanding by rotating through the multiple medical clerkships, including Medicine, Surgery, Psychiatry, Pediatrics, Obstetrics and Gynecology, and Neurology. In the final two years, called the Immersion Phase, students participate in month-long immersion courses that are tailored and most relevant to their individual interests. Immersion courses are designed to solidify clinical skills, deepen foundational science knowledge, and enhance readiness for residency. These electives include integrated science courses (ISCs), advanced clinical experiences (ACEs), acting internships (AIs), and advanced electives (AE) (Figs. 1 and 2).
Fig. 1.
Vanderbilt Curriculum 2.0 schedule compared to traditional 4-year curriculum
Fig. 2.
Schematic diagram of Vanderbilt Curriculum 2.0 Immersion Phase that includes a broad menu of courses including advanced clinical experiences (ACEs), integrated science courses (ISCs), acting internships (AIs), and advanced electives in addition to longitudinal curricular elements
Integrated Science Courses (ISCs)
In a traditional curriculum, foundational science instruction is primarily provided during the preclinical phase of undergraduate medical education. By accelerating the preclinical phase from 2 years to 1 year, Curriculum 2.0 provides students with a greater opportunity to personalize and customize their education in the post-clerkship Immersion Phase. VUSM Curriculum leaders have previously published on the importance and success of integrating foundational sciences in the post-clerkship curriculum in order to enhance scientifically based clinical reasoning skills and knowledge [17]. Most ISCs are co-directed by a scientist and a practicing clinician to allow for broad coverage of the selected foundational science topics and relevant clinical practice. Purposeful repetition of basic foundational sciences within a clinical context can promote better retention of the basic sciences [14]. By integrating basic science and clinical concepts, students build stronger cognitive associations that can guide their diagnostic performance and success [18]. Of the 16 ISCs offered throughout the academic year, five of them integrate components of anatomy into their instruction. Among these ISCs, the Medical Imaging and Anatomy course, which we describe in this monograph, has the greatest focus on anatomy.
Competency-Based Milestones for Professional Development
In Curriculum 2.0, assessment is performed through competency-based milestones, which have been well-studied in the literature in both the undergraduate medical education setting [19] and graduate medical education setting [20]. They are designed to provide higher quality feedback and assessment to help students in their professional development. VUSM students are evaluated by the competency milestones beginning in the pre-clerkship year so they can begin receiving holistic feedback towards their professional growth from the very beginning of their medical education [21]. Previously published work from VUSM Curriculum leaders has demonstrated the implementation and efficacy of competency milestone-based curricular changes across multiple domains [19, 21, 22]. A comprehensive list of competency-based milestones assessed in VUSM students over the 4 years is provided in Online Resource 1. A sample milestone rating form used to evaluate each individual milestone is provided in Online Resource 2.
Here, we present our methodology for developing an elective course for the post-clerkship curriculum that was specifically designed to integrate advanced clinical anatomy with imaging science in the clinical context, with the opportunity for additional personalization of the course to students’ intended specialty of interest.
Methods
ISC Medical Imaging and Anatomy (ISC MIA) Course Design
With new advances in imaging technology in clinical practice, a strong foundational knowledge of anatomy becomes important to interpret results of different imaging modalities [13]. Imaging is also an essential component of diagnosis and disease management across all fields of medicine, as physicians interact with medical imaging in both emergent and non-emergent settings. They are expected to understand the proper utility, indications, limitations, and risks of medical imaging and their correlative anatomy to assist in disease diagnosis and management. Given the importance of anatomy and radiology, other institutions have successfully implemented first-year pre-clerkship curricular changes to integrate clinically oriented anatomy with radiology in a competency-based assessment design [23, 24]. The competency-based design allows for formative feedback early on in their training and invites self- and peer-evaluations to further student professional development and self-reflection.
Previously published survey data suggests that medical students have a generally positive response to integrating radiology into anatomy teaching [25]. However, this survey was performed in a first-year pre-clerkship student population. They also viewed radiology as an adjunct to learning anatomy, rather than a primary learning modality. However, incorporating radiology as a primary modality for in vivo visualization of the anatomy can improve students’ knowledge of anatomical spatial relationships [13, 24]. Full body dissection has been found to be the best modality for medical students, especially those interested in surgical subspecialties, when compared to prosection or plastination [26].
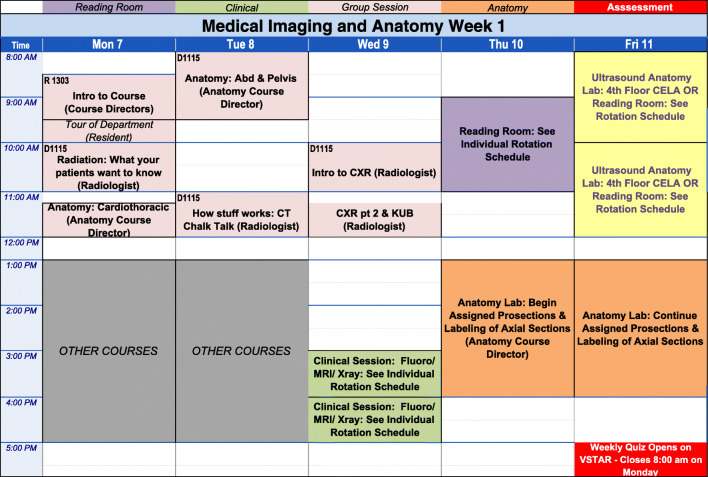
To address the lack of anatomy and radiology education in the post-clerkship curriculum, the “Medical Imaging and Anatomy” course was developed. It is a 4-week-long integrated science course offered to third and fourth years in the post-clerkship Immersion Elective phase of the Vanderbilt’s Curriculum 2.0. It combines laboratory-based anatomic dissections with classroom-based didactic instruction and workplace-based radiologic clinical experiences. The goal of the course is to review key anatomy, improve imaging reading skills, and enhance appropriate ordering of radiologic procedures. With each course offering, a group of 8–10 students learns through a wide range of learning modalities, including gross anatomy dissection, peer teaching, self-assessment, didactics, simulations, and radiology suite observations, as detailed below. Through this novel design, post-clerkship students are better able to incorporate advanced clinical anatomy with imaging and personalize their learning to specialty-specific topics of their interest. A sample weekly schedule is provided in Fig. 3. The milestones assessed in this course are provided in Table 1.
Fig. 3.
Sample weekly schedule for ISC Medical Imaging and Anatomy Course including variety of learning sessions, including reading room experience, clinical imaging experiences, group lectures, dedicated anatomy lab dissection time, and Center of Experiential Learning and Assessment (CELA) Simulation Center Ultrasound workshops
Table 1.
Qualitative (milestone) assessments in medical imaging and anatomy
| Component | Milestones assessed |
|---|---|
| Oral presentation of topic |
Interpersonal communication: IPCS7b.1 Medical knowledge: MK7b Inquiry, MK7c Use of info resources, MK2a Integration (assessed by peers and faculty) |
| Oral demonstration/presentation in GA lab |
Interpersonal communication: IPCS7b.1 Medical knowledge: MK7b Inquiry, MK7c Use of info resources, MK2a Integration Systems-based practice: SBP2a Initiative and contribution to group efforts during dissections (assessed by peers and faculty) |
|
Verbal contributions to peer discussion during the course • Case conference • Show-and-teach sessions • Daily classroom interactions |
Professional duty: PR1b Medical knowledge: MK7a Analysis, MK7B Inquiry Practice-based learning and improvement: PBLI3a |
| Reading room checklist assignment |
Patient care: PC2a Thought process, PC7a Self-knowledge Medical knowledge: MK7b Inquiry, MK7c Use of info resources Systems-based practice: SBP2a Initiative and contribution to group efforts |
| Completion of peer assessments of GA labs and oral presentations | Professionalism: PR1b Professional duty |
Instructional Components
Gross Anatomy Dissections
The full body dissection is divided into ten regions that are individually assigned to students. The ten regions are the brain, head and neck, lungs and posterior mediastinum, external heart and great vessels, internal heart, abdomen, retroperitoneum, pelvis, upper extremity, and lower extremity. Two donor cadaver bodies are designated for this month-long course for student dissection. A third body is used for axial cross-sectional prosections, which are provided to assist students in learning spatial relationships when reading cross-sectional radiographic imaging. A total of 6 h of supervised dissection is provided in the schedule. These two 3-h sessions are overseen by the anatomy course co-director, while students also dedicate additional time in the anatomy for self-directed learning and further dissection. Many of these post-clerkship students have already developed a sense of their intended specialty. Students are ideally assigned to dissect a region of the body relevant to this specialty. For example, a student interested in neurology dissects the brain, while another student interested in otolaryngology dissects the head and neck.
Anatomy Lectures
As part of classroom-based learning, students attend a daily lecture series that builds upon their foundational medical knowledge. A total of 3 h is dedicated to anatomy review of the cardiothoracic, abdominal, and pelvic regions. Anatomy lectures are taught by the anatomy course co-director.
Radiology Lectures and Case Conferences
Twenty-three hours of the didactic lecture series is focused on radiology. Specialty-specific lectures are given by the radiology course co-director, attending and resident physicians, and medical physicists who volunteer their lecture time. Common topics included a systematic approach to evaluating and interpreting images, magnetic resonance imaging (MRI) safety, commonly evaluated anatomy in medical imaging, and differential diagnosis development based on key imaging findings and patient history. Subspecialty-specific topics included Interventional Radiology Overview, Introduction to Neuroradiology, and Introduction to Nuclear Medicine. Some lectures are modeled after interactive case conferences where students are presented with a clinical vignette and image and are prompted to discuss the diagnosis and management.
Bone Session
This 2-h session is an entirely peer-led teaching session where students are divided into four groups of 2–3 students each and assigned a different region of the human skeleton to review and teach back to other groups. Boxed sets of preserved human bones are provided by the School of Medicine for student use. Groups review either the skull, the upper extremities, the lower extremities, or the axial skeleton. Students are able to personalize their own learning by reviewing and demonstrating bony features that are clinically relevant or radiologically pertinent to their peers. The anatomy course co-director and anatomy textbooks are available throughout the session as a reference.
Show and Teach Sessions
Modeled after Resident Teaching Case Conferences, this entirely student-led session asks students to bring interesting radiology cases and to review interesting radiologic findings with their peers. Radiology resident physicians are present to help facilitate the session and provide additional clinical context as needed. This session is intended to be student-driven, where students, rather than certified radiologists, navigate through images on the picture archiving and communication system (PACS). Students receive a lecture on how to navigate the PACS images earlier in the course from a resident physician.
Simulation Center Ultrasound Workshops
Students spend two afternoons learning abdominal ultrasound exam technique with certified radiologists and the Director of the Ultrasound Technologist Program. Sessions are hosted in Vanderbilt’s Center for Experiential Learning and Assessment (CELA). They gain basic hands-on ultrasound scanning experience and recognition of key anatomic structures on the Focused Assessment with Sonography (FAST) exam. They also spend one afternoon with the interventional radiology fellow practicing ultrasound-guided placement of central lines on simulated mannequins.
QuizTime
QuizTime is an electronic learning platform that assesses medical knowledge and clinical reasoning through multiple-choice questions delivered daily through email or text message at a designated time. When students receive the daily question, they have 24 h to respond. As soon as the recipient responds, they receive immediate feedback with the correct answer and complete explanation and reference links to supporting resources. The daily quiz questions do not impact the student’s final evaluation and are designed to supplement the material taught in other didactic sessions.
Experiential Components
Radiology Reading Room Experience
Three 2-h sessions are allocated to dedicated clinical reading room time. Students are provided the opportunity to work with diagnostic radiologists of various subspecialties. Reading room options include chest imaging, body imaging, neuroradiology, musculoskeletal imaging, nuclear medicine, and pediatric imaging. Observation of more specialized radiology procedures, including Nuclear Medicine, computed tomography (CT)-guided interventions, and Interventional Radiology, is also scheduled. These experiences aim to educate students on the indications and logistics of performing these procedures.
Clinical Imaging Suite Experiences
Students are scheduled a total of 5 h to clinically observe radiology technologists perform a variety of imaging modalities, including fluoroscopy, X-ray, and MRI. These sessions provide students with firsthand experience with the standard imaging tools and protocols used in clinical practice. Students observe and interact with the technologists, as well as the patient, to better understand the logistical challenges of these procedures, such as the special instructions that may be provided to the patient before or after imaging and positions that need to be tolerated in order to proceed. These observations help students better identify the indications to ordering the exam and limitations that may preclude a patient from undergoing such exams in the future.
Tumor Board Conference
These 1-h multidisciplinary conferences are offered as an optional opportunity for students to observe how radiologic findings may guide clinical diagnosis and management. During this case-based conference, students observe interactions between various specialties, often including pathology, radiology, diagnosticians, and interventionalists, in the development of the management plan.
Specialized Track Options Available
In addition to the core curriculum, specialized tracks, known as “selectives,” are available to students who would like to customize their radiologic education. The four options available include Musculoskeletal (MSK) Selective, Neuro Imaging Selective, Oncology Selective, and Chest and Body Imaging Selective.
In the MSK Selective, students complete additional self-directed MSK modules that focus heavily on MRI and osteology of the extremities. Students interested in Emergency Medicine or Orthopedics commonly opt into the Musculoskeletal pathway.
In the Neuro Imaging Selective, students complete additional self-directed modules on neuro-specific findings and imaging modalities. Students interested in Neurosurgery, Otolaryngology, Ophthalmology, Neurology, and Psychiatry often opt into this pathway.
In the Oncology Selective, students attend weekly tumor board conferences to supplement their clinical reading room experience. This pathway is geared more towards students interested in Pathology, Radiology, and Radiation Oncology.
All other students who do not select a different track are default placed in the Chest and Body Imaging Selective, where no additional modules or lectures outside of the scheduled lectures were required.
Based on the selective chosen, students complete a different supplemental imaging section on the final exam that is tailored to their chosen selective.
Qualitative Modes of Assessment
Anatomy Prosection Demonstrations
Students are assigned a region of the donor body to dissect and prepare a 40-min demonstration of their dissection to the class. They are asked to highlight clinically relevant structures that may be seen on imaging, along with identifying two axial cross-sections and correlating CT images at that level of the body. Students are evaluated on their presentation delivery, content and organization, enthusiasm and audience engagement, and careful use of their dissection, axial cross-sections, and other imaging resources to enhance their peers’ knowledge of anatomy. Clinical correlations that relate to their donor body and specific anatomy are incorporated into this demonstration. For example, a student interested in Urology who dissects the retroperitoneal organs may choose to present on nephrostomy tubes and their clinical indications, radiologic findings, and anatomical placements.
Oral Presentations
Students deliver a 25-min oral presentation to their peers and faculty on a self-selected topic that showcases how specific anatomical knowledge enhances image interpretation and usefulness in the clinical setting. These interest-driven student topics supplement the range of existing course lecture material. Students receive qualitative feedback anonymously from three randomly assigned peers, as well as faculty, who provide qualitative milestone feedback based on presentation delivery, organization of content, enthusiasm and audience engagement, and use of anatomy and radiology resources (such as ACR Criteria and epidemiologic data). Competency milestone assessments include depth of medical knowledge, ability to conduct inquiry and enhance their own self-knowledge, and communication skills in their presentation to colleagues (Table 1).
Reading Room Case Report Assignment
In order to optimize students’ clinical experience in the Radiology reading rooms, students are asked to submit written summaries for eight cases they observe. This assignment encourages deliberate practice and engagement with radiographic interpretation when in the reading room environment. Students provide the type of imaging test performed, the final diagnosis (or differential if the final diagnosis is unknown), brief patient history of presentation leading to imaging study, and two radiographic findings corroborating the diagnosis. They also evaluate if the imaging study was the most useful or optimal modality to evaluate the chief complaint and pertinent anatomy, with justification from resources such as the ACR Appropriateness Criteria. For example, if an MRI rather than ultrasound was used in a young female presenting with pelvic pain, students will explain the clinical reasoning for the decision. Students’ medical knowledge and use of resources are assessed based upon the competency-based milestones (Table 1).
Quantitative Modes of Assessment
Weekly Quizzes
Students are assessed with timed weekly quizzes on lecture material covered during each of the first three weeks. Students are allotted 20 min to answer 10–15 quiz questions that include multiple-choice, short response, and imaging interpretation, as well as daily QuizTime app questions. Multiple-choice questions are automatically graded when the quiz is submitted. Students are able to review the quiz as a formative tool to enhance their learning, once the quiz for the week has closed. Free text answer responses require course director grading and review prior to score release. Quizzes are available on Vanderbilt’s VSTAR Learning platform from 5:00 pm on Friday until 8:00 am the following Monday.
Gross Anatomy Practical Exam
The gross anatomy practical is a one-on-one oral practical exam with the anatomy co-course director designed to assess the student’s anatomical knowledge in a case-based format. Questions are derived from prior lectures, peer anatomy demonstrations, and relevant clinical presentations. The exam relies heavily on student dissections from that month. As a result, each exam is different per course offering, depending on the quality and/or specific clinical correlations presented during student demonstrations. On exam day, each student is allotted 30 min with the course director. The exam integrates clinical cases to relevant imaging and anatomy. Students are asked to engage with the donor bodies when answering questions and identifying relevant anatomical structures or images. For example, the course director may ask the student to identify the most common location for a thrombus to form in a patient with atrial fibrillation. The student should correctly identify the left atrial appendage on the donor body, as well as relevant CT cross-section of the heart. A follow-up clinical correlation may be, “What procedure can be performed to prevent thrombus and keep a patient off anticoagulation?” The student should then identify occlusion of the left atrial appendage, having learned about it from the student presentations earlier in the course.
End of Course Final Exam
The final exam assesses students on their knowledge of different imaging modalities and their indications, acquisition technique, limitations, and associated risks. Questions are designed to assess students’ anatomical understanding with corresponding structures as it is revealed by imaging modalities.
Selective Final Exam
This Selective portion of the final exam is only taken by the students who chose to be included in the specific track. It includes imaging questions and clinical applications more relevant and closely associated with the specific focus of the selective, which include musculoskeletal imaging and neuro imaging.
Course directors make an overall qualitative assessment score based on the accumulation of milestones assessed and observed behaviors throughout the course (Table 1). Quantitative scores are based upon multiple assignments and exams (Table 2). Together, students are assigned a final grade based on their quantitative and qualitative scores. Final evaluations are categorized into honors, high pass, pass, and fail.
Table 2.
Quantitative assessments in Medical Imaging and Anatomy
| Component | Percentage |
|---|---|
| Quantitative scores on 3 weekly quizzes | 30 |
| Quantitative score oral topic presentation | 10 |
| Quantitative score peer anatomy lab demo | 15 |
| Quantitative score on anatomy lab practical | 15 |
| General final exam | 20 |
| Selective final exam of student’s choosing | 10 |
Results
This ISC Medical Imaging and Anatomy (ISC MIA) course is offered five times per academic year. There is a range of 8–10 students enrolled per course offering, with a maximum capacity of 10 students. This course is normally filled to capacity, often with registration waitlists also filled. Since 2015, this course has been offered 15 times to over 140 students.
On the end-of-course surveys, 64 of 65 (98%) students from October 2017 to November 2018 answered that they were “satisfied” or “very satisfied” with the overall course, “agreed” or “strongly agreed” that the course advanced their foundational science knowledge and that they expect to use this knowledge as part of their future practice, and would recommend this course of their peers. Students also expressed favorable responses in terms of rating the content, assessment, learning objectives, integration of foundational science and clinical experience, mix of learning activities, and leadership of the course (Table 3). Furthermore, 63/65 (97%) students indicated that the course increased their ability to care for patients, especially those presenting with trauma (62/65), chest pain (60/65), abdominal pain (58/65), and back pain (58/65). On average, 37.5% of students choose a specialized track selective, with additional learning modules in MSK, neuro, or oncology, compared to those who are by default placed into the Chest and Body Imaging Selective.
Table 3.
Student responses to end-of-course evaluations
| Please rate the following aspects of the course | Number of students answering “above average/satisfied” or “excellent/very satisfied” (n = 65) |
|---|---|
| Content | 62 (95%) |
| Assessment | 52 (80%) |
| Learning objectives | 57 (88%) |
| Mix of learning activities | 64 (98%) |
| Course leadership | 64 (98%) |
| Integration of foundational science and clinical experience | 63 (94%) |
| Overall course | 64 (98%) |
| This course advanced my foundational science knowledge | 64 (98%) |
| I anticipate using the foundational science knowledge I acquired in this course in my future practice | 64 (98%) |
| I would recommend this course to peers | 64 (98%) |
Answer choices included 1 (very poor/very dissatisfied), 2 (below average/dissatisfied), 3 (average/neutral), 4 (above average/satisfied), and 5 (excellent/very satisfied)
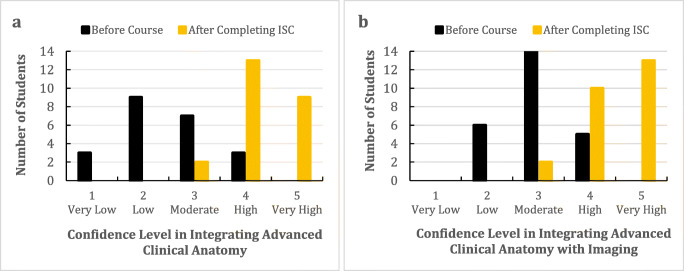
Of 25 more detailed student evaluation surveys completed by students taking the course, the majority of students reported “high” or “very high” confidence in their ability to integrate advanced clinical anatomy into their chosen field of interest after completing the ISC, as compared to before taking the course (92% vs. 14%) (Fig. 4a). Students were also more likely to report “high” or “very high” confidence in their ability to integrate imaging and anatomy in their chosen field of interest after completing the course (92% vs. 20%) (Fig. 4b). Representative student comments included, “This was a great chance for me to get an in depth understanding of the anatomy that applies to my chosen surgical subspecialty” and “Giving my gross anatomy presentation and hearing my classmates’ presentations was one of the most helpful med school experiences in terms of improving my integration of gross anatomy and medical imaging.”
Fig. 4.
After completing ISC Medical Imaging and Anatomy, students had higher confidence in a integrating advanced clinical anatomy and b integrating advanced clinical anatomy with imaging in their specific chosen field of interest. Data shown below is representative from one course offering
Discussion
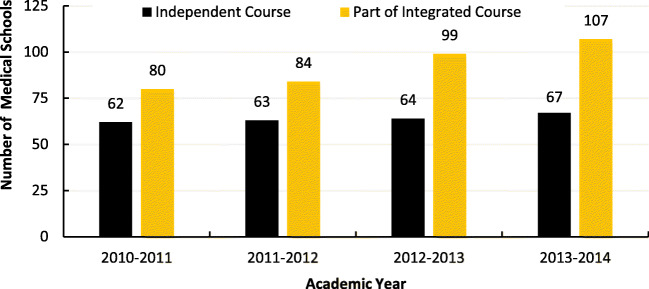
Medical schools are increasingly interested in teaching foundational anatomy in the pre-clerkship phase within an integrated course, rather than as an independent course (Fig. 5). The distinct lack of anatomy education in the post-clerkship setting led to the development of ISC MIA. Previous studies have shown that students are receptive to integrated science courses designed to enrich their basic foundational science knowledge by integrating it within a clinical context [17]. Our students also seem to share this view, as suggested by the enrollment trends of the course and the positive student feedback about the course. It is also reassuring that students felt increased confidence in their ability to use their anatomical knowledge in their future careers. The success of ISC MIA, along with the other ISC courses that incorporate the anatomy foundational science, has allowed for vertical integration of anatomical science into all phases of undergraduate medical student education at VUSM.
Fig. 5.
LCME Annual Medical School Questionnaire Part II, academic years 2010–2014, demonstrates the number of schools that included Anatomy as an independent course or part of an integrated course in the pre-clerkship phase [30]
Integration of Anatomy with Radiology
ISC MIA is a unique course designed specifically to teach anatomy to the post-clerkship student in a clinical radiology context. In Curriculum 2.0, for students interested in learning anatomy, there are three other ISCs that utilize anatomy dissection as part of their curriculum, but none feature anatomy as prominently in the course as ISC MIA. Other courses may use lightly embalmed donor bodies for short sessions with a limited focus, such as dissecting the great vessels and to simulate cannulating the femoral artery. ISC MIA is the primary course offered at Vanderbilt University School of Medicine that dedicates time to anatomical dissection and learning of a wide variety of human body systems intently and intensively. For students interested in bolstering their radiology knowledge, there are four other clinical radiology ACEs students may consider. These courses include general diagnostic radiology, neuroradiology, pediatric, and interventional radiology. However, they are focused on clinical radiology rather than an integration of foundational sciences. ISC MIA is the only radiology course that uses correlative anatomy to help students review how those images are generated and tangibly visualize the anatomical relations of structures seen on imaging.
Personalized Learning
ISC MIA provides an example of how post-clerkship students can personalize their own learning in order to best prepare themselves for their intended specialty. Students pursuing surgical or procedural specialties may elect to spend extra time on specific organ systems. This narrowed focus can deepen their knowledge of relevant anatomy in a low-stress, low-risk learning environment so they may become competent clinicians who can perform safe clinical procedures, particularly surgeons. For example, for future otolaryngologists, this course offers the opportunity to dissect various head and neck structures, including the parotid gland to visualize branches of the facial nerve. They can also simulate performing a laryngectomy on the cadaver and better review the pharyngeal muscles that control the vocal cords, without the fear of causing adverse effects to a live patient. However, the course is designed for students applying to any specialty. The student applying to Internal Medicine may dissect and present the external and internal features of the heart and the Emergency Medicine-bound student may dissect the upper and lower extremities, while the student wishing to enter Psychiatry may complete a detailed dissection of the brain. Students also have 24-h card access to the anatomy lab for additional self-directed learning and review. The chest X-ray and computerized tomography interpretation skills acquired through this course are also widely applicable to any specialty.
Reciprocal Peer Teaching
This course capitalizes on opportunities for students to participate in reciprocal peer teaching through multiple components, including the show-and-teach sessions, bone session, anatomy dissection presentations, and oral presentations. In these sessions, students are given a general framework but otherwise minimal instruction on how to structure their presentation. Prior reports have emphasized the importance of allowing student preferences to guide the most optimal teaching method, particularly with anatomical education [27]. Peer teaching has been associated with acquisition of more knowledge, better attitudes towards anatomy, and improved communication skills [28, 29]. In order to teach their peers, the students themselves must be very knowledgeable in the material that they are presenting. Engaging in other presentations can promote cooperative learning and improved communication skills to both peers and faculty that can be useful in future clinical practice. To a degree, allowing students to teach each other also reduces the number of trained anatomy or radiology faculty that would be needed to direct these sessions as students can self-regulate their material to what they find most relevant or clinically pertinent.
Potential Challenges
Enrollment Demand
As part of their graduation requirements, third- and fourth-year elective students are required to take four ISCs over a 22-month period. There are 16 total ISCs offered throughout the year. They cover a broad range of topics, from sexual medicine and palliative care to clinical immunology and community heath. Each course may be offered two to eleven times a year depending on course director preference and class size. ISC MIA teaches the second largest volume of students among the other ISCs. It is offered five times a year in January, March, September, October, and November, with maximum 10 students each month. September and October are the months of highest ISC demand [17]. November is most popular with third-year post-clerkship students as the fourth-year students are often away for residency interviews. January and March are high-demand months for fourth-year post-clerkship students as they are seeking to improve knowledge and skills relevant to the specialty to which they have just applied. For institutions with larger class sizes, it may be beneficial to expand the maximum enrollment cap each month to accommodate more learners. By grouping students into teams of two or three to dissect one region of the body, the same number of donor bodies could be used. Alternatively, the course could be offered during more months of the year depending on faculty and donor body resources.
Anatomical Donation Resources
This course demands a broad scope of anatomical resources, from donor bodies to dedicated faculty time to oversee dissections. This course utilizes two formalin-fixed bodies designated strictly for post-clerkship student use of this course, so as not to interfere with pre-clerkship dissections that are occurring simultaneously in the school year. If possible, there is one female and one male cadaver to review both types of pelvic anatomy. With female cadavers, ideally the uterus would still be present to facilitate understanding of the three-dimensional female pelvic anatomy, though historically many of our donors have undergone hysterectomies during their lifetime.
Lecture Scheduling
Scheduling dedicated faculty time to lecture medical students may be difficult in a busy academic center. Lectures are not a large time commitment, lasting 1–2 h each, with most lecturers giving only one lecture per course offering. However, with five course offerings per year, it is important to contact faculty lecturers well in advance. However, radiology resident physicians can also serve as well-received lecturers, especially for those interested in medical education. Case conferences and show-and-teach sessions that are primarily image-based are great opportunities for residents to facilitate. Residents can volunteer to teach sessions at times that best fit their schedule, often with relatively minimal preparation beforehand. Established slide sets are provided prior to the lecture so lecturers can review the material to cover, in addition to updating images or cases as needed.
Clinical Imaging Suite Scheduling
Clinical imaging suite experiences in MRI, X-ray, and fluoroscopy are one of the highlights of this course. Students are able to observe the patient experience and how the exam is performed. In the MRI suite, students observe the size of the machine and important precautions that must be taken to avoid injury and appreciate the claustrophobia that some patients may experience. The X-ray suite is similar in that students observe how quickly the images are obtained if the patient is mobile, lucid, and able to follow commands. MRI and X-rays are often performed continuously throughout the day, which makes it convenient to schedule student observation. However, sessions such as fluoroscopic swallow studies are not performed as frequently throughout the day and depend on the schedule of the speech pathologist to administer the exam, so it will be important to obtain this exam schedule ahead of time and schedule students accordingly. Students may be assigned individually or in pairs to go and observe these imaging modalities, so as not to overcrowd the imaging suite space and disrupt workflow.
Summary
In summary, the Medical Imaging and Anatomy Integrated Science Course demonstrates how advanced clinical anatomy education can be incorporated into the post-clerkship curriculum, while providing students with the opportunity for personalized learning towards their intended career. Although it is challenging to balance didactic teaching with relevant clinical experience, ISC MIA allows anatomy foundational sciences to be directly correlated with radiologic clinical imaging so that students may apply their advanced clinical anatomy knowledge to their future practice.
Electronic Supplementary Material
(PDF 86 kb)
(PNG 194 kb)
Compliance with ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sritharan K. The rise and fall of anatomy. Student BMJ; London. 2005 [cited 2019 Mar 17];13. Available from: https://search.proquest.com/docview/1786514246/abstract/D160CBB2228E41CEPQ/1
- 2.Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2:253–259. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]
- 3.Craig S, Tait N, Boers D, McAndrew D. Review of anatomy education in Australian and New Zealand medical schools. ANZ J Surg. 2010;80:212–216. doi: 10.1111/j.1445-2197.2010.05241.x. [DOI] [PubMed] [Google Scholar]
- 4.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ 2017;83–93. [DOI] [PubMed]
- 5.Winkelmann A. Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ. 2007;41:15–22. doi: 10.1111/j.1365-2929.2006.02625.x. [DOI] [PubMed] [Google Scholar]
- 6.Shaffer K. Teaching anatomy in the digital world. New Engl J Med. 2004;351:1279–1281. doi: 10.1056/NEJMp048100. [DOI] [PubMed] [Google Scholar]
- 7.Flack NAMS, Nicholson HD. What do medical students learn from dissection? Anat Sci Educ. 2018;11:325–335. doi: 10.1002/ase.1758. [DOI] [PubMed] [Google Scholar]
- 8.Kerby J, Shukur ZN, Shalhoub J. The relationships between learning outcomes and methods of teaching anatomy as perceived by medical students. Clin Anat. 2011;24:489–497. doi: 10.1002/ca.21059. [DOI] [PubMed] [Google Scholar]
- 9.Korf H-W, Wicht H, Snipes RL, Timmermans J-P, Paulsen F, Rune G, et al. The dissection course – necessary and indispensable for teaching anatomy to medical students. Ann Anat. 2008;190:16–22. doi: 10.1016/j.aanat.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Irby DM, Cooke M, O’Brien BC. Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med. 2010;85:220–227. doi: 10.1097/ACM.0b013e3181c88449. [DOI] [PubMed] [Google Scholar]
- 11.Drake RL. A retrospective and prospective look at medical education in the United States: trends shaping anatomical sciences education. J Anat. 2014;224:256–260. doi: 10.1111/joa.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Estai M, Bunt S. Best teaching practices in anatomy education: a critical review. Ann Anat. 2016;208:151–157. doi: 10.1016/j.aanat.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Johnson EO, Charchanti AV, Troupis TG. Modernization of an anatomy class: from conceptualization to implementation. A case for integrated multimodal–multidisciplinary teaching. Anat Sci Educ. 2012;5:354–366. doi: 10.1002/ase.1296. [DOI] [PubMed] [Google Scholar]
- 14.Ling Y, Swanson D, Holtzman K, Bucak S. Retention of basic science information by senior medical students. Academic Medicine. 2008 [cited 2019 Mar 17];83. Available from: insights.ovid.com [DOI] [PubMed]
- 15.Drake RL, McBride JM, Pawlina W. An update on the status of anatomical sciences education in United States medical schools. Anat Sci Educ. 2014;7:321–325. doi: 10.1002/ase.1468. [DOI] [PubMed] [Google Scholar]
- 16.MD Curriculum. Vanderbilt University. [cited 2019 Mar 17]. Available from: https://medschool.vanderbilt.edu/ume/academic-program/md-curriculum/
- 17.Dahlman KB, Weinger MB, Lomis KD, Nanney L, Osheroff N, Moore DE, et al. Integrating foundational sciences in a clinical context in the post-clerkship curriculum. Med Sci Educ. 2018;28:145–154. doi: 10.1007/s40670-017-0522-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kulasegaram KM, Martimianakis MA, Mylopoulos M, Whitehead CR, Woods NN. Cognition before curriculum: rethinking the integration of basic science and clinical learning. Acad Med. 2013;88:1578–1585. doi: 10.1097/ACM.0b013e3182a45def. [DOI] [PubMed] [Google Scholar]
- 19.Lomis KD, Russell RG, Davidson MA, Fleming AE, Pettepher CC, Cutrer WB, et al. Competency milestones for medical students: design, implementation, and analysis at one medical school. Med Teach. 2017;39:494–504. doi: 10.1080/0142159X.2017.1299924. [DOI] [PubMed] [Google Scholar]
- 20.Holmboe ES, Call S, Ficalora RD. Milestones and competency-based medical education in internal medicine. JAMA Intern Med. 2016;176:1601–1602. doi: 10.1001/jamainternmed.2016.5556. [DOI] [PubMed] [Google Scholar]
- 21.Pettepher CC, Lomis KD, Osheroff N. From theory to practice: utilizing competency-based milestones to assess professional growth and development in the foundational science blocks of a pre-clerkship medical school curriculum. Med Sci Educ. 2016;26:491–497. doi: 10.1007/s40670-016-0262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bird EC, Osheroff N, Pettepher CC, Cutrer WB, Carnahan RH. Using small case-based learning groups as a setting for teaching medical students how to provide and receive peer feedback. Med Sci Educ. 2017;27:759–765. doi: 10.1007/s40670-017-0461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gregory JK, Lachman N, Camp CL, Chen LP, Pawlina W. Restructuring a basic science course for core competencies: an example from anatomy teaching. Med Teach. 2009;31:855–861. doi: 10.1080/01421590903183795. [DOI] [PubMed] [Google Scholar]
- 24.Lufler RS, Zumwalt AC, Romney CA, Hoagland TM. Incorporating radiology into medical gross anatomy: does the use of cadaver CT scans improve students’ academic performance in anatomy? Anat Sci Educ. 2010;3:56–63. doi: 10.1002/ase.141. [DOI] [PubMed] [Google Scholar]
- 25.Murphy KP, Crush L, O’Malley E, Daly FE, Twomey M, O’Tuathaigh CMP, et al. Medical student perceptions of radiology use in anatomy teaching. Anat Sci Educ. 2015;8:510–517. doi: 10.1002/ase.1502. [DOI] [PubMed] [Google Scholar]
- 26.Meguid EMA, Khalil MK. Measuring medical students’ motivation to learning anatomy by cadaveric dissection. Anat Sci Educ. 2017;10:363–371. doi: 10.1002/ase.1669. [DOI] [PubMed] [Google Scholar]
- 27.Davis CR, Bates AS, Ellis H, Roberts AM. Human anatomy: let the students tell us how to teach. Anat Sci Educ. 2014;7:262–272. doi: 10.1002/ase.1424. [DOI] [PubMed] [Google Scholar]
- 28.Krych AJ, March CN, Bryan RE, Peake BJ, Pawlina W, Carmichael SW. Reciprocal peer teaching: students teaching students in the gross anatomy laboratory. Clin Anat. 2005;18:296–301. doi: 10.1002/ca.20090. [DOI] [PubMed] [Google Scholar]
- 29.Evans DJR, Cuffe T. Near-peer teaching in anatomy: an approach for deeper learning. Anat Sci Educ. 2009;2:227–233. doi: 10.1002/ase.110. [DOI] [PubMed] [Google Scholar]
- 30.Curriculum Inventory and Reports (CIR) - Initiatives - AAMC. [cited 2019 Mar 18]. Available from: https://www.aamc.org/initiatives/cir/406466/06b.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 86 kb)
(PNG 194 kb)