Abstract
Introduction
Three-dimensional (3D)-printed models have become increasingly popular as an alternative to the traditional method of cadaveric dissection in teaching anatomy. It has the advantage of lower cost and higher reproducibility. It has been widely used in the postgraduate setting, but its efficacy in undergraduate education has not been studied extensively.
Objectives
A scoping review of the literature was undertaken systematically to investigate the role of 3D printing in the anatomy education of undergraduate medical students.
Methods
A systematic literature search of databases (EMBASE, Pubmed, Educational Resources Information Center, British Education Index and Australian Education Index) was undertaken using relevant keywords.
Results
The search yielded 83 results, which were narrowed down to 13 articles after application of exclusion criteria. The literature supported that 3D printing was a useful tool for studying normal, uncommon and pathological anatomy. However, limitations include low fidelity in replicating the colour and textural physical properties of soft tissues and the trade-off between cost and fidelity.
Conclusions
It is believed that 3D printing would increasingly be integrated into undergraduate anatomy education, and it might also potentially be used in the assessment of anatomical knowledge and clinical skills training. The establishment of an online 3D model database may facilitate educators to easily manufacture models for specific educational purposes.
Keywords: Anatomy education, Medical education, Human anatomy, Undergraduate education, 3D printing, Anatomical models
Introduction
Dissecting cadavers has long been regarded as one of the cornerstones in learning human anatomy [1, 2]. It is often an activity that is exclusively available to the medical profession and anatomists. However, dissection laboratories are expensive to maintain and there are often ethical, cultural and technical concerns about the processing of human specimens, as well as infection risks. The low donation rate in some countries is also problematic, where dissection can often only be performed in large groups [3–6]. Furthermore, there is an argument that since medical practitioners primarily interact with patients via face-to-face consultation and through imaging technology, dissection of cadavers is not essential in the medical school curriculum [7]. For these reasons, certain medical schools have abandoned the use of dissection [7, 8]. New adjuncts or even replacements of teaching aids are therefore being sought. Novel technologies, such as computer-generated virtual reality models [9, 10], are one example. However, the software and hardware can be very costly [2]. Furthermore, there is evidence that virtual reality learning was inferior to plastic models in anatomy education [11]. In the face of the financial challenges to higher education and the healthcare service, sustainable, cost-effective teaching resources are essential in order to deliver high-quality education to medical students [12].
Recently, the cost of three-dimensional (3D) printing has reduced dramatically and it poses as a much cheaper alternative. It also offers tactile response and allows simulations of surgical and dissection techniques. It provides extra value to the two-dimensional (2D) anatomical atlases and textbooks currently residing in classrooms.
There are a number of different types of 3D printers with different mechanisms. The majority employ a layer-by-layer “additive” approach, in which digital data is sent to a printer, where molten material such as plastics or metal is extruded onto a base. As the base moves relative to the nozzle, layers of material are built up to form complex 3D objects [2, 13, 14]. It also allows rapid production of identical copies of models. The detailed technical aspects are beyond the scope of this study.
3D Printing in Medicine
At the early developmental phases of the 3D printing technology, it was primarily used in the manufacturing of industrial prototypes [13]. However, 3D printing has recently become increasingly popular in medical use. Examples include custom-made prosthetics, models for pre-surgical planning, tissue and organ engineering, and models for patient and health professional education [2, 13, 14].
In the context of anatomy education, as depicted in the ‘Results’ section, 3D models can be reconstructed from computed tomography (CT) and/or magnetic resonance imaging (MRI) patient or volunteer data.
This scoping review focuses on the current literature in the use of 3D printing in anatomy education at the undergraduate medical school level.
Methods
A systematic literature search according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [15] criteria was performed. Databases searched included EMBASE, Pubmed, Educational Resources Information Center (ERIC), British Education Index and Australian Education Index [16–20]. The keywords used were ((anatomy OR anatomical) AND ("student"[tiab] OR "school"[tiab] OR undergraduate[tiab])) AND 3d print*, where * denotes truncation and [tiab] denotes searches within title and abstract.
Inclusion criteria
The study population included medical students of all years. The intervention of concern was the use of 3D printing as an education tool for anatomy, comparing with other teaching modalities (where a comparison is available in the studies), and the outcome was the efficacy such as student and trainer feedback.
Exclusion criteria
Studies primarily based on non-human anatomy, anatomical basic sciences research, proof-of-concept or surgical intervention and articles focussing on other allied health professions (e.g. nursing or optometry students) were excluded. In addition, abstracts from conferences were excluded since the amount of details was not the same as that of a journal article.
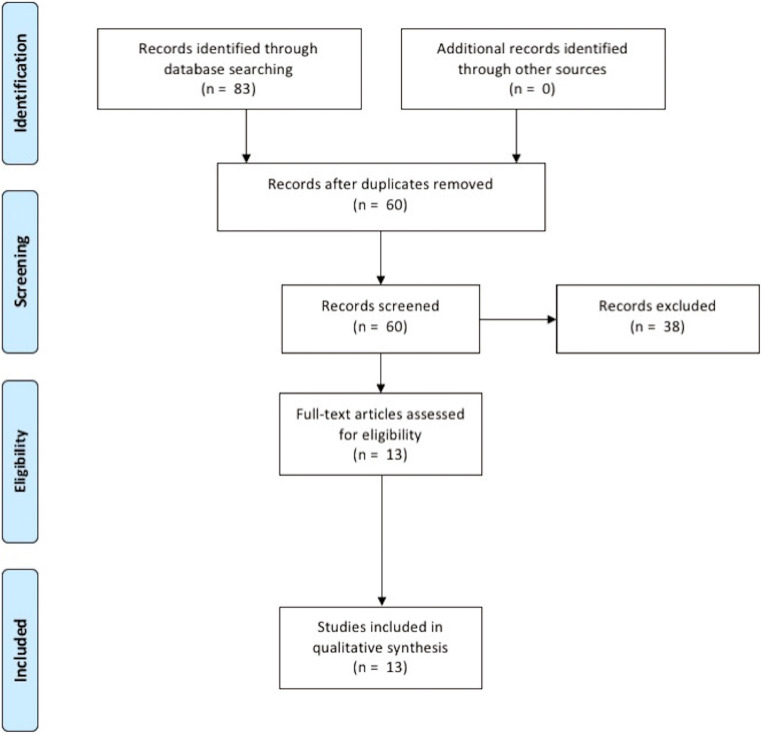
Results were screened using the title and abstract provided. The PRISMA flowchart for this review is shown in Fig. 1, with the application of the described exclusion criteria.
Fig. 1.
Search results from the databases (PRISMA flowchart). ERIC, Educational Resources Information Center; BEI, British Education Index; AEI, Australian Education Index
Results
The literature search yielded 13 entries, after application of our inclusion and exclusion criteria. The article type is shown in Table 1. A more detailed summary is given in Table 2. The results were divided into two groups—those based on normal anatomy and those based on abnormal anatomy, i.e. pathology.
Table 1.
The type of articles included in the critical review
| Type of study | References |
|---|---|
| Randomised controlled trial | (Lim et al., 2016 [23], Chen et al., 2017 [5], AlAli et al., 2017 [28], Smith et al., 2018 [21], Wu et al., 2018 [6]) |
| Sequential comparison study | (Garas et al., 2018 [22], Lee et al., 2018 [29]) |
| Survey | (Jones et al., 2016 [36], Mogali et al., 2018 [24]) |
| Review | (Li et al., 2017 [4]) |
| Others (non-specific descriptive studies) | (Fasel et al., 2016 [25], Lozano et al., 2017, Young et al., 2018 [27]) |
Table 2.
Summary of the articles included in the literature review (AlAli et al., 2017 [28], Chen et al., 2017 [5], Fasel et al., 2016 [25], Garas et al., 2018 [22], Jones et al., 2016 [36], Lee et al., 2018 [29], Li et al., 2017 [4], Lim et al., 2016 [23], Lozano et al., 2017, Mogali et al., 2018 [24], Smith et al., 2018 [21], Wu et al., 2018 [6], Young et al., 2018 [27])
| Study | n | Geographic region | Year | Key points (“N” or “A” denotes whether normal or abnormal/uncommon anatomy was demonstrated) | Strengths | Weaknesses |
|---|---|---|---|---|---|---|
| RCT | ||||||
| Lim et al. | 52 | Australia | 2016 | Comparing the use of cadaveric materials/3D model/combined materials in teaching cardiac anatomy, the 3D model group performed best (p = 0.012) (N) |
Randomised groups Assessor blinded to teaching |
Difficult to explain why the “combined” group did not confer the same advantage |
| Chen et al. | 79 | China | 2017 | Coloured skull models provided better educational outcome than cadaveric skulls and atlas groups (p < 0.05), as evaluated with junior medical students (N) |
Post-tests evaluated by both written and lab tests Inexpensive and precise skull models used |
Lack of pre-tests Not blinded Defects in cadavers |
| AlAli et al. | 67 | UK | 2017 |
Students were randomised into 2 groups (Powerpoint presentation vs Powerpoint +3D models) in the education of cleft lips and palates Post-tests showed improvement in knowledge with 3D model group (p = 0.038) (A) |
Clear learning objectives Low cost |
A heterogenous sample group (sampled from two universities) Not compared to cadavers (gold standard) |
| Smith et al. | 127 | UK | 2018 |
Randomised groups (2D teaching vs 3D model) participated in anatomy training with a range of 3D models—3D group performed better Questionnaires also showed excellent feedback (N) |
Mixed methods (also uses student focus group and questionnaires, faculty evaluation) Pre-tests showing same baseline between randomised groups A range of anatomical models used |
Lack of intravascular contrast in a cadaver specimen meant that the vascular structures were indistinguishable from surrounding soft tissues of similar density, affecting fidelity Formats of pre- and post-tests were different but rationale was not explained (short answer vs single best answer, respectively) |
| Wu et al. | 90 | China | 2018 | Models with spinal, pelvic, upper limb and lower limb fractures were evaluated by medical students (radiographic image group vs 3D-printed model group)—3D model group performed better with the pelvic and spinal test (A) |
Involvement of pathologies (fractures) Diverse range of bony anatomy |
No improvement in the upper and lower limb tests—perhaps advantage was only applicable to more complex anatomy |
| Sequential comparison study | ||||||
| Lee et al. | 20 | Korea | 2018 |
Renal models from ten patients with renal tumours were evaluated by urologists and medical students using questionnaires Students also located tumours more accurately using the 3D models compared to CT images alone (A) |
Introduction of pathology into the models helped to mimic real-life clinical scenarios High-fidelity models Also taught on radiological anatomy |
Not randomised Small sample size |
| Garas et al. | 23 | Australia | 2018 |
Students were all exposed to 3D, wet and plastinated specimens of the heart, shoulder and thigh. With each model, they were asked to identify pinned structures with the aid of 2D atlases A larger number of participants achieved right answers for 3D models compared to wet and plastinated materials (N) |
Used both wet and plastinated materials for comparison Covered three different anatomical parts |
No pre-tests to assess baseline knowledge Not randomised Small sample size Contained a heterogenous mixture of samples (1st and 3rd year students) |
| Survey | ||||||
| Jones et al. | 51 | USA | 2016 | High-fidelity replicas of a number of surgical models were presented at a conference and feedback was provided from written survey (A) |
A range of models evaluated (breast, lung, liver, aorta) High fidelity |
Surveys were filled in by a mixture of surgeons (majority) and medical students |
| Mogali et al. | 15 | Singapore | 2018 |
Multi-coloured and multi-material 3D models of the upper limb were compared with plastinated prosections using surveys and focus group discussion Anatomical features in 3D models were rated as accurate by all students (N) |
High fidelity—uses multiple material |
Compared to plastinated prosections but not soft-prepared cadavers Small sample size |
| Review | ||||||
| Li et al. | N/A | Hong Kong | 2017 | The authors provided a broad overview of applications of 3D printing in surgery (A) |
Put the application of 3D models into a broader context Also reviewed several cardinal papers (some included here) |
Focused on surgical education—especially postgraduate level |
| Others | ||||||
| Fasel et al. | 12 | Switzerland | 2016 |
Anatomy teaching was undertaken by making measurements on replica, scans and cadavers Measurements from 3D-printed models were close to authentic anatomic reality (N) |
Kinaesthetic approach to teaching by making measurements Also taught on radiological anatomy |
Lack of a control group Likely more time-consuming Small sample size |
| Lozano et al. | N/A | Spain | 2017 | A process of manufacturing of a 3D-printed skull model was described (N) | Detailed description of the manufacturing process including both the soft and hardware settings | Did not specify how students were systematically involved in the evaluation of models |
| Young et al. | N/A | Australia | 2018 | CT imaging was used to create replicates of embryonic and fetal anatomical specimens, with good responses from students (A) |
A novel concept that studied a difficult aspect of anatomical sciences Also lessened the potential for adverse student reaction (due to cultural background or personal experience) |
Did not specify how students were systematically involved in the evaluation of models No quantitative results |
RCT randomised controlled trial, CT computed tomography
3D-Printed Models as a Learning and Teaching Tool for Normal Anatomy
A number of innovative studies have been performed to assess the efficacy of 3D-printed models in facilitating anatomy education. Most of these focus on normal anatomy. In a study using a mixed-method sequential strategy, authors based at Brighton and Sussex Medical School manufactured a variety of 3D print models of different organs using high-resolution CT scanning of the cadaver from a recently deceased volunteer [21]. The 127 medical students included were then randomised into 2D (control) and 3D (interventional) teaching groups, with pre- and post-tests. The 3D group performed better statistically in the post-tests. The overall feedback from the students and teaching faculty was also very positive. This was also consistent with another smaller study of similar nature (n = 23) conducted in Australia [22].
In a more focused organ-specific study, a blinded randomised controlled trial (RCT) was conducted involving 52 undergraduate medical students without prior formal cardiac anatomical teaching [23]. In this study, the participants were divided into three groups of self-directed learning. One group used cadaveric materials, one group used 3D prints and the last group used a combination of both. During the self-directed learning sessions, students were given learning objectives, which involve identification of certain key anatomical landmarks. They were then divided up to study the models, where invigilators were refrained from providing any didactic teaching. While the pre-study tests showed similar baseline, the post-study tests found that the group using only 3D prints had the highest mark. The author concluded that the heart anatomy as a single organ might be comparatively simpler than, for example, the pelvis; hence, the result might not be generalised to other organs.
However, the benefits appeared to apply to more complex anatomy as well. A similar RCT randomised 79 junior medical students into three groups, using 3D-printed skulls, cadaveric skulls and atlas, respectively, to study the anatomical structures in the skull via an introductory lecture and small-group discussions [5]. In their 3D models, as well as containing detailed bony prominences, each piece of skull bone was coloured differently to provide further anatomical information. The 3D group performed better than the other two groups in the post-test (combination of written and laboratory tests), with no statistical difference in the pre-test scores. The author attributed the fact that the 3D group performed better than the cadaveric group to the structural variation and damaged structures in the cadavers. In this study, the printer cost $500 and the raw materials cost only $14, demonstrating the sustainability of 3D printing in this context. The colouring of specimens might have also been a contributing factor to the success of this study. This is consistent with a study using colour-coded, 3D-printed models of the upper limb (n = 15), which also showed high satisfaction rates in their educational value [24].
In a more interactive study by Fasel et al., medical students were asked to make measurements of anatomical structures on 2D scans from cadavers and then make measurements on the 3D model and subsequently dissected specimens [25]. Not only did it verify the accuracy of the models, this innovative, multimodal teaching technique was well appreciated by students. It also helped them to better understand the relationship between scans and real-life anatomy.
In addition, more sophisticated models were manufactured to simulate lower limb anatomy and arterial supply, where blood vessels were reconstructed using silicon coating [26]. Vascular simulation was possible through application of pumps and artificial blood. The overall feedback was very positive (although this study mostly targeted surgeons).
3D-Printed Models as a Learning and Teaching Tool for Abnormal or Uncommon Anatomy
3D prints also helped to provide learning aids for structures that are often difficult to sample as specimens, such as those with pathologies and rare anatomical variations. This may be especially useful for more senior medical students who are now more familiar with the normal anatomy.
One example is fetal anatomy, which is usually difficult to access for educational purposes. Young et al. described a method to manufacture 3D-printed models of human embryonic and fetal specimens using data collected from CT scans [27]. They described the approach as a valid way to provide realistic anatomical models to help in the study of developmental anatomy, as the actual specimens were often difficult to obtain and preserve. Furthermore, it lessened the potential for adverse student reaction (due to cultural background, personal experience or revulsion) to observing actual human embryonic or fetal anatomical specimens. Structures that were not previously visualisable can now be explored with haptic feedback using the printed models.
Another example is the anatomy of bony fractures. In a randomised trial targeting 90 medical students, 3D-printed models of bony fractures (spine, pelvis, upper and lower limbs) were shown to provide better understanding than teaching using traditional radiographic images, according to the results of the 20-question post-test [6].
Consistent with the examples above, other pathologies studied in the literature also showed improved educational outcomes. These include cleft lips (3D prints vs slideshow presentations; n = 67) [28] and renal tumours (3D prints vs CT scan imaging) [29].
Discussion
Anatomy learning is known to require complex visuo-spatial skills [30]. Different strategies have been investigated to improve its efficacy, such as multimodal anatomy education, which was found to improve student performance [31]. The important role of processing 3D information in understanding complex anatomy was also supported by studies focusing on virtual reality [32–34]. On that basis, 3D printing is an ideal tool for anatomy education, as students can physically observe and manipulate the 3D topographic features in their hands.
It helps to promote “deep learning” as students can interact with the content directly and more readily apply the concepts to everyday practice [35]. This is likely to be especially useful for students who have a preference for anatomy-heavy specialties such as surgery, histopathology and radiology. Indeed, from surveys directed at medical students and surgeons (n = 51) [36], they all thought 3D models would be useful for integration into the medical school curriculum. As Wilson and Korn explained, students’ attention varies during lectures, and visual aids and active learning methods help teachers to capture the students’ attention, therefore helping them retain more information [37]. For these reasons, unsurprisingly, 3D models have had such a positive effect on the educational outcome compared to conventional learning methods.
In addition, 3D prints provide a versatile adjunct for anatomy education. As students become increasingly confident with normal anatomy, pathologies can be integrated into the more complex models. Hence, clinical knowledge can be obtained via a scaffolding approach in a “spiral curriculum” [38, 39]. This can be employed in teaching modalities such as small-group problem-based learning [40], especially since small-group learning provides higher efficiency than anatomy lectures [41].
From a teacher’s perspective, as Biggs pointed out, it is important to create a learning environment that supports the educational activities appropriate to achieving the desired learning outcomes [42]. In the case of anatomy education, this translates into understanding the 3D structures and functions of the organs. 3D-printed models have large potential to facilitate that process as students can easily use them to participate in interactive group work and independent learning.
Limitations of 3D Printing
The biggest concern with 3D-printed models is whether or not they are realistic enough in resembling the human anatomy. As cautioned in the literature [23], given the variability in human anatomy, an over-reliance on anatomically accurate models may create false understandings of the nuances in study and handling of cadaveric materials. Also, 3D-printed models do not have the same colour and textural physical properties as cadaveric specimens, or indeed the real body organs.
Despite the advances in technology, a recent survey of anatomy teachers still rated plastic models as a teaching aid much inferior to soft-preserved cadavers, when it comes to resembling features of the human body [43]. The amount of details also depends on the resolution of the CT or MRI scans they are based on. However, as technology advances, higher-quality scanners and materials that more closely resemble the textural properties of human tissues are likely to emerge. Certainly, for bony models, it would be a reasonable alternative for now. The message is similarly reflected in a medical student survey of upper limb 3D models [24].
In addition, there is often a trade-off between costs and fidelity of the model, which the teacher has to bear in mind [21]. A quick search of “3D printer” on online retail store Amazon UK® revealed a price tag from just over £100 to almost £9000 [44]. Increasing the engineering fidelity of the model inevitably leads to increases in cost (and time for manufacturing), but depending on the context, beyond certain levels, increasing the fidelity of the training device may only produce small improvements in performance over a simpler device [45]. The correlation between physical fidelity and educational outcome of models remains contentious, with certain simulation studies showing a low-fidelity model may be more cost-effective than a high-fidelity one [46–48].
Limitations of This Study
This article focuses on studies targeted at an undergraduate audience. Therefore, the findings may not extend to pre-university and postgraduate students—although there is a wealth of literature related to its use in the latter group. Students in other allied health professions were also excluded. For example, there is an article on how 3D-printed skull models might help optometry undergraduate students to learn orbital bone anatomy [49]. This kind of article is outside the scope of the study, since the learning needs and the depth of knowledge required are not the same in these two cohorts.
Also, the articles included came from a range of different countries (Table 2), with only two UK-based studies. As different countries have a different structure for their medical education, the conclusions made here may not generalise to all systems.
The randomised trials (Table 1) involved student volunteers. These students tended to be self-selecting since the activities were extra-curricular. The results might therefore be biased and could not be generalised to all student groups. Nevertheless, they demonstrated that 3D models are a potentially valuable complement to learning anatomy.
Most of the randomised trials [5, 21, 23] that showed a difference in the 3D printing as an educational aid employed a written test. As the students could not be “blinded” from the teaching they received, this might potentially have introduced bias in the outcome. Moreover, high performance in a written test does not necessarily translate into better understanding of the details required in real life while treating patients, for example, in the operating theatre. Furthermore, given that the tests were performed almost immediately after the teaching sessions, it is not known if there would be any long-term benefits e.g. higher passing rate for postgraduate surgical examinations.
No meta-analysis was conducted due to the heterogeneity of the studies involved. A significant proportion of the studies was also qualitative in measuring their outcome.
Finally, despite the overwhelmingly positive outcomes in the aforementioned studies, the possibility that the published results were cherry-picked cannot be excluded, as observed in other disciplines [50, 51]. This implies that certain authors might not be reporting their collected data because the results did not support their initial hypothesis i.e. 3D printing improves educational outcome.
Future Directions
3D printing is gradually becoming a standard tool in anatomy education, as demonstrated by the increasing number of studies published. However, unlike many 3D printing-related studies performed in the postgraduate population, most studies involving undergraduates tend to focus on anatomy demonstration (static simulator) rather than improvement of practical skills. Given simulators are capable of providing safe, realistic learning environments for repeated practice [45, 52, 53], it is likely to be used more often in clinical skills training for undergraduates as well, such as in suturing and lumbar puncture.
In terms of data used to produce models, either educators may use their own banks of datasets or there are open datasets which they could use [21, 54]. This provides a very powerful resource that can potentially cover a larger range of different anatomy, when compared to individual cadavers. A regulated online database of appropriate datasets for printing with proper consent from the donors will be a highly useful establishment. Also, online and classroom-based workshops on how to utilise this potentially powerful learning resource to generate teaching material will also be welcomed.
More medical schools are expected to eventually see the value in 3D printing for anatomy education and would increasingly take up its use. In one study, the teachers printed off models of vertebrae, heart and other organs and offered to sell them to interested students as learning aid at a cost as low as USD$10 [21]. This is much cheaper than the alternatives online, which can cost tenfold that amount. Some authors also advocated that every medical school should have a 3D printer for education purposes [2]. However, it will be some time until they can completely replace cadavers due to the limitations mentioned, if it ever happens [55].
As well as being a helpful educational aid, 3D models will be useful in the conduct of further pedagogical studies, for example, how demographics or interest in anatomy would alter educational outcome, as suggested by one of the authors [22]. As mentioned above, studies should also investigate the long-term effect of the integration of 3D prints into the curriculum.
In addition, it may become an essential element in the assessment of undergraduate anatomy due to its low cost and highly reproducible nature. As Brown argued, the most appropriate method of assessment should focus on the evidence of achievement rather than the ability to regurgitate information [56]. Assessing student’s knowledge using a 3D model is likely to be more realistic than asking them to recall a list of facts from a wordy question.
Conclusions
The contemporary literature on the use of 3D printing in undergraduate anatomy education has been reviewed. It has proven to be a cheap, reproducible adjunct to anatomy education. It also provides educators easier means to show pathologies and rarer anatomical variations. Further recommendations would include the establishment of a regulated, collaborated database, where educators may easily access and use the datasets to print appropriate models, tailored to their students’ educational need. It is anticipated that more medical schools would eventually see the value in 3D printing for anatomy education and increasingly take up its use.
Further research into how student demographics or interest in anatomy would alter educational outcome should be considered with the help of 3D-printed models. The utility of 3D printing in setting learning objectives and assessment of students’ anatomy knowledge should also be explored. In addition, studies measuring the long-term educational effects of 3D prints are warranted.
Acknowledgements
The author would like to acknowledge the contribution of Dr. Lucy Spowart, PFHEA, FAcadMEd (University of Plymouth) for proofreading the manuscript and contributing to some of the discussion points mentioned.
Compliance with Ethical Standards
Conflict of Interest
The author declares that he has no conflict of interest.
Ethical Approval
NA
Informed Consent
NA
Footnotes
Notes on Contributors
Jason Yuen, M.Sci., M.A. (Cantab), B.M. B.Ch. (Oxon), M.R.C.S., P.G.Cert. Clin. Ed. is an honorary University Fellow (teaching) at Plymouth University Peninsula Schools of Medicine & Dentistry, England. He is also a Neurosurgical Registrar at Derriford Hospital, Plymouth. He regularly teaches and assesses undergraduate students (formally and informally) and has a strong interest in surgical education.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McLachlan JC, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ. 2006;40(3):243–253. doi: 10.1111/j.1365-2929.2006.02401.x. [DOI] [PubMed] [Google Scholar]
- 2.Balestrini C, Campo-Celaya T. With the advent of domestic 3-dimensional (3D) printers and their associated reduced cost, is it now time for every medical school to have their own 3D printer? Med Teach. 2016;38(3):312–313. doi: 10.3109/0142159X.2015.1060305. [DOI] [PubMed] [Google Scholar]
- 3.Reznick RK, MacRae H. Teaching surgical skills--changes in the wind. N Engl J Med. 2006;355(25):2664–2669. doi: 10.1056/NEJMra054785. [DOI] [PubMed] [Google Scholar]
- 4.Li C, Cheung TF, Fan VC, Sin KM, Wong CW, Leung GK. Applications of three-dimensional printing in surgery. Surg Innov. 2017;24(1):82–88. doi: 10.1177/1553350616681889. [DOI] [PubMed] [Google Scholar]
- 5.Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, Zhu H, Yao Y, Shui W, Shen Z, Zhao J, Pan H. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep. 2017;7(1):575. doi: 10.1038/s41598-017-00647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu AM, Wang K, Wang JS, Chen CH, Yang XD, Ni WF, et al. The addition of 3D printed models to enhance the teaching and learning of bone spatial anatomy and fractures for undergraduate students: a randomized controlled study. Ann Transl Med. 2018;6(20):Y. doi: 10.21037/atm.2018.09.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLachlan JC, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38(4):418–424. doi: 10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 8.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ. 2010;3(2):83–93. doi: 10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- 9.Nicholson DT, Chalk C, Funnell WR, Daniel SJ. Can virtual reality improve anatomy education? A randomised controlled study of a computer-generated three-dimensional anatomical ear model. Med Educ. 2006;40(11):1081–1087. doi: 10.1111/j.1365-2929.2006.02611.x. [DOI] [PubMed] [Google Scholar]
- 10.Levinson AJ, Weaver B, Garside S, McGinn H, Norman GR. Virtual reality and brain anatomy: a randomised trial of e-learning instructional designs. Med Educ. 2007;41(5):495–501. doi: 10.1111/j.1365-2929.2006.02694.x. [DOI] [PubMed] [Google Scholar]
- 11.Khot Z, Quinlan K, Norman GR, Wainman B. The relative effectiveness of computer-based and traditional resources for education in anatomy. Anat Sci Educ. 2013;6(4):211–215. doi: 10.1002/ase.1355. [DOI] [PubMed] [Google Scholar]
- 12.Brice J, Corrigan O. The changing landscape of medical education in the UK. Med Teach. 2010;32(9):727–732. doi: 10.3109/0142159X.2010.497828. [DOI] [PubMed] [Google Scholar]
- 13.Schubert C, van Langeveld MC, Donoso LA. Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol. 2014;98(2):159–161. doi: 10.1136/bjophthalmol-2013-304446. [DOI] [PubMed] [Google Scholar]
- 14.Michalski MH, Ross JS. The shape of things to come: 3D printing in medicine. JAMA. 2014;312(21):2213–2214. doi: 10.1001/jama.2014.9542. [DOI] [PubMed] [Google Scholar]
- 15.PRISMA. PRISMA checklist. 2009. http://www.prisma-statement.org/documents/PRISMA%202009%20checklist.doc. Accessed 6/1/2019.
- 16.Elsevier. Embase(R). Elsevier. 2018. https://www.elsevier.com/solutions/embase-biomedical-research. Accessed 25/11/2018.
- 17.National Center for Biotechnology Information. PubMed. 2018. https://www.ncbi.nlm.nih.gov/pubmed/. Accessed 25/11/2018.
- 18.U.S. Department of Education. ERIC. 2018. https://eric.ed.gov. Accessed 25/11/2018.
- 19.EBSCO. British Education Index. 2018. https://www.ebsco.com/products/research-databases/british-education-index. Accessed 25/11/2018.
- 20.Cunningham Library. Australian Education Index. 2018. https://www.acer.org/library/australian-education-index-aei. Accessed 25/11/2018.
- 21.Smith CF, Tollemache N, Covill D, Johnston M. Take away body parts! An investigation into the use of 3D-printed anatomical models in undergraduate anatomy education. Anat Sci Educ. 2018;11(1):44–53. doi: 10.1002/ase.1718. [DOI] [PubMed] [Google Scholar]
- 22.Garas M, Vaccarezza M, Newland G, McVay-Doornbusch K, Hasani J. 3D-Printed specimens as a valuable tool in anatomy education: a pilot study. Ann Anat. 2018;219:57–64. doi: 10.1016/j.aanat.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Lim KHA, Loo ZY, Goldie SJ, Adams JW, McMenamin PG. Use of 3D printed models in medical education: a randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat Sci Educ. 2016;9(3):213–221. doi: 10.1002/ase.1573. [DOI] [PubMed] [Google Scholar]
- 24.Mogali SR, Yeong WY, Tan HKJ, Tan GJS, Abrahams PH, Zary N, Low-Beer N, Ferenczi MA. Evaluation by medical students of the educational value of multi-material and multi-colored three-dimensional printed models of the upper limb for anatomical education. Anat Sci Educ. 2018;11(1):54–64. doi: 10.1002/ase.1703. [DOI] [PubMed] [Google Scholar]
- 25.Fasel JH, Aguiar D, Kiss-Bodolay D, Montet X, Kalangos A, Stimec BV, et al. Adapting anatomy teaching to surgical trends: a combination of classical dissection, medical imaging, and 3D-printing technologies. Surg Radiol Anat SRA. 2016;38(3):361–367. doi: 10.1007/s00276-015-1588-3. [DOI] [PubMed] [Google Scholar]
- 26.O'Reilly MK, Reese S, Herlihy T, Geoghegan T, Cantwell CP, Feeney RNM, Jones JFX. Fabrication and assessment of 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training in medicine. Anat Sci Educ. 2016;9(1):71–79. doi: 10.1002/ase.1538. [DOI] [PubMed] [Google Scholar]
- 27.Young JC, Quayle MR, Adams JW, Bertram JF, McMenamin PG. Three-dimensional printing of archived human fetal material for teaching purposes. Anat Sci Educ. 2018;12:90–96. doi: 10.1002/ase.1805. [DOI] [PubMed] [Google Scholar]
- 28.AlAli AB, Griffin MF, Calonge WM, Butler PE. Evaluating the use of cleft lip and palate 3D-printed models as a teaching aid. J Surg Educ. 2017. 10.1016/j.jsurg.2017.07.023. [DOI] [PubMed]
- 29.Lee H, Nguyen NH, Hwang SI, Lee HJ, Hong SK, Byun SS. Personalized 3D kidney model produced by rapid prototyping method and its usefulness in clinical applications. Int Braz J Urol. 2018;44(5):952–957. doi: 10.1590/S1677-5538.IBJU.2018.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guillot A, Champely S, Batier C, Thiriet P, Collet C. Relationship between spatial abilities, mental rotation and functional anatomy learning. Adv Health Sci Educ. 2007;12:491–507. doi: 10.1007/s10459-006-9021-7. [DOI] [PubMed] [Google Scholar]
- 31.Johnson EO, Charchanti AV, Troupis TG. Modernization of an anatomy class: from conceptualization to implementation. A case for integrated multimodal-multidisciplinary teaching. Anat Sci Educ. 2012;5(6):354–366. doi: 10.1002/ase.1296. [DOI] [PubMed] [Google Scholar]
- 32.Luursema J-MV, Willem B, Kommers PAM, Annema J-H. The role of stereopsis in virtual anatomical learning. Interact Comput. 2008;20(4-5):455–460. doi: 10.1016/j.intcom.2008.04.003. [DOI] [Google Scholar]
- 33.Brewer DN, Wilson TD, Eagleson R, de Ribaupierre S. Evaluation of neuroanatomical training using a 3D visual reality model. Stud Health Technol Inform. 2012;173:85–91. [PubMed] [Google Scholar]
- 34.Govsa F, Ozer MA, Sirinturk S, Eraslan C, Alagoz AK. Creating vascular models by postprocessing computed tomography angiography images: a guide for anatomical education. Surg Radiol Anat SRA. 2017;39(8):905–910. doi: 10.1007/s00276-017-1822-2. [DOI] [PubMed] [Google Scholar]
- 35.Marton FS, R. On qualitative differences in learning: I. Outcome and process. Br J Educ Psychol. 1976;46(1):4–11. doi: 10.1111/j.2044-8279.1976.tb02980.x. [DOI] [Google Scholar]
- 36.Jones DB, Sung R, Weinberg C, Korelitz T, Andrews R. Three-dimensional modeling may improve surgical education and clinical practice. Surg Innov. 2016;23(2):189–195. doi: 10.1177/1553350615607641. [DOI] [PubMed] [Google Scholar]
- 37.Wilson KK, James H. Attention during lectures: beyond ten minutes. Teach Psychol. 2007;34(2):85–89. doi: 10.1177/009862830703400202. [DOI] [Google Scholar]
- 38.Wood D, Bruner JS, Ross G. The role of tutoring in problem solving. J Child Psychol Psychiatry. 1976;17(2):89–100. doi: 10.1111/j.1469-7610.1976.tb00381.x. [DOI] [PubMed] [Google Scholar]
- 39.Harden RM. What is a spiral curriculum? Med Teach. 1999;21(2):141–143. doi: 10.1080/01421599979752. [DOI] [PubMed] [Google Scholar]
- 40.Greening T. Scaffolding for success in problem-based learning. Med Educ Online. 1998;3(1):4297. doi: 10.3402/meo.v3i.4297. [DOI] [Google Scholar]
- 41.Vasan NS, DeFouw D. Team learning in a medical gross anatomy course. Med Educ. 2005;39(5):524. doi: 10.1111/j.1365-2929.2005.02146.x. [DOI] [PubMed] [Google Scholar]
- 42.Biggs J Aligning teaching for constructing learning. The Higher Education Academy. 2003. https://www.heacademy.ac.uk/system/files/resources/id477_aligning_teaching_for_constructing_learning.pdf.
- 43.Balta JY, Cronin M, Cryan JF, O'Mahony SM. The utility of cadaver-based approaches for the teaching of human anatomy: a survey of British and Irish anatomy teachers. Anat Sci Educ. 2017;10(2):137–143. doi: 10.1002/ase.1629. [DOI] [PubMed] [Google Scholar]
- 44.Amazon. Amazon.co.uk. 2018. http://www.amazon.co.uk. Accessed 25/11/2018.
- 45.Maran NJ, Glavin RJ. Low- to high-fidelity simulation - a continuum of medical education? Med Educ. 2003;37(Suppl 1):22–28. doi: 10.1046/j.1365-2923.37.s1.9.x. [DOI] [PubMed] [Google Scholar]
- 46.Matsumoto ED, Hamstra SJ, Radomski SB, Cusimano MD. The effect of bench model fidelity on endourological skills: a randomized controlled study. J Urol. 2002;167(3):1243–1247. doi: 10.1016/S0022-5347(05)65274-3. [DOI] [PubMed] [Google Scholar]
- 47.McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003-2009. Med Educ. 2010;44(1):50–63. doi: 10.1111/j.1365-2923.2009.03547.x. [DOI] [PubMed] [Google Scholar]
- 48.Munshi FL. Hani; Alyousef, Sawsan. Low- versus high-fidelity simulations in teaching and assessing clinical skills. J Taibah Univ Med Sci. 2015;10(1):12–15. [Google Scholar]
- 49.Backhouse S, Taylor D, Armitage JA. Is this mine to keep? Three-dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ. 2018;12:518–528. doi: 10.1002/ase.1840. [DOI] [PubMed] [Google Scholar]
- 50.John LK, Loewenstein G, Prelec D. Measuring the prevalence of questionable research practices with incentives for truth telling. Psychol Sci. 2012;23(5):524–532. doi: 10.1177/0956797611430953. [DOI] [PubMed] [Google Scholar]
- 51.Bekkers R Risk factors for fraud and academic misconduct in the social sciences. 2012. https://renebekkers.wordpress.com/2012/11/29/risk-factors-for-fraud-and-academic-misconduct-in-the-social-sciences/. Accessed 25/11/2018.
- 52.Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ. 2003;37(3):267–277. doi: 10.1046/j.1365-2923.2003.01440.x. [DOI] [PubMed] [Google Scholar]
- 53.Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 54.Smith ML, Jones JFX. Dual-Extrusion 3D Printing of anatomical models for education. Anat Sci Educ. 2018;11(1):65–72. doi: 10.1002/ase.1730. [DOI] [PubMed] [Google Scholar]
- 55.McMenamin PG, Quayle MR, McHenry CR, Adams JW. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ. 2014;7(6):479–486. doi: 10.1002/ase.1475. [DOI] [PubMed] [Google Scholar]
- 56.Brown S. Assessment for learning. Learn Teach High Educ. 2004;1:81–89. [Google Scholar]