Abstract
Human anatomy education has been traditionally taught using methods such as lecture and cadaveric dissection. Modern technologies that enhance 3-dimensional (3D) visualization, such as virtual reality (VR), are currently being implemented as adjuncts. VR technology provides a level of 3D visualization and interactivity that allows users to explore structures in ways that are often unattainable by direct cadaveric dissection. For example, users can experience simulations in which they can teleport themselves to structures inside of a virtual human body, resize and observe objects from any visual perspective, and draw in a 3D space to test their understanding. In the following study, the utility of VR in anatomy education was assessed and compared with traditional teaching methods including lecture and cadaveric dissection. A VR platform was created in which first-year medical students identified anatomical structures on a virtual cadaveric specimen and then drew these structures on a virtual skeleton using a 3D drawing tool. After completing these tasks, subjects answered survey questions that assessed the usefulness of the virtual platform for learning the names and locations of anatomical structures and understanding 3D anatomical relationships. The survey was also used to evaluate the perceived educational value of VR relative to lectures and cadaveric dissection. The results of our study showed strong subject support for VR technology, suggesting VR is a helpful tool for learning human anatomy and a useful adjunct to lecture and cadaveric dissection.
Keywords: Virtual reality, 3D anatomical relationships, Anatomy-training module, Anatomy education, Medical education, 3D drawing
Introduction
Advances in technology over the past few decades have sparked an interest by medical educators to incorporate computer applications into medical school curricula [1]. This has resulted in the development of various multimedia information delivery tools that enhance medical students’ learning outcomes [2]. One technology that has received a lot of attention from medical educators and may be particularly useful in applications where 3-dimensional (3D) visualization is required is virtual reality (VR). VR provides a highly interactive and dynamic form of simulation where 3D objects can be explored through visual, aural, and haptic senses [3]. VR offers the opportunity to recreate the real world or create different worlds that allow users to perform certain tasks repeatedly in a safe environment [4].
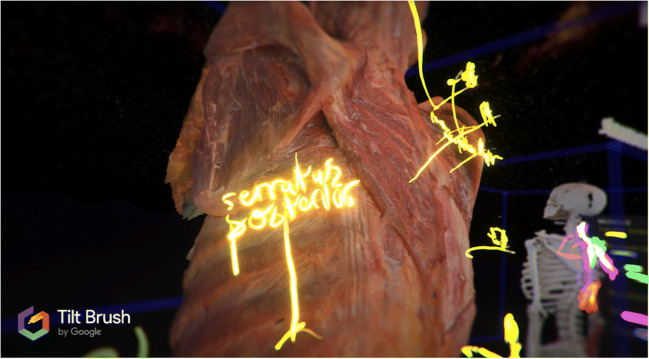
VR 3D drawing applications, such as Gravity Sketch (London, GB) and Google Tiltbrush (Google LLC, Mountain View, CA), provide additional means of interacting with virtual structures. These applications provide the tools to draw in a 3D space and thus provide a means of exploring complex 3D anatomical relationships. For example, it could be difficult for many students to draw the path of the suprascapular nerve from its origin near the roots of the brachial plexus, posterior along the base of the neck, and then illustrate the nerve passing deep to the transverse scapular ligament when limited to drawing in a two-dimensional (2D) format. Drawing this pathway using 3D drawing tools on a virtual reproduction of the human skeleton could provide a simple means for recreating spatial relationships that might otherwise be difficult to draw or visualize on paper.
Medical educators have been studying VR for various purposes, including human anatomy education. One recurrent theme found in the literature that favors the use of VR is that users found this technology motivating, engaging, and entertaining for learning anatomy [4–6]. VR provides a more immersive experience than any 2D or 3D visualization technology, which makes it a compelling and motivating learning environment [7]. Hariri et al. [8] introduced a VR surgical simulation to medical students for learning shoulder anatomy and found that it enhanced student learning through increased motivation. Moro et al. [2] noted how students generally enjoy a VR learning environment because they are inherently curious to explore it.
3D applications, including VR, are equal to, if not more useful, than traditional methods (lectures, textbooks, cadaveric dissection) for understanding anatomy [9]. A study comparing computer model versus textbook pictures showed that subjects who used the student-controlled rotation of a computer graphics hand-model gained significantly better spatial understanding compared with subjects who used 2D images [10].
To validate these highlighted features of VR, we created an educational VR platform for first-year medical students at Cooper Medical School of Rowan University. The platform emphasizes learning the names and locations of anatomical structures and understanding basic 3D anatomical relationships through the use of a virtual cadaver, a virtual skeleton, and a 3D drawing tool. For this study, the authors created virtual cadaveric models from a prosected cadaveric specimen. This contrasts with other commercially available VR platforms in anatomy education that use 3D computer-graphic models of anatomical structures. Therefore, the virtual learning environment used in our platform emphasizes the cadaveric anatomy students would likely experience during a cadaver dissection course. Furthermore, this provides us the opportunity to understand student perception of VR in direct comparison to cadaveric dissection for learning 3D anatomical relationships. We hypothesize that the immersive learning experience provided by this technology along with the ability to draw in 3D would be perceived as a useful adjunct to the standard lecture and cadaveric dissection modalities of anatomy instruction.
Methods
Twenty-eight first-year medical students took part in a VR anatomy training exercise during the second and third weeks of a 4-week anatomy course on the musculoskeletal system. The pertinent gross anatomy coursework that subjects had before the data collection included back and shoulder anatomy lectures and associated cadaveric dissections during the first week of the anatomy course. An email was sent to all 95 first-year medical students describing the study and asking them to voluntarily sign up for a VR session to which 28 students responded. An introductory 5-min video explaining the VR controllers and how to navigate the VR world was included in the email.
During each subject’s VR session, the IRB-approved informed consent was read out loud and signatures were obtained. The subjects then put on the VR equipment, which included the VR headset and 2 controllers, one for each hand. After entering the VR environment, the subjects received 5 min of researcher-guided training on how to use the controllers to navigate in the VR world and how to access the 3D drawing tool. To introduce the drawing tool, subjects were asked to draw a circle in front of them. Upon completion of these instructions, subjects began the VR anatomy-training module with the freedom to proceed at their own pace.
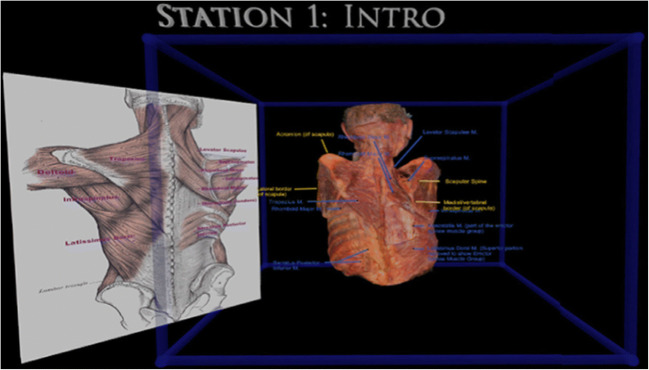
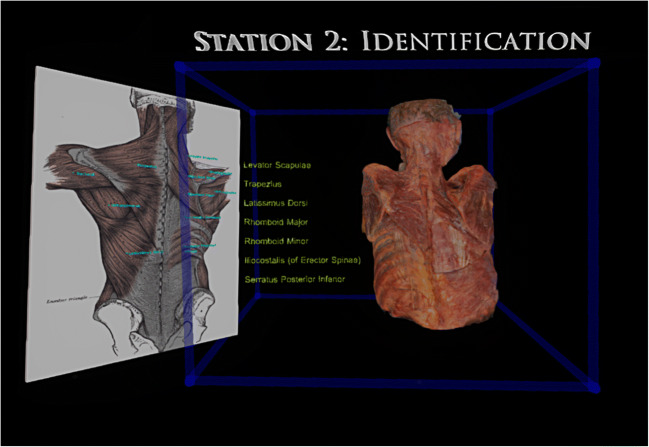
The anatomy-training module consisted of 3 “stations.” In station 1, subjects viewed a labeled 2D image of muscles and bony structures of the back as well as a VR model of a dissected cadaver labeled with the same muscles and bony landmarks (Fig. 1). In this station, subjects were directed to use the labeled 2D image of muscles and bony structures as references and recognize the identical structures on the virtual cadaver. Labeled structures included muscles (deltoid, erector spinae muscle group iliocostalis, infraspinatus, latissimus dorsi, rhomboid major, rhomboid minor, serratus posterior inferior, supraspinatus, teres major, teres minor, and trapezius) and bony landmarks (acromion, lateral border of the scapula, medial border of the scapula, and scapular spine). Subjects informed the researcher once they felt confident about recognizing these structures after which they were instructed to proceed to station 2. Subjects navigated to station 2 using one of the three methods: (a) “teleportation,” which is a feature of VR technology; (b) “pulling” the station closer to themselves using VR tools; or (c) physically walking in the real world. At station 2, subjects were able to view (a) the original labeled 2D reference image; (b) a list of 7 muscles (latissimus dorsi, levator scapulae, longissimus, rhomboid major, rhomboid minor, serratus posterior inferior, and trapezius), and (c) an unlabeled virtual cadaver (Fig. 2). Subjects used the virtual drawing tool to draw a line from the list of muscle labels to the respective muscles on the cadaveric model.
Fig. 1.
Station 1 of the VR training module where subjects were introduced to the labeled virtual cadaver and asked to identify structures that were identical to the two-dimensional labeled image
Fig. 2.
Station 2 of the VR training module where subjects were instructed to draw a line from the list of muscles to their respective location on the virtual cadaver using the 2D image as a guide
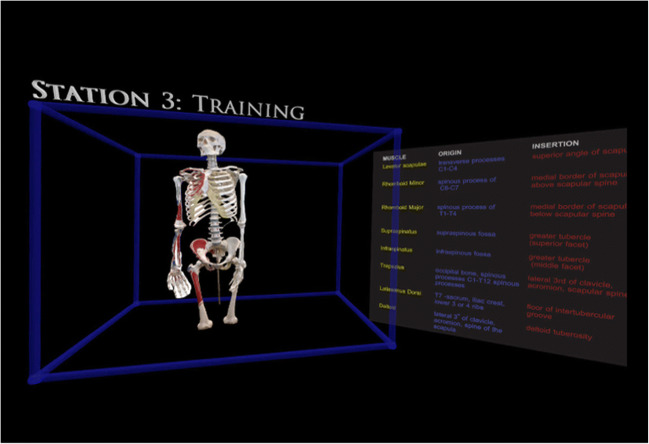
Subjects were not given any feedback from the researcher about whether their labeling was correct or incorrect. Instead, they were instructed to use the labeled 2D reference image to double-check their answers. Only after informing the researcher that they were confident with their labeling were they asked to proceed to station 3. Station 3 consisted of an unlabeled virtual skeleton and a “muscle table” containing the names of eight muscles (deltoid, infraspinatus, latissimus dorsi, levator scapulae, rhomboid major, rhomboid minor, supraspinatus, and trapezius) and their bony attachment sites (origin, insertion) (Fig. 3). Subjects used the virtual drawing tool to draw each of these muscles on the virtual skeleton. They were asked to sequentially go through the muscles listed on the table and draw each according to the listed bony attachments. The only communication between the subject and researcher was regarding how to alter the color and size of the virtual drawing tool if the subject wanted to distinguish each muscle. After completing station 3, each subject was given a survey to help gauge his/her perceptions on the utility of VR in anatomy education, as well as provide open feedback that might help improve the tool.
Fig. 3.
Station 3 of the VR training module where subjects drew muscles on a virtual skeleton using the provided table as a guide
The VR headset used for the study was the HTC VIVE (HTC Corporation, Xiandian District, New Taipei City, Taiwan). The anatomy-training module environment was created using Tiltbrush (Google LLC, Mountain View, CA). The VR model portrayed in stations 1 and 2 was created using a cadaveric specimen. The authors dissected the specimen and photographed it with a Nikon D750. Conversion of the cadaveric specimen and the skeleton to a 3D virtual model was accomplished using 3D Zephyr (3DFlow: Verona, Italy).
Support for this study came from internal funding. The costs associated with the study include the VR headset ($500) and a personal computer ($1700), which contained a GTX1080 graphics-processing unit (NVIDEA). Additional materials and software used to create the virtual cadaveric models totaled approximately $11,000, including cameras, lenses, lighting, structures for holding and moving the cadaveric specimen, and software licenses.
Results
The following questions were analyzed from the survey:
How helpful do you feel VR technology is for learning anatomy?
How effective was this VR training module at helping you learn the names and locations of anatomical structures?
How effective was this VR training module at helping you understand 3D anatomical relationships?
Compared to the lecture portion of the medical school course in which you learned upper back anatomy, was this method worse, the same, or better at helping you understand 3D anatomical relationships?
Compared to the dissection portion of the medical school course in which you learned upper back anatomy, was this method worse, the same, or better at helping you understand 3D anatomical relationships?
For questions 1–3, subjects were given the option to choose from very unhelpful, somewhat unhelpful, neutral, somewhat helpful, and very helpful. For questions 4 and 5, subjects were given the option to choose from much worse, somewhat worse, the same, somewhat better, and much better. The responses for each of these options can be found in Table 1. Responses to question 1 were cross-tabulated with responses to questions 2–5 and these results can be found in Tables 2, 3, 4, and 5. To make it easier to interpret the cross tabulation data, we combined the responses “very helpful” and “somewhat helpful” into a single category “helpful.” “Somewhat unhelpful” and “very unhelpful” were combined to create a single category “unhelpful.” Likewise, we combined the responses “somewhat better” and “much better” to a single category “better.” “Somewhat worse” and “much worse” were combined to a single category “worse.” The comments from the feedback section can be found in Table 6.
Table 1.
Survey results for questions asking whether VR was helpful for learning anatomy, the names and locations of anatomical structures, and 3D anatomical relationships. Survey questions 4 and 5 asked whether VR was better or worse than lecture and cadaveric dissection for understanding 3D anatomical relationships
| Survey questions | Very Helpful | Somewhat helpful | Neutral | Somewhat unhelpful | Very unhelpful | |
|---|---|---|---|---|---|---|
| 1. Learning anatomy | Frequency (n = 28) | 17 | 7 | 0 | 2 | 2 |
| Percentage (%) | 60.7 | 25.0 | 0 | 7.1 | 7.1 | |
| 2. Learning names and locations of anatomical structures | Frequency (n = 28) | 14 | 11 | 0 | 2 | 1 |
| Percentage (%) | 50.0 | 39.3 | 0 | 7.1 | 3.6 | |
| 3. Learning 3D anatomical relationships | Frequency (n = 27) | 18 | 4 | 1 | 1 | 3 |
| Percentage (%) | 66.7 | 14.8 | 3.7 | 3.7 | 11.1 | |
| Much better | Somewhat better | The same | Somewhat worse | Much worse | ||
| 4. Lecture | Frequency (n = 28) | 22 | 5 | 1 | 0 | 0 |
| Percentage (%) | 78.6 | 17.9 | 3.6 | 0 | 0 | |
| 5. Dissection | Frequency (n = 28) | 5 | 15 | 5 | 3 | 0 |
| Percentage (%) | 17.9 | 53.6 | 17.9 | 10.7 | 0 | |
Table 2.
Cross tabulations between the question “How helpful do you feel VR technology is for learning anatomy?” and “Perceived helpfulness of VR for learning names and locations of anatomical structures.” Pertinent findings: All 100% of the subjects that reported VR to be helpful for learning anatomy also reported VR to be helpful for learning the names and locations of anatomical structures
| Perceived helpfulness of VR for learning names and locations of anatomical structures: | ||||
|---|---|---|---|---|
| Perceived helpfulness of VR for learning anatomy: | Helpful | Unhelpful | Total | |
| Helpful |
Frequency Percentage (%) |
24 100.0 |
0 0 |
24 |
| Unhelpful |
Frequency Percentage (%) |
1 25.0 |
3 75.0 |
4 |
| Total | 25 | 3 | n = 28 | |
Fisher’s exact test P = 0.0012
Table 3.
Cross tabulations between the question “How helpful do you feel VR technology is for learning anatomy?” and “Perceived helpfulness of VR for learning 3D anatomical relationships.” Pertinent findings: 91.3% of the subjects that reported VR to be helpful for learning anatomy also reported it to be helpful for learning 3D anatomical relationships
| Perceived helpfulness of VR for learning 3D anatomical relationships: | |||||
|---|---|---|---|---|---|
| Perceived helpfulness of VR for learning anatomy: | Helpful | Neutral | Unhelpful | Total | |
| Helpful |
Frequency Percentage (%) |
21 91.3 |
1 4.4 |
1 4.4 |
23 |
| Unhelpful |
Frequency Percentage (%) |
1 25.0 |
0 0 |
3 75.0 |
4 |
| Total | 22 | 1 | 4 | n = 27 | |
Fisher’s exact test P = 0.0053
Table 4.
Cross tabulations between the question “How helpful do you feel VR technology is for learning anatomy?” and “Perceived value of VR relative to lecture.” Pertinent findings: All 4 of the subjects that found VR unhelpful for learning anatomy found VR to be better than lecture for learning 3D anatomical relationships
| Perceived value of VR relative to lecture: | ||||
|---|---|---|---|---|
| Perceived helpfulness of VR for learning anatomy: | Better | Same | Total | |
| Helpful |
Frequency Percentage (%) |
23 95.8 |
1 4.2 |
24 |
| Unhelpful |
Frequency Percentage (%) |
4 100 |
0 0 |
4 |
| Total | 27 | 1 | n = 28 | |
Fisher’s exact test P = 0.6239
Table 5.
Cross tabulations between the question “How helpful do you feel VR technology is for learning anatomy?” and “Perceived value of VR relative to dissection.” Pertinent findings: 75% of the subjects that found VR to be helpful for learning anatomy also found VR to be better than dissection for learning 3D anatomical relationships
| Perceived value of VR relative to dissection: | |||||
|---|---|---|---|---|---|
| Perceived helpfulness of VR for learning anatomy: | Better | Same | Worse | Total | |
| Helpful |
Frequency Percentage (%) |
18 75.0 |
4 16.7 |
2 8.3 |
24 |
| Unhelpful |
Frequency Percentage (%) |
2 50.0 |
1 25.0 |
1 25.0 |
4 |
| Total | 20 | 5 | 3 | n = 28 | |
Fisher’s exact test P = 0.3624
Table 6.
Comments received from the open-ended portion of the survey regarding the VR technology, the instructions given during the individual sessions, and its utility in anatomy education
| Feedback received from subjects | |
|---|---|
| How the VR training module could be improved? | |
|
Drawing tool 1. Automatically change colors as you move from one muscle to the next. The student could click a box or something indicating that they are done with one muscle then the color could change automatically. 2. Eraser tool rather than undo button 3. A differently style of tip would make it easier to visualize exactly where I am drawing. 4. The paint automatically "sticking" to the bone where you want it to 5. I think the size change feature for the brush could be a little better. The brush strokes were very big even after I tried to change them. | |
|
Controllers 1. The location of the buttons on the controllers in the virtual reality could have better matched with their location in reality 2. More time to get used to the controls | |
|
Simulations 1. When trying to draw lines from the muscle names to muscles it would be helpful if the muscles would light up to ensure the correct connection is being made, like it does with the names. 2. A feature where you can "fade" muscles to help learn and draw superficial vs. intermediate vs. deep muscles | |
|
Training module 1. It was terrific but having more muscles to draw would be great. 2. I wish that some structures had been labeled before hand (i.e., intraspinous fossa) before i got to the drawing portion. Because I couldn't recall what the intraspinous was or where it was located and had no way to look it up in the program while I was in it 3. It would be nice if it also pointed out the exact location for some things like the greater tubercle. 4. I just needed more time with the VR to learn how to use it more effectively. | |
| How instructions could be improved? | |
|
Drawing instructions 1. More clarification on how close to get to the skeleton to draw on the bones 2. For the drawing portion, I wasn't sure how close to the skeleton I should go so there could be some clarification on that. 3. It would be helpful if we are told we can go directly up to the structure itself and draw directly on it. 4. Describing how the dimensions for drawing work. | |
| Suggestions on how VR can be used in improving anatomy instruction? | |
|
Supplement to current anatomy curriculum 1. Using VR every non-lab day to review the lab dissection would be very helpful. 2. This should be a tool offered to us. It is extremely helpful. Since this was our first session the results might be limited because we were still adjusting to the VR technology 4. Making it available after lab would be a great idea 5. Maybe during lecture the professor can use the VR to help show 3D relationships and project them on the screen for students to see. 6. If we cannot gain access as students, video record the correct filling in and make video viewable to students 7. VR would be very helpful to supplement the lectures and dissection portion because it forces you to draw your way through the structures 8. Drawing out the structures definitely helps get an idea of where all of the attachments are. If students had the option to do a simulation as part of the course I think it would be helpful. 9. I believe it would be a great addition to our SMS class. It helped me clarify what areas in Anatomy I should focus on such as insertion and origin of muscles. 10. Having VR technology in designated rooms as a resource for students to use. Perhaps students can book an appointment such as through the SIM center during working hours but it could be open 24/7 after working hours (depends on numbers of VR controllers) 11. It would be very beneficial for independent studying 12. Could be used in a number of system blocks 13. It would be great if we could have a personal VR where we can move around and look at the muscle and identify them, have quizzes, can see nerves and arteries. Basically like complete anatomy but the VR version of it. 14. Weekly sessions in VR at end of week to review spatial relationships/solidify what we learn during dissection 15. Supplement to anatomy lab. As a lab students can sign up to use/study with 16. I think it should be provided for students to study from after lecture and lab because it’s definitely more beneficial for those who do not have much experience in anatomy. 17. I think in terms of studying just having VR headsets available for use where students can book time if needed would be very helpful. | |
|
Replacing lecture 1. It would be a good study tool or in place or some lectures | |
|
Learning anatomy concepts 1. I think this would be an amazing tool for understanding the 3d features of anatomy and elucidate the actions of each muscle in context to their attachments 2. It can help students understand the connections between all of the structures. Its extremely beneficial for the entire anatomy course because you are physically applying the knowledge you learn in class to the VR program. As well as strengthening material you are unsure of by utilizing the drawings and seeing the connections. 3. It’s useful to visualize all the parts especially in terms of what is deep to what. |
VR’s Helpfulness in Learning Anatomy
For question 1, 17/28 (60.7%) of the subjects reported VR to be “very helpful” and 7/28 (25.0%) reported VR to be “somewhat helpful” for learning anatomy. For question 2, 14/28 (50.0%) reported VR to be “very helpful” and 11/28 (39.3%) reported VR to be “somewhat helpful” for learning the names and locations of anatomical structures. Cross tabulations between question 1 and question 2 showed that 24/24 (100%) of the subjects that reported VR helpful for learning anatomy also reported VR helpful for learning the names and locations of anatomical structures (Table 2).
We had an occurrence of human error where we did not receive an answer from one of our subjects for question 3. As a result, we can only present data for 27 subjects. Furthermore, we omitted this subject’s response to question 1 while creating the cross tabulations with question 3 to maintain accuracy. Of the 27 subjects who answered this question, 18/27 (66.7%) of the subjects reported VR “very helpful” and 4/27 (14.8%) of the subjects reported VR “somewhat helpful” for learning 3D anatomical relationships. Cross tabulations between question 1 and question 3 showed that 21/23 (91.3%) of the subjects that reported VR helpful for learning anatomy also reported VR helpful for learning 3D anatomical relationships (Table 3).
VR’s Helpfulness in Learning 3D Anatomical Relationships Relative to Lecture and Cadaveric Dissection
For survey question 4, 22/28 (78.6%) of the subjects reported VR to be “much better” and 5/28 (17.9%) of the subjects reported VR to be “somewhat better” than lecture for learning 3D anatomical relationships. Of note, cross tabulations between question 1 and question 4 showed that all 4 of the subjects who reported VR unhelpful for learning anatomy reported VR to be better than lecture (Table 4).
For question 5, 5/28 (17.9%) of the subjects reported VR to be “much better” and 15/28 (53.6%) of the subjects reported VR to be “somewhat better” than dissection for learning 3D anatomical relationships.
Open-Ended Feedback
The feedback section asked how the VR training module and instructions could be improved going forward and how VR technology can be used to improve anatomy education. For the VR training module itself, the majority of suggestions were regarding the drawing tool and how it could better facilitate our subjects to draw in 3D. For the instructions given during the VR session, subjects mentioned how they initially had difficulty perceiving how close the drawing tool was to the models, and some provided examples of how the instructions could better facilitate this. In terms of how VR could improve anatomy instruction, several subjects suggested having VR as an optional study tool they can use during their self-directed study time to enhance what they learned in lecture and dissection. One subject mentioned possibly using VR during lecture to better demonstrate 3D anatomical relationships. Another mentioned how VR is more beneficial for students who do not have much experience in anatomy.
Discussion
We developed a VR anatomy-training module to supplement the musculoskeletal anatomy course taken by our first-year medical students. Using the VR module, subjects progressed through 3 virtual “stations” that culminated in drawing muscles on a virtual skeleton. We surveyed our subjects to evaluate whether they felt the anatomy-training module (a) improved knowledge of names and locations of anatomical structures, (b) improved subjects’ understanding of 3D anatomical relationships, and (c) whether subjects considered VR training better or worse than the didactic (lecture) and practical (cadaveric dissection) components of their anatomy course.
Subjects’ exposure to 3D anatomical relationships in our VR environment was provided through two mechanisms: first through manipulation of the VR human cadaver to better visualize how the muscles lay on top of each other and second through using the 3D drawing tool to draw on a virtual skeleton. We were unable to find evidence in the literature of others evaluating three-dimensional drawing tools in anatomy education, but there have been several studies that cite drawing anatomical structures on paper alone evoke a form of active learning that enhances drawer’s 3D spatial understanding [11]. We incorporated the 3D drawing tool into 2 of the 3 stations, though primarily in the last station in which subjects drew muscles on a virtual skeleton.
Approximately 80% of our subjects reported VR technology was helpful for learning anatomy and 90% reported it was helpful for learning the names and locations of anatomical structures. These results may lend further support for the effectiveness of VR technology in anatomy education [4–6]; however, we were particularly interested in whether our subjects thought VR technology was an effective tool for teaching 3D anatomical relationships and, specifically, how they perceived it in comparison with (a) lecture and (b) cadaveric dissection. Our VR module utilized 3D cadaveric models, whereas during our lectures, our medical students were presented with 2D images. The VR module also allowed subjects to test their understanding of the relevant anatomy by giving them tools to draw in 3D in the VR environment. These features, specific to VR, were not available in our lecture-based anatomy classes. These features may have contributed to the large percentage (97%) of our subjects reporting VR more helpful than lecture. We found a number of studies that provided additional insight into why students might prefer VR over lecture. Lectures mainly use 2D images to teach spatial relationships. This requires students to mentally reconstruct the images to a 3D structure which can be a challenging cognitive leap [12]. In addition, Stepan et al. [13] found that a VR experience was more engaging, enjoyable, and useful by students, compared with 2D images that are commonly used in lectures. Chittaro et al. [4] discussed how virtual environments provide a “first-person” experience that allows for spontaneous knowledge acquisition as opposed to a lecture, which is a “third-person” experience requiring deliberate reflection and more cognitive effort. Accordingly, we infer that compared with a lecture, VR may provide a less cognitively demanding method and a better learning experience for our subjects to acquire 3D knowledge.
When comparing VR to cadaveric dissection, the majority of the subjects reported the VR module to be better for understanding 3D anatomical relationships compared with the dissection portion of the medical school course. However, it is noteworthy that only 5/28 (17.9%) reported it “much better.” This may suggest that our subjects found cadaveric dissection to have some utility for understanding 3D anatomical relationships [6, 14, 15]. These data support the findings of other studies suggesting dissection to be a valuable tool for learning 3D anatomical relationships and an important part of medical education.
There are benefits gained from the cadaveric dissection experience that are not presently incorporated into available VR software. Dissection remains a useful mechanism to experience the consistency and texture of organs [6]. Additionally, dissection provides training in manual dexterity through the use of blunt dissection, scissors, and scalpels. These skills allow students to learn the degree of physical contact that can damage or preserve human organs during manipulation. VR requires manual dexterity to use controllers, but the type of dexterity acquired through physical dissection can provide clinical skills [14]. Also, The encounter with the human cadaver in the dissection lab provides an educational platform for medical students to discuss mortality and get acquainted with the concept of death, which is a vital objective in medical education [14, 15]. Our VR module was designed as a supplement for anatomy instruction and we did not attempt to include these types of additional experiences into our VR environment. However, if future developers of VR anatomy tools intend to closely approximate experiences gained from cadaveric dissection, methods for including this type of content into VR will need to be explored. With many medical programs considering alternates to cadaveric education, the authors of this study believe this a particularly important area for future development and study.
While most of our data shows strong support for the VR module, it is noteworthy that not all subjects ranked it helpful. Four of the subjects reported VR unhelpful for learning anatomy and 3 out of 4 of these reported VR to be unhelpful for learning the names and locations of anatomical structures and 3D anatomical relationships. VR may not be uniformly appropriate for all learners. Kooi et al. [16] reported that viewing stereoscopic 3D images could result in visual discomfort. Additionally, Chittaro et al. [4] noted how head-mounted displays tend to have lower resolutions and this can make it discomforting to read text in a virtual platform. Our VR platform required subjects to read a moderate level of text, which could have contributed to some experiencing visual discomfort. Also, the study’s open-ended feedback section provided some additional clarification on why some subjects might have found VR unhelpful. A few subjects described difficulty in understanding how to use the controllers and how to navigate in the VR environment. Some indicated that they would have benefited from having additional time to get used to the VR controllers. For future studies, we recognize the need to provide a preliminary training session that includes exercises such as games or drawing pictures in a VR environment, before exposing the subjects to our anatomy platform. We believe this would provide a foundation that would help improve the user’s VR experience.
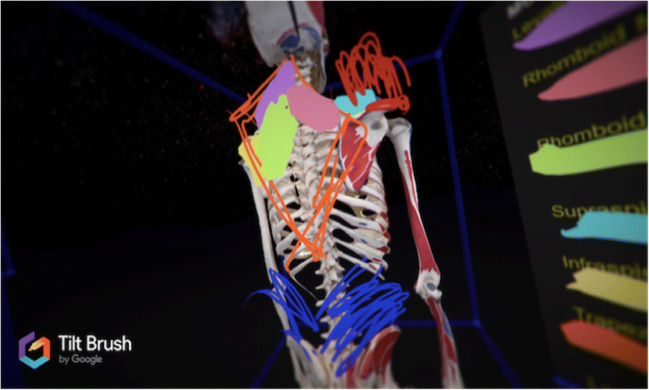
During the experiment, it was observed by the study researchers that some subjects had significant difficulty placing the drawing tool directly on the VR models (Fig. 4). Some had to be repeatedly guided to “paint closer to the skeleton” so that the muscle attached to the bone. The difficulty in perceiving the proximity of the paint to the model may be a shortcoming of the design of the VR module rather than the VR technology itself. We recognize that an important factor in the utility of the VR tool is the user interface and as a result, we hope to incorporate activities into future training sessions that improve the subjects’ perception of how close they are to objects in VR.
Fig. 4.
Drawings of the muscles on the virtual skeleton are not directly attached to the skeleton and appear to be drawn from a two-dimensional point of view
While observing the subjects interact with the VR platform, we noted how each subject used the technology uniquely. One subject started labeling vertebrae C1–T12 on the virtual skeleton to draw the attachment of the trapezius muscle. Another subject labeled and wrote out the name of each muscle in station 2 instead of drawing a line from the list of muscle labels (Fig. 5). This feature of VR reflects the findings of Bradley et al. [17], in which they report that VR simulations accommodate individual learning styles and allow users to learn at their own pace. The versatility we observed in our subjects’ use of VR and its ability to accommodate individual learning styles may well benefit the medical students who are developing their own methods for learning anatomy.
Fig. 5.
Subject directly labeled and wrote out the muscle names in station 2 instead of drawing a line from the list of muscle labels
Due to the nature of the recruitment process, this study may be susceptible to selection bias. An email was sent to 95 first-year medical students describing the study after which 28 voluntarily signed up. We did not control for confounding variables such as the subject’s experience, like or dislike of anatomy, VR, and technology. Subjects who were more enthusiastic about anatomy or the use of VR may have been more likely to pursue this opportunity. Also, subjects who had prior experience with VR might have benefited more from this experience, which could have biased their survey responses.
Conclusion
The subjects in this study reported VR as a helpful tool for learning the names and locations of anatomical structures and 3D anatomical relationships. There was a high preference for VR, rather than lecture and cadaveric dissection for learning 3D anatomical relationships. It is noteworthy that the majority of our subjects chose dissection to be “somewhat better” compared with “much better” suggesting that they held value to cadaveric dissection for learning 3D anatomical relationships. While we can postulate the benefits of replacing lecture, and potentially cadaveric dissection with VR, such advancement eliminates many important skills and psychosocial aspects that are currently obtainable through cadaveric dissection alone. VR technologies need further development and warrant an in-depth study before they can be extensively adopted into anatomy programs. Particularly we would like to see additional studies that directly compare VR technologies with cadaveric dissection courses.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
NA
Informed Consent
Yes, IRB-approved study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nicholson DT, Chalk C, Funnell WRJ, Daniel SJ. Can virtual reality improve anatomy education? A randomised controlled study of a computer-generated three-dimensional anatomical ear model. Med Educ. 2006;40(11):1081–1087. doi: 10.1111/j.1365-2929.2006.02611.x. [DOI] [PubMed] [Google Scholar]
- 2.Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ. 2017;10(6):549–559. doi: 10.1002/ase.1696. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman H, Vu D. Virtual reality: teaching tool of the twenty-first century? Acad Med. 1997;72(12):1076–1081. doi: 10.1097/00001888-199712000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Chittaro L, Ranon R. Web3D technologies in learning, education and training: motivations, issues, opportunities. Comput Educ. 2007;49(1):3–18. doi: 10.1016/j.compedu.2005.06.002. [DOI] [Google Scholar]
- 5.Silverstein JC, Ehrenfeld JM, Croft DA, Dech FW, Small S, Cook S. Tele-immersion: preferred infrastructure for anatomy instruction. J Comput High Educ. 2006;18(1):80–93. doi: 10.1007/BF03032725. [DOI] [Google Scholar]
- 6.Jastrow H, Hollinderbaumer A. On the use and value of new media and how medical students assess their effectiveness in learning anatomy. Anat Rec B New Anat. 2004;280(1):20–29. doi: 10.1002/ar.b.20027. [DOI] [PubMed] [Google Scholar]
- 7.Guimaraes B, et al. Rethinking anatomy: how to overcome challenges of medical education’s evolution. Acta Medica Port. 2017;30(2):134–140. doi: 10.20344/amp.8404. [DOI] [PubMed] [Google Scholar]
- 8.Hariri S, Rawn C, Srivastava S, Youngblood P, Ladd A. Evaluation of a surgical simulator for learning clinical anatomy. Med Educ. 2004;38(8):896–902. doi: 10.1111/j.1365-2929.2004.01897.x. [DOI] [PubMed] [Google Scholar]
- 9.Yammine K, Violato C. The effectiveness of physical models in teaching anatomy: a meta-analysis of comparative studies. Adv Health Sci Educ Theory Pract. 2016;21(4):883–95. [DOI] [PubMed]
- 10.Garg AX, Norman G, Sperotable L. How medical students learn spatial anatomy. Lancet. 2001;357(9253):363–4. [DOI] [PubMed]
- 11.Grogan K, Ferguson L. Cutting deep: the transformative power of art in the anatomy lab. J Med Humanit. 2018;39(4):417–30. [DOI] [PubMed]
- 12.Brewer DN, et al. Evaluation of neuroanatomical training using a 3D visual reality model. Stud Health Technol Inform. 2012;173:85–91. [PubMed]
- 13.Stepan K, Zeiger J, Hanchuk S, del Signore A, Shrivastava R, Govindaraj S, et al. Immersive virtual reality as a teaching tool for neuroanatomy. Int Forum Allergy Rhinol. 2017;7(10):1006–13. [DOI] [PubMed]
- 14.Ellis H. Teaching in the dissecting room. Clin Anat. 2001;14(2):149–51. [DOI] [PubMed]
- 15.McLachlan JC, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38(4):418–24. [DOI] [PubMed]
- 16.Kooi FL, Toet A. Visual comfort of binocular and 3D displays. Displays. 2004;25(2-3):99–108.
- 17.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–62. [DOI] [PubMed]