Abstract
Rationale and Objectives
Our goal was to determine whether use of the iPad would increase the students’ radiologic knowledge, aid in their interpretation of imaging exams, and increase learner satisfaction.
Material and Methods
iPads were pre-populated with ten image data sets, which included plain film, ultrasound, and CT of the head, chest, abdomen, and pelvis. The students, working in small groups, were charged with identifying the salient imaging findings, formulating a differential diagnosis, and choosing the most appropriate imaging modality, if further work-up was necessary. After the student group problem-solved for an hour, a faculty facilitator joined the group and reviewed the cases with them in an interactive fashion. Pre- and post- intervention tests were administered, and statistical analysis was performed.
Results
Student satisfaction surveys were administered to 125 students in the first 2 years of the study. These scores rated their assessment of the iPad exercise and ranged from 4.6 to 4.9 out of 5. The knowledge evaluation group included 219 students, 110 in the study group and 109 in the control group, in the latter 3 years of the study. The average improvement from the initial to the second test was 1.04 points among the control group and 2.32 among the study group, which was statistically significant (p = 0.0001).
Conclusion
We demonstrate increased learner satisfaction, as well as improved knowledge acquisition and interpretive skills of third year medical students engaged in hands-on learning using iPads.
Keywords: Education, Medical student, iPad
Introduction
Prior generations of medical students routinely sat for hours in large lecture halls taking notes and looking up answers to their questions in books. The internet has changed the educational landscape and transformed the learning styles of our current medical students. In many institutions, including our own, lectures are recorded and hence sparsely attended. The students can watch the lecture from the comfort of their apartment in a shorter amount of time. In contrast, the majority of current physician-educators are baby boomers or members of generation X who must strive to embrace the learning style that appeals to current students in order to produce intellectually curious, knowledgeable, and enthusiastic physicians.
This current generation of medical students needs to learn an exponentially larger body of knowledge than previous generations, and this trend will continue as scientific advances rapidly progress. Radiology educators cannot possibly impart all the necessary information during these limited hours of instruction. Our most important role as educators is to help the students develop the ability to reason and apply their knowledge. Our trainees must be lifelong learners, with a sound foundation of knowledge, critical thinking skills, and the ability to access the answers to their questions. As eloquently stated by PJ Salnetz in 2013, “An effective teacher of the millennial generation … must aim to facilitate learning rather than solely function as the expert” [1].
Traditionally, medical students rotating on a radiology clerkship listen to didactic lectures and observe the radiologist and residents reviewing imaging studies. In this environment, the learner is not actively engaged in the interpretative process. This familiar paradigm of instruction is in direct conflict with the preferred learning style of current medical students, who are millennial learners, with the internet at their fingertips, who thrive on self-directed learning, a form of active learning [2]. Their attention spans are limited, they are impatient, and they get bored quickly [1, 3]. According to the VARK model of learning styles, developed by Fleming, these students enjoy visual, aural, and kinesthetic channels to process information rather than only reading and writing [4].
In contrast, on other clinical rotations, the medical students are directly involved with active patient care: students on medicine, pediatrics, and surgery clerkships take histories; examine patients; participate in rounds; and even assist with procedures. They are directly working with patients and clinical teams, which requires them to integrate information and apply it to patient management. In comparison, the radiology clerkship has, by nature, been passive, with students less involved in direct patient care.
Radiology has a unique place in medical student education, as technology is an inherent component of our daily practice, and can be incorporated into the learning experience of these technologically savvy students. Blending technology and active learning principles, by using simulation training, more closely mirrors clinical practice. Simulation provides “understanding through practice in realistic situations” as described in the constructivist theory of education [5–9]. Surgical clerkships and residencies commonly use simulation techniques to teach procedures and reinforce concepts. However, few computer-based simulation models have been designed for radiology [1, 9]. The goal of our study was to incorporate a simulation model into our existing clerkship curriculum, combining technology with active learning.
In the ideal radiology clerkship, after the students were taught the fundamentals of chest x-ray and cross-sectional anatomy as well as common pathology, they would be assigned a set of representative images to analyze independently or in small groups in order to apply their newly acquired knowledge, rather than just watch the radiologist point out findings and dictate cases. In our institution, a very busy academic institution in a poor, urban environment, space and resources for medical student education are scarce. No idle Picture Archiving and Communicating System (PACs) workstations are available for medical students to independently review cases. There is not an abundance of funds to purchase additional workstations solely for teaching purposes. Buying a set of iPad- or Android-compatible devices for each clerkship location, which we would preload with representative imaging cases, is a rather low-cost investment and would simulate the real-life practice of a radiologist more closely than a lecture format.
In our medical school, third year medical students have a 2-week radiology clerkship, at one of three different sites. Each group is composed of 4–6 students at each site. The objectives of this required clerkship include the following: learning about plain film and cross-sectional imaging interpretation, radiation safety, and the American College of Radiology (ACR) Appropriateness Criteria. Our curriculum consists of a set of didactic lectures, dedicated time reviewing cases with attendings and residents at the PACs workstation, and observing procedures.
In our study, third year medical students, during their radiology clerkship, used iPads to simulate the radiologist’s experience at the workstation, using their knowledge to analyze images and make accurate observations and diagnoses in a team-based setting. We harnessed the millenials’ familiarity with technology while encouraging active learning of radiology fundamentals, which we hypothesized would result in a higher level of comprehension in a more positive learning environment. Our goal was to determine whether use of a faculty-facilitated iPad excercise would increase the students’ radiologic knowledge, aid in interpretation of imaging exams, and increase learner satisfaction.
Material and Methods
Study Setting
Our study took place at two separate academic, inner city medical centers under the umbrella of a single medical school. The educational initiative was held in a small conference room in the radiology department with a circular table to enhance student collaboration.
Study Design
The iPads were purchased as part of two educational grants awarded to us by the medical school. At the time that the study was initiated, the iPad was the optimal platform for the available imaging application. However, currently, there are multiple tablets with applications that can be used for this purpose. The iPads were pre-populated with ten image data sets, using the Dicom viewer OsiriX©, which included plain film, ultrasound, and CT of the head, chest, abdomen, and pelvis. Cases included subarachnoid hemorrhage, tuberculosis, pleural effusion, ruptured aortic aneurysm, ruptured viscous, hydronephrosis, and bladder cancer. Each student was given an iPad to use during the exercise. The students had the ability to manipulate imaging parameters on the iPad, in a manner similar to radiologists at the workstation. The students, working in small groups, in a conference room, needed to know radiographic anatomy in order to identify the salient imaging findings, as well as formulate a differential diagnosis, and choose the most appropriate imaging modality for further work-up. After the student group problem-solved for an hour, a faculty facilitator joined the group and reviewed the cases with them in an interactive fashion. Our goal was to enable our students to be active thinkers, who can apply their knowledge as they move toward increased patient responsibility and independence.
Data Collection
During the first 2 years of this iPad study, a student satisfaction survey, which was anonymous, was administered after completion of the iPad exercise, to determine if the students enjoyed the activity and considered it educationally worthwhile (Table 1). Knowledge acquisition was not evaluated in this initial part of the study.
Table 1.
Student satisfaction survey (n = 125)
| iPad exercise | Strongly disagree (%) | Disagree (%) | Neutral (%) | Agree (%) | Strongly agree (%) |
|---|---|---|---|---|---|
| Was enjoyable | 0 | 0 | 0 | 18 (14.7) | 107 (85.3) |
| Helped me learn | 0 | 0 | 4 (3) | 26 (20.5) | 95 (76.5) |
| Improved my ability to analyze images | 0 | 0 | 4 (3) | 36 (29.4) | 85 (67.6) |
| Was time efficient | 0 | 0 | 7 (5.9) | 18 (14.7) | 100 (79.4) |
| Gave me the opportunity to participate in my own learning | 0 | 0 | 0 | 22 (17.6) | 103 (82.4) |
During the subsequent 3 years of the study, students were given a 10-question multiple-choice image-rich pre-test to determine their baseline knowledge. On days 3–5 of the clerkship, students participated in the iPad exercise. On day 8 of the clerkship, the students took a 10-question image-based multiple-choice post-test identical to the pre-test. These tests were anonymous. Tests were scored in a range from 0 to 10, with 10 meaning all were correct answers and 0 meaning there were no correct answers. The test scores did not affect the students’ grades.
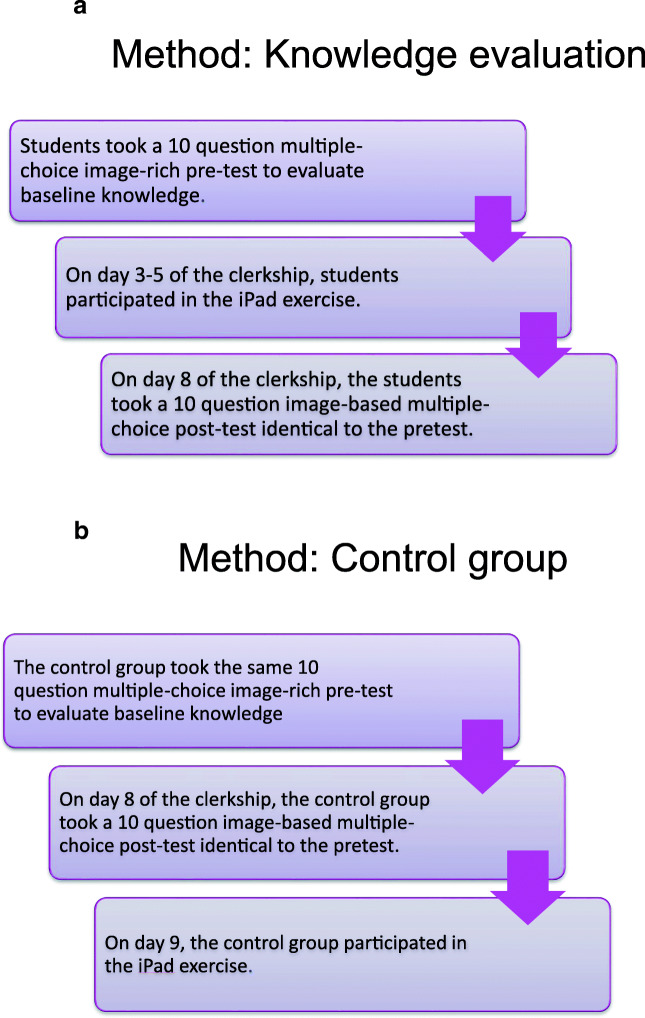
The methodology of the study differed on alternate months of the radiology clerkship to enable us to have a control group of students. To eliminate the effect of increasing medical student knowledge over the course of the academic year, the control groups were matched to the study group by the number of completed clinical rotations. The difference between the groups was that the control group took the post-test before participating in the iPad exercise while the study group performed the iPad exercise and then took the post-test. There was no other difference in the curriculum between the two groups (Fig. 1a, b). We calculated the difference in scores between the study and control groups.
Fig. 1.
a Study group design. The students took a pre-test, and then participated in the iPad exercise several days later. They took a post-test at the end of the clerkship. b Control group design. These students took a pre-test, and then a post-test toward the end of the clerkship. These students participated in the iPad exercise after the post-test
Data Analysis
Statistical analysis was performed using a paired T test to compare the difference between the pre- and post-test scores between the two groups, as well as the initial test scores between the two groups.
This study received exempt status from the Institutional Review Board. Informed consent was not required.
Results
Satisfaction surveys were administered to 125 students in the first 2 years of the study to rate their assessment of the iPad exercise (Table 1). The scores ranged from 4.6 to 4.9 out of 5, with 5 signifying the strongest approval. For example, the mean rating for student enjoyment of the exercise was 4.9 and the mean rating for increasing their ability to analyze images was 4.7. The student satisfaction surveys were not given to the students in the second phase of the study, as it was clearly evident from the first 2 years of the study that the students enjoyed this learning experience, and consistently rated it highly.
The knowledge evaluation group included 219 students, 110 in the study group and 109 in the control group, in the latter 3 years of the study. All but 4 students in the study group completed both pre- and post-tests, resulting in a total of 215 students. We found no statistical significant difference (p value = 0.315) in initial scoring between the study (mean = 6.92) and control (mean = 6.71) groups. In the post-tests, the study group achieved an average of 9.24, a 2.32-point improvement, while the control groups had an average of 7.75, a 1.04-point improvement. This difference is statistically significant at p value = 0.0001. The results are summarized in Table 2.
Table 2.
Knowledge evaluation scores
| Group | No. of subjects | Mean pre-test (SD) | Mean post-test (SD) | Post- minus pre-test mean (SD) |
|---|---|---|---|---|
| Study group | 106 | 6.92 (1.45) | 9.24 (0.89) | 2.32 (1.72) |
| Control group | 109 | 6.71 (1.49) | 7.75 (0.43) | 1.04 (1.74) |
| p values | 0.35 | 7.69 × 10−5 |
Discussion
This prospective study used iPad technology to promote self-directed learning of basic radiologic concepts to third year medical students. We demonstrated improved test scores in plain film and cross-sectional imaging interpretation as well as high learner satisfaction. In our study, we evaluated the higher levels of learning, which require application, synthesis, and analysis as described in Bloom’s taxonomy, rather than merely knowledge acquisition [10]. Our data mirrors the Kirkpatrick Model of evaluation in which level 1 assesses learner satisfaction and level 2 evaluates changes in knowledge and skills [11].
Review of the literature reveals that some medical schools have incorporated active educational techniques into their curriculum, such as audience response systems, jeopardy-type games, on-line cases, and computer simulation. One institution used simulations to enhance radiology resident training and preparation for on-call responsibility [12]. In that study, a computer-based teaching file of pulmonary imaging cases, with clinical information readily accessible, was utilized to teach the residents and fellows. Recently, Friedman et al. [13] created an interactive workstation for medical students with musculoskeletal radiology cases. They found an improvement in student competency scores and an increase in learner satisfaction in this active learning group compared with a control group, who passively observed radiologists in the reading room. Our study confirms the findings of Friedman et al. with an even larger study population.
Engaging these millennial learners in an enriching hands-on learning experience during their radiology clerkship gives students the experience of being a radiologist, as well as demonstrates our role within the larger healthcare community. In our study, the students first discuss the cases as a group, mirroring the collaborative setting in which many radiologists work, sharing ideas and opinions with colleagues. The students can manipulate the windows and levels of the images of CT cases on the iPads, as well as measure Hounsfield units, to best perceive the findings, and arrive at a diagnosis, similar to the radiologist in day-to-day practice. This interactive exercise enables the students to receive feedback about their knowledge and interpretive skills in a timely fashion, with the aid of a faculty facilitator.
Our clerkship takes place at several different sites with different patient populations, faculty, and resources, a scenario common throughout the country. A common complaint regarding medical student education in the clinical years concerns the lack of standardization of the students’ educational experience and evaluation across sites. Specifically, the content of the clerkship is not identical between sites due to different patient populations, and, therefore, different imaging studies encountered. Also, evaluation across sites may be variable, as the radiologists, who are the evaluators, are different at the various sites. The combination of dedicated radiologist-educators facilitating discussion and interpretation of a standard set of images loaded on iPad or Android devices can aid in standardization of the curriculum and grading across teaching sites. There are numerous imaging programs compatible with iPad or Android devices. These include Osirix, which we used, and Horos, but the landscape is evolving quickly, and it is worthwhile to review available options when implementing a program.
Our study has some limitations. The medical students in our study all attended the same medical school, which may limit the generalizability of our results. In addition, as the study spanned a 2-week radiology clerkship, long-term learning and skill acquisition was not evaluated. Lastly, the faculty facilitators in our study were the clerkship director and site leaders, all very invested in the success of the rotation, and with dedicated time for educational initiatives.
The radiologist-educator needs to become familiar with current educational theory and its effective implementation. Creation of active learning tools requires time and creativity for optimal content development, which is a different skill set and mind set than when creating a PowerPoint presentation for a didactic lecture. There is a difference in the amount of time required by faculty to develop active teaching tools compared with the familiar didactic lecture format [3]. With time, the development of these new active learning exercises will become more routine and an intrinsic part of graduate medical education in radiology.
Conclusion
Our study, which has a large study population with data accumulated over 5 years, reinforces the existing clinical radiology literature. We demonstrate increased learned satisfaction as well as improved knowledge acquisition and interpretive skills of third year medical students engaged in hands-on learning using iPads. There are numerous imaging applications constantly being developed; before instituting a tablet-based initiative, it is worthwhile to thoroughly review available options. The benefits are potentially large, not only for the trainees and their teachers but also potentially for the future of radiology education.
Funding Information
This study was funded by an educational grant from Albert Einstein College of Medicine, which provided the funds for the purchase of 10 iPads.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was granted exemption by the Institutional Review Board of Montefiore Medical Center/Albert Einstein College of Medicine which certified that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Slanetz PJ, Kung J, Eisenberg R. Teaching radiology in the millennial era. Acad Radiol. 2013;20:26–34. doi: 10.1016/j.acra.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Van Hout-Wolters B. Simons RJ., Volet S. Active learning: self-directed learning and independent work. In: Simons RJ, van der Linden J, Duffy T, editors. New learning. Dordrecht: Springer; 2000. p. 21–36.
- 3.Fischer R, Jacobs S, Herbert W. Small-group discussion versus lecture format for third-year students in obstetrics and gynecology. Obstet Gynecol. 2004;104:349–353. doi: 10.1097/01.AOG.0000133485.02727.ba. [DOI] [PubMed] [Google Scholar]
- 4.Dantas, LA, Cunha A. An integrative debate on learning styles and the learning process. Soc Sci Humanit Open 2.1 ,2020; 100017.
- 5.Gunderman RB. The fight for education. AJR. 2001;176:23–26. doi: 10.2214/ajr.176.1.1760023. [DOI] [PubMed] [Google Scholar]
- 6.Gunderman RB, Kang Y, Fraley RE, et al. Instructional technology and radiologic education. Radiology. 2001;221:1–4. doi: 10.1148/radiol.2211010366. [DOI] [PubMed] [Google Scholar]
- 7.Collins J. Education techniques for lifelong learning: principles of adult learning. Radio Graphics. 2004;24:1483–1489. doi: 10.1148/rg.245045020. [DOI] [PubMed] [Google Scholar]
- 8.Williamson KB, Gunderman RB, Cohen MD, Frank MS. Learning theory in radiology education. Radiology. 2004;233:15–18. doi: 10.1148/radiol.2331040198. [DOI] [PubMed] [Google Scholar]
- 9.Bedi HS, Yucel EK. I just bought my residents iPads … now what? The integration of mobile devices into radiology resident education. AJR. 2013;201:704–709. doi: 10.2214/AJR.13.10674. [DOI] [PubMed] [Google Scholar]
- 10.Adams N. Bloom’s taxonomy of cognitive learning objectives. J Med Libr Assoc. 2015;103(3):152–153. doi: 10.3163/1536-5050.103.3.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ragsdale, JB, Berry, A, Gibson J, et al, Representing the Program Evaluation Special Interest Group of the Southern Group on Educational Affairs (SGEA) within the Association of American Medical Colleges (AAMC) (2020) Evaluating the effectiveness of undergraduate clinical education programs, Med Educ Online, 25:1, 10.1080/10872981.2020.1757883. [DOI] [PMC free article] [PubMed]
- 12.Rojas C, Jawad H, Chung J. The new era of radiology teaching files. AJR. 2012;198:773–776. doi: 10.2214/AJR.11.7409. [DOI] [PubMed] [Google Scholar]
- 13.Friedman MV, Demertzis J, Hillen TJ, et al. Impact of an interactive diagnostic case simulator on a medical student radiology rotation. AJR. 2017;6:1256–1261. doi: 10.2214/AJR.16.17537. [DOI] [PubMed] [Google Scholar]