Abstract
Physician burnout is a widespread problem. We examined how coping, mentorship, and life events correlated with burnout in Internal Medicine Residents. We performed a cross-sectional study of survey data collected over multiple time points and used Spearman correlation of coping, mentorship, and life events to emotional exhaustion (EE) and cynicism (CYN). Burnout was assessed using the Maslach Burnout Inventory–General Survey (MBI-GS), coping skills were measured using the Brief COPE, mentorship with an institutional mentoring survey, and life events with a shortened Social Readjustment Rating Scale (SRRS). Two thousand one surveys were distributed to 616 residents from 2010 to 2015. There were 1144 cases of completion of both the Brief COPE and the MBI-GS (58%), 744 of the MBI-GS and the Mentoring survey (47%), and 1138 of the MBI-GS and Life Events Scale (57%). There were correlations between acceptance (ρ 0.1–0.24), denial (ρ 0.13–0.20), substance abuse (ρ 0.15–0.22), behavioral disengagement (ρ 0.18–.037), self-blame (ρ 0.27–0.45), self-distraction (ρ 0.18–0.32) and venting (ρ 0.15–0.47) and EE. There were correlations with acceptance (ρ 0.11–0.15), denial (ρ 0.18–0.26), humor (ρ 0.13–0.20), substance abuse (ρ 0.10–0.29), behavioral disengagement (ρ 0.19–0.40), self-blame (ρ 0.24–0.35), self-distraction (ρ 0.14–0.34) and venting (ρ 0.12–0.38) and CYN. There was a negative correlation between mentorship and EE (ρ − 0.15, − 0.18) and CYN (ρ − 0.30 to − 0.20). There were correlations between life events and EE (ρ 0.15–0.20) and CYN (ρ = 0.14–0.15). Maladaptive coping mechanisms, acceptance, and life stressors correlate with burnout in internal medicine residents and mentoring may be protective.
Keywords: Wellness, Burnout, Graduate medical education, Mentorship, Coping
Introduction
Burnout is a syndrome of emotional exhaustion, cynicism, and a low sense of accomplishment caused by work-related stress [1]. It is a well-known and well-studied phenomenon affecting more than half of all physicians at all levels of training and practice [2, 3]. It is known to increase the risk of medical errors, decrease physician productivity, increase attrition, and contribute to depression and suicide [4–8]. Preventing burnout is likely multifactorial consisting of national, institutional, and individual components [9, 10]. Our study evaluates how coping, mentorship, and life events correlate with burnout in internal medicine (IM) residents.
Coping is how we deal with stress and may affect burnout [11–13]. The usefulness of a specific coping mechanism varies based on the individual and the situation; however, they can be grouped into adaptive and maladaptive. Adaptive coping mechanisms include acceptance, active coping, planning, positive reframing, religion, seeking emotional support, and seeking instrumental support. Maladaptive coping mechanisms include behavioral disengagement, denial, humor, self-blame, self-distraction, substance abuse, and venting [14–18]. Few studies have looked at coping and burnout in IM residents. One study showed acceptance, active coping, and positive reframing inversely correlated with burnout, while denial, behavioral disengagement, self-blame, and humor correlated with burnout [13]. In another study, residents reported that a lack of coping skills contributed to their burnout [19]. Our study aims to assess how coping affects burnout in IM residents.
While experts agree that mentorship needs to be a component to wellness interventions [20], no studies have measured how mentorship affects burnout in IM residents. In surgical trainees, the absence of a formal mentorship program has been associated with higher levels of burnout [21]. Additionally, strong mentorship is considered essential for the development of early career general internists [22] and has been linked to higher levels of satisfaction in academic physicians across all specialties [23]. For IM residents, successful mentorship has been associated with an increased likelihood to enter a career in IM [24], and increased perceived career preparation [25]. Our study correlates resident-reported mentorship satisfaction with burnout.
Residents experience not only work-related but also life-related stress. Life events like marriage, moving, loss of a loved one, and having children are common occurrences in residency. They have been shown to be associated with burnout in medical students [26], but they have not been studied in IM residents.
At the University of Pittsburgh, we screened residents for burnout from 2010 to 2015 as a part of a battery of surveys that also included measurement of coping, mentoring, and life events. We hypothesized that adaptive coping and mentorship would be protective against burnout while maladaptive coping and life stress would correlate with burnout.
Methods
IM, transitional, preliminary year, and medicine-pediatrics residents at a large academic facility were surveyed from 2010 to 2015 using the Maslach Burnout Inventory–General Survey (MBI-GS), the Brief COPE, a mentoring survey, and a shortened Social Readjustment Rating Scale (SRRS). The residents were contacted by email with reminder emails sent. Residents were surveyed annually in June beginning prior to the start of their intern year. We included surveys completed prior to the intern year until the end of the third post graduate year.
The surveys were used to screen residents for burnout and therefore, the surveys were not anonymous. The results were shared with the resident, their advisor, and the program director. There has been diligent faculty education regarding interpretation of the surveys, processing of results, resident counseling, and mentorship. Residents met with their mentors every 6 months.
This research was reviewed by the University of Pittsburgh IRB and considered exempt. IRB#PRO12030703.
Burnout
The Maslach Burnout Inventory–General Survey (MBI-GS), considered the gold standard and well validated, was used to measure burnout [27, 28]. Burnout is measured on three subscales: emotional exhaustion (EE), cynicism (CYN), and professional efficacy. A person with a high level or burnout on the EE or CYN subscale is considered to have at least one manifestation of professional burnout [2]. Scores of 3.20 or higher on EE and 2.20 or higher on CYN indicate high levels of burnout [27].
Coping
Coping was assessed using the Brief COPE, a 28-item inventory measuring 14 different coping mechanisms on a 4-point Likert scale. The use of each coping mechanism ranges from 2 to 8 with higher values indicating more frequent use [14]. Psychometric properties of the Brief COPE have been studied, and the scales show good internal consistency and validity [14].
Mentorship
Mentorship was measured using an institutional mentoring survey that asked 7 questions on a 5-point Likert scale. Residents were asked how helpful their faculty mentor was in terms of providing professional guidance, providing feedback, discussing academic and nonacademic career options, and identifying research topics. It also assessed if the resident felt the mentor was effective in his/her role, met the resident’s needs, and if they had been satisfied with the mentorship. Higher scores on the mentoring survey indicate greater resident satisfaction with their mentor. This survey was distributed annually starting at the end of the first post graduate year.
Life Events
The Social Readjustment Rating Scale (SRRS) assessed the occurrence of life events in the last year. Our survey only included a subscale of the events: divorce, child birth, serious personal illness or injury, serious illness or injury of a loved one, death of a loved one, marital separation, moving, marriage, miscarriage, spouse starting or stopping work, financial difficulty, and death of a child. Higher scores indicate more stressful life events [29].
Statistical Analysis
Results were stratified into post graduate year (PGY) level. Those survey results from the beginning of the intern year were labeled as PGY-0. We used Spearman correlation to determine the relationship between EE and CYN with coping mechanisms, mentorship, and life events. A small association was considered to have a rho coefficient from 0.1 to 0.29, a moderate association from 0.30 to 0.49, and a strong association of greater than 0.5 [30]. For all analyses, we used Stata/SE 14.0 (StataCorp, College Station, Texas) and we considered a p value of < 0.05 to be significant.
Results
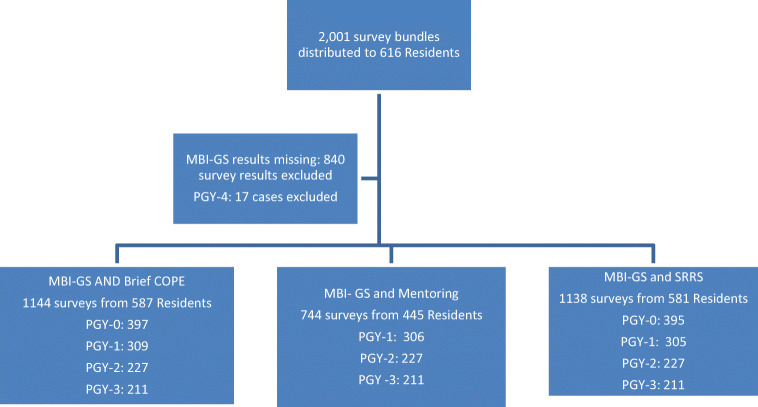
From 2010 to 2015, 2001 surveys were distributed to 616 IM, transitional, preliminary year, and medicine-pediatrics residents. Burnout data was missing in 840 cases so these were excluded. There were 17 surveys from PGY-4 residents also excluded. There were 1144 cases of completion of both the Brief COPE and the MBI-GS by 587 residents. There were 744 cases of completion of both the MBI-GS and the Mentoring survey by 445 residents and 1138 cases from 581 residents of the MBI-GS and Life Events Scale (Fig. 1). Of all the surveys analyzed, 566 (49.5%) were from male residents, 681 (61%) were from white residents, and 65% were from categorical residents. For full demographic data, see Table 1.
Fig. 1.
Surveys distributed to internal medicine, transitional, preliminary year, and medicine pediatric residents from 2010 to 2015. MBI-GS is the Maslach Burnout Inventory–General Survey used to measure burnout. Brief COPE measures coping mechanism use. Mentoring refers to an institutional survey measuring resident reported satisfaction with their mentor. SRRS is the Social Readjustment rating scale, also called the Holmes and Rahe Social Readjustment Rating Scale, measures life events
Table 1.
Demographic characteristics
| All (n = 1144) | PGY-0 (n = 397) | PGY1 (n = 309) | PGY2 (n = 227) | PGY3 (n = 211) | |
|---|---|---|---|---|---|
| PGY level, n (%) | |||||
| New intern | 397 (34.7%) | ||||
| PGY 1 | 309 (27.0%) | ||||
| PGY 2 | 227 (19.8%) | ||||
| PGY 3 | 211 (18.4%) | ||||
| Gender | |||||
| Male | 566 (49.5%) | 200 (50.4%) | 154 (49.8%) | 112 (49.3%) | 100 (47.4%) |
| Female | 574 (50.2%) | 194 (48.9%) | 154 (49.8%) | 115 (50.7%) | 111 (52.6%) |
| No response | 4 (0.3%) | 3 (0.8%) | 1 (0.3%) | 0 (0.0%) | 0 (0.0%) |
| Race, n (%) | |||||
| White | 698 (61.0%) | 247 (62.2%) | 182 (58.9%) | 139 (61.2%) | 130 (61.6%) |
| African American | 45 (3.9%) | 16 (4.0%) | 14 (4.5%) | 10 (4.4%) | 5 (2.4%) |
| Asian | 301 (26.3%) | 100 (25.2%) | 92 (29.8%) | 54 (23.8%) | 55 (26.1%) |
| Othera | 96 (8.4%) | 31 (7.8%) | 20 (6.5%) | 24 (10.6%) | 21 (9.9%) |
| No response | 4 (0.3%) | 3 (0.8%) | 1 (0.3%) | 0 (0.0%) | 0 (0.0%) |
| Track | |||||
| Categorical | 754 (65.9%) | ||||
| Med Peds | 72 (6.3%) | ||||
| Preliminary | 66 (5.8%) | ||||
| Transitional | 65 (5.6%) | ||||
| Neurology | 15 (1.3%) | ||||
| Radiology | 14 (1.2%) | ||||
| Dermatology | 10 (0.9%) | ||||
| Anesthesiology | 4 (0.3%) | ||||
|
Physical medicine and rehabilitation No response |
4 (0.3%) 140 (12.2%) |
||||
aOther: Native Hawaiian or Pacific Islander, Native Indian, other races, or multiple races
Burnout
There was burnout data for at least one time point on 587 of the 616 residents (95%). Of the 1984 surveys distributed to incoming interns, PGY-1, PGY-2, and PGY-3 residents, there were 1144 survey responses (58%). Residents with high scores on EE or CYN subscales met criteria for professional burnout. In the pre-intern assessment, 8.3% and 7.1% had high levels of EE and CYN respectively. At the end of PGY-1, 21.7% and 23.6% had high levels of EE and CYN. At the end of PGY-2, 15% and 22.5% had high levels of EE and CYN. At the end of PGY-3, 13.7% and 16.1% had high levels of EE and CYN (Table 2).
Table 2.
Emotional exhaustion and cynicism by PGY level
| PGY-0 (n = 397) | PGY-1 (n = 309) | PGY-2 (n = 227) | PGY-3 (n = 211) | |
|---|---|---|---|---|
| Emotional exhaustion | ||||
| Low ≤ 2.0 | 299 (75.3%) | 159 (51.5%) | 141 (62.1%) | 139 (65.9%) |
| Moderate 2.01–3.19 | 65 (16.4%) | 83 (26.9%) | 52 (22.9%) | 43 (20.4%) |
| High ≥ 3.2 | 33 (8.3%) | 67 (21.7%) | 34 (15%) | 29 (13.7%) |
| Cynicism | ||||
| Low ≤ 1.0 | 258 (65.0%) | 135 (43.7%) | 102 (44.9%) | 107 (50.7%) |
| Moderate 1.01–2.19 | 111 (28.0%) | 101 (32.7%) | 74 (32.6%) | 70 (33.2%) |
| High ≥ 2.2 | 28 (7.1%) | 73 (23.6%) | 51 (22.5%) | 34 (16.1%) |
Burnout and Coping
There was coping data on all the residents who completed the MBI-GS (Table 3). There were small correlations between acceptance (ρ 0.1–0.24), denial (ρ 0.13–0.20), and substance abuse (ρ 0.15–0.22) and EE. There were small to moderate correlations with behavioral disengagement (ρ 0.18–.037), self-blame (ρ 0.27–0.45), self-distraction (ρ 0.18–0.32) and venting (ρ 0.15–0.47) and EE.
Table 3.
Spearman correlation between coping mechanisms and emotional exhaustion (EE) and cynicism (CYN)
| Coping mechanism | PGY-0 (n = 397) ρ | PGY-1 (n = 309) ρ | PGY-2 (n = 227) ρ | PGY-3 (n = 211) ρ |
|---|---|---|---|---|
| Acceptance | ||||
| EE | 0.10* | 0.20** | 0.13* | 0.24** |
| CYN | 0.11* | 0.15** | 0.13* | 0.15* |
| Active coping | ||||
| EE | 0.06 | − 0.002 | 0.09 | 0.13* |
| CYN | 0.02 | − 0.01 | 0.06 | 0.09 |
| Planning | ||||
| EE | 0.11* | 0.04 | 0.05 | 0.10 |
| CYN | 0.06 | 0.02 | 0.01 | − 0.02 |
| Positive reframing | ||||
| EE | 0.10* | 0.01 | 0.003 | 0.09 |
| CYN | − 0.01 | − 0.01 | − 0.03 | 0.02 |
| Religion | ||||
| EE | − 0.03 | − 0.09 | − 0.01 | − 0.10 |
| CYN | − 0.05 | − 0.05 | 0.01 | − 0.13* |
| Emotional support | ||||
| EE | 0.07 | 0.09 | 0.04 | 0.14* |
| CYN | − 0.04 | 0.01 | − 0.01 | 0.06 |
| Instrumental support | ||||
| EE | 0.11* | 0.05 | 0.05 | 0.10 |
| CYN | − 0.04 | − 0.01 | 0.01 | 0.03 |
| Behavioral disengagement | ||||
| EE | 0.18** | 0.22** | 0.25** | 0.37** |
| CYN | 0.19** | 0.21** | 0.32** | 0.40** |
| Denial | ||||
| EE | 0.13* | 0.07 | 0.13* | 0.20** |
| CYN | 0.18** | 0.10 | 0.26** | 0.18* |
| Humor | ||||
| EE | 0.13* | 0.16** | 0.12 | 0.11 |
| CYN | 0.13* | 0.21** | 0.20** | 0.20** |
| Self-blame | ||||
| EE | 0.27** | 0.27** | 0.30** | 0.45** |
| CYN | 0.25** | 0.24** | 0.32** | 0.35** |
| Self-distraction | ||||
| EE | 0.18** | 0.25** | 0.20** | 0.32** |
| CYN | 0.14** | 0.17** | 0.24** | 0.34** |
| Substance abuse | ||||
| EE | 0.03 | 0.22** | 0.15* | 0.22** |
| CYN | 0.10* | 0.21** | 0.18* | 0.29** |
| Venting | ||||
| EE | 0.15** | 0.34** | 0.25** | 0.47** |
| CYN | 0.12* | 0.31** | 0.25** | 0.38** |
*p < 0.05
**p < 0.005
There were small correlations with acceptance (ρ 0.11–0.15), denial (ρ 0.18–0.26), humor (ρ 0.13–0.20), and substance abuse (ρ 0.10–0.29) and CYN. There were small to moderate correlation with behavioral disengagement (ρ 0.19–0.40), self-blame (ρ 0.24–0.35), self-distraction (ρ 0.14–0.34) and venting (ρ 0.12–0.38) and CYN.
Burnout and Mentorship
There was mentoring data for at least one time point on 445 of the 616 residents (72%). There were 744 cases of completion of both the Mentoring survey and the MBI-GS out of 1587 surveys distributed (47%). There was a small negative correlation between mentorship and EE at the end of PGY-1 and PGY-2 (ρ = − 0.15 and − 0.18). There was a small to moderate negative correlation between mentorship and CYN at all time points (ρ = − 0.22, − 0.30, and − 0.20). (Table 4).
Table 4.
Spearman correlation between mentorship and life events with emotional exhaustion and cynicism
| PGY-0 (n = 395) | PGY-1 (n = 306) | PGY-2 (n = 227) | PGY-3 (n = 211) | |
|---|---|---|---|---|
| Mentorship | ||||
| EE | − 0.15* | − 0.18* | − 0.04 | |
| CYN | − 0.22** | − 0.30** | − 0.20** | |
| Life events | (n = 305) | |||
| EE | 0.15** | 0.16* | 0.20** | 0.10 |
| CYN | 0.14** | 0.11 | 0.15* | 0.02 |
*p < 0.05
**p < 0.005
Burnout and Life Events
There was life events data for at least one time point on 581 of the 616 residents (94%). There were 1138 surveys with burnout and life events data completed out of the 1984 surveys distributed (57%). There was a small correlation between life events and EE prior at PGY-0 (ρ = 0.15), at the end of PGY-1 (ρ = 0.16), and PGY-2 (ρ = 0.20). There was a small correlation between life events and CYN at PGY-0 (ρ = 0.14) and at the end of PGY-2 (ρ = 0.15). (Table 4).
Discussion
Our study looked at correlation of resident burnout with coping, mentorship, and life events. We found that acceptance and maladaptive coping mechanisms correlated with burnout. The strongest correlations were seen with behavioral disengagement, self-blame, self-distraction, and venting. We found that mentorship inversely correlated with burnout and life events correlated with burnout.
Coping mechanisms are grouped into adaptive and maladaptive. Acceptance, thought to be adaptive, correlated with burnout in our study. The use of this coping mechanism may indicate the resident is giving up, which may be maladaptive in IM residents. Our findings differ from a prior study of IM residents that found a small negative correlation with burnout and acceptance. While our correlation was small, it was consistent throughout all time points in both subdomains of burnout.
We found all maladaptive coping strategies correlated with burnout. The most harmful strategies were behavioral disengagement, self-blame, self-distraction, and venting. Medical educators should be screening for the use of these coping mechanisms, formally or informally, and adaptive coping should be encouraged. There are many factors that are out of our control when it comes to burnout, but coping is not one of them. Coping mechanisms can be taught and have been shown to decrease burnout in physicians [12, 31]. While efforts should be made from an institutional level to decrease stressors inherent to training, efforts also should be made on how to counsel our trainees to deal with stress.
We found resident self-reported satisfaction with their faculty mentor was protective against burnout. While this has been postulated in prior studies, ours is the first to show this objectively. While meeting with mentors and being involved in scholarly projects has not been shown to affect burnout in residents [13], we believe our study shows that satisfaction with mentorship may be protective against burnout.
While burnout is defined as a syndrome caused by work-related stress, life-related stressors have been shown to contribute to burnout in medical students [16]. We found a small correlation between life stress and burnout. We scored the SRRS as per convention with different values given to different events, with more stressful events receiving more points. We did not however divide the events into those that may be perceived as positive (marriage, birth of a child) to those that may be perceived as negative (divorce, death of a loved one). This may have affected our results.
The limitations of our study include that it is a single-center study and we used non-anonymous self-reported data. Strengths of our study include a high number of participants and a good response rate. Our data were gathered over 6 years and included IM, preliminary, transitional, and medicine-pediatrics residents, which increases its generalizability.
Conclusion
Maladaptive coping mechanisms, acceptance, and life stressors correlate with burnout in internal medicine residents. Mentoring may be protective against burnout. Those involved in graduate medical education need to discourage the use of maladaptive coping mechanisms and promote programs to ensure resident satisfaction with mentorship. They need to be aware that life events contribute to burnout and those residents experiencing life stressors may benefit from extra support.
Acknowledgments
The authors wish to thank Kwonho Jeong, MS, Data Analyst at the University of Pittsburgh Center for Research on Health Care Data Center, for his assistance with statistical analysis. We thank Shanta Zimmer, MD (University of Colorado), Asher Tulsky, MD (Boston University), and Jennifer Corbelli, MD, MS, (University of Pittsburgh) for initiating the wellness screening program and distributing the surveys to internal medicine residents at the University of Pittsburgh.
Authors’ Contributions
All authors made sufficient contributions for authorship. All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Brielle Spataro, Sarah Tilstra, Doris Rubio, and Melissa McNeil. The first draft of the manuscript was written by Brielle Spataro and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research was funded using an internal Division of General Internal Medicine research award. The authors report no external sources of funding for this study.
Data Availability
All surveys and results can be made available for review.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
This research was reviewed the by University of Pittsburgh IRB and was deemed to be exempt.
Consent to Participate
This research was reviewed by the Pittsburgh IRB and was considered to be exempt.
Consent for Publication
No identifiable personal data is included in our study.
Code Availability
For all analyses, we used Stata/SE 14.0 (StataCorp, College Station, Texas).
Footnotes
Previous Presentations
Portions of this research were presented as an oral abstract at the annual Society of General Internal Medicine Meeting, in April 2017 in Washington D.C.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 3.Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt RD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513–519. doi: 10.1016/S0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 5.Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dyrbye LN, Massie FS, Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–1180. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 7.Dyrbye LN, West CP, Satele D, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med. 2008;149:334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 8.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, Shanafelt TD. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 9.West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Hellyer JMH, Sloan JA, Shanafelt TF. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 10.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 11.Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. 2017;6:144. doi: 10.1186/s13643-017-0526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Isaksson Ro KE, Tyssen R, Hoffart A, Sexton H, Aasland OG, Gude T. A three-year cohort study of the relationships between coping, job stress and burnout after a counselling intervention for help-seeking physicians. BMC Public Health. 2010;10:213. doi: 10.1186/1471-2458-10-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doolittle BR, Windish DM, Seelig CB. Burnout, coping, and spirituality among internal medicine resident physicians. J Grad Med Educ. 2013;5(2):257–261. doi: 10.4300/JGME-D-12-00136.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 15.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 16.Amoyal NR, Mason ST, Gould NF, Corry N, Mahfouz S, Barkey A, Fauerbach JA. Measuring coping behavior in patients with major burn injuries: a psychometric evaluation of the BCOPE. J Burn Care Res. 2011;32(3):392–398. doi: 10.1097/BCR.0b013e318217f97a. [DOI] [PubMed] [Google Scholar]
- 17.Kimemia M, Asner-Self KK, Daire AP. An exploratory factor analysis of the Brief COPE with a sample of Kenyan caregivers. Int J Adv Couns. 2011;33(3):149–160. doi: 10.1007/s10447-011-9122-8. [DOI] [Google Scholar]
- 18.Miyazaki Y, Bodenhorn N, Zalaquett C, Ng KM. Factorial structure of Brief COPE for international students attending U.S. colleges. Coll Stud J. 2008;42(3):795–806. [Google Scholar]
- 19.Eckleberry-Hunt J, Lick D, Boura J. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269–277. doi: 10.1097/ACM.0b013e3181938a45. [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317(9):901–902. doi: 10.1001/jama.2017.0076. [DOI] [PubMed] [Google Scholar]
- 21.Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National Survey of Burnout among US General Surgery Residents. J Am Coll Surg. 2016;223(3):440–451. doi: 10.1016/j.jamcollsurg.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schapira MM, Kalet A, Schwartz MD, Gerrity MS. Mentorship in general internal medicine. J Gen Intern Med. 1992;7:248–251. doi: 10.1007/BF02598026. [DOI] [PubMed] [Google Scholar]
- 23.DeCastro R, Griffith KA, Ubel PA, Stewart A, Jagsi R. Mentoring and the career satisfaction of male and female academic medical faculty. Acad Med. 2014;89(2):301–311. doi: 10.1097/ACM.0000000000000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peccoralo LA, Tackett S, Ward L, Federman A, Helenius I, Christmas C, Thomas DC. Resident satisfaction with continuity clinic and career choice in general internal medicine. J Gen Intern Med. 2013;28(8):1020–1027. doi: 10.1007/s11606-012-2280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramanan RA, Taylor WC, Davis RB, Phillips RS. Mentoring matters: mentoring and career preparation in internal medicine residency training. J Gen Intern Med. 2006;21(4):340–345. doi: 10.1111/j.1525-1497.2006.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dyrbye LN, Thomas MR, Huntington JL, Lawsom KL, Novotny PJ, Sloan JA, Shanafelt TD. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006;81(4):374–384. 10.1097/00001888-200604000-00010 [DOI] [PubMed]
- 27.Maslach C. Maslach burnout inventory manual. 3. Palo Alto: Consulting Psychologist Press; 1996. [Google Scholar]
- 28.Thomas NK. Resident burnout. JAMA. 2004;292:2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 29.Holmes TH, et al. The social readjustment rating scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 30.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Erlbaum; 1988. [Google Scholar]
- 31.McCue JD, Sachs CL. A stress management workshop improves residents' coping skills. Arch Intern Med. 1991;151(11):2273–2277. doi: 10.1001/archinte.1991.00400110117023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All surveys and results can be made available for review.