Abstract
Introduction
There is a paucity of comparative clinical data between arthroscopic all-inside end-to-end meniscal root suture and transtibial pullout technique in medial meniscus posterior root tears (MMPRT). Therefore, this study aimed to compare treatment failure, mid-term clinical and radiological outcomes of all-inside meniscus root repair versus the transtibial pullout technique and to analyze prognostic factors of postoperative clinical and radiological outcomes.
Material and methods
Forty-four patients were included in two therapeutic group: arthroscopic all-inside meniscal suture (MS: 13 knees) and transtibial pullout technique (TP: 31 knees).
Primary clinical outcomes at a minimum of 27.2 months postoperatively included Knee injury and Osteoarthritis Outcome Score (KOOS) and Lysholm Knee Questionnare (LKQ). Radiographic assessment of the knee was performed to determine osteoarthritis severity using the Kellgren-Lawrence (KL) grading system.
In addition, pre and postoperative MRI scans and intraoperative arthroscopic findings were recorded and the correlations between these findings, as outcome predictors and postoperative patients reported subjective outcome were assessed.
Results
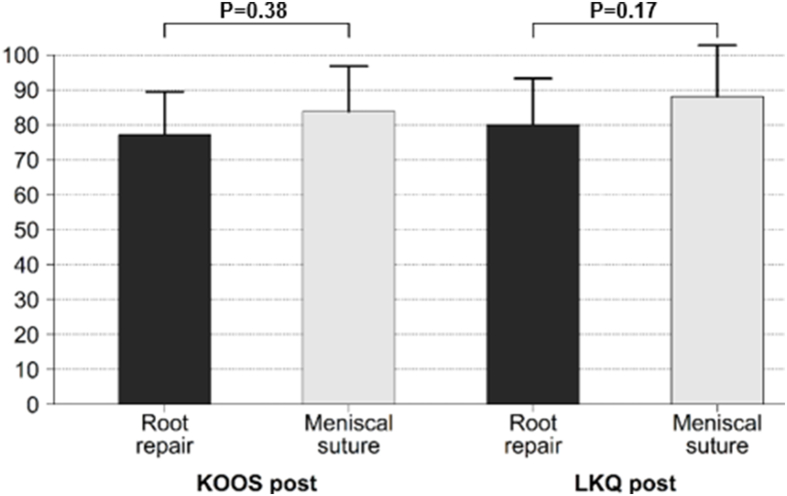
No significant differences in postoperative KOOS and LKQ scores were found between the MS and TP group (p = 0.38 and 0.17, respectively).
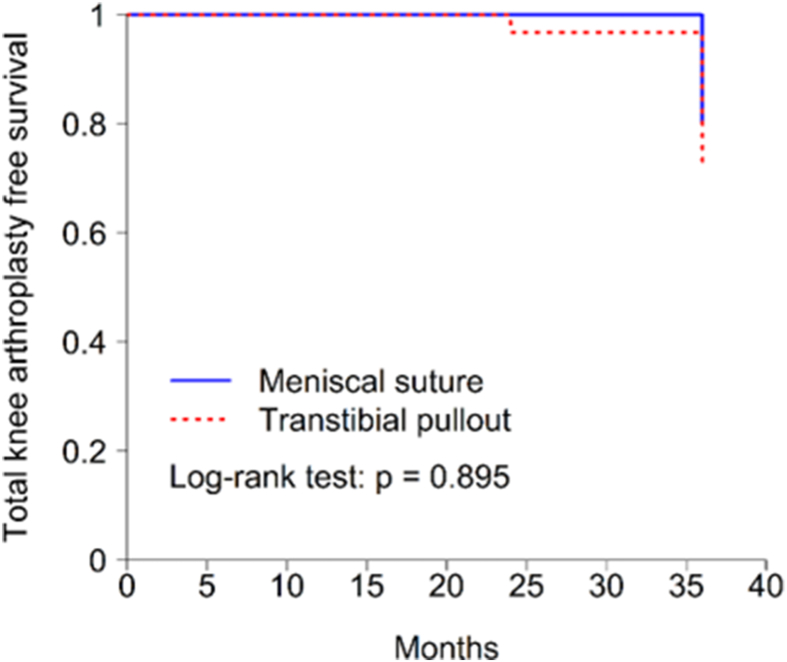
During follow-up one patients (7.7%) in the MS group and two (6.5%) in the TP group underwent total knee arthroplasty. The difference did not reach the statistical significance (p = 0.88).
No differences were observed in postoperative MRI findings such as meniscal extrusion, osteochondral defect, chondromalacia patella, and bone morrow edema (p = 0.25, 0.97, 0.97, and 0.88, respectively).
A univariate model revealed that the presence of postoperative meniscal extrusion; osteochondral defect; chondromalacia patella; increased BMI; age (>40 years) and longer time lapse between clinical onset to surgery (>6 months) were predictors of poor clinical outcome. The presence of meniscal extrusion, osteochondral defect and chondropatia patella portended worst postoperative outcomes in a multiple linear regression model.
Conclusions
It can be concluded that both techniques can reach good results when performed properly and if the injury pattern allows meniscal suture may be considered a treatment option for the management of MMPRT in well-selected patients.
Patients with increased BMI, preoperative meniscal extrusion, chondromalacia patella, and osteochondral defect were at higher risk of poor clinical outcomes.
Keywords: Medial meniscus root tear, All-inside meniscal suture, Transtibial pullout repair, Meniscal root repair, Outcomes of meniscal root repair
1. Introduction
Over the last few decades, meniscal root tears have been increasingly recognized as a ‘silent epidemic'1 and have thus received considerable attention. Now it is believed that the majority of these injuries were previously overlooked, predisposing these patients to an increased risk damage to the articular cartilage and progressive knee osteoarthritis.
The importance of meniscal root repair has been widely supported by clinical studies as a method of anatomic restitution of the meniscal function restoring the ability to absorb hoop stresses and subsequently decrease contact peak pressures nearly to normal condition found in the intact state.2,3 Furthermore, given the increased risk of conversion to knee arthroplasty with both meniscectomy and non-operative management, root repair is a desirable choice whenever possible.
To the best of our knowledge, there is scant data comparing between all-inside meniscal repair and the transtibial pullout technique for medial meniscus posterior root tears. Moreover, no studies addressed the relationship between demographic and radiological characteristics as prognostic factors of postoperative clinical outcome in patients undergoing medial meniscus posterior root repair (MMPRT).
The purpose of this study was twofold. First, we set out to evaluate meniscal root repair outcomes and survivorship in two surgical treatment groups: transtibial pullout technique and all-inside meniscal repair. As secondary end-point, we aimed to determine the value of MRI findings as prognostic factors and as separate measures of functional postoperative outcomes for each type of surgical treatment in patients with MMPRT at a minimum of 2 years of follow-up.
We hypothesized that an all-inside meniscal suture and the transtibial pullout repair would have comparable results in terms of patient-reported clinical outcomes; progression of osteoarthritis, rate of conversion to TKA, and one or more prognostic factors for poor clinical outcome could be identified.
2. Material and methods
2.1. Study design
A retrospective case-control analysis was conducted. Local Ethics Committee (EC) approval was obtained prior to undertaking the study (EC study code EO 138–20). Patients who had undergone medial meniscal posterior root surgery in a tertiary hospital between January 2016 and December 2018 were divided into two therapeutic groups based on the treatment performed: a transtibial pullout technique (TP) group and a meniscal suture (MS) group. The inclusion criteria for this study were as follows: (1) patients over 18 years with a medial meniscal posterior root avulsion or radial tear adjacent (within 10 mm) to the posterior meniscal root; (2) presenting clinical symptom that correlated with MRI findings; and (3) a minimum of 2 years of follow-up. Patients treated nonoperatively, who presented grade 4 osteoarthritis according to Kellgren-Lawrence (KL) grading system4; prior ligamentous knee injury; lateral meniscus root tear; concomitant traumatic tibial plateau fracture; systemic inflammatory disease; knee malalignment (varus or valgus >8°) or congenital knee deformity were excluded. All patients gave their written consent to participate in the study.
2.2. Study population and data analysis
All included patients were retrospectively reviewed with prospectively collected data. Demographic and clinical information was retrieved from electronic medical records (e.i., sex, age, body mass index (BMI), mechanism of injury, time lapse from clinical onset to surgery, previous knee surgeries and conversion to knee arthroplasty). The type of meniscal root tear according to LaPrade classification system5 and the Outerbridge grading6 of osteochondral lesions were documented at the time of surgery.
The primary endpoints were subjective patient-reported outcome measures (PROMs) and radiological stabilization or progression of knee osteoarthritis. Outcome measure assessment was based on the Knee injury and Osteoarthritis Outcome Score (KOOS) and Lysholm Knee Questionnare (LKQ) determined at a minimum of 2 years after surgery 7,8. To assess whether an intervention was associated with an improved PROMs, the minimal clinically important differences (MCIDs) with regard to KOOS and LKQ were taken into account from previous studies.9,10
Regarding the imaging study, posteroanterior weight-bearing radiographs were obtained with the knee at 45° of flexion (Rosenberg view) at baseline and final follow-up. The Kellgren-Lawrence (KL) grading system was used to determine the severity of knee osteoarthritis.11 Preoperative findings were compared to final results within each group and between groups. Radiographic images were examined by one author in blinded fashion and independently of the surgeons performing the intervention. Additionally, pre and postoperative MRI scans were reviewed for presence of meniscal extrusion, osteochondral defect, chondromalacia patella, subchondral edema and were used to calculate prognostic factors of surgical outcomes.
The meniscus was considered to be extruded if the amount of meniscal subluxation exceeded 3 mm from medial tibial margin.12,13 An osteochondral defect was defined as a low-signal-intensity focal lesion beneath the articular surface in the weight-bearing area of the tibiofemoral compartment on T1-weighted images. Subchondral edema was defined as focal bone marrow signal alteration, including edema or cyst-like changes.
The secondary objectives was to assess the possible correlation between the aforementioned radiological findings and clinical outcome after meniscal repair. Treatment failure was defined as need for conversion to knee arthroplasty. In those patients who underwent conversion to TKA, the final clinical and radiologic outcomes were assessed just before arthroplasty and were included in the prognostic factor analysis.
The decision to perform meniscal root repair using all-inside meniscal repair or the transtibial pullout technique was typically determined based on the tear pattern and location; the ultimate surgical decision was based on surgeon preference.
2.3. Statistical analysis
Statistical analysis was performed using R-3.6.0, R Core Team 2020, Vienna, Austria. Statistical significance was considered when p < 0.05. Qualitative variables were described by absolute and relative frequencies, and quantitative variables by mean and standard deviation. The chi-squared test was applied to compare qualitative variables, while the comparison of quantitative variables exhibiting a normal distribution versus dichotomous qualitative variables was carried out using the Student's t-test. Before-after analyses were carried out using the Student's t-test for paired samples when analyzing quantitative variables, and Mc Nemar test for qualitative variables. To identify variables potentially associated with a poor response, univariate and multivariate linear regression models were calculated. Regression models were summarized by the regression coefficient and p-values. The pooled cumulative incidence of TKA after meniscal root repair or partial meniscectomy was obtained using the Kaplan-Meier survival analysis and a hazard ratio was created by means of the Cox proportional hazards model.
3. Results
Table 1 summarizes the baseline data of the two study groups. There were no significant differences between the cohorts with respect to sex, BMI, knee laterality, mechanism of injury, time from injury to surgery, presence of osteochondral defect, or preoperative KL grade (Table 1). Regarding the type of tear, significantly higher rates of incomplete type 1 and complete radial type 2 tears were observed in the MS group (46.2% and 53.8%, respectively), while the presence of a complex oblique type 4 and bucket handle type 3 was predominantly encountered among the patients in the TP group.
Table 1.
Patients’ demographics, and preoperative clinical and radiological characteristics by cohort*.
| Variable | Root repair N = 31 | Meniscal suture N = 13 | p-value^ |
|---|---|---|---|
| Age | 50.29 ± 9.5 | 33.08 ± 10.2 | 0.001 |
| BMI | 28.17 ± 4.9 | 25.6 ± 3.05 | 0.16 |
| Right knee Left knee |
17 (54.8%) 14 (45.2%) |
7 (53.8%) 6 (46.2%) |
0.95 |
| Traumatic tear Degenerative tear |
15 (48.4%) 16 (51.6%) |
3 (23.1%) 10 (76.9%) |
0.11 |
| LaPrade Classification | |||
| 1 | 0 | 7 (53.8%) | |
| 2 | 21 (67,7%) | 6 (46.2%) | |
| 3 | 2 (6.4%) | 0 | |
| 4 | 8 (25.8%) | 0 | <0.001 |
| Kellgren-Lawrence classification | |||
| 0 | 0 | 1 (7.7%) | |
| 1 | 7 (22.6%) | 6 (46.2%) | |
| 2 | 20 (64.5%) | 4 (30.8%) | |
| 3 | 4 (12.9%) | 2 (15.4%) | |
| Time from injury to surgery (months) | 7.83 (7.4) | 6.92 (6.6) | 0.17 |
| Osteochondral defect | 5 (16.1%) | 2 (15.4%) | 0.95 |
| Outerbridge grade | |||
| 0 | 0 | 0 | |
| 1 | 5 (16.1%) | 4 (30.8%) | |
| 2 | 19 (61.3%) | 7 (53.8%) | |
| 3 | 3 (9.7%) | 2 (15.4%) | |
| 4 | 4 (12.9%) | 0 | 0.39 |
*Values are reported as mean ± SD and n (%).
^ Significant at the level of p < 0.05.
KOOS: Knee injury and Osteoarthritis Outcome Score; LKQ: Lysholm Knee Questionnaire.
When analyzing postoperative outcomes, there were no significant inter-group differences in KOOS or LKQ scores (Fig. 1). Moreover, no statistically significant differences were found for the proportion of postoperative meniscal extrusion, chondromalacia patella, osteochondral defect, or subchondral edema (p < 0.25, 0.97, 0.95, and 0.88 respectively).
Fig. 1.
Postoperative patient reported outcomes. No statistically significant difference was found between study groups.
At the final follow-up, pre and postoperative differences in osteoarthritic changes were determined according to the KL grading system. Four patients (13%) in the TP group presented progression of preexisting degenerative changes compared to two patients (15.4%) in the MS group. However, the difference did not reach statistical significance. Postoperative clinical and radiological data are depicted in Table 2.
Table 2.
Postoperative clinical and radiological outcome by cohort*.
| Variable | Root repair N = 31 | Meniscal suture N = 13 | p-value |
|---|---|---|---|
| KOOS α | 77.13 ± 12.2 | 80 ± 13.2 | 0.38 |
| LKQ α | 83.74 ± 13 | 88.08 ± 14.6 | 0.17 |
| KL classification | |||
| 0 | 0 | 1 (7.7%) | |
| 1 | 6 (19.4%) | 6 (46.2%) | |
| 2 | 18 (58.1%) | 3 (23.1%) | |
| 3 | 6 (19.4%) | 2 (15.4%) | |
| 4 | 1 (3.2%) | 1 (7.7%) | 0.1 |
| KL grade progression | 4 (13%) | 2 (15.4%) | 0.7 |
| Meniscal extrusion | 10 (32.3%) | 2 (15.4%) | 0.25 |
| Osteochondral defect | 5 (16.1%) | 2 (15.4%) | 0.95 |
| Chondromalacia patellae | 24 (77.4%) | 10 (76.9%) | 0.97 |
| Subchondral edema | 2 (6.5%) | 1 (7.7%) | 0.88 |
| Follow-up α | 27.2 (4.5) | 28.5 (6.1) | 0.93 |
| TKA | 2 (6.5%) | 1 (7.7%) | 0.89 |
*Values are expressed as n (%).
α mean ± SD.
^ Significant at the level of P < 0.05.
KOOS: Knee injury and Osteoarthritis Outcome Score; LKQ: Lysholm Knee Questionnaire; KL: Kellgren-Lawrence classification; TKA: Total Knee Arthroplasty.
Independent prognostic factor analysis revealed that increasing BMI, intraoperative Outerbridge score (grade ≥3), presence of meniscal extrusion and osteochondral defect in the MRI were inversely correlated with clinical outcome in the TP group (p = 0.008, 0.001, 0.001, and 0.001, respectively). A high BMI, time lapse between clinical onset to surgery (>6 months); Outerbridge score (grade ≥3), and the presence of meniscal extrusion were also significantly inversely correlated with KOOS and LKQ scores in the MS group (p = 0.003, <0.006, 0.01, and 0.007, respectively). In addition, age (>40 years) portended a worst clinical outcome (p < 0.04) in the MS group (Table 3).
Table 3.
Clinical and radiological predictors for each therapeutic group and their correlation with outcome scores using univariable analysis.
| PROM | Group* | Independent variable | bi | CI95% | p value | R2 |
|---|---|---|---|---|---|---|
| KOOS | TP | BMI | −13.4 | (-23.1, −3.7) | 0.008 | 0.21 |
| Meniscal extrusion | −18.2 | (-25.1, −11.2) | <0.001 | 0.49 | ||
| Osteochondral defect | −19.4 | (-29.5, −9.4) | <0.001 | 0.35 | ||
| Preoperative Outerbridge grade 4 | −20.2 | (-31.5, −8.9) | 0.001 | 0.31 | ||
| Meniscal extrusion | −24.8 | (-41.5, −8.1) | 0.007 | 0.49 | ||
| MS | Preoperative Outerbridge grade 3 | −26 | (-41.8, −10.1) | 0.04 | 0.54 | |
| Time lapse from clinical onset to surgery (>6 months) | −18.8 | (-30.9, −6.7) | 0.006 | 0.51 | ||
| LKQ | TP | BMI | −15.7 | (-25.7, −5.7) | 0.003 | 0.26 |
| Meniscal extrusion | −19.4 | (-26.7, −12) | <0.001 | 0.57 | ||
| Osteochondral defect | −22.8 | (-32.8, −12.8) | <0.001 | 0.42 | ||
| Preoperative Outerbridge grade 4 | −20 | (-32.4, −7.7) | 0.02 | 0.27 | ||
| MS | BMI | −30.4 | (-59, −1.7) | 0.003 | 0.33 | |
| Meniscal extrusion | −32 | (-46.8, −17.1) | <0.001 | 0.67 | ||
| Preoperative Outerbridge grade 3 | −25.5 | (-45, −6) | 0.01 | 0.42 | ||
| Time lapse from clinical onset to surgery (>6 months) | −20.9 | (-34, −7.6) | 0.005 | 0.52 | ||
| Age (>40 years) | −18.7 | (-37, −0.4) | 0.04 | 0.35 |
* Treatment group: TP tibial pullout, PM partial meniscectomy.
+ Individual p value.
^ F Snedecor p value.
KOOS: Knee injury and Osteoarthritis Outcome Score; LKQ: Lysholm Knee Questionnaire; BMI: Body Mass Index.
Multivariate regression analysis showed meniscal extrusion and intraoperative Outerbridge score (grade ≥3) as significant prognosis factors for both study groups. In addition, poor patient-reported outcomes were predicted by increased BMI and the presence of preoperative osteochondral defect after meniscal suture and transtibial repair, respectively.
Survivorship analysis for conversion to total knee arthroplasty was conducted using Kaplan-Meier curves. Two patients (6.5%) in the TP group underwent TKA at the final follow-up versus one patient (7.7%) in the MS group. No statistically significant differences were found in the survival rate between study groups (p = 0.89). Survival analysis is demonstrated in Fig. 2.
Fig. 2.
Kaplan-Meier survival curve demonstrating patients free from conversion to total knee arthroplasty through minimum 27-month follow-up.
4. Discussion
The main finding of our study is that the postoperative results were comparable between the two study groups in terms of postoperative functional outcomes after arthroscopic repair. Furthermore, no significant differences were observed with respect to radiological progression and the need for conversion to knee arthroplasty. All patients included in the MS group presented LaPrade type 1 and 2 tears, which were treated with a specific approach (all-inside meniscal suture) that has not previously been investigated.
Dragoo et al.14 compared the clinical outcomes in patients over 45 years of age with moderate knee osteoarthritis and who underwent an all-inside meniscus root repair technique versus nonoperative management for either medial or lateral meniscus root tears. Although improved functional outcomes and decrease TKA conversion rate was observed compared with nonoperative treatment, it should be noted that external validity of these findings is discussed because the anatomic configuration of the lateral meniscus is different from its counterpart, the medial meniscus.
Jung et al.4 reported a case series of 13 female patients with a mean age of 53.2 years (range, 47–60) who underwent an all-inside repair of posterior root tear of the medial meniscus using a suture anchor. In 2 patients high tibial osteotomy was performed concomitantly. The authors reported symptomatic improvement after root repair; however, meniscal extrusion was not significantly decreased after an average of 30.8 months of follow-up.
The relationship between meniscal extrusions on MRI scan and osteoarthritic changes has been widely studied suggesting the relative urgency of surgical treatment due to negative functional outcome after conservative treatment of MMPRT.12,13 Kwak et al.15 noted that the large meniscus extrusion ratio was the most reliable poor prognostic factor of conservative treatment for MMPRT. Therefore, early surgical repair was recommended as the primary treatment option in such cases. However, the role of meniscal extrusion as a prognostic factor after meniscal root repair is still unknown. Our data showed that the preexisting meniscal extrusion was a poor prognostic factor related to postoperative clinical outcomes after medial meniscus posterior root repair.
It was previously reported that patients with a MMPRT were more likely to have concomitant chondral defects.16 On the other hand, the association of meniscal injuries leading to spontaneous osteonecrosis of the knee (SONK) has been widely established in the literature. Previously, SONK was recognized as an idiopathic condition prior to the recognition that this condition was actually caused by a meniscal tear.17,18 Husain et al.19 investigated relationship between clinical outcomes and imaging patterns on MRI after subchondral fractur around the knee. Irregularity of the subchondral articular surface contour (on any sequence) was the only imaging predictor for worse clinical results. Presence of isolated meniscal tear/extrusion was not statistically significant predictor, however, it was identified as enhancing factors predisposing to unfavorable clinical outcomes.
The present study found presence of preoperative osteochondral defect as a determinant of poor mid-term clinical outcome following root repair.
The main advantage of all-inside meniscal suture is that is a less invasive and less surgically demanding technique that avoids additional incisions or tibial tunnel drilling which could interfere with concomitant ligament reconstruction tunnels. Furthermore, this technique allows for restoration of the natural meniscus position, anatomy, and tension in well-selected patients with type-1 and -2 tears.
This study has a number of strengths. It is the first case-control study to date comparing all-inside meniscal repair and transtibial pullout technique in patients treated in a routine clinical setting where the decision to perform a joint preservation procedure is crucial for a successful clinical outcome.
In the current study, both groups had comparable with respect to preoperative clinical data. The main advantage of establishing homogenous groups is that it allows precise determination of treatment effect. In addition, this study is the first to establish radiological predictors of clinical outcome after root repair to date, no studies have investigated correlations between demographic and radiological variables as prognostic factors and postoperative clinical outcomes. Knowledge of prognostic factors for a MMPRT may increase surgeon’ awareness of this injury pattern, and such considerations may have a positive impact on clinical decision-making and subsequent patient-reported clinical outcomes.
Furthermore, all patients included were attended and evaluated on an outpatient basis, as which can increase external validity and enhance generalizability to the population at large. Surgical procedures were performed in the same facility where the surgical technique and postoperative management protocol were standardized for all patients.
It can be postulated that as certain tear type may have certain effect on patient’ outcome. This type-specific approach and the effect that certain tear types may have on patient outcomes have not been addressed previously, and we consider further investigation would be beneficial. Nonetheless, there remains a pressing for better designed prospective studies to explore some unanswered questions.
The limitations of this study stem from its retrospective nature. First, outcomes from these series were reported at a mean of 27.2 months as of the index surgery, and as such long-term complications cannot be assessed, as further evaluation of osteoarthritic changes to the knee require a longer follow-up period. Secondly, we are aware that the statistically significant inter-group difference in patients’ mean age and the relatively small sample size used here (13 patients in the meniscal suture group) could reduce the likelihood of detecting a true difference. Long-term follow-up will be needed to determine whether the rate of conversion to TKA in the MS group continue to be similar to that in patients treated with transtibial pullout technique. Mean patient age differed between the study groups; however, severity of osteoarthritis was similar. About 45% in the MS group had Kellgren-Lawrence grade II or III osteoarthritis with a mean age of 33 years. It appears, that there could have been other reasons for early-onset of osteoarthritis in this group. It will be a subject for future investigation.
Finally, we do not have baseline PROM data with which to compare our sample studied using prospectively collected postoperative scores. Further follow-up and periodic clinical and radiological assessment of these cohorts are warranted.
5. Conclusion
It can be concluded that both techniques can produce good results when performed properly and if the injury pattern allows meniscal suture may be considered a treatment option for the management of MMPRT in well-selected patients.
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Compliance with ethical standards
Approval to perform this study was granted by the local ethics committee. All patients provided informed consent to participate in the study.
Acknowledgements
We thank Dr Ignacio Mahillo Fernández, BS, for his contributions to the statistical analysis.
References
- 1.Cinque M.E., Chahla J., Moatshe G., Faucett S.C., Krych A.J., LaPrade R.F. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52(13):872–876. doi: 10.1136/bjsports-2017-098942. 2018. [DOI] [PubMed] [Google Scholar]
- 2.Chung K.S., Ha J.K., Yeom C.H. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–1950. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 3.Krych A.J., Reardon P.J., Johnson N.R. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 4.Jung Y.H., Choi N.H., Oh J.S., Victoroff B.N. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40(6):1406–1411. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 6.Outerbridge R.E. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 7.Roos E.M., Roos H.P., Lohmander L.S., Ekdahl C., Beynnon B.D. Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 8.Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 9.Ebert J.R., Smith A., Wood D.J., Ackland T.R. A comparison of the responsiveness of 4 commonly used patient-reported outcome instruments at 5 years after matrix-induced autologous chondrocyte implantation. Am J Sports Med. 2013;41(12):2791–2799. doi: 10.1177/0363546513502314. [DOI] [PubMed] [Google Scholar]
- 10.Ogura T., Ackermann J., Mestriner A.B., Merkely G., Gomoll A.H. The minimal clinically important difference and substantial clinical benefit in the patient-reported outcome measures of patients undergoing osteochondral allograft transplantation in the knee. Cartilage. 2021;12(1):42–50. doi: 10.1177/1947603518812552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costa D.R., Morrison W.B., Carrino J.A. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? Am J Roentgenol. 2004;183:17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 13.Lerer D.B., Umans H.R., Hu M.X., Jones M.H. The role of meniscus root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 14.Dragoo J.L., Konopka J.A., Guzman R.A., Segovia N., Kandil A., Pappas G.P. Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med. 2020;48(5):1127–1133. doi: 10.1177/0363546520909828. Apr. [DOI] [PubMed] [Google Scholar]
- 15.Kwak Y.H., Lee S., Lee M.C., Han H.S. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781–786. doi: 10.1007/s00167-017-4441-x. [DOI] [PubMed] [Google Scholar]
- 16.Matheny L.M., Ockuly A.C., Steadman J.R., LaPrade R.F. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–3131. doi: 10.1007/s00167-014-3073-7. [DOI] [PubMed] [Google Scholar]
- 17.Hussain Z.B., Chahla J., Mandelbaum B.R., Gomoll A.H., LaPrade R.F. The role of meniscal tears in spontaneous osteonecrosis of the knee: a systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47(2):501–507. doi: 10.1177/0363546517743734. [DOI] [PubMed] [Google Scholar]
- 18.Robertson D.D., Armfield D.R., Towers J.D., Irrgang J.J., Maloney W.J., Harner C.D. Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Joint Surg Br. 2009;91(2):190–195. doi: 10.1302/0301-620X.91B2.21097. [DOI] [PubMed] [Google Scholar]
- 19.Husain R., Nesbitt J., Tank D., Verastegui M.O., Gould E.S., Huang M. Spontaneous osteonecrosis of the knee (SONK): the role of MR imaging in predicting clinical outcome. J Orthop. 2020;22:606–611. doi: 10.1016/j.jor.2020.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]