Abstract
Purpose
Precision medicine is revolutionizing healthcare practices, most notably in oncology. With cancer being the second leading cause of death in the USA, it is important to integrate precision oncology content in undergraduate medical education.
Methods
In 2015, we launched a Clinical Cancer Medicine Integrated Science Course (ISC) for post-clerkship medical students at Vanderbilt University School of Medicine (VUSM). In this ISC, students learned cancer biology and clinical oncology concepts through a combination of classroom and patient care activities. Student feedback from mid- and end-of-course surveys and student match data were analyzed and used to develop ongoing course improvements.
Results
To date, 72 medical students have taken the Clinical Cancer Medicine ISC. Over 90% of students who completed end-of-course surveys agreed or strongly agreed that this course advanced their foundational science knowledge in clinical cancer medicine, that clinical relevance was provided during non-clinical foundational science learning activities, and that foundational science learning was embedded in course clinical experiences. Students who took this course most commonly matched in Internal Medicine, Pathology, Pediatrics, and Radiation Oncology. VUSM students who matched into Pathology and Radiation Oncology were more likely to take this ISC than students who matched in other specialties.
Conclusion
The Clinical Cancer Medicine ISC serves as a model for incorporating precision oncology, cancer biology foundational science, and oncology patient care activities in undergraduate medical education. The course prepares students to care for oncology patients in their fields of interests during their future career in medicine.
Keywords: Cancer, Oncology, Integration, Foundational Science, Medical Education
Introduction
Completion of the Human Genome Project in 2003 revolutionized the field of genomic medicine and ushered a new era of precision medicine. Precision medicine is the tailoring of patient therapy based on pharmacogenetic biomarkers that predict the likelihood of drug response or risk of adverse events [1]. This emerging healthcare paradigm was quickly embraced in the field of oncology and highlights the importance of foundational science translation in improving patient outcomes.
Cancer is the second leading cause of death in the United States (US) with an estimated incidence of 1.8 million new cancer cases and over 600,000 cancer deaths projected to occur in 2020 [2]. Over the last decade, there has been an increase in the understanding of cancer molecular drivers, and gene mutation–specific inhibitors have been successfully used to target sub-populations of patients with particular tumor genotypes. As a result, oncology providers must have an appreciation of the fundamental molecular biology underlying a patient’s tumor to effectively translate tumor genotype to precision patient care [1, 3–5]. In addition to sub-specialists who provide oncologic care, primary care physicians and many other healthcare providers play a crucial role in cancer prevention, screening, early diagnosis, management, and survivorship care [6, 7]. As strategies in oncologic management and precision medicine continue to improve and the number of cancer survivors increases, all medical trainees will need to gain foundational knowledge in clinical oncology regardless of specialty aspiration [7, 8].
The rapid growth of our knowledge of the human genome and development of genomic clinical applications has resulted in a knowledge gap between discovery and practical clinical implementation. Many non-oncology physicians and medical trainees have reported low levels of comfort regarding provision of oncologic and survivorship care and interpretation of genetic tests for use in precision medicine [1, 3, 4, 6, 9, 10]. A 2014 single-institution study using a customized National Board of Medical Examiners (NBME) assessment tool coupled with a self-assessment survey revealed knowledge deficits in molecular techniques, mutations and cancer, and interpretation of genomic test results. Students also expressed low levels of confidence explaining analytic and clinical validity and clinical utility of genomic testing and using online genetics resources [10]. Another study found that although 79% medical students agreed it was important to learn about personalized medicine, only 6% felt as though their curriculum adequately prepared them to practice personalized medicine [4].
The multidisciplinary and interprofessional nature of oncologic and survivorship care combined with the lack of national guidelines for undergraduate oncology education in the US makes it challenging to develop effective oncology curricula for medical students [7, 11–13]. Multi-institutional studies have shown that medical students receive a disproportionate amount of curricular time dedicated to cancer education relative to the other common causes of death in the US (heart disease, chronic lung disease, cerebrovascular disease) [7, 8]. Many US medical schools do not incorporate oncology-related clinical rotations into required clerkships, and coordination of oncology didactics across the four years of medical school is often lacking, leading to a fractured understanding of cancer management [7]. Furthermore, several studies have indicated a deficit in knowledge of oncology among medical students, which may be due in part to the structure of the oncology curriculum [11, 14–18]. Given the need for improved precision medicine and oncology training among future physicians, we describe an approach that integrates active learning of foundational sciences in cancer, emphasizing genomics, with personalized clinical experiences in a post-clerkship Clinical Cancer Medicine course.
Methods
In 2013, VUSM launched an innovative, personalized undergraduate medical education curriculum called Curriculum 2.0 [19]. Curriculum 2.0 is a competency-based, agile, and individualized curriculum that supports student lifelong learning [20–22]. Curriculum 2.0 is divided into 3 phases: Foundations of Medical Knowledge (pre-clerkship, year 1), Foundations of Clinical Care (clerkship, year 2), and Immersion Phase (post-clerkship, years 3–4) [20]. During the Immersion Phase, students design individualized schedules consisting of month-long immersive experiences that aim to strengthen connections between foundational science knowledge and clinical skills and foster adaptive expertise needed to thrive in rapidly evolving fields of medicine [23–26]. Rotations offered during the Immersion Phase include Acting Internships, Advanced Clinical Experiences (clinical experiences previously referred to as sub-internships), Advanced Electives (non-clinical rotations), Research Immersions, and Integrated Science Courses (ISCs) [20].
The primary goal of the ISCs is to reinforce and integrate foundational science knowledge, traditionally taught in the pre-clerkship curriculum, within a meaningful clinical context [20]. These four-week courses utilize a variety of instructional modalities including classroom-, workplace-, simulation-, laboratory-, and community-based settings. Students are evaluated using quantitative and qualitative (competency-based milestone) assessments, and each ISC undergoes a rigorous annual quality-improvement process that includes review of foundational science and patient care/clinical skills content and integration, assessment best practices, and the student experience [20]. Currently, there are 16 ISCs offered in the post-clerkship curriculum at VUSM.
Clinical Cancer Medicine Course Design
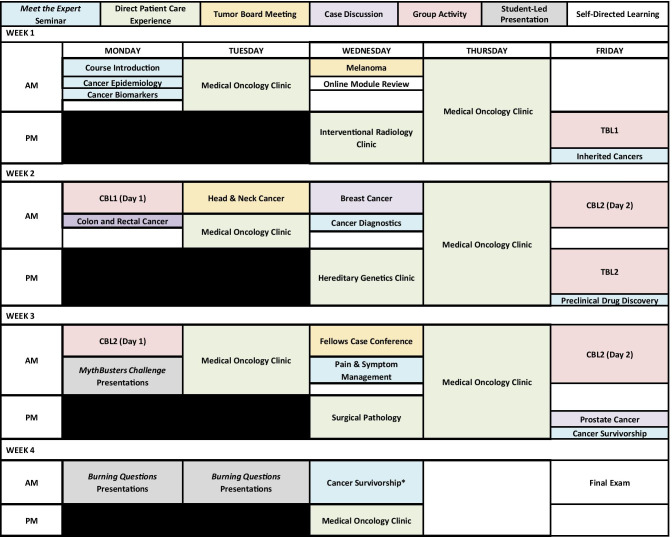
Responding to a need to increase oncology and precision medicine education in medical school curricula, the Clinical Cancer Medicine ISC was launched in 2015. This 4-week course enrolled up to 12 third- and fourth-year medical students each offering. The goal of this course was to reinforce the foundational principles of tumor biology, demonstrate how that information is leveraged for optimal and personalized cancer patient care, and illustrate how that care affects the physical, psychosocial, and financial well-being of cancer survivors (Fig. 1). Foundational science topics included anatomy, physiology, histology, biochemistry, cell biology, genetics, molecular biology, immunology, and pathology.
Fig. 1.
The Clinical Cancer Medicine ISC reinforced foundational science and patient care in the context of cancer. This course reinforced the foundational principles of tumor biology while demonstrating how that information drives imaging and laboratory tests, treatment strategies, and response and resistance to therapy. In addition, this course illustrated how that care affects the physical, psychosocial, and financial well-being of cancer survivors
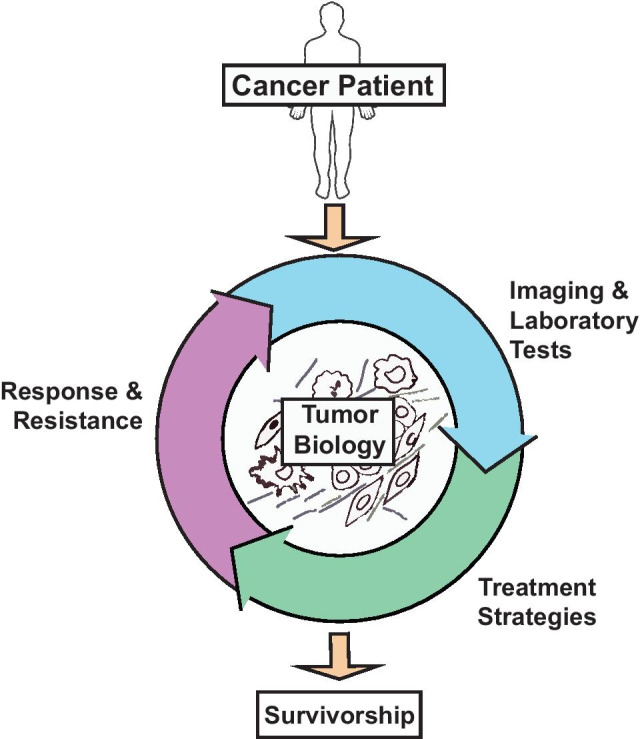
Active and personalized learning were emphasized in this course. In the classroom, students explored the concepts of oncogene addiction, de novo and acquired resistance to therapy, immunotherapy, tumor heterogeneity, and drug discovery through seminars, team-based learning, and case-based learning activities. The information learned was used as a platform to describe how molecular changes are detected in the laboratory and leveraged in the clinic for personalized patient care. Students actively participated in the multidisciplinary approach necessary for the optimal care of cancer patients through clinical experiences and tumor board meetings. Students also gained an understanding of patients’ expectations and the importance of a broad fund of knowledge in addressing complex clinical problems. The small class size (12 students maximum) allowed for tailoring of integrated clinical experiences with students’ professional preferences and/or goals. A sample student course schedule is depicted in Fig. 2. All course materials and student assessments are organized electronically using VUSM’s VSTAR Lifelong Learning Platform [27].
Fig. 2.
Students experienced classroom, workplace-based, and self-directed learning. A sample student schedule in the Clinical Cancer Medicine ISC. Students participated in approximately 40 h of course activities. Classroom sessions included Meet the Expert seminars (blue), Case Discussions (purple), group activities (red), and student-led presentations (gray). Workplace activities (green) included ten half days in a clinic of the student’s choice (in this example, medical oncology) in addition to one half day each in three of the following clinics: hereditary cancer, pathology, interventional radiology, interventional pulmonology, or cardio-oncology. Students also participated in three tumor board meetings (yellow). The remaining time (white) was dedicated to self-directed learning activities. Times blocked out in black are allocated for longitudinal courses and cannot be used for mandatory ISC activities. *This activity included a cancer survivor led classroom discussion
Classroom Activities
Meet the Expert Seminars and Case Discussions
Classroom-based learning included seven one-hour Meet the Expert seminars and three one-hour Case Discussions which brought students face to face with leading figures across many foundational science domains and clinical aspects of cancer medicine. The seminars included topics on epidemiology, cancer biomarkers, genetic inheritance syndromes, pre-clinical drug discovery, diagnostics, pain management, and cancer survivorship that apply to all types of malignancy. Additionally, three Case Discussions were developed in response to student feedback and interest. The case discussions focused on common cancers seen in the US including colorectal, prostate, and breast cancer. In these sessions, experts discussed the current clinical management and an overview of the emerging therapeutic strategies and research trials for each disease, while integrating appropriate foundational sciences.
Case-Based Learning
Two case-based learning (CBL) activities were built into this course that focused on lung cancer and chronic myelogenous leukemia (CML) [28]. Each activity was spread over two days for a total of three-hours of face-to-face time per case. Through independent research and group discussion, students learned molecular biology concepts underlying these diseases, recommendations for screening and diagnosis, and options for medical, radiation, and surgical management. In addition to highlighting cancers with high prevalence and mortality, cases were intentionally chosen to allow for integration of foundational sciences related to precision medicine. In the US, lung cancer is the 2nd most common cancer in males and females and has the highest mortality rate; thus, it was important to discuss in this course [2]. Although CML is relatively uncommon, this case introduced students to the broader concept of tyrosine kinase inhibition use in oncology and created an opportunity to discuss a hematological malignancy while much of the course focused on solid tumors.
Team-Based Learning
Students also participated in two team-based learning (TBL) activities that heavily engaged the primary literature [29, 30]. Both three-hour TBL sessions centered on the evolution of precision medicine strategies in BRAF mutant melanoma. In addition to illustrating how scientists, drug developers, and physicians leveraged oncogene addiction to treat cancer, these TBL sessions also highlighted the concepts of tumor evolution and tumor heterogeneity, mechanisms that drive adverse drug events, and mechanisms and clinical implications of de novo and acquired resistance to therapy. Given the need for all healthcare providers to stay abreast of rapidly evolving literature, students were given up to five primary manuscripts to critically interpret and assess in preparation for each session. To assist with integration of this information, we added a “debrief session” after the TBL individual and group readiness assessments (iRAT and gRAT, respectively) to contextualize the basic science concepts and give students a historical understanding of the concept implications.
Patient Care Experiences
In addition to classroom-based activities, students also participated in meaningful and active patient care experiences including direct patient interactions in an outpatient clinical environment and multidisciplinary tumor board meetings. It was important that students observed the significant role that each member of the team played in the comprehensive plan for cancer patient care. Furthermore, our goal was for students to assess the integration of specialties and foundational science concepts and assimilate evidence-based principles in developing treatment plans.
Patient Interactions
Students in this course actively participated in the care of cancer patients at the Vanderbilt-Ingram Cancer Center. In the clinical setting, students learned about diagnostic work-up, treatment plans (including clinical trials), and the side effects of cancer treatments. Notably, students witnessed how somatic and germline genetic testing results influenced medical management decisions as well as the benefits and challenges that precision medicine offered oncologists. Students selected up to ten half-days in primary clinics (medical, pediatric, radiation, and surgical oncology) and three half-days in secondary clinics (hereditary cancer, pathology, interventional radiology, interventional pulmonology, and cardio-oncology) based on their interests and learning goals. Other clinical specialties were also considered upon individual student request.
Tumor Board Meetings
Tumor board meetings are weekly case-based conferences where a multidisciplinary group of providers discuss specific cancer patients and advise one another on treatment options. These conferences offered students a unique opportunity to gain early exposure to the multidisciplinary nature of clinical oncology. During the course, students were required to attend two tumor board meetings of their choice from a menu of eleven tumor board meetings (i.e., multidisciplinary solid tumor, thoracic, sarcoma, melanoma, malignant hematology, breast cancer, head and neck cancer, VA tumor board, genitourinary, gynecology oncology, and molecular tumor board), in addition to an assigned hematology/oncology fellows case conference for a total of three tumor board meetings. Notably, the newly established molecular tumor board offered an excellent opportunity for students to understand the complexity of the decision-making process involving genetic testing and precision medicine [31]. In the hematology/oncology fellows case conference, one solid tumor case was discussed weekly, allowing for a slower pace, detailed disease descriptions, and comprehensive review of the relevant literature.
Clinical Experience Essays
Students were required to write two 1000-word essays related to a direct patient interaction in clinic or an interesting case presented at tumor board meetings. This activity allowed students to explore how foundational science drives clinical decision-making in oncology and communicate their experiential learnings to their peers. A successful essay demonstrated a firm recall of underlying foundational science principles, the application of these principles to a new case or problem, and the evaluation of multiple data sources. The essays were shared on an open forum where students commented on each other’s unique clinical experiences and learned about the diverse presentation and management of cancer patients.
Self-Directed Course Elements
Personal Learning Goals
Personal learning goals are specific and measurable statements of intent to attain essential concepts and skills that one identifies as important to one’s learning with a clearly outlined path to reach these goals. Learning goals may relate to work/study habits, specific knowledge areas, or both. At the beginning of the course, students were asked to document and submit two personal learning goals for the course. By establishing personal learning goals, students could tailor the integrated clinical experiences to their professional goals and pursue their own interests in oncology during this course. These goals were reviewed by the course directors during the first week, and individualized feedback was provided as to whether the course activities scheduled would help the students meet these goals. If course content was lacking, the course directors provided additional resources for the students to pursue on their own. Furthermore, the learning goals allowed the course directors to reflect on the course content and to adjust the curriculum if certain content was requested multiple times by students. The attainments of learning goals were determined at the midpoint and final course evaluations.
Online Modules
Online learning modules were included as a part of self-paced learning in this course. During the first week, students were required to review five online modules on cancer staging and grading, genetic alteration terminology, molecular diagnostics used in cancer, and phase I, II, and III cancer clinical trials. Each module consisted of 10–25 voice-accompanied PowerPoint slides, and the collection took about 3 h to view in entirety. The material presented in the modules was review from the pre-clerkship curriculum, and the intent was to remind students of the foundational science concepts upon which the course was built. Furthermore, presenting these materials online allowed for more in-class time that focused on advanced precision medicine concepts. An optional, in-class, review session of the online modules was hosted by the course directors to clarify any concepts in preparation for a closed-book quiz. The information in the modules was also included in the final examination.
Burning Question Presentation
At the end of the course, individual students gave a 30 min Burning Question presentation on a topic of their choosing. The origin of the question could be from, but was not limited to, a clinical experience, seminar, student forum discussion, online module, popular news story, or other course activity and reading. Answering the burning question necessitated integration and evaluation of multiple information sources and application of appropriate underlying foundational sciences. In a “chalk talk” presentation format, students taught the topic to their peers, where they practiced succinctly summarizing and communicating findings that were accurate, logical, and pertinent to answering the question.
MythBusters Challenge
In addition to individual Burning Question presentations, students also completed 30 min group “MythBusters” presentations on common cancer myths. The goal of this activity was to promote peer teaching of foundational science concepts (i.e., biochemistry, immunology, and cell biology) in the context of cancer patient care. In teams of three or four, students selected one cancer myth (pre-determined by the course directors) to research. Topics included the role of dietary sugar in cancer recurrence, the role of soy in breast cancer growth, the concept of tumor seeding during biopsy or surgical resection of tumors, and the impact of smoking in patients undergoing treatment of lung cancer. Students leveraged evidence from the literature and applied appropriate underlying foundational science to deem the myth “confirmed,” “busted,” or “plausible.” Furthermore, students formulated a response to the patient regarding the myth. To guide students in this endeavor, each team was given a set of learning objectives for each myth.
Primary Literature Reading
Cancer patient care is rapidly evolving and oncologists at academic centers are challenged to engage the primary literature to deliver the most effective treatments. As a result, this course emphasized student use and interpretation of the primary literature. There was an expectation that the primary literature was be used in CBL, self-directed learning, and clinical experience essays. Furthermore, the assigned reading for TBL was from the primary literature. The course also offered a list of recommended readings on cancer topics, including hallmarks of cancer, oncogene addiction, and precision cancer medicine.
Assessment
Student assessment in all ISCs offered through VUSM’s Curriculum 2.0 is multi-modal and uses both quantitative and qualitative (competency-based milestones) measures. Assessments occur throughout the course so that students have an opportunity to improve when they are given mid-course feedback [20].
Competency-Based Assessment
Students were assessed in their performance in six equally important competency domains: medical knowledge, patient care, interpersonal communication, practice-based learning and improvement, systems-based practice, and professionalism [21]. Student milestone data were collected from multiple evaluators (i.e., course directors, facilitators, peers, attendings, residents) who assessed student performance in key competencies during various course activities (Table 1). Students received, on average, 15 unique qualitative assessments during the course. Course directors synthesized input from these assessors to make one final assessment for each competency domain.
Table 1.
Competency-based milestone assessments
| Competency domain | Activity evaluated (evaluator |
|---|---|
| Medical knowledge | |
| Integration |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Clinical experience essay (course directors) |
| Depth |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Clinical experience essay (course directors) • MythBusters challenge presentation (course directors) • “Burning Questions” presentation (course directors) |
| Analysis |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Clinical experience essay (course directors) • MythBusters challenge presentation (course directors) • “Burning Questions” presentation (course directors) |
| Inquiry |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • MythBusters challenge presentation (course directors) • “Burning Questions” presentation (course directors) |
| Use of information resources |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Clinical experience essay (course directors) • MythBusters challenge presentation (course directors) • “Burning Questions” presentation (course directors) |
| Patient care | |
| Thought process |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) |
| Self-knowledge |
• CBL (course directors and peers) • Clinical experience (faculty/attendings/residents) |
| Interpersonal communication | |
| Content of presentations to colleagues |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Clinical experience essay (course directors) |
| Practice-based learning and improvement | |
| Receptivity to feedback |
• Mid-course feedback (course directors) • CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) |
| Systems-based practice | |
| Initiative and contribution to group efforts |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • MythBusters challenge presentation (peers) |
| Professionalism | |
| Professional duty |
• CBL (facilitator and peers) • Clinical experience (faculty/attendings/residents) • Compass requests (course directors) • On-time attendance to mandatory activities (course directors) |
Quantitative Assessment
The quantitative assessment in this course was determined by students’ grades in the following activities: online module quiz, TBL, MythBusters presentation, Burning Questions presentation, and final exam (Table 2). The online module quiz was a closed-note, 30 min, online assessment comprised of 17 multiple choice questions that was taken at the end of the first week. TBL assessments included an individual readiness assessment test (iRAT) followed by a group readiness assessment test (gRAT) taken at the beginning of each session. Each RAT was worth 2.5% of the student’s final quantitative grade, for a total of 5% of the student’s final quantitative grade per TBL session. The iRAT and gRAT are identical within each TBL session and comprised ten multiple-choice questions. The MythBusters and Burning Questions presentations each had a distinct 20-point grading rubric that was used by the course directors to assess student presentations. Each presentation was independently assessed by at least two of three course directors. The assessments were then discussed between all course directors, and a final score was assigned for each presentation. For the MythBusters challenge, the same quantitative score was assigned to each member of the group. The final exam was an individual, closed-note, 35-point, 26-question multiple-choice, short answer, and essay exam that probed foundational science and patient care integration.
Table 2.
Student quantitative assessments
| Activity | % of final quantitative grad |
|---|---|
| Online Module Quiz | 15 |
| TBL1 (iRAT 50%; gRAT 50%) | 5 |
| TBL2 (iRAT 50%; gRAT 50%) | 5 |
| MythBusters Challenge presentation | 20 |
| Burning Questions presentation | 20 |
| Final exam | 35 |
| Total | 100 |
iRAT individual readiness assurance test, gRAT group readiness assurance test
Results
Enrollment
From September 2015 to February 2020, the Clinical Cancer Medicine ISC was offered nine times (2–3 times per AY), with a maximum capacity of 12 students per section. Seventy-two medical students have taken the course, including 48 third-year students (66.7%) and 24 fourth-year students (33.3%), with an average of eight medical students per section (SD 4, range 2–12). The course was not offered in AY 17–18 due to lack of enrollment.
Mid-Course Feedback
At the course midpoint, students were asked to complete a survey about their personal learning goals that they documented at the beginning of the course. This survey was administered to seven sections from September 2016 to February 2020 (not administered in AY 15–16). When students were asked if they thought that they would achieve their personal learning goals by the end of the course, 59 of 60 (98.3%) students felt that they would achieve their personal learning goals at the end of the course. The student who answered that they would not be able to achieve their personal learning goals wanted to explore surgical oncology and requested operating room experience, which was not offered during that section.
End-of-Course Feedback
At the end of each ISC offering, an anonymous and standardized electronic evaluation survey was distributed to students by VUSM [20]. Sixty-five to 69 (90.2–95.8%) of the 72 medical students who took the Clinical Cancer Medicine ISC completed at least part of this end-of-course evaluation (Table 3). Most students were satisfied or very satisfied with the overall learning experience (92.7%), effectiveness of course leadership (94.2%), and mix of learning activities to support objectives (92.8%). All students agreed or strongly agreed that clinical relevance was provided during non-clinical foundational science learning activities (100.0%), and almost all agreed or strongly agreed that participation in this course advanced their foundational science knowledge in clinical cancer medicine (97.1%) and that foundational science learning was embedded in course clinical experiences (91.3%). Furthermore, most students anticipated using the foundational science knowledge acquired through this course in their future clinical training and practice (91.3%) and reported that they would recommend this course to their peers (91.3%). Student comments from this survey included “I thought that the course content tied in nicely with what I was seeing in the clinic,” “Good review of basic science related to oncology,” “The multiple learning modalities were balanced well and contributed to a unique group-based and sharing-oriented learning environment in all facets of the course,” and “This was hands down the best class I’ve taken in my life…everything we did was relevant.”
Table 3.
Student feedback from end-of-course evaluations (AY 15–20)
| Very dissatisfied (1) | Dissatisfied (2) | Neutral (3) | Satisfied (4) | Very satisfied (5) | Mean (SD)b overall | |
|---|---|---|---|---|---|---|
| Overall learning experience (n = 69) | 0 (0.0%)a | 0 (0.0%) | 5 (7.2%) | 25 (36.2%) | 39 (56.5%) | 4.5 (0.6) |
| Effectiveness of course leadership (n = 69) | 0 (0.0%) | 1 (1.4%) | 3 (4.3%) | 20 (29.0%) | 45 (65.2%) | 4.6 (0.7) |
| Mix of learning activities to support objectives (n = 69) | 0 (0.0%) | 2 (2.9%) | 3 (4.3%) | 26 (37.7%) | 38 (55.1%) | 4.4 (0.7) |
| Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly agree (5) | Mean (SD) | |
| Foundational science learning was embedded in the clinical experiences (n = 69) | 0 (0.0%) | 1 (1.4%) | 5 (7.2%) | 29 (42.0%) | 36 (49.3%) | 4.4 (0.7%) |
| Clinical relevance was provided during non-clinical foundational science learning activities (n = 69) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 33 (47.8%) | 36 (52.2%) | 4.5 (0.5%) |
| Participation in this course advanced my foundational science knowledge in this area (n = 69)c | 1 (1.8%) | 0 (0.0%) | 1 (1.8%) | 26 (37.7%) | 41 (59.4%) | 4.5 (0.7%) |
| I anticipate using the foundational science knowledge I acquired in this course in my future clinical training and practice (n = 69 | 0 (0.0%) | 2 (2.9%) | 4 (5.8%) | 32 (46.4%) | 31 (44.9%) | 4.3 (0.7) |
| I would recommend this course to my peers (n = 69) | 0 (0.0%) | 1 (1.4%) | 5 (7.2%) | 29 (42.0%) | 34 (49.3%) | 4.4 (0.7) |
| Participation in patient encounters during the clinical experiences was positive and reinforced the applicability of the foundational science learned during other class activities (n = 65) | 0 (0.0%) | 0 (0.0%) | 2 (3.1%) | 27 (41.5%) | 36 (55.4%) | 4.5 (0.6) |
SD standard deviation
aNumber of responses (percent)
bIn AY 15–16, the wording for this question was, “Participation in this course helped me learn relevant foundational sciences.”
In the end-of-course survey for AYs 18–19 and 19–20, students were also asked to rank order the primary reason(s) that they enrolled in the Clinical Cancer Medicine ISC when given a field of six choices and the option to write-in an alternative reason (Table 4). Students did not have to rank all reasons provided. The most common primary reasons students from AYs 18–19 and 19–20 took this course were that they thought the content would be valuable (64.7%) and help them to be more “marketable” for match (32.4%) given their field of choice. Furthermore, 26.5% of students primarily thought that the course would help them decide between two subspecialties for their future career and 20.6% of students heard that the ISC was more flexible (fewer mandatory sessions) than other ISCs (Table 4). Substantially fewer students (11.8%) primarily took this course because they heard that it was easier to get a good grade in the Clinical Cancer Medicine ISC than in other ISCs.
Table 4.
Reasons students enrolled in the Clinical Cancer Medicine ISC (AY18–19 and 19–20)
| Rank | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| I thought the content would be valuable to me, given my field of choice. (n = 34 | 22 (64.7%)b | 11 (32.4%) | 1 (2.9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| I believed it would help me be more “marketable” for match in my field of choice. (n = 34) | 11 (32.4%) | 8 (23.5%) | 8 (23.5%) | 7 (20.6%) | 0 (0.0%) | 0 (0.0%) |
| I thought it would help me decide between two subspecialties for my future career. (n = 34) | 9 (26.5%) | 15 (44.1%) | 4 (11.8%) | 4 (11.8%) | 2 (5.9%) | 0 (0.0%) |
| I have a general interest in the field/topic, but it may not be highly applicable to my field of choice. (n = 34) | 8 (23.5%) | 5 (14.7%) | 14 (41.2%) | 3 (8.8%) | 2 (5.9%) | 2 (5.9%) |
| I heard that this ISC was more flexible (fewer mandatory sessions) than other ISCs. (n = 34) | 7 (20.6%) | 5 (14.7%) | 12 (35.3%) | 5 (14.7%) | 4 (11.8%) | 1 (2.9%) |
| I heard that it was easier to get a good grade in this ISC than in other ISCs. (n = 34) | 4 (11.8%) | 13 (38.2%) | 3 (8.8%) | 7 (20.6%) | 3 (8.8%) | 4 (11.8%) |
aStudents were asked to rank order the primary reason(s) that they enrolled in this course. A rank of 1 indicates that most relevant reason and 6 was the least relevant reason. Students did not have to rank all primary reasons. Students had an option to give an alternate primary reason if not listed above
bNumber of responses (percent)
Match Data
Among 51 medical students who took the Clinical Cancer Medicine ISC for whom match data was available (published online), the most common specialties in which students matched were Internal Medicine (21.6%), Pathology (9.8%), and Pediatrics (9.8%) (Table 5). Interestingly, when compared with published match data for all VUSM students (2016–2020, n = 449), students who matched into Pathology were more likely to have taken the Clinical Cancer Medicine ISC (5/10 (50.0%)), than students who matched into other specialties (49/439 (11.2%), OR = 7.96, p = 0.0002). Similarly, students who matched into Radiation Oncology were more likely to have taken the Clinical Cancer Medicine ISC (4/9 (44.4%)), than students who matched into other specialties (50/440 (11.4%), OR = 6.24, p = 0.003) (Table 5).
Table 5.
Match data for students who completed the Clinical Cancer Medicine ISC (AY 15–20)
| Specialty | n (%) |
|---|---|
| Internal Medicine | 11 (21.6%) |
| Pathology | 5 (9.8%) |
| Pediatrics | 5 (9.8%) |
| Radiation Oncology | 4 (7.8%) |
| Interventional Radiology | 3 (5.9%) |
| Neurology | 3 (5.9%) |
| Neurosurgery | 3 (5.9%) |
| Diagnostic Radiology | 2 (3.9%) |
| General Surgery | 2 (3.9%) |
| Orthopedic Surgery | 2 (3.9%) |
| Otolaryngology | 2 (3.9%) |
| Urology | 2 (3.9%) |
| Child Neurology | 1 (2.0%) |
| Dermatology | 1 (2.0%) |
| Medicine Preliminary Year | 1 (2.0%) |
| Obstetrics and Gynecology | 1 (2.0%) |
| Ophthalmology | 1 (2.0%) |
| Psychiatry | 1 (2.0%) |
| Transitional Year | 1 (2.0%) |
Discussion
Foundational Science and Patient Care Integration
An overwhelming body of evidence suggests that integration of foundational sciences with clinical application throughout medical training enriches the clinical experience and leads to improved understanding and retention of foundational medical knowledge [32–41]. Additionally, integration of foundational sciences has been shown to enhance clinical diagnostic accuracy and decision-making skills [37–41]. Thus, many medical schools have sought to better integrate foundational sciences and clinical experiential learning throughout medical training, including in the post-clerkship curriculum [20, 32–34]. Few reports in the medical education literature have described immersive courses that integrate foundational sciences related to cancer biology with clinical experiences in provision of oncology and survivorship care in undergraduate medical education, though none have focused on precision medicine [42–44]. The lack of immersive courses integrating foundational sciences related to cancer biology and precision medicine, with clinical experiences in oncology and survivorship care led to the development of the Clinical Cancer Medicine ISC in the post-clerkship curriculum at VUSM. Our study shows that over the past five years, this course was successful in integrating foundational science and cancer patient care in both classroom- and workplace-based settings (Table 3).
The course directors were intentional with foundational science and patient care integration at the course and session levels, and in student assessments. For example, all sessions included learning objectives that contained both foundational science and patient care. Most often, both foundational science and patient care were included in the same learning objective. Furthermore, assessments emphasized the integration of foundational science and patient care by including patient vignettes and essay questions on exams and by including foundational science and patient care on presentation assessment rubrics. The competency-based assessments also emphasized medical knowledge and patient care (Table 1).
Reassuringly, students indicated that participation in the course advanced their foundational science knowledge in clinical cancer medicine (Table 3). Furthermore, student comments reflected the importance that course leadership, mix of learning activities, and perceived relevance of the material had on the impact of the course (Table 3). Specific elements that contributed to this success of this course include personalized learning opportunities for students and a rigorous annual quality improvement process that allowed for continuous course improvements based on student feedback and foundational science and student assessment expert input.
Personalized Learning
One goal of the Clinical Cancer Medicine ISC was to allow medical students to personalize their learning in pursuit of their interests, which was highly valued by the students. These personal learning goals not only helped students direct their learning, but they also informed the course directors if additional content needed to be added to the course. For example, in early course offerings the course directors heard from many students that they wanted to learn about prostate cancer, but that was not a cancer type discussed in any of the classroom-based sessions and was only be touched upon by a few patient care experiences, if at all. Since the course directors heard this topic over multiple years, and it is a common cancer in the US, it resulted in the addition of a Case Discussion on prostate cancer. Overall, based on the student feedback at mid-course the course directors were reassured that the vast majority of students perceived they would meet their personal learning goals by the end of the course. For the student who did not think that they would achieve one of their personal learning goals, the course directors provided other opportunities to supplement their learning.
For clinical activities, students chose from primary oncologic specialties including medical, pediatric, radiation, and surgical oncology. These primary specialties were longitudinal in the context of this course as the course directors learned that students wanted more time with one preceptor to better build relationships and participate more in the experience. Furthermore, students could request other clinical specialties and the course directors accommodated those requests, when possible. For example, if an enrolled student expressed interest in exploring otolaryngology the course directors matched that student with an otolaryngologist who saw primarily head and neck cancer patients. Students were also encouraged to explore other cancer-related clinical experiences including hereditary cancer, pathology, interventional radiology, interventional pulmonology, and cardio-oncology. This secondary, shorter, experience was designed to expose students to the multidisciplinary teams that are involved oncology care. For all clinical experiences, the course directors hand-selected faculty with whom the students worked to ensure that the faculty clearly understood the overall course objectives and goals, and could teach to them. The small class size of up to 12 students also facilitated this course individualization.
Other course activities also enabled students to personalize their learning experiences. For example, the Burning Questions presentation encouraged students to explore oncologic topics of their interests that were not directly addressed in the course and teach it to their peers. This activity was suggested by a student in a course evaluation survey. End-of-course survey data indicated that the students valued this activity and that the personal learning opportunities in the course were appreciated (data not shown).
Further supporting the importance of personal learning in this course were data about the match. In the end-of-course survey, students indicated that their primary reason for taking the course was that the content would be valuable, given their field of choice and/or that it would help them be more “marketable” for match in their field of choice (Table 5). The end-of-course survey results indicated that most students anticipated using the foundational science knowledge learned in the course in their future clinical training and practice (Table 3). VUSM post-clerkship students chose from a menu of 15 courses, and these data indicate that they chose the Clinical Cancer Medicine ISC to meet a personal need to learn more content in this area, given in what field they wanted to match.
Course Improvements
At the end of every AY, each ISC underwent a comprehensive course consultation and quality improvement process that focused on student evaluation data, foundational science and patient care integration, and assessment best practices [20]. From these data, the course directors have made yearly improvements to the Clinical Cancer Medicine course. These improvements included the addition of three Case Discussions to add a focus on breast cancer, prostate cancer, and colorectal cancer. Prior to this addition, the course highlighted only three cancers (melanoma, lung cancer, and CML) as a model to reinforce foundational science knowledge and patient care concepts that were broadly applicable across tumor types. However, the course directors heard from students, over many offerings, that they wanted to learn more about the most common cancers in the US. This feedback led the course directors to add these three sessions to complete the coverage of the three most common cancers in males and females in the US.
The course directors also heard from students early in the course offering that it was sometimes challenging to make connections between the foundational science presented in the primary literature and the patient care activity in the application activity during TBL. These comments prompted the inclusion of a 45-min “debrief session” after completion of the iRAT and gRAT for each TBL to help contextualize the foundational sciences learned. During this debrief session, the course director led discussed the rationale behind the selection of the manuscripts and explicitly made connections between patient care and the foundational sciences, which was favorably received by students.
The course directors also made significant changes to course assessments based on student feedback. This included increasing the number of competency-based assessments during classroom-based sessions to make a comprehensive student assessment. Procuring competency-based assessments from some clinical experiences was sometimes challenging. The course directors also reduced the clinical experience essay questions from three to two to ensure that all students had time to thoughtfully complete all course activities.
The Clinical Cancer Medicine ISC included material that is at the cutting edge of oncology. Cancer is a rapidly evolving field, which required the course directors to make course changes before each academic year. This included the addition of immunotherapy, other new therapeutic modalities, and the use of cell-free tumor DNA. Furthermore, the course directors and seminar speakers consistently changed guidelines to cancer screening and updated clinical cases as guidelines were updated.
Potential Challenges
VUSM graduation requirements include that students complete at least four ISCs during their third and fourth years of medical school. There were 15 ISCs offered covering a broad range of topics including diabetes, emergency medicine, medical imaging and anatomy, sexual health, global health, and palliative care [45]. Each course was offered at least two times per year in the highest student-demand months to a variable number of students based on course-specific capacity. Students enrolled in courses that are of the highest interest to them, and those courses, typically, were ones that were perceived as more broadly applicable (data not shown). Although match data indicated that students who took this course match in a variety of disciplines (Table 5), student focus group data showed that the Clinical Cancer Medicine ISC was sometimes perceived as being more narrowly focused (i.e., only applicable to oncologists and focused only on molecular biology). This ISC had the capacity to enroll up to 12 students per offering due to limited clinical placements; however, course enrollment averaged eight students per offering. The course was not offered to medical students in AY17–18 due to lack of enrollment, for reasons that are unclear. After that academic year, changes to the course were made as described above and the course name was changed from Precision Cancer Medicine to Clinical Cancer Medicine to highlight the clinical relevance of the course, with increased enrollment in subsequent years.
As shown in the sample student schedule (Fig. 2) every course offering demanded dedicated time by many faculty, diversity of classroom-based activities, and a breadth of clinical placements. As a result, every course offering was not sequenced the same due to faculty availability. In addition, every student’s schedule was different as we accommodated personal learning goals. Furthermore, the need to update course materials every AY due to the rapidly evolving landscape of cancer care led to an extraordinary amount of effort by our participating faculty. To help alleviate these challenges, VUSM has an incredible administrative team to support the course directors in scheduling events, reserving classrooms, and uploading documents and assessments to our VSTAR online learning platform. For our course, we also onboarded fellows as CBL facilitators and have created more sustainable materials, where possible (i.e., online modules and video recordings).
Future Directions
In future offerings of the Clinical Cancer Medicine ISC, we would like to integrate additional topics into existing course activities and add other experiences to enrich learning. Cancer prevention is an important part of clinical oncology but is not discussed in depth in this course. We aim to give students the opportunity to practice motivational interviewing skills on healthy behavioral changes such as smoking cessation in a clinical simulation setting. Furthermore, we would like to include a 2-h community survivorship experience to reinforce the psychosocial, financial, and physical implications of cancer care. While this course provides opportunities to discuss cancer disparities and cancer health care inequity, we aim to intentionally integrate these topics across existing sessions.
We would like to collect data to determine the impact of this course on career trajectory (e.g., specialty, research interests) and eventual clinical practice. Given the personalized nature of the Immersion Phase of Curriculum 2.0, there are several confounding factors that may influence clinical practice between the time students take this course and when they begin independent practice (i.e., residency). As such, we are interested in collectively measuring knowledge transfer and changes in practice for all students, post-graduation, as a result of the Immersion Phase Curriculum.
Conclusion
In summary, the Clinical Cancer Medicine ISC serves as an example of how precision oncology can be successfully incorporated into post-clerkship undergraduate medical education. This course facilitates meaningful integration of cancer biology and precision medicine, with active participation in clinical oncology experiences. The small size of this course and the specific educational activities allowed for personalized learning based on students’ interests and career aspirations, which further enhanced student investment in the topic. Notably, most students who took this course were highly satisfied with the integration of foundational sciences with clinical experiences and most anticipated using the foundational science knowledge acquired through this course in their future clinical training and practice. It is possible that course directors who represent medicine and research (in this case medical oncology, surgical oncology, and basic science in cancer biology) were able to collaborate successfully to deliver this exciting curriculum, with substantial support from the medical school.
Acknowledgements
We thank Dr. Bonnie Miller and the Vanderbilt University School of Medicine (VUSM) leadership for their support. We also thank the faculty who delivered cancer patient care and/or foundational sciences education in this course. Furthermore, we thank the Master Science Teachers and students for their honest and constructive course feedback. Special thanks are given to Brenna Hansen, LaToya Ford, and Bethanie McCrary for their administrative support and the VUSM Curriculum Evaluation & Student Assessment team. Finally, we appreciate the work of cancer survivors and advocates for enriching the student experience.
Author Contribution
All authors contributed to the study conception, design, and/or writing of the manuscript. Material preparation was performed by MH, VK, and KBD; data collection was performed by KBD; and data analysis was performed by CZ, KS, XL, and KBD. The first draft of the manuscript was written by CZ, KS, XL, and KBD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Kimberly Brown Dahlman was supported in part by grants 5P30CA068485-21, 2P50CA098131-11, and 5T32CA009582-32 from the National Institutes of Health (NIH), and the TJ Martell Foundation. The innovation described in this study was implemented with partial financial support from the American Medical Association (AMA) as part of its Accelerating Change in Medical Education Initiative. The content of this manuscript reflects the experience of VUSM and does not necessarily represent the views of AMA or other participants in this Initiative.
Declarations
Ethics Approval
This study was approved by the Vanderbilt Institutional Review Board (study #200875) and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Conflict of Interest
KBD receives contracted research funding from Kadmon Holdings, Inc. CZ, XL, KPS, LE, WBC, MH, and VK declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xuanyi Li and Kaustav P. Shah these authors contributed equally.
References
- 1.McGrath S, Ghersi D. Building towards precision medicine: empowering medical professionals for the next revolution. BMC Med Genomics. 2016;9(1):23. doi: 10.1186/s12920-016-0183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 3.Rubanovich CK, Cheung C, Mandel J, Bloss CS. Physician preparedness for big genomic data: a review of genomic medicine education initiatives in the United States. Hum Mol Genet. 2018;27(R2):R250–R258. doi: 10.1093/hmg/ddy170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eden C, Johnson KW, Gottesman O, Bottinger EP, Abul-Husn NS. Medical student preparedness for an era of personalized medicine: findings from one US medical school. Per Med. 2016;13(2):129–141. doi: 10.2217/pme.15.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green JS, O'Brien TJ, Chiappinelli VA, Harralson AF. Pharmacogenomics instruction in US and Canadian medical schools: implications for personalized medicine. Pharmacogenomics. 2010;11(9):1331–1340. doi: 10.2217/pgs.10.122. [DOI] [PubMed] [Google Scholar]
- 6.Oskvarek J, Braunstein S, Farnan J, Ferguson MK, Hahn O, Henderson T, et al. Medical student knowledge of oncology and related disciplines: a targeted needs assessment. J Cancer Educ. 2016;31(3):529–532. doi: 10.1007/s13187-015-0876-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neeley BC, Golden DW, Brower JV, Braunstein SE, Hirsch AE, Mattes MD. Student perspectives on oncology curricula at United States medical schools. J Cancer Educ. 2019;34(1):56–58. doi: 10.1007/s13187-017-1265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattes MD, Patel KR, Burt LM, Hirsch AE. A nationwide medical student assessment of oncology education. J Cancer Educ. 2016;31(4):679–686. doi: 10.1007/s13187-015-0872-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Potosky AL, Han PK, Rowland J, Klabunde CN, Smith T, Aziz N, et al. Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med. 2011;26(12):1403–1410. doi: 10.1007/s11606-011-1808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilcox RL, Adem PV, Afshinnekoo E, Atkinson JB, Burke LW, Cheung H, et al. The Undergraduate Training in Genomics (UTRIG) Initiative: early & active training for physicians in the genomic medicine era. Per Med. 2018;15(3):199–208. doi: 10.2217/pme-2017-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McRae RJ. Oncology education in medical schools: towards an approach that reflects Australia’s health care needs. J Cancer Educ. 2016;31(4):621–625. doi: 10.1007/s13187-016-1088-0. [DOI] [PubMed] [Google Scholar]
- 12.Kwan JY, Nyhof-Young J, Catton P, Giuliani ME. Mapping the future: towards oncology curriculum reform in undergraduate medical education at a Canadian medical school. Int J Radiat Oncol Biol Phys. 2015;91(3):669–677. doi: 10.1016/j.ijrobp.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 13.Pavlidis N, Vermorken JB, Stahel R, Bernier J, Cervantes A, Pentheroudakis G, et al. Undergraduate training in oncology: an ESO continuing challenge for medical students. Surg Oncol. 2012;21(1):15–21. doi: 10.1016/j.suronc.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Cecilio-Fernandes D, Aalders WS, Bremers AJA, Tio RA, de Vries J. The impact of curriculum design in the acquisition of knowledge of oncology: comparison among four medical schools. J Cancer Educ. 2018;33(5):1110–1114. doi: 10.1007/s13187-017-1219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boehler M, Advani V, Schwind CJ, Wietfeldt ED, Becker Y, Lewis B, et al. Knowledge and attitudes regarding colorectal cancer screening among medical students: a tale of two schools. J Cancer Educ. 2011;26(1):147–152. doi: 10.1007/s13187-010-0161-3. [DOI] [PubMed] [Google Scholar]
- 16.Villarreal-Garza C, Garcia-Aceituno L, Villa AR, Perfecto-Arroyo M, Rojas-Flores M, Leon-Rodriguez E. Knowledge about cancer screening among medical students and internal medicine residents in Mexico City. J Cancer Educ. 2010;25(4):624–631. doi: 10.1007/s13187-010-0098-6. [DOI] [PubMed] [Google Scholar]
- 17.Mohyuddin N, Langerman A, LeHew C, Kaste L, Pytynia K. Knowledge of head and neck cancer among medical students at 2 Chicago universities. Arch Otolaryngol Head Neck Surg. 2008;134(12):1294–1298. doi: 10.1001/archotol.134.12.1294. [DOI] [PubMed] [Google Scholar]
- 18.Geller AC, Prout M, Sun T, Lew RA, Culbert AL, Koh HK. Medical students' knowledge, attitudes, skills, and practices of cancer prevention and detection. J Cancer Educ. 1999;14(2):72–77. doi: 10.1080/08858199909528583. [DOI] [PubMed] [Google Scholar]
- 19.MD Curriculum [cited 2020. Available from: www.medschool.vanderbil.edu/curriculum/.
- 20.Dahlman KB, Weinger MB, Lomis KD, Nanney L, Osheroff N, Moore DE, Jr, et al. Integrating foundational sciences in a clinical context in the post-clerkship curriculum. Med Sci Educ. 2018;28(1):145–154. doi: 10.1007/s40670-017-0522-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lomis KD, Russell RG, Davidson MA, Fleming AE, Pettepher CC, Cutrer WB, et al. Competency milestones for medical students: design, implementation, and analysis at one medical school. Med Teach. 2017;39(5):494–504. doi: 10.1080/0142159X.2017.1299924. [DOI] [PubMed] [Google Scholar]
- 22.Pettepher CC, Lomis KD, Osheroff N. From theory to practice: utilizing competency-based milestones to assess professional growth and development in the foundational science blocks of a pre-clerkship medical school curriculum. Med Sci Educ. 2016;26(3):491–497. doi: 10.1007/s40670-016-0262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cutrer WB, Miller B, Pusic MV, Mejicano G, Mangrulkar RS, Gruppen LD, et al. Fostering the development of master adaptive learners: a conceptual model to guide skill acquisition in medical education. Acad Med. 2017;92(1):70–75. doi: 10.1097/ACM.0000000000001323. [DOI] [PubMed] [Google Scholar]
- 24.Mylopoulos M, Lohfeld L, Norman GR, Dhaliwal G, Eva KW. Renowned physicians’ perceptions of expert diagnostic practice. Acad Med. 2012;87(10):1413–1417. doi: 10.1097/ACM.0b013e31826735fc. [DOI] [PubMed] [Google Scholar]
- 25.Mylopoulos M, Regehr G. How student models of expertise and innovation impact the development of adaptive expertise in medicine. Med Educ. 2009;43(2):127–132. doi: 10.1111/j.1365-2923.2008.03254.x. [DOI] [PubMed] [Google Scholar]
- 26.Mylopoulos M, Woods N. Preparing medical students for future learning using basic science instruction. Med Educ. 2014;48(7):667–673. doi: 10.1111/medu.12426. [DOI] [PubMed] [Google Scholar]
- 27.Spickard A, 3rd, Ahmed T, Lomis K, Johnson K, Miller B. Changing medical school IT to support medical education transformation. Teach Learn Med. 2016;28(1):80–87. doi: 10.1080/10401334.2015.1107488. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt HG, Rotgans JI, Yew EH. The process of problem-based learning: what works and why. Med Educ. 2011;45(8):792–806. doi: 10.1111/j.1365-2923.2011.04035.x. [DOI] [PubMed] [Google Scholar]
- 29.Davis MH. AMEE Medical Education Guide No. 15: Problem-based learning: a practical guide. Med Teach. 1999;21(2):130–140. doi: 10.1080/01421599979743. [DOI] [PubMed] [Google Scholar]
- 30.Parmelee D, Michaelsen LK, Cook S, Hudes PD. Team-based learning: a practical guide: AMEE guide no. 65. Med Teach. 2012;34(5):e275–e287. doi: 10.3109/0142159X.2012.651179. [DOI] [PubMed] [Google Scholar]
- 31.Rao S, Pitel B, Wagner AH, Boca SM, McCoy M, King I, et al. Collaborative, multidisciplinary evaluation of cancer variants through virtual molecular tumor boards informs local clinical practices. JCO Clin Cancer Inform. 2020;4:602–613. doi: 10.1200/CCI.19.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kulasegaram KM, Martimianakis MA, Mylopoulos M, Whitehead CR, Woods NN. Cognition before curriculum: rethinking the integration of basic science and clinical learning. Acad Med. 2013;88(10):1578–1585. doi: 10.1097/ACM.0b013e3182a45def. [DOI] [PubMed] [Google Scholar]
- 33.Finnerty EP, Chauvin S, Bonaminio G, Andrews M, Carroll RG, Pangaro LN. Flexner revisited: the role and value of the basic sciences in medical education. Acad Med. 2010;85(2):349–355. doi: 10.1097/ACM.0b013e3181c88b09. [DOI] [PubMed] [Google Scholar]
- 34.Goldman E, Schroth WS. Perspective: deconstructing integration: a framework for the rational application of integration as a guiding curricular strategy. Acad Med. 2012;87(6):729–734. doi: 10.1097/ACM.0b013e318253cad4. [DOI] [PubMed] [Google Scholar]
- 35.Kulasegaram K, Manzone JC, Ku C, Skye A, Wadey V, Woods NN. Cause and effect: testing a mechanism and method for the cognitive integration of basic science. Acad Med. 2015;90(11 Suppl):S63–S69. doi: 10.1097/ACM.0000000000000896. [DOI] [PubMed] [Google Scholar]
- 36.Ling Y, Swanson DB, Holtzman K, Bucak SD. Retention of basic science information by senior medical students. Acad Med. 2008;83(10 Suppl):S82–S85. doi: 10.1097/ACM.0b013e318183e2fc. [DOI] [PubMed] [Google Scholar]
- 37.de Bruin AB, Schmidt HG, Rikers RM. The role of basic science knowledge and clinical knowledge in diagnostic reasoning: a structural equation modeling approach. Acad Med. 2005;80(8):765–773. doi: 10.1097/00001888-200508000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt HG, Machiels-Bongaerts M, Hermans H, ten Cate TJ, Venekamp R, Boshuizen HP. The development of diagnostic competence: comparison of a problem-based, an integrated, and a conventional medical curriculum. Acad Med. 1996;71(6):658–664. doi: 10.1097/00001888-199606000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Woods NN. Science is fundamental: the role of biomedical knowledge in clinical reasoning. Med Educ. 2007;41(12):1173–1177. doi: 10.1111/j.1365-2923.2007.02911.x. [DOI] [PubMed] [Google Scholar]
- 40.Woods NN, Brooks LR, Norman GR. The value of basic science in clinical diagnosis: creating coherence among signs and symptoms. Med Educ. 2005;39(1):107–112. doi: 10.1111/j.1365-2929.2004.02036.x. [DOI] [PubMed] [Google Scholar]
- 41.Woods NN, Neville AJ, Levinson AJ, Howey EH, Oczkowski WJ, Norman GR. The value of basic science in clinical diagnosis. Acad Med. 2006;81(10 Suppl):S124–S127. doi: 10.1097/00001888-200610001-00031. [DOI] [PubMed] [Google Scholar]
- 42.McKillip RP, Hahn OM, Bartkowiak B, Rosenberg CA, Olopade OI, Arora VM, et al. Implementation of a novel medical school multidisciplinary and interprofessional oncology curriculum: a mixed method study. J Cancer Educ. 2019;34(1):50–55. doi: 10.1007/s13187-017-1264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abacioglu U, Sarikaya O, Iskit S, Sengoz M. Integration of a problem-based multidisciplinary clinical cancer management course into undergraduate education. J Cancer Educ. 2004;19(3):144–148. doi: 10.1207/s15430154jce1903_7. [DOI] [PubMed] [Google Scholar]
- 44.Ha FJ, Parakh S. Novel approaches to undergraduate oncology education. J Cancer Educ. 2018;33(3):500–504. doi: 10.1007/s13187-016-1109-z. [DOI] [PubMed] [Google Scholar]
- 45.Wong RE, Quach HT, Wong JS, Laxton WH, Nanney LB, Motuzas CL, Pearson AS. Integrating specialty-specific clinical anatomy education into the post-clerkship curriculum. Medical Science Educator. 2020;30:487–497. doi: 10.1007/s40670-019-00833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]