Abstract
Cardiac impalement is a rare and usually fatal injury. Immediate recognition and surgical intervention are decisive factors for patient survival. This is a reported case of cardiac impalement with left ventricular transfixation, whose prehospital management, surgical treatment and postoperative care were successful.
Keywords: Penetrating cardiac injury, Cardiac impalement, Thoracic trauma, Penetratin lesion
Introduction
Penetrating cardiac trauma is a rare event (0.1% of trauma admissions) [1]. Impalement injuries occur when a foreign body penetrates a body cavity or extremity and transfixes the internal structures [3]. Data from the National Trauma Data Bank version 3.0 points out that among cardiac penetrating trauma cases, cardiac impalement injuries account for only 0.9% of all such injuries. Unlike injuries that cause only perforation of the heart, impalement trauma is almost always fatal, and patients rarely reach the care center [3]. Considering the severity of the injuries and the risk of imminent death [4] a rapid initial assessment is essential and immediate surgical management is imperative [2].
Case report
Male patient, 70 years old, victim of self-aggression with impalement by tool (Phillips screwdriver) in the left hemithorax. In the pre-hospital care, the object was fixed on the thorax (Fig. 1) and the patient was immobilized with a rigid board and cervical collar. Oxygenation was ensured via orotracheal intubation and peripheral venous access with serum therapy. The patient was quickly transported via helicopter to the emergency department. On admission, he was pale, with decreased peripheral perfusion, hypotensive, tachycardic, intubated, and with decreased vesicular murmur in the left hemithorax. The patient was referred directly to the operating room.
Fig. 1.
Phillips® screwdriver impaled, stabilized with bandage.
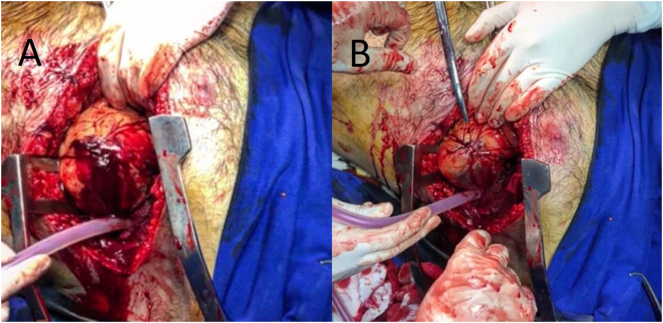
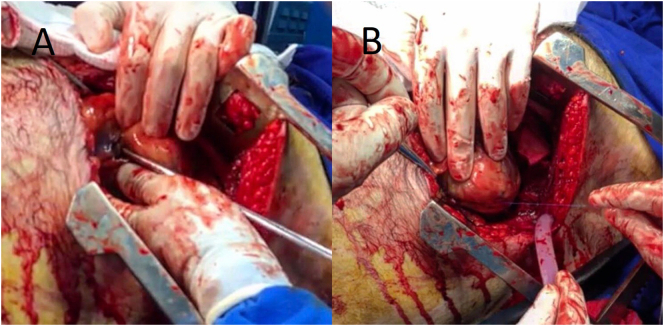
Left anterolateral thoracotomy was performed in the 5th intercostal space (ICS). After opening the cavity, a tense, dark-colored pericardial sac was noted, indicating cardiac tamponade. Longitudinal pericardiotomy was performed, cutting parallel and anteriorly to the phrenic nerve, with immediate extravasation of approximately 200 ml of blood. A stabbing weapon transfixing the left ventricle (LV) was identified. After removal of the sharp object, the cardiac lesions were observed in the LV anterior wall near the anterior descending artery (Fig. 2), which presented bleeding from inside this cardiac chamber, and in the LV posterior wall, near the posterior descending artery (Fig. 3). After digital tamponade of the injured sites, the anterior orifice was repaired by continuous suture with 3-0 polypropylene yarn; the posterior orifice was sutured under a square fragment (4cm [2]) with 3-0 polypropylene suture. After repair of the lesions and review of hemostasis, two water sealed drains (UWSD) were inserted and the surgery was concluded.
Fig. 2.
A: Orifice in the anterior wall of the LV, close to the anterior descending artery; B: Repair of the anterior hole with 3-0 polypropylene suture.
Fig. 3.
A: Orifice in the posterior wall of the LV, close to the posterior descending artery; B: Repair of the posterior orifice with 3-0 polypropylene suture and Gelfoam®.
The patient was stable and then referred to the Intensive Care Unit (ICU). He developed paroxysmal atrial fibrillation and atrial flutter, controlled with amiodarone, carvedilol and full anticoagulation. He showed good recovery after clinical support measures and intensive care. Transthoracic echocardiogram on the fifth postoperative day showed LV with increased mass, mild global systolic dysfunction and normal diastolic function, in addition to enlargement in left atrium and right ventricle. There was also a psychiatric evaluation. He remained in ICU for 14 days and was discharged 20 days after the operation.
Despite the severity of the cardiac lesions suffered by the patient, he returned to his daily life after hospital discharge.
Discussion
Most Penetrating Cardiac Trauma (PCT) occur from stabbing weapons or firearm projectiles [2]. In the care, one should consider that penetrating injuries in the thorax or abdomen have the potential to cause cardiac injury, especially when they occur within the area known as Ziedler's area (Cardiac box), an area limited superiorly by the clavicles, laterally by the hemiclavicular lines and inferiorly by the costal margins [5]. Because it comprises most of the anterior face of the heart, the right ventricle is the most vulnerable cardiac chamber to penetrating injuries [2]. A relative frequency of 43% is estimated for the right ventricle and 34% for the left ventricle [2], [6].
The majority of penetrating cardiac injuries have life-threatening complications: cardiac tamponade, hemorrhage, hypovolemic shock, and arrhythmias [3], [4].
Impalement cardiac injuries are an extremely rare type of PCT and survival outcomes are even rarer [3]. National Trauma Data Bank 3.0 counted 2016 patients with PCT out of a total of 1,310,720 patients. 13 out of 19 patients with cardiac impalement died. This corresponds to a 68.4% mortality rate. However, this rate may be underestimated, because many victims die at the scene [1].
Pre-hospital care (PHC) is the main variable related to prognosis [4]. A retrospective study showed that the improvement in PHC resulted in better monitored parameters at the emergency room and reduced mortality from PCT [7]. The approach in impalement injuries should be to stabilize the object, ideally, not manipulating or removing it before direct visualization is guaranteed [8]. If cardiac trauma is suspected, a quick transport to the closest trauma center is crucial for patient survival and must be priorized [9], [10]. Most patients are shocked, requiring immediate resuscitation manouvers and surgical treatment [2], [5]. However, stable patients may benefit from complementary exams. In this case, imaging exams were not performed because of the patient instability, high probability of cardiac injury and tamponade - related to the location, direction and pulsatile pattern of the object and requiring immediate intervention.
Immediate surgery is the only significant treatment [2]. A anterolateral thoracotomy, at the 4th or 5th ICS is the beginning [2], [4]. There are several techniques for temporary control of the lesion: digital maneuver, use of foley catheter and skin staples [11]. It is not necessary to completely stop the bleeding, but to reduce it, in order to facilitate cardiac repair. The digital compression is the simplest and most direct method [5]. The definitive repair can be realized with continuous or separate stitches, with 3-0 diameter polypropylene sutures, using pledgets (preferably in ventricular wounds. The surgeon should cover as much myocardial tissue as possible, because superficial repairs can cause more injuries to the tissue around the wound, usually friable [5]. Posterior cardiac wounds are a problem because they require heart elevation, which often leads to hypotension, bradycardia, and possibly cardiac arrest. Because of these risks, the lifting should not be extended beyond necessary. When closing the wounds, the sutures usually cannot be tied at the same moment when placed, but only after a moment of recovery in the normal position [12]. For the posterior hole approach in this case, a local hemostatic fragment was anchored, reducing the amount of stitches and minimizing cardiac manipulation.
Studies about surgical complications from PCT are limited. In the immediate postoperatory, monitoring bleeding and the recurrence of pericardial fluid is required, because they are both risk factors for new tamponade, and cardiogenic shock. These patients are at risk for pericarditis and post-cardiac injury syndromes [13]. Complications also include those seen after elective surgery, including cardiac dysfunction from infarction, arrhythmias, surgical site infection, sternal dehiscence, and mediastinitis [14]. In the present case, the patient developed atrial fibrillation and flutter. They were controlled with medication in intensive care. He also had a mild global systolic dysfunction on echocardiography, probably related to his age or to the cardiac lesion itself.
This case is rare, because even after an uncommon severe injury, a good outcome happened. Fast and efficient PHC, immediate transfer to a trauma center, primary and secondary evaluation according to the ATLS® protocol, recognition, immediate surgery and intensive postoperative care contributed to the good prognosis.
Acknowledgements/disclosures
-
●
The authors are grateful for the translation done by Adam Lai.
-
●
The manuscript did not require, nor did receive any funding from industry or otherwise.
-
●
The authors have no disclosures relevant to the topic.
References
- 1.Asensio J.A., Ogun O.A., Petrone P. Penetrating cardiac injuries: predictive model for outcomes based on 2016 patients from the national trauma data bank. Eur. J. Trauma Emerg. Surg. 2017:1–7. doi: 10.1007/s00068-017-0806-6. [DOI] [PubMed] [Google Scholar]
- 2.Kang N., Hsee L., Rizoli S., Alison P. Penetrating cardiac injury: overcoming the limits set by nature. Injury. 2009;40(9):919–927. doi: 10.1016/j.injury.2008.12.008. Sep. [DOI] [PubMed] [Google Scholar]
- 3.Pradhan S., Sapkota R., Shrestha U.K., Amatya R., Koirala B. Impalement injury to the heart. Kathmandu Univ. Med. J. 2011;33(1):80–82. doi: 10.3126/kumj.v9i1.6270. [DOI] [PubMed] [Google Scholar]
- 4.Karigyo C.J.T., Silva D.R., Pelisson T.M., Fan O.G., Tarasiewich M.J. Trauma cardíaco penetrante. Rev. Med. Res. 2013;15(3):198–206. [Google Scholar]
- 5.O’Connor J., Ditillo M., Scalea T. Penetrating cardiac injury. J. R. Army Med. Corps. 2009;155(3):185–190. doi: 10.1136/jramc-155-03-02. Sep. [DOI] [PubMed] [Google Scholar]
- 6.Asensio J.A., Garcia-Nunez L.M., Petrone P. Trauma to the heart. In: Feliciano D.V., Mattox K.L., Moore E.E., editors. Trauma. 6th ed. McGraw Hill; New York: 2008. pp. 569–588. [Google Scholar]
- 7.Pereira B.M., Nogueira V.B., Calderan T.R., Villaça M.P., Petrucci O., Fraga G.P. Penetrating cardiac trauma: 20-y experience from a university teaching hospital. J. Surg. Res. 2013;183(2):792–797. doi: 10.1016/j.jss.2013.02.015. Aug. [DOI] [PubMed] [Google Scholar]
- 8.Shimokawa S., Shiota K., Ogata S., Toyohira H., Moriyama Y., Taira A. Impalement injury of the thorax: report of a case. Surg. Today. 1994;24(10):926–928. doi: 10.1007/BF01651012. [DOI] [PubMed] [Google Scholar]
- 9.Ivatury R.R., Mattox K.L., Feliciano D.V., Moore E.E. 4th ed. McGraw-Hill; New York: 2000. Trauma. The Injured Heart. [Google Scholar]
- 10.Haas B., Nathens A.B. Pro/con debate: is the scoop and run approach the best approach to trauma services organization? Crit. Care. 2008;12:224. doi: 10.1186/cc6980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degiannis E., Bowley D.M., Westaby S. Penetrating cardiac injury. Ann. R. Coll. Surg. Engl. 2005;87(1):61–63. doi: 10.1308/1478708051207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kokotsakis J., Hountis P., Antonopoulos N., Skouteli E., Athanasiou T., Lioulias A. Intravenous adenosine for surgical management of penetrating heart wounds. Tex. Heart Inst. J. 2007;34(1):80–81. [PMC free article] [PubMed] [Google Scholar]
- 13.Wessman D.E., Stafford C.M. The Postcardiac Injury Syndrome: Case Report and Review of the Literature. Vol. 99. 2006. pp. 309–314. 3. [DOI] [PubMed] [Google Scholar]
- 14.Ball L., Costantino F., Pelosi P. Postoperative complications of patients undergoing cardiac surgery. Curr. Opin. Crit. Care. 2016;22:386. doi: 10.1097/MCC.0000000000000319. [DOI] [PubMed] [Google Scholar]