Abstract
Assessing the impact of the COVID-19 pandemic on perceived stress in older adults is critical to understanding how to best support elderly individuals navigating stressful situations, with the aim to lessen the impact of stressors on their brain health. Here, we collected measures on perceived stress, resilience, and behavioral coping strategies, in the context of the COVID-19 pandemic, in a cross-sectional sample of 141 community dwelling older adults (mean age = 74.4 ± 8.4, 59% females) who were part of two longitudinal observational studies in Massachusetts, U.S. Our results indicate that participants demonstrated moderate levels of stress related to COVID-19 and showed relatively high levels of resilience. Higher resilience was associated with greater use of adaptive coping behaviors and less use of maladaptive coping behaviors. The use of maladaptive coping strategies was associated with more stress. Moreover, hierarchical regression analyses revealed that resilience was the strongest unique predictor of stress, thus, largely accounting for the observed coping-outcome associations. Individual differences in resilience levels moderated the effects of two coping strategies (planning and self-blame) on stress. Specifically, planning was associated with increased levels of stress for people with low resilience. In contrast, high personal resilience attenuated the negative effect of self-blame on their stress levels. Taken together, our findings suggest that resilience is critical for coping with stress during the COVID-19 pandemic. Future approaches for augmenting resilience could prove to be important potential interventions to help support older adults navigating stressful situations as well as lessen adverse effects on neurocognitive and mental health in the future.
Keywords: COVID-19, Older adults, Stress, Resilience, Coping
1. Introduction
The coronavirus (COVID-19) pandemic caused by the 2019 novel coronavirus SARS-CoV-2, has become a global public health crisis and a major source of stress. This is especially true in older adults, as the risk of developing more severe complications from COVID-19 has been shown to increase with age. As of March 2021, there have been nearly 30,000,000 cases and more than 500,000 deaths attributed to COVID-19 in the USA, of which nearly 80% of the deaths were among people over the age of 65 (www.CDC.gov). The impact of the current pandemic on the incidence and severity of stress-related disorders is unknown and is expected to be highly heterogenous (Vinkers et al., 2020). For older adults, there is evidence suggesting that chronic stress may even lead to higher rates of age-related diseases, such as Alzheimer's disease (AD) (Graham et al., 2006), and to worsening mental health. There is a need to understand the impact of the COVID-19 pandemic on perceived stress in older adults and how best to advise and support older adults during this time to lessen adverse effects on neurocognitive and mental health outcomes (Holmes, 2020).
Even though we are all experiencing the same event, an individual's perception of how stressful this event is for them is highly variable. Thus, different people may appraise the same stressor differently. Several factors influence a person's perceived level of stress, with resilience and coping being the most studied in humans (MacLeod et al., 2016). Resilience has been defined by the American Psychological Association (APA) as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress,” or “bouncing back” from difficult experiences (The American Psychological Association 2015). Although still a matter of debate, the APA's definition of resilience as a process versus a personality trait (often termed resiliency) implies that each individual has the capacity to build and demonstrate resilience, regardless of their socioeconomic backgrounds, personal experiences, or social environments (Feder et al., 2019). Importantly, with respect to stress, previous studies have found that individuals demonstrating high resilience later in life required less time to recover and more quickly terminate the stress response after experiencing stressor exposure thereby reducing the damaging effect of any chronic elevations of stress hormones (i.e., glucocorticoids; Sampedro-Piquero et al., 2018). The second factor that can influence a person's perceived level of stress is coping strategies, defined as behaviors to protect oneself by avoiding psychological harm from bad experiences (Pearlin and Schooler 1978). Previous research has shown that certain coping strategies can alleviate stress and promote positive psychological outcomes (Parker and Endler 1992; Endler and Parker 1994). To this effect, the Centers for Disease Control and Prevention (CDC) has recommended several coping strategies that may be particularly useful during the COVID-19 pandemic, including 1) Pause (breathe, notice how you feel); 2) Take breaks from COVID-19 content; 3) Make time to sleep and exercise; 4) Reach out and stay connected; and 5) Seek help if feeling overwhelmed or unsafe. However, whether these recommendations are being implemented amongst older adults during this pandemic remains unknown. Finally, previous research has proposed a link between resilience and coping, such that the efficacy of any given behavioral strategy may depend on a person's level of resilience (Smith et al., 2016). Specifically, resilience has been proposed to influence coping efficacy through two theoretical pathways (Lazarus and Folkman 1984; Zeidner, Saklofske et al., 1996): First, according to the matching hypothesis, high resilience may increase the use of proactive/task-oriented coping strategies (including problem solving, action planning and positive reappraisal) and reduce the use of reactive coping strategies, including non-constructive emotion-oriented strategies such as rumination and self-blame. Second, the goodness-of-fit hypothesis states that high resilience may moderate the efficacy of coping strategies such that it amplifies the positive psychological effects and dampens the negative psychological effects of coping. Thus, especially for older adults, stress, resilience and coping may all interact with each other to determine the health outcome of an individual.
The overall objective of this study was to investigate perceived levels of stress, resilience, and coping strategies related to COVID-19 in a sample of community dwelling older adults who were part of two longitudinal observational studies in Massachusetts, U.S. We used validated questionnaires as well as questions formulated based on information from the Centers for Disease Control and Prevention (CDC) on recommended coping strategies to use during the Covid-19 pandemic. With regard to the matching hypothesis, we expected that increased resilience would be related to increased use of proactive coping strategies and decreased use of reactive coping strategies. In addition, we were interested in investigating both main effects of resilience and coping strategies on stress, as well as examining whether resilience, as an important coping resource, would moderate the effect of different coping strategies on the perceived level of stress. Specifically, with regard to the goodness-of-fit hypothesis we expected that increased resilience would interact with coping strategies such that it increased the effectiveness of proactive coping and dampened the negative psychological effects of maladaptive coping behaviors on individuals’ stress levels.
2. Methods
2.1. Procedure
The COVID-19 survey was reviewed and approved by the Partners Institutional Review board (IRB) as a sub-study for participants who are actively enrolled in longitudinal observational research studies of older adults (Harvard Aging Brain Study, HABS, P01 AG036694, PI: Sperling and Johnson; and the Instrumental Activities of Daily Living Study, IADL, R01 AG053184, PI: Marshall) at Massachusetts General Hospital, in Boston, MA, U.S. Both the HABS and IADL studies are carried out within the integrated clinical research, imaging, and neuroscience resources directed toward the study of Alzheimer's disease (AD) across Brigham and Women's Hospital (BWH) and the Massachusetts General Hospital (MGH). HABS comprised approximately 300 participants, of which 254 are currently actively enrolled in the study. The participants in HABS were all cognitively normal at baseline and have been evaluated longitudinally with multi-modal neuroimaging and extensive clinical evaluations. Specifically, participants have been studied annually up to 10 years with the first participants now entering year 10. About 20% of the participants now meet mild cognitive impairment (MCI) or AD criteria over the 10 years of follow-up. IADL is a natural history, non-interventional imaging 3-year study of older adult individuals who were either cognitively normal or had a diagnosis of amnestic MCI at the time of enrollment. The study is actively enrolling participants and at the time of this study it was comprised of 36 individuals. To assess clinical diagnosis, a group of 6–7 experienced clinicians hold recurrent consensus meetings to evaluate whether a participant is cognitively normal or meets criteria for either MCI or AD dementia (using same criteria as Alzheimer's Disease Neuroimaging Initiative (ADNI). The inclusion criteria for each group are as follows: Cognitively normal older individuals who have a global Clinical Dementia Rating (CDR) (Morris 1993) score of 0, a Mini-Mental State Exam (MMSE) (Folstein et al., 1975) score of 27–30, and a performance above an education adjusted cut-off score on the Logical Memory II subscale delayed paragraph recall (LM-II) of the Wechsler Memory Scale-Revised (WMS-R) (Wechsler 1981) (≥16 years of education: ≥9; 8–15 years: ≥5; 0–7 years: ≥3). MCI individuals are all amnestic (single or multiple domain) with a performance below an education adjusted cut-off score on the WMS-R LM-II (≥16 years of education: 9–11; 8–15 years: 5–9; 0–7 years: 3–6), have an MMSE score of 24–30, have a CDR global score of 0.5 (with memory box score of 0.5 or 1), and have essentially preserved IADL, as determined by a clinician.
In addition, participants in HABS and IADL are evaluated annually with a comprehensive battery of cognitive and neuropsychiatric assessments, including tests of episodic memory, executive function, global cognition, CDR and depression (using the Geriatric Depression Scale (GDS; Yesavage et al., 1983). Cognition is evaluated using the Preclinical Alzheimer Cognitive Composite-5 (PACC5) (Papp et al., 2017), a summary measure calculated as a mean of z-score performance on 5 tests sensitive to cognitive decline in at-risk individuals including global cognition, episodic and semantic memory and executive function domains. Specifically, MMSE (0–30), WMS-R Logical Memory Delayed Recall (LMDR; 0–25), the Digit-Symbol Coding Test (DSC; 0–93), the Free and Cued Selective Reminding Test-Free 1 Total Recall (FCSRT96; 0–96), and category fluency (CAT). The PACC5 is currently used as an outcome in both pharmacological and nonpharmacological secondary prevention trials (Papp et al., 2019). Finally, socioeconomic status is evaluated using the Hollingshead four-factor index (Hollingshead 1957).
Participants were sent an invitation to participate via electronic mail (e-mail), which provided them with context for the study, and included a link to access the online consent form and subsequent survey via Research Electronic Data Capture (REDCap; http://project-redcap.org/; Harris et al., 2009; Harris et al., 2019). REDCap is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources. Note that the invitation was only sent to participants with a listed email address and those who had not previously opted out of consideration for sub-studies. The flowchart in Supplemental Figure 1 shows how participants in the two cohorts were selected to take part in the study.
Completion of the survey was voluntary, and participants were instructed that they could stop at any time. They were also instructed that they could skip any questions they did not feel comfortable answering. A total of 144 participants consented to the survey. One person was excluded as he/she did not submit any responses aside from the consent form. Two people were excluded as they responded outside of the time window of the survey.
2.2. Survey timeframe and COVID-19 cases in Massachusetts
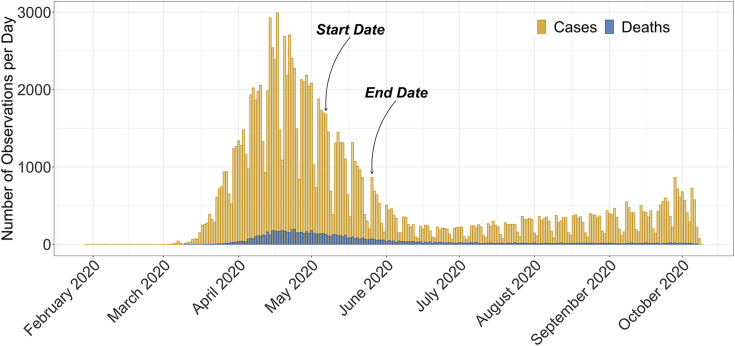
The surveys were completed between May 07, 2020 and May 26, 2020, Fig. 1 . Illustrates the time window of the survey and its relationship to observed cases and deaths in Massachusetts (data source: https://www.mass.gov). The majority of survey responses (N = 58, 41%) were received the same day the survey was sent out.
Fig. 1.
The time window of the survey with arrows showing the start date (May 7, 2020) and end date (May 26, 2020) and its relationship to observed cases and reported deaths per day in Massachusetts between February 2020 to October 2020. Data source: https://www.mass.gov.
2.3. Survey components
The survey consisted of several questionnaires which are presented in detail below and in the same order they were asked.
2.3.1. Covid-19 related questions
Three questions asked participants about their living circumstances (living alone or with others, pet ownership) during the pandemic and whether members of their social network had been diagnosed with COVID-19.
2.3.2. Questions estimating level of perceived stress
Perceived stress was measured using the Perceived Stress Scale (PSS-14 (Cohen et al., 1983); which consists of 14 question that measure the degree to which situations in a person's life are appraised as stressful. The questions are framed to ask about feelings and thoughts during the last month and participants are asked to appraise how often they have felt a certain way using a 5-point Likert scale. The total score was used to assess participants' level of stress with higher scores indicating increased perceived stress.
Using an analogous Likert scale, six additional questions were added to capture perceptions of stress relevant to the COVID-19 pandemic. These questions were derived from the CDC website (https://www.cdc.gov/coronavirus/2019-ncov/index.html) and addressed: (1) Fear and worry about my own health;(2) Fear and worry about the health of my friends and loved ones; (3) Fear and worry about my financial situation; (4) Decreased ability to concentrate;(5) Changes in my sleeping patterns; and (6) Changes in my appetite or eating patterns.
2.3.3. Questions estimating level of resilience
The Connor-Davidson Resilience Scale (CD-RISC 10) was administered to measure resilience (http://www.connordavidson-resiliencescale.com/about.php; Connor and Davidson 2003). The scale consists of 10 items that measure an individual's self-reported ability to face changes or personal problems over the past month. Items are rated on a 5-point Likert scale with higher individual and total scores indicating higher resilience.
2.3.4. Coping
The Brief COPE (Carver 1997) inventory was used to measure coping strategies. The scale assesses 14 different coping strategies; active coping, planning, positive reframing, humor, use of emotional support, use of instrumental support, acceptance, religion, self-distraction, denial, substance use, behavioral disengagement, venting, and self-blame; using 2 questions for each strategy for a total of 28 questions. Participants were asked to appraise how often they have used each strategy as it applies to them in this current situation using a 4-point Likert scale. Scores were summed and averaged for each of the 14 coping strategies, with a higher score representing more frequent use of that coping strategy.
Using an analogous Likert scale, seven questions were added to capture coping strategies recommended during the COVID-19 pandemic on the CDC website (https://www.cdc.gov/coronavirus/2019-ncov/index.html): (1) I've been taking breaks from watching, reading, or listening to news stories, including social media; (2) I've been practicing mindful movements (e.g., yoga, qigong, tai chi); (3) I've been doing simple breathing exercises; (4) I've been getting plenty of sleep; (5) I've been eating healthy and well-balanced meals; (6) I've been exercising regularly (e.g., walking, jogging, bicycling, resistance exercises); (7) I've been taking action to try to help others (e.g., sewing masks, donating money and/or supplies).
2.3.5. Statistical methods
All statistical analyses were performed using R 3.6.3 (https://www.R-project.org/). Descriptive statistics were performed to evaluate participants’ demographic and psychological characteristics. Correlation analyses were conducted to investigate the associations between stress and resilience to demographic data, and t-tests were used to examine differences in stress and resilience for women and men. Correlation analyses using linear mixed effects models were also conducted to investigate the associations between stress, resilience and coping mechanisms. Hierarchical multiple regression analyses were conducted to examine whether resilience would moderate the association between coping strategies and stress. Moderation was defined as when a model with the interaction terms accounted for significantly more variance than the model without the interaction terms and if the regression coefficient corresponding to an interaction term was statistically significant (p < 0.05). Simple slope analysis (Aiken et al., 1991) was performed in the event of a significant interaction effect to determine the relationship between coping strategy and stress at high (+1SD) and low (-1SD) levels of resilience.
To address potentially missing responses in the CD-RISC-10, we used the instructions from the CD-RISC manual (http://www.connordavidson-resiliencescale.com/faq.php). That is, at least 7 of the 10 items must have been completed in order to consider the scale as valid. Of note, no participant answered less than 7 items. For missing responses, the mean of all completed answers was used to impute the score. For all the other questionnaires, we used a threshold of less than 2% for missing responses across all participants to include that question. Of note, no question fell below this threshold. For missing data, the mean for that question across all participants was used to impute the score.
3. Results
The 141 participants (83 women, 58 men) had a mean age of 74.4, with an average of 16.8 years of education. Of the 141 in total, 109 participants came from the HABS and 32 from the IADL study. Table 1 shows participant characteristics as well as distributions of variables.
Table 1.
Demographic characteristics of participants.
| Variables | Frequency % |
S.D. ± |
Range [min; max] | Distributions | |
|---|---|---|---|---|---|
| N | 141 | ||||
| Gender (Females) | 83 | 58.87 | |||
| APOE4 (carrier) | 34 | 24.11 | |||
| CDR (score = 0) | 136 | 96.45 | |||
| Clinical diagnosis (normal) | 138 | 97.87 | |||
| Age (mean years) | 74.36 | 8.35 | [52; 91.25] | ▁▂▃▇▇▇▃▂ | |
| Education (mean years) | 16.76 | 2.56 | [12; 20] | ▃▂▁▆▁▇▁▅ | |
| MMSE (mean score) | 29.31 | 1.02 | [25; 30] | ▁▁▁▁▁▁▃▇ | |
| Depression (mean score) | 3.48 | 3.52 | [0; 19] | ▇▂▂▁▁▁▁▁ | |
| Global cognition (mean score) | 0.36 | 0.69 | [-2.1; 2.36] | ▁▁▃▆▇▇▁▁ | |
Note: CDR = clinical dementia rating scale; MMSE = Mini mental state examination. S.D. = Standard deviation. Depression was assessed using the Geriatric Depression Scale (GDS) and global cognition was assessed using the Preclinical Alzheimer Cognitive Composite-5 (PACC5). The CDR, clinical diagnosis, MMSE, depression and memory composite represents previously collected data (closest to the survey) for the participants.
The Table also shows previously collected data from our participants. That is, the global Clinical Dementia Rating (CDR; Morris 1993); mean days since administration = 230.6 ± 179.55; Mini-Mental State Examination (MMSE; Folstein et al., 1975) mean days since administration = 225.38 ± 179.71; Geriatric Depression Scale (GDS; Yesavage et al., 1983) mean days since administration = 284.3 ± 146.72 and the preclinical Alzheimer's Cognitive Composite (PACC; Mormino et al., 2017) mean days since administration = 284.3 ± 146.72. Of the 141, three participants had previously (mean days ago = 432.46 ± 162.23) received a diagnosis of MCI by a consensus meeting (see Procedures).
To gain more insight into the sample characteristic of the participants of the survey we compared the demographic characteristics presented in Table 1 to the individuals that were invited but did not respond to the survey as well as the overall cohort (see Supplemental Table 1). As compared to the whole cohort, we found that there was no significant difference in gender, APOE4 carriers, depression scores, ethnicity and socioeconomic status. However, the participants who responded to this survey were younger, had more education, and comprised of more white people. They also demonstrated better cognitive performance, including higher MMSE, CDR and global cognition score as compared to the overall cohort. As compared to the participants who were invited but did not respond to this survey, we found that there was no significant difference in gender, ethnicity, socioeconomic status and APOE4 carriers. The participants who responded to this survey were younger, and had more education, lower depression score, and comprised of more white people. They also demonstrated better cognitive performance, including higher MMSE, CDR, and global cognition score as compared to the participants who were invited but did not respond to the survey.
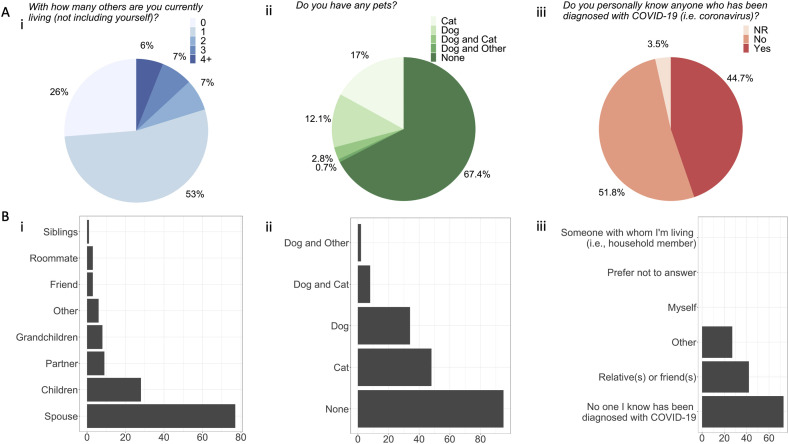
3.1. COVID-19 questions
Twenty-six percent of participants indicated that they lived alone, and among the remaining participants, 53% reported that they lived with 1 other person, 7% with 2 other people, 7% with 3 other people and 6% lived with 4 or more (Fig. 2 Ai). Among those living with others, the majority (78%) of participants were living with their spouse/partner, 25.5% with their children and 7.3% lived with grandchildren in the same household (Fig. 2Bi). The majority of participants (67.4%) did not own a pet (Fig. 2Aii). Among pet-owners, the majority indicated that they had a cat in their household (Fig. 2Bii). Forty-four percent of participants reported that an acquaintance had been diagnosed with COVID-19 (Fig. 2Aiii) of which 61% was a relative or friend and 39% other (Fig. 2Biii). None of the participants reported having been diagnosed with COVID-19.
Fig. 2.
Distribution of responses for living situations during COVID-19. The figures demonstrate the Ai) pie chart of percentage of how many people (none to 4+) the participants were living with (not including themselves) and Bi) description of those people (participants were instructed to select all responses that apply). Axis represents number of responses; Aii) the percentage of participants with and without pets and Bii) description of those pets (participants were instructed to select all responses that apply). Axis represents number of responses; Aiii) percentage of people that knew anyone who had been diagnosed with COVID-19 (NR = no response given) and Biii) description of those people (participants were instructed to select all responses that apply). Axis represents number of responses.
3.2. Levels of perceived stress
The mean perceived stress score as assessed with the PSS-14 questionnaire was 23.5 ± 5.2 (SD), corresponding to moderate levels of stress. The values were normally distributed ranging from 12 to 35. Stress was inversely related to age (r = −0.29, p = 0.001). Women reported significantly more stress than men (t = 2.05, df = 135, p = 0.042). No relationship was found between stress and education (r = −0.01, p = 0.89).
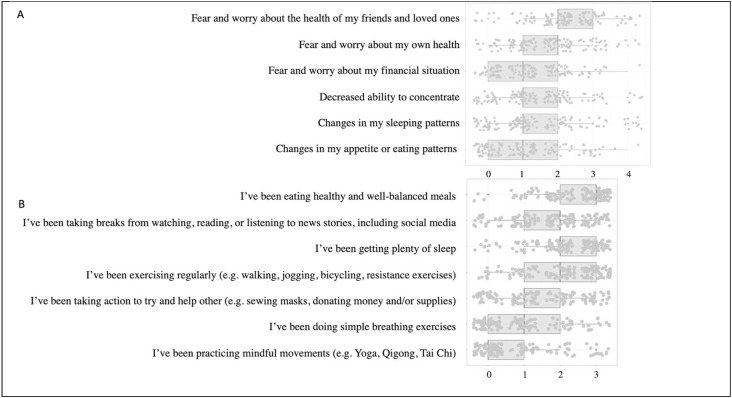
The mean score for the six additional COVID-19 questions were 12.24 ± 5.58 (range 0–26). Participants felt most stressed about the health of friends and loved ones and less so about their own health (Fig. 3 A). Similar to the PSS-14, the COVID-19 scores were inversely related to age (r = −0.18, p = 0.03) but were not correlated with gender (t = 0.56, df = 139, p = 0.58) or education (r = 0.13, p = 0.12). The PSS -14 and the additional COVID-19 total scores were significantly correlated with each other (r = 0.63, p < 0.001).
Fig. 3.
CDC COVID-19 specific stressors (A) and coping strategies (B). A. Boxplot for each of the six CDC COVID-19 stress questions showing the median (vertical line in the center of each box), and quartiles (25 respectively 75 indicated by the box), range of observations (horizontal lines) as well as each individual observation (dots). Responses are labeled as 0 = Never; 1 = Almost never; 2 = Sometimes; 3 = Fairly often; 4 = Very often. B. Boxplot for each of the seven CDC recommended COVID-19 coping strategy questions showing the median (vertical line in the center of each box), and quartiles (25 respectively 75 indicated by the box), range of observations (horizontal lines) as well as each individual observation (dots). Responses are labeled as 0 = I haven't been doing this at all; 1 = I've been doing this a little bit; 2 = I've been doing this a medium amount; 3 = I've been doing this a lot.
3.3. Level of resilience
The mean total score for resilience on the CD-RISC-10 questionnaire was 29.5 ± 5.9 corresponding to high levels of resilience. Scores were normally distributed ranging from 7 to 40. Level of resilience was not associated with age (r = 0.11, p = 0.23), education (r = 0.07, p = 0.43) or gender (t = −1.41, df = 133, p = 0.16).
3.4. Coping strategies
Mean and SD for the (14) coping strategies from the Brief COPE are presented in Fig. 4 . The three most endorsed coping strategies were acceptance (mean and S.D = 2.5 ± 0.8), positive reframing (mean and S.D = 1.84 ± 1.06) and active coping (mean and S.D = 1.7 ± 1.0), and the three least endorsed coping strategies were behavioral disengagement (mean and S.D = 0.2 ± 0.5), substance use (mean and S.D = 0.3 ± 0.7) and self-blame (mean and S.D = 0.5 ± 0.7). The mean score of the (7) CDC specific COVID-19 coping questions was 1.7 ± 1.0 ranging from 0 to 3, indicating that the participants had been using these strategies ‘a little’ to ‘a medium amount’. The highest endorsed coping strategy was I've been eating healthy and well-balanced meals (mean and S.D = 2.4 ± 0.8) and the least endorsed coping strategy was I've been practicing mindful movements (e.g., Yoga, Qigong and Tai Chi (mean and S.D = 0.7 ± 1.0; Fig. 3B).
Fig. 4.
Bivariate correlations between stress, resilience and coping strategies. The numbers and circles in the correlation matrix demonstrates significant r-values. The color coded scale depicts the strength of the correlation with a darker color representing higher significance. Blue represents positive relationships and red are negative relationships. The bottom rows in the figure shows the mean and standard deviation for each variable.
3.5. Bivariate correlations between stress, resilience and coping strategies
Bivariate correlations for all measured variables are presented in Fig. 4. Higher resilience was strongly related to lower stress. Higher resilience was also significantly related to less frequent use of behavioral disengagement, self-blame and substance use as coping strategies. By contrast, higher resilience was significantly related to more frequent use of acceptance, humor, and active coping. Higher stress was related to more frequent use of behavioral disengagement, self-blame, substance use, venting, instrumental support and self-distraction. There was no significant correlation between stress and other main coping strategies.
We performed similar analyses for the CDC-recommended COVID-19 coping strategies. Bivariate correlations for stress, resilience and the (7) CDC-recommended coping strategies are presented in Supplemental Figure 2. Higher resilience was significantly related to more frequent use of two COVID-19 coping strategies; I've been exercising regularly (e.g., walking, jogging, bicycling, resistance exercises) and I've been taking action to try to help others (e.g., sewing masks, donating money and/or supplies. Level of stress was not significantly related to any of the COVID-19 coping strategies.
3.6. Investigating the interaction between resilience and coping in predicting stress
Hierarchical multiple regression analyses were conducted for stress. The (14) coping strategies and the potential moderator, resilience, were entered at Step 1, and the interaction terms between resilience and each separate coping strategy were entered at Step 2. Tests conducted to evaluate whether the assumption of collinearity had been made demonstrated that multicollinearity was not a concern. We found that resilience and coping strategies accounted for 52% of the variance in stress (Table 2 ). Much of this variance was due to the independent main effect of resilience.
Table 2.
Hierarchical Multiple regression analysis results of main (step 1) and interaction effects (step 2).
| Step 1 – Main Effects | |||
|---|---|---|---|
| Variables | ß | R2 | |
| 0.52*** | |||
| Resilience | −0.39*** | ||
| Acceptance | 0.14 | ||
| Active Coping | −0.18 | ||
| Behavioral Disengagement | −0.84 | ||
| Denial | 0.69 | ||
| Emotional Support | −1.11* | ||
| Humor | −0.22 | ||
| Instrumental Support | 1.59*** | ||
| Planning | 0.25 | ||
| Positive Reframing | −0.71 | ||
| Religion | 0.21 | ||
| Self-Blame | 1.92*** | ||
| Self-Distraction | 1.32*** | ||
| Substance Use | 1.08* | ||
| Venting |
0.64 |
||
| Step 2 – Interactions Between Resilience and Coping Strategies | |||
| Variables |
ß |
R2 |
|
| 0.61*** | 0.089 | ||
| Resilience x Acceptance | 0.06 | ||
| Resilience x Active Coping | −0.04 | ||
| Resilience x Behavioral Disengagement | −0.29 | ||
| Resilience x Denial | 0.06 | ||
| Resilience x Emotional Support | −0.17 | ||
| Resilience x Humor | −0.08 | ||
| Resilience x Instrumental Support | 0.06 | ||
| Resilience x Planning | −0.18* | ||
| Resilience x Positive Reframing | 0.09 | ||
| Resilience x Religion | 0.02 | ||
| Resilience x Self-Blame | 0.25* | ||
| Resilience x Self-Distraction | 0.12 | ||
| Resilience x Substance Use | 0.10 | ||
| Resilience x Venting | −0.10 | ||
Note. Beta values represent standardized values at final model. *p < 0.05, ***p < 0.001.
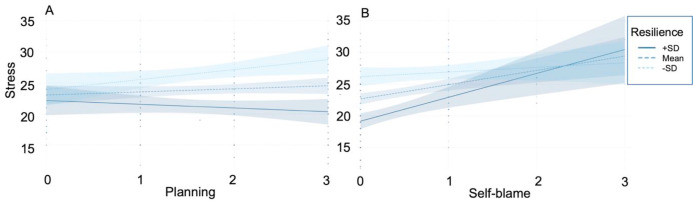
However, independent main effects remained significant for emotional and instrumental support, self-blame and self-distraction. The model at Step 2 including the interaction between resilience and each coping strategy was statistically significant, F(29, 111) = 5.97, p < 0.001. Moreover, the interaction terms between resilience and coping strategies explained a significant proportion of the variance in stress, , (14, 111) = 1.79, p = 0.047. Specifically, a significant interaction effect was found between resilience and planning, ß = −1.24, t(111) = -1.98, p = 0.049, Fig. 5 A. Simple slope analysis demonstrated that at high levels of resilience (+1SD) the relationship between planning and stress was non-significant (ß = −0.61, p = 0.35). At low levels of resilience (-1SD) the relationship between planning and stress was positive and significant (ß = 1.60, p = 0.03), indicating that more planning was less beneficial and somewhat deleterious for people with low resilience.
Fig. 5.
The relationship between stress and planning (A) or self-blame (B) at low (-1SD), mean, and high (+1SD) levels of resilience. Responses are labeled as 0 = I haven't been doing this at all; 1 = I've been doing this a little bit; 2 = I've been doing this a medium amount; 3 = I've been doing this a lot.
In addition, we found a significant interaction effect between resilience and self-blame, ß = 0.93, t(111) = 2.41, p = 0.018, Fig. 5B. Simple slope analysis demonstrated that at low levels of resilience (-1SD) the relationship between self-blame and stress was non-significant (ß = 0.73, p = 0.31). At high levels of resilience (+1SD) the relationship between self-blame and stress was positive and significant (ß = 3.77, p < 0.001). However, high resilient people only endorsed 0 (I haven't been doing this at all) and 1 (I've been doing this a little bit).
We reran the hierarchical models using the (7) COVID-19 coping strategies and resilience as a moderator. Similar to our previous model, no collinearity was found in this analysis. In Step 1, the main effects of resilience and the (7) COVID-19 coping strategies accounted for 31% of the variance. Much of this variance was due to the independent main effect of resilience. In fact, no other main effect was significant in the model (see Supplemental Table 2). Although the model at Step 2 including the product term predicting stress was statistically significant, F(15,125) = 4.15, p < 0.001, the interaction terms between resilience and coping strategies did not account for a significant proportion of variance in stress , = 0.55, p = 0.79).
4. Discussion
This study examined perceived levels of stress, resilience, and coping strategies among older adults living in Massachusetts and neighboring states (U.S.) during the COVID-19 pandemic. Participants reported moderate levels of stress on average, in line with other studies examining stress related to COVID-19 (Daly and Robinson, 2021; Umucu and Lee 2020). We found that participants reported feeling most stressed about the health of friends and loved ones, more so than about their own health. None of the participants themselves had been diagnosed with COVID-19 at the time of the survey, although nearly half of the sample indicated that one or more acquaintances (61% relative/s or friend/s and 39% other) had been diagnosed with COVID-19. Both stress questionnaires (PSS-14 and our CDC COVID-19 stress questions) were related to age, such that with increased age, individuals perceived less stress. In addition, women overall perceived more stress than men, although this was only true for the PSS-14 stress scale and not for the CDC COVID-19 stress questions. These findings are in line with a previous study reporting increased stress in women as compared to men during the COVID-19 outbreak in China (Hou et al., 2020). A significant association was found between the stress questions formulated based on the CDC information and the perceived stress scale indicating that the concepts measured are related to each other and both provide a good estimate of perceived stress in the individual during the pandemic.
The mean level of resilience was high in the participants, Our findings of high resilience in this sample are in line with previous studies reporting high resilience in the range of 14%–35% in older adults (see review by MacLeod et al. (2016)). For example, previous studies have found that adults age 85 and older demonstrate the same or even greater capacity for resilience as compared to those who are younger (Hamarat et al., 2002; Netuveli et al., 2008). Furthermore, we did not find any difference in resilience between men and women. Previous studies have found that while gender is not always associated with resilience, some studies have found that women appear to demonstrate more resilience than men; and older women more so than younger women (Netuveli et al., 2008; Hahn et al., 2011). Finally, we did not find a relationship between resilience and education, which may suggest that an individual has the capacity to build and demonstrate resilience, regardless of their socioeconomic backgrounds, personal experiences, or social environments. However, these results should be interpreted with caution as the mean years of education was high (mean years 16.8 ± 2.6) in our sample.
With regard to coping strategies, we found that acceptance was the most endorsed behavior in our sample. This finding is in line with a recent study by Umucu and Lee (2020) who found that acceptance during COVID-19 was the highest endorsed coping strategy in people with self-reported chronic conditions and disabilities. In the literature, acceptance has also been associated with better quality of life (Elfström et al., 2005). The three most highly endorsed, CDC recommended, coping strategies where I've been eating healthy and well-balanced meals, I've been getting plenty of sleep, and I've been exercising regularly (e.g., walking, jogging, bicycling, resistance exercises), indicating that in general the study participants have been engaged in healthy living habits during the pandemic. Not surprisingly, and in direct contrast to acceptance, we found that behavioral disengagement, was the least endorsed coping strategy in the participants. In addition, and in contrast to our findings that older adults seem to have engaged in healthy eating and exercising habits, we found that the second least used coping strategy was substance use, indicating that older adults were not very likely to use substances to cope with COVID-19. This results is, again, in line with the findings from Umucu and Lee (2020) who found that substance use was one of the least commonly used coping strategies during COVID-19 in people with self-reported chronic conditions and disabilities. However, other studies have reported an increased substance use during COVID-19 (https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm).
Resilience was negatively associated with coping strategies involving behavioral disengagement, self-blame and substance use, and positively associated with acceptance, humor, and active coping. Resilience was also significantly positively related to two CDC recommended COVID-19 coping strategies; I've been exercising regularly (e.g., walking, jogging, bicycling, resistance exercises) and I've been taking action to try to help others (e.g., sewing masks, donating money and/or supplies), such that higher resilience was related to more of these behaviors. The finding that exercising was related to higher resilience is in line with previous studies demonstrating that being physically active (Childs and de Wit 2014) and maintaining better physical health was associated with higher resilience (Gill et al., 1997; Resnick and Inguito 2011; Stewart-Knox et al., 2012; Smith and Hollinger-Smith 2015).
According to Meyer (2001) the coping strategies in the Brief COPE can be categorized into adaptive strategies including active coping, planning, use of emotional support, use of instrumental support, positive reframing, religion, humor, and acceptance and maladaptive strategies including venting, denial, substance use, self-blame, behavioral disengagement, and self-distraction). In regard to this, the matching hypothesis states that increased resilience may promote the use of proactive coping strategies (same as the adaptive strategies proposed by Meyer (2001) and reduce the use of reactive coping strategies (same as the maladaptive strategies proposed by Meyer (2001)). Thus, our findings are in line with the matching hypothesis by demonstrating that high resilience is related to increased use of adaptive (acceptance, humor, and active coping) and decreased use of maladaptive (behavioral disengagement, self-blame and substance use) coping strategies.
In turn, we found that stress was positively related to maladaptive/reactive coping strategies including behavioral disengagement, self-blame, substance use, venting, and self-distraction, such that more of these behaviors were associated with increased perceived stress. These findings are in line with past research (see meta-analysis in Penley et al. (2002)). Surprisingly, we also found that increased instrumental support was related to increased stress. Although speculative, one possible explanation for this finding could be that in the beginning of the pandemic, there was a diverse array of instructions on how to best respond to the pandemic. Thus, people might have felt increased stressed if they received conflicting advice from people around them. We did not find any negative relationships between stress and the different coping strategies.
More importantly, we found that resilience largely accounted for these coping outcome associations as it emerged as the strongest unique predictor for stress in the hierarchical regression models. This may be an important finding as it suggests that resilience may buffer against the negative effects of stress during the COVID-19 pandemic. Although encouraging, it will be important to determine whether high resilience in older adults has the capacity to buffer against long-term exposure of stressors during the pandemic, and especially whether resilience can reduce the onset of stress-related disorders and its maladaptive processes on health in older adults. For example, previous studies have found that individuals demonstrating high resilience later in life required less time to recover and terminated the stress response more quickly after experiencing stressor exposure, thereby reducing the damaging effects of chronic elevations of stress hormone glucocorticoids (Sampedro-Piquero et al., 2018). In addition, Arenaza-Urquijo et al. (2020) recently showed that higher stress coping ability was associated with lower tau burden (one of the hallmark pathologies in Alzheimer's disease) in the medial temporal lobe, and that this effect was strongest in individuals with preclinical Alzheimer's disease (i.e. individuals with increased amyloid pathology), suggesting that higher resilience may limit the effects of stress on tau.
Finally, we investigated whether resilience could moderate the efficacy of coping strategies. In accordance with the goodness-of-fit hypothesis, high resilience should amplify the positive effects and dampen the negative effects of coping. In support of this hypothesis, we found that planning, an adaptive/task-oriented coping strategy, was significantly associated with increased stress for individuals with low levels of resilience, whereas this relationship was non-significant for individuals with high levels of resilience. In accordance with the goodness-of-fit hypothesis, adaptive or task-oriented coping would be more beneficial for people with high resilience, but less beneficial for people with low resilience, indicating that this form of coping behavior might be less efficacious during the pandemic for people with low resilience. Although not possible to examine with the current dataset, one explanation for this finding could be that even though individuals with low resilience used planning as a coping behavior, they may have felt overwhelmed resulting in higher perceived stress levels.
Furthermore, we found that resilience interacted with self-blame, a maladaptive/reactive coping strategy, such that high resilience attenuated the effect of self-blame on perceived stress levels. Again, this indicates that, in line with the goodness-of-fit hypothesis, high resilience seems to dampen the effect of stress on behaviors that are maladaptive. However, we do acknowledge that since the high resilient people did not endorse this behavior overall, i.e., indicating that they had not been doing this at all or only been doing this a little bit, the current data is not able to show us what the effect of stress would have been if high-resilient people had indeed been using this behavior more frequently during the pandemic. Overall, our findings indicate that high resilience may act as a moderator, by enhancing the effectiveness of adaptive/reactive coping and act as a buffer against maladaptive coping behaviors on individuals’ stress levels.
Finally, the hierarchical linear regressions investigating possible interactions between resilience and the CDC recommended COVID-19 coping strategies did not reveal any significant interaction terms between resilience and coping strategies that could account for a significant proportion of variance in stress. In fact, we found that much of the variance was explained by the independent main effect of resilience, possibly suggesting that these coping behaviors are not as effective in lowering the perceived level of stress in older adults.
The main limitation of the present study is that the design of the study was cross-sectional and did not include an intervention, hence not allowing us to assess causality, directionality, and duration of coping effects. In addition, we believe that our results should also be considered in light of the time window of the survey (May 07, 2020 until May 26, 2020). In Massachusetts the number of individuals diagnosed COVID-19 started to rise around mid-March with the highest number of cases and reported deaths of COVID-19 reported in mid-April. Because the levels of appraised stress are influenced by major events and changing coping strategies some of the initial stress response in the participants might have been lower compared to if the survey had been sent out earlier. In line with this, a recent observational population based study in the USA conducted by Daly and Robinson, (2021) who collected data on psychological distress between March 10th and July 20th, 2020 found that distress increased significantly by 0.27 standard deviations (95% CI [0.23,0.31], p < 0.001) from March 10–18 to April 1–14, 2020 as the COVID-19 crisis emerged and lockdown restrictions began in the US. However, they found that distress levels subsequently declined to mid-March levels by June 2020 (d = −0.31, 95% CI [–0.34, −0.27], p < 0.001) (Daly and Robinson, 2021). Although the time window for our survey was limited, the day of response did not predict the level of stress in our participants (data not shown). That is, stress did not decrease the further away from the peak that an individual responded. Nonetheless, a follow-up survey would be interesting to conduct in order to evaluate whether our participants are reporting the same levels of stress now as at the time of the survey. Another limitation is that we may have a biased sample of individuals that responded to our survey. The survey was sent out to participants in our ongoing longitudinal cohorts who have provided us with an email address (see supplemental Figure 1). We acknowledge that specific groups in the population may be under-represented as they may not have an email address and/or have limited or no access to internet (Bethlehem 2010). For instance, Bethlehem (2010) have reported that individuals with a higher level of education more frequently have internet than people with a lower level of education. Comparing the individuals who completed the survey versus the individuals who did not respond to the survey as well as the overall cohort are in line with these findings as the individuals who responded to the survey were significantly more educated than the individuals who did not respond as well as the whole sample. Furthermore, we acknowledge that the recruitment of respondents may be based on self-selection (Bethlehem 2010). That is, we sent out the survey to 269 individuals of which 54% responded. Although there might be multiple reasons for people not responding, one possible reason could be that nonrespondents did not have the bandwidth to respond because they were less resilient and were experiencing more stress. This limitation is difficult to assess fully. However, based on the comparison between the individuals that completed the survey versus the people who were invited but did not respond to the survey, we found that there was no significant difference in gender, ethnicity, socioeconomic status and APOE4 carriers. However, the participants that responded to this survey were slightly younger and less depressed (as measured pre pandemic). Perhaps more importantly, we also found that survey respondents seemed to be significantly more cognitively intact (as indicated by increased MMSE, CDR and global cognition score) as compared to survey nonrespondents as well as the overall cohort. This data further supports our statement above that the individuals that did not respond to this survey may have less resilience, feel more stressed, and reduced bandwidth to respond to the survey. In addition, we also acknowledge that the interpretation of our results are limited to the fact that our sample comprised of mostly white people, especially given that minority groups have been demonstrated to have been most impacted by the pandemic (Lee and Miller 2020, Babulal et al., 2021). Last, there are numerous tools that have been developed to measure resilience, but no true gold standard has been determined. This should be considered when comparing our findings to similar studies conducted during the pandemic in other cohorts. Again, even though our time window for the survey was limited, we did not find a relationship between the day of survey response and individual resilience (data not shown). A follow-up study would be necessary to determine whether an individual's level of resilience may change as people try to adapt to this global crisis.
5. Conclusion
Our findings suggest that resilience is critical for coping with stress during the COVID-19 pandemic and adds to the current discussion about the urgent need to augment resilience and develop strategies to enhance it (Chen 2020; Vinkers et al., 2020).
Funding and/or competing interests statement
Patrizia Vannini, funding: NIH-NIA R01 AG061083 and R21 AG064348. No competing interests.
Geoffroy Gagliardi no competing interests. Madeline Kuppe no competing interests.
Michelle Dossett, funding: K23AT009218; Competing interests: received money from UpToDate (within the last year) and Harvard Health Publishing (within the last 2 years).
Nancy Donovan, None.
Gad Marshall, funding: R01 AG053184; competing interests: GAM has received research salary support from Eisai Inc., Eli Lilly and Company, Janssen Alzheimer Immunotherapy, Novartis, and Genentech, and consulting fees from Grifols Shared Services North America, Inc., Eisai Inc., and Pfizer.
Jennifer R Gatchel K23 AG058805; Alzheimer’s Association Clinical Fellowship (AACF-16-440965). No competing interests.
Pranitha Y Premnath no competing interests.
Rebecca Amariglio.
Yakeel Quiroz was supported by grants from the NIH NIA (R01 AG054671) and Massachusetts General Hospital ECOR.
Risa Sperling: NIH/ NIA P01AG036694. competing interests: reports grants from Eli Lilly, NIA, Alzheimer’s Association, Janssen, Eisai, personal fees from Shionogi, Genentech, Oligomerix, Cytox, Prothena, Acumen, JOMDD, Renew, Alnylam Pharmaceuticals, Neuraly, Janssen, Neurocentria, AC Immune, Biogen and Eisai.
CRediT authorship contribution statement
Patrizia Vannini: Supervision, Formal analysis, Data curation, Writing – original draft. Geoffroy P. Gagliardi: Formal analysis, Writing – original draft. Madeline Kuppe: Data curation, Writing – original draft, involved in collection and quality checking of data, design of the study, reading the ms. Michelle L. Dossett: Writing – original draft, coming up with the idea, design of the study, reading the ms. Nancy J. Donovan: Writing – original draft, design of the study, reading the ms. Jennifer R. Gatchel: Writing – original draft, design of the study, reading the ms. Yakeel T. Quiroz: Writing – original draft, design of the study, reading the ms. Pranitha Y. Premnath: Writing – original draft, reading the ms. Rebecca Amariglio: Writing – original draft, design of the study, reading the ms. Reisa A. Sperling: Writing – original draft, design of the study, reading the ms. Gad A. Marshall: design of the study, reading the ms.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.03.050.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplemental Figure 1. Flowchart demonstrating how individuals were selected to take part in the online survey. The number of participants in HABS (N = 253) and IADL (N = 36) represents the total number of participants that were actively enrolled in these studies at the time of the survey. Of these, an invitation to participate in the study was sent to HABS (N = 233) and IADL (N = 36) participants with a listed email address and /or that had not previously opted out of consideration for sub-studies (only HABS). Of these, 141 individuals consented and responded to the survey within the time window (HABS N = 109 and IADL N = 32).
Supplemental Figure 2. Bivariate correlations between stress, resilience and coping strategies recommended by the CDC. Note that the legends on the top have been replaced by numbers. The numbers and circles in the correlation matrix demonstrate significant r-values. The color coded scale depicts the strength of the correlation with a darker color representing higher significance. Blue represents positive relationships and red are negative relationships.
References
- Aiken L.S., et al. Sage; 1991. Multiple Regression: Testing and Interpreting Interactions. [Google Scholar]
- Arenaza-Urquijo E.M., et al. Better stress coping associated with lower tau in amyloid-positive cognitively unimpaired older adults. Neurology. 2020;94:1571–1579. doi: 10.1212/WNL.0000000000008979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association T.A.P. 2015. The Road to Resilience. [Google Scholar]
- Babulal G.M., Torres V.L., Acosta D., Agüero C., Aguilar-Navarro S., Amariglio R., Ussui J.A., Baena A., Bocanegra Y., Dozzi Brucki S.M., Bustin J., Cabrera D.M., Custodio N., Diaz M.M., Duque Peñailillo L., Franco I., Gatchel J.R., Garza-Naveda A.P., González Lara M., Gutiérrez-Gutiérrez L., Guzmán-Vélez E., Hanseeuw B.J., Jimenez-Velazquez I.Z., Rodríguez T.L., Llibre-Guerra J., Marquine M.J., Martinez J., Medina L.D., Miranda-Castillo C., Morlett Paredes A., Munera D., Nuñez-Herrera A., Okada de Oliveira M., Palmer-Cancel S.J., Pardilla-Delgado E., Perales-Puchalt J., Pluim C., Ramirez-Gomez L., Rentz D.M., Rivera-Fernández C., Rosselli M., Serrano C.M., Jose Suing-Ortega M., Slachevsky A., Soto-Añari M., Sperling R.A., Torrente F., Thumala D., Vannini P., Vila-Castelar C., Yañez-Escalante T., Quiroz Y.T. The Impact of COVID-19 on the well-being and cognition of older adults living in the United States and Latin America. EClin. Med. 2021 doi: 10.1016/j.eclinm.2021.100848. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethlehem J. Selection bias in web surveys. Int. Stat. Rev. 2010;78:161–188. [Google Scholar]
- Carver C.S. You want to measure coping but your protocol’ too long: consider the brief cope. Int. J. Behav. Med. 1997;4(1):92. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chen L.-K. Older adults and COVID-19 pandemic: resilience matters. Arch. Gerontol. Geriatr. 2020;89:104124. doi: 10.1016/j.archger.2020.104124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs E., de Wit H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front. Psychol. 2014;5:161. doi: 10.3389/fphys.2014.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., et al. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: the Connor- Davidson resilience scale (CD-RISC) Depress. Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfström M., et al. Relations between coping strategies and health-related quality of life in patients with spinal cord lesion. J. Rehabil. Med. 2005;37:9–16. doi: 10.1080/16501970410034414. [DOI] [PubMed] [Google Scholar]
- Endler N., Parker J. Assessment of multidimensional coping: task, emotion, and avoidance strategies. Psychol. Assess. 1994;6:50–60. [Google Scholar]
- Feder A., et al. The biology of human resilience: opportunities for enhancing resilience across the life span. Biol. Psychiatr. 2019;86:443–453. doi: 10.1016/j.biopsych.2019.07.012. [DOI] [PubMed] [Google Scholar]
- Folstein M.F., et al. Mini-Mental State": a practical method for grading cognit9ive state of patients for the clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gill T.M., et al. Predictors of recovery in activities of daily living among disabled older persons living in the community. J. Gen. Intern. Med. 1997;12:757–762. doi: 10.1046/j.1525-1497.1997.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J.E., et al. Stress, age, and immune function: toward a lifespan approach. J. Behav. Med. 2006;29:389–400. doi: 10.1007/s10865-006-9057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn E.A., et al. Time use and well-being in older widows: adaptation and resilience. J. Women Aging. 2011;23:149–159. doi: 10.1080/08952841.2011.561139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamarat E., et al. Age differences in coping resources and satisfaction with life among middle-aged, young- old, and oldest-old adults. J. Genet. Psychol. 2002;163:360–367. doi: 10.1080/00221320209598689. [DOI] [PubMed] [Google Scholar]
- Harris P.A., et al. 2019. The REDCap Consortium: Building an International Community of Software Partners. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead A.B. Yale University; New Haven, CT: 1957. Two Factor Index of Social Position. [Google Scholar]
- Holmes E.A., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou F., et al. Gender differences of depression andanxiety among social media users duringthe COVID-19 outbreak in China:a cross-sectional study. BMC Publ. Health. 2020;20 doi: 10.1186/s12889-020-09738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R., Folkman S. Springer; New York, NY: 1984. Stress, Appraisal, and Coping. [Google Scholar]
- Lee H., Miller V. The disproportionate impact of COVID-19 on minority groups: a social justice concern. J. Gerontol. Soc. Work. 2020;63:580–584. doi: 10.1080/01634372.2020.1777241. [DOI] [PubMed] [Google Scholar]
- MacLeod S., et al. The impact of resilience among older adults. Geriatr. Nurs. 2016;37:266–272. doi: 10.1016/j.gerinurse.2016.02.014. [DOI] [PubMed] [Google Scholar]
- Meyer B.C. Oping with severe mental illness: relations of the Brief COPE with symptoms, functioning, and well-being. J. Psychopathol. Behav. Assess. 2001;23:265–277. [Google Scholar]
- Mormino E.C., et al. Early and late change on the preclinical Alzheimer's cognitive composite in clinically normal older individuals with elevated β-amyloid. Alzheimers Dement. 2017;13:1004–1012. doi: 10.1016/j.jalz.2017.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J.C. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- Netuveli G., et al. Mental health and resilience at older ages: bouncing back after adversity in the British Household Panel Survey. J. Epidemiol. Community Health. 2008;62:987–991. doi: 10.1136/jech.2007.069138. [DOI] [PubMed] [Google Scholar]
- Papp K.V., et al. Clinical meaningfulness of subtle cognitive decline on longitudinal testing in preclinical AD. Alzheimer's Dementia: J. Alzhemeir's Assoc. 2019;16:552–560. doi: 10.1016/j.jalz.2019.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papp K.V., et al. Optimizing the preclinical Alzheimer's cognitive composite with semantic processing: the PACC5. Alzheimer's Dementia: Transl. Res. Clin. Interven. 2017;4:668–677. doi: 10.1016/j.trci.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker J., Endler N. Coping with coping assessment: a critical review. Eur. J. Pers. 1992;6:321–344. [Google Scholar]
- Pearlin L.I., Schooler C. The structure of coping. J. Health Soc. Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- Penley J., et al. The association of coping to physical and psychological health outcomes: a meta-analytic review. J. Behav. Med. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- Resnick B.A., Inguito P.L. The resilience scale: psychometric properties and clinical applicability in older adults. Arch. Psychiatr. Nurs. 2011;25:11–20. doi: 10.1016/j.apnu.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Sampedro-Piquero P., et al. Coping with stress during aging: the importance of a resilient brain. Curr. Neuropharmacol. 2018;16:284–296. doi: 10.2174/1570159X15666170915141610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.L., Hollinger-Smith L. Savoring, resilience, and psychological well-being in older adults. Aging Ment. Health. 2015;19:192–200. doi: 10.1080/13607863.2014.986647. [DOI] [PubMed] [Google Scholar]
- Smith M.M., et al. Coping strategies and psychological outcomes: the moderating effects of personal resiliency. J. Psychol. 2016;150:318–332. doi: 10.1080/00223980.2015.1036828. [DOI] [PubMed] [Google Scholar]
- Stewart-Knox B., et al. Associations between obesity (BMI and waist circumference) and sociodemographic factors, physical activity, dietary habits, life events, resilience, mood, perceived stress and hopelessness in healthy older Europeans. BMC Publ. Health. 2012;12:424. doi: 10.1186/1471-2458-12-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umucu E., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020;65:193–198. doi: 10.1037/rep0000328. [DOI] [PubMed] [Google Scholar]
- Vinkers C.H., et al. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020;35:12–16. doi: 10.1016/j.euroneuro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Psychological Corp; San Antonio: 1981. Wechsler Memory Scale - Revised Manual. [Google Scholar]
- Yesavage J.A., et al. Development and validation of a geriatric depression screening scale. Psychiatr. Res. 1983;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Zeidner M., et al. In: Handbook of Coping: Theory, Research, and Applications M. Zeidner. Endler N., editor. Wiley & Sons; Oxford: 1996. Adaptive and maladaptive coping; pp. 505–531. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Flowchart demonstrating how individuals were selected to take part in the online survey. The number of participants in HABS (N = 253) and IADL (N = 36) represents the total number of participants that were actively enrolled in these studies at the time of the survey. Of these, an invitation to participate in the study was sent to HABS (N = 233) and IADL (N = 36) participants with a listed email address and /or that had not previously opted out of consideration for sub-studies (only HABS). Of these, 141 individuals consented and responded to the survey within the time window (HABS N = 109 and IADL N = 32).
Supplemental Figure 2. Bivariate correlations between stress, resilience and coping strategies recommended by the CDC. Note that the legends on the top have been replaced by numbers. The numbers and circles in the correlation matrix demonstrate significant r-values. The color coded scale depicts the strength of the correlation with a darker color representing higher significance. Blue represents positive relationships and red are negative relationships.