Abstract
Background
Fibroids are present in approximately one in ten pregnancies and are inconsistently linked with preterm birth. We sought to determine the association between fibroids and preterm birth in a prospective cohort with standardized research ultrasounds for characterizing fibroids in early pregnancy while accounting for the clinical paths that precede preterm birth.
Methods
Participants who were pregnant or planning a pregnancy were recruited from communities in three states between 2000 and 2012. Members of this prospective cohort had a research ultrasound in the first trimester to establish pregnancy dating and to record detailed information about the presence, size, number, and location of fibroids. Baseline information from time of enrollment and a detailed first trimester interview contributed key information about candidate confounders. Birth outcomes, including clinical classification of type of preterm birth (preterm labor, preterm premature rupture of membranes, and medically indicated preterm birth) were cross-validated from participant report, labor and delivery records, and birth certificate data.
Results
Among 4,622 women with singleton pregnancies, 475 had at least one fibroid (10.3%) and 352 pregnancies resulted in preterm birth (7.6%). Prevalence of fibroids was similar for women with preterm and term births (10.2% vs. 10.3%). Fibroids were not associated with increased risk of preterm birth after taking into account confounding (risk ratio adjusted for race/ethnicity and maternal age, 0.88; 95% confidence interval, 0.62–1.24) nor any clinical subtype of preterm birth. No fibroid characteristic or combination of characteristics was associated with risk.
Conclusions
If fibroids increase risk of preterm birth, the effect is substantially smaller than previous estimates. Given lack of effect in a large population of women from the general population, rather than higher risk academic tertiary populations previously most studied, we encourage a reconsideration of the clinical impression that presence of fibroids is a major risk factor for preterm birth.
Keywords: Uterine Fibroids, Leiomyoma, Premature Birth, Preterm Labor, Preterm Premature Rupture of Membranes, Ultrasound
Background
Approximately 10% of women have a uterine fibroid detectable by ultrasound in the first trimester [1]. Fibroids are thought to increase preterm birth risk by 50% [2], yet effect estimates range from protective to more than tripling risk [3–18]. The estimated association between specific fibroid characteristics, such as size and number, and preterm birth vary to an even greater extent [4, 14, 19, 20]. Half of studies about fibroids and preterm birth do not account for maternal characteristics that may bias the association, such as maternal age and race, and almost all determine fibroid status via methods prone to misclassification: maternal self-report, insurance codes, medical records, or clinical ultrasounds not intended for fibroid characterization. Preterm birth is the leading cause of neonatal morbidity and mortality in developed countries [21, 22] and a more rigorous evaluation of the relationship between fibroid characteristics and preterm birth is warranted.
Preterm birth is commonly treated as a single outcome. However, multiple etiologic pathways contribute to preterm birth, including spontaneous onset of labor, preterm premature rupture of membranes, and medically indicated delivery for maternal or fetal complications [23, 24]. Each preterm birth subtype has a unique risk profile [25–28]. Studying the association between presence of fibroids and preterm birth subtypes may uncover more insightful risk-relationships [23, 29].
We sought to characterize the association between fibroids and preterm birth in a community-based cohort of women with standardized imaging for fibroid characterization during early pregnancy. We also evaluated the association by clinical subtype of preterm birth with the hypothesis that fibroid status would relate differently to risk of spontaneous versus medically indicated preterm birth.
Methods
Right from the Start is a prospective, community-based pregnancy cohort that recruited women who were pregnant or planning a pregnancy from three states (North Carolina, Tennessee, and Texas) between 2000 and 2012 [30]. Study recruitment materials were distributed through businesses, paid advertising, community groups, and direct mail. Private obstetric and public prenatal care providers also posted flyers and offered brochures about the study. If interested, women were directed to call a toll-free number to be screened for eligibility: aged 18 years and older, trying to become pregnant or pregnant for less than twelve weeks, fluent in English or Spanish, and not using assisted reproductive technologies to conceive. Women planning a pregnancy were provided free pregnancy tests for up to six months and were fully enrolled at first positive pregnancy test. Vanderbilt University’s Institutional Review Board approved study procedures and all participants gave informed consent. Data from this study has also provided evidence about the association between fibroids and first trimester bleeding [31], fibroids and miscarriage [32], fibroids and birthweight [33], and fibroids and C-section risk [34].
Participants completed a baseline interview upon enrollment and a detailed computer-assisted telephone interview in the first trimester. Interviews collected basic demographic information, maternal medical history, reproductive history, and health-related behaviors during early pregnancy.
Fibroid assessment
Participants had a transvaginal ultrasound for fetal viability assessment, gestational age confirmation, and fibroid characterization. Ultrasounds were performed at a median of 57 days’ gestation (interquartile range [IQR], 48–68 days). Study sonographers with at least five years of obstetric experience followed a detailed protocol for fibroid assessment, which required three sets of caliper measurements for each fibroid’s length, width, and height. Fibroid volume was calculated using the formula for an ellipsoid. Sonographers took multiple images with caliper markings of all fibroids and completed a fibroid map, which indicated fibroid location (cervix, corpus, fundus) and type. Fibroid type was classified as submucosal (distorting or in contact with the uterine cavity without myometrium between fibroid and endometrium), intramural (within the myometrium without distorting the uterine cavity), subserosal (distorting the external contour of the uterus), or pedunculated (located within the uterine cavity and attached by a stalk). Obstetrician investigators masked to pregnancy outcome assessed all images. Gestational age was based on self-reported last menstrual period (LMP) if within seven days of ultrasound predicted gestational age, otherwise ultrasound predicted gestational age was used. Maternal height and weight measured at ultrasound appointment were used to calculate body mass index (BMI).
Outcome definitions
Participants were followed until pregnancy outcome, which was self-reported and validated by medical and birth certificate records. We defined preterm birth as live birth at less than 37 weeks’ gestation. We categorized preterm birth into three distinct subtypes using hospital records or vital records. Spontaneous preterm labor was defined as onset of spontaneous preterm contractions leading to a preterm birth. Preterm premature rupture of membranes (PPROM) was defined as preterm birth following spontaneous rupture of membranes with subsequent onset of labor. We defined medically indicated preterm birth as labor induction or cesarean birth in the absence of preterm labor or PPROM for maternal or fetal conditions such as pre-eclampsia, fetal growth restriction, or fetal distress. We used the term spontaneous preterm birth to refer to births resulting from either preterm labor or PPROM.
In a secondary analysis, we evaluated preterm birth categories by gestational age. We defined late preterm birth as deliveries occurring for any indication between 34 weeks and 0 days and 36 weeks and 6 days, early preterm birth as deliveries occurring between 28 weeks and 0 days and 33 weeks and 6 days, and very early preterm birth as deliveries occurring prior to 28 weeks.
Inclusion and exclusion criteria
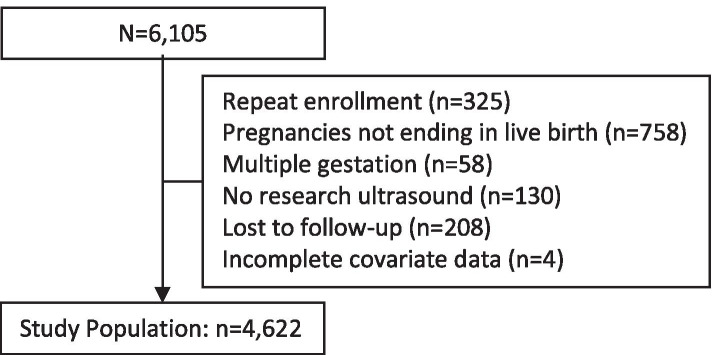
This analysis was limited to women with a singleton pregnancy resulting in a live birth after 20 weeks’ gestation (a prior analysis of this dataset demonstrated no association between fibroids and spontaneous abortion defined as loss prior to 20 weeks) [32]. If a woman was enrolled for more than one pregnancy, only the first study pregnancy was included in this analysis. We excluded pregnancies without a research ultrasound to confirm fibroid status, and those lacking information about maternal race/ethnicity. Three percent of participants were lost to follow-up (208/6,105). These participants were less likely to have fibroids (3.4% versus 10.3%, chi-squared p-value 0.001), were younger (median age 25 versus 29, Wilcoxon rank-sum p-value <0.001), and were more likely to be black (35.1% versus 17.4%, chi-squared p-value <0.001) compared with participants observed until pregnancy outcome. A total of 4,622 women were included (Fig. 1). All participants enrolled prior to twelve weeks' gestation (median gestational age at enrollment: 46 days’ gestation; IQR, 36-57 days).
Fig. 1.
Fibroids and preterm birth study population flow diagram
Statistical analysis
We used log-binomial generalized linear regression models to calculate crude and adjusted risk ratios (RRs) and 95% confidence intervals (CIs) associated with overall preterm birth risk for fibroid presence, fibroid number, total fibroid volume (quartiles), largest fibroid volume (quartiles), fibroid type, and location. We also quantified the association between fibroid presence and preterm birth subtypes: spontaneous preterm birth as preterm labor and PPROM and medically indicated preterm birth. We decided a priori to include maternal race/ethnicity (white, non-Hispanic; black, non-Hispanic; Hispanic, or other) and age (continuous) in all adjusted models. Other potential confounders (BMI, smoking status, parity, education, and household income) were retained in the final model if their inclusion resulted in a 10% change in the association between fibroids and preterm birth. We tested for effect modification of the relationship between fibroid status and preterm birth by maternal race/ethnicity using the likelihood ratio test. Stratified estimates were reported if the test suggested effect heterogeneity (p<0.15).
We did not consider history of preterm birth a confounder in the primary model since fibroid status in prior pregnancies could have impacted prior pregnancy outcome [35, 36]. Instead, we quantified associations with preterm birth and preterm birth subtypes adjusted for history of preterm birth (none, one, two or more) in a sensitivity analysis.
We performed a series of secondary analyses evaluating the association between fibroid presence, number, type, size, and location with late preterm, early preterm, and very early preterm birth using both chi-squared testing and log-binomial generalized linear regression models. We also evaluated the relationship between fibroids with different combinations of characteristics (e.g., multiple large fibroids) and risk of overall preterm birth. We performed all analyses in Stata (Version 14.2, StataCorp, College Station, TX).
Results
Among 4,622 women, 475 had at least one fibroid on research ultrasound (10.3%) and 352 had a pregnancy ending in preterm birth (7.6%). This population included mostly white or black, non-Hispanic women (71.5% and 17.4%, respectively) from a range of household income and education levels. Forty-eight percent of women were nulliparous and 8.2% reported a prior preterm birth. A notable proportion of women were overweight or obese at pregnancy onset (43.4%) and few smoked (3.5%). Women who were older than 35, black, or obese were more likely to have fibroids (Table 1). Average gestational age at birth for both women with and without fibroids was 39 weeks and 2 days (p=0.34, Wilcoxon rank-sum test). Among preterm births, 88% were late preterm (n=309), 29 were early preterm, and 14 were very early preterm.
Table 1.
Participant characteristics by fibroid status, Right from the Start, 2000–2012 (n = 4,622)
| Characteristic | Fibroids n = 475 |
No Fibroids n = 4,147 |
ORa | 95% CI | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Maternal Age (years) | ||||||
| <25 | 42 | 8.8 | 868 | 20.9 | 1.00 | Referent |
| 25–29 | 120 | 25.3 | 1,531 | 36.9 | 1.62 | 1.13–2.32 |
| 30–34 | 197 | 41.5 | 1,294 | 31.2 | 3.15 | 2.23–4.44 |
| ≥ 35 | 116 | 24.4 | 454 | 10.9 | 5.28 | 3.64–7.65 |
| Race | ||||||
| White, non-Hispanic | 268 | 56.4 | 3,038 | 73.3 | 1.00 | Referent |
| Black, non-Hispanic | 156 | 32.8 | 650 | 15.7 | 2.72 | 2.19–3.37 |
| Hispanic | 25 | 5.3 | 286 | 6.9 | 0.99 | 0.65–1.52 |
| Other | 26 | 5.5 | 173 | 4.2 | 1.70 | 1.11–2.62 |
| Parity | ||||||
| Nulliparous | 223 | 46.9 | 1,890 | 45.6 | 1.00 | Referent |
| 1 | 153 | 32.3 | 1,367 | 33.0 | 0.95 | 0.76–1.18 |
| 2 + | 87 | 18.3 | 669 | 16.1 | 1.10 | 0.85–1.43 |
| Missing | 12 | 2.5 | 221 | 5.3 | ||
| History of SAB | ||||||
| No | 323 | 68.0 | 3,097 | 74.7 | 1.00 | Referent |
| Yes | 140 | 29.5 | 829 | 20.0 | 1.62 | 1.31–2.00 |
| Missing | 12 | 2.5 | 221 | 5.3 | ||
| History of Preterm Birth | ||||||
| No | 419 | 88.2 | 3,608 | 87.0 | 1.00 | Referent |
| Yes | 44 | 9.3 | 318 | 7.7 | 1.19 | 0.85–1.66 |
| Missing | 12 | 2.5 | 221 | 5.3 | ||
| Marital Status | ||||||
| Married | 421 | 88.6 | 3,702 | 89.3 | 1.00 | Referent |
| Other | 54 | 11.4 | 445 | 10.7 | 1.07 | 0.79–1.44 |
| BMIb | ||||||
| Underweight | 11 | 2.3 | 106 | 2.6 | 1.18 | 0.62–2.23 |
| Normal weight | 200 | 42.1 | 2,266 | 54.6 | 1.00 | Referent |
| Overweight | 134 | 28.2 | 945 | 22.8 | 1.61 | 1.28–2.03 |
| Obese | 127 | 26.7 | 772 | 18.6 | 1.86 | 1.47–2.36 |
| Missing | 3 | 0.6 | 58 | 1.4 | ||
| Education | ||||||
| High school or less | 57 | 12.0 | 735 | 17.7 | 1.00 | Referent |
| Some college | 84 | 17.7 | 759 | 18.3 | 1.43 | 1.00–2.03 |
| College or more | 334 | 70.3 | 2,653 | 64.0 | 1.62 | 1.21–2.18 |
| Annual Income ($) | ||||||
| ≤ 40,000 | 112 | 23.6 | 1,184 | 28.6 | 1.00 | Referent |
| 40,001 to < 80,000 | 176 | 37.1 | 1,468 | 35.4 | 1.27 | 0.99–1.63 |
| ≥ 80,000 | 166 | 34.9 | 1,175 | 28.3 | 1.49 | 1.16–1.92 |
| Missing | 21 | 4.4 | 320 | 7.7 | ||
| Smoking Statusc | ||||||
| Never smoker | 350 | 73.7 | 2,891 | 69.7 | 1.00 | Referent |
| Current | 34 | 7.2 | 488 | 11.8 | 0.58 | 0.40–0.83 |
| Former | 83 | 17.5 | 576 | 13.9 | 1.19 | 0.92–1.54 |
| Missing | 8 | 1.7 | 192 | 4.6 | ||
Abbreviations: OR Odds ratio, CI Confidence interval, SAB Spontaneous abortion, BMI Body mass index
a Crude odds of exposure given maternal characteristic
b BMI categories from Institute of Medicine guidelines: Underweight < 18.5, Normal weight 18.5–24.99, Overweight 25–29.99, Obese ≥ 30
c Former smoker defined as smoking cessation one month or more before last menstrual period
Prevalence of fibroids in pregnancies ending in preterm and term birth was 10.2% and 10.3%, respectively. Among women with fibroids, 29.3% had more than one. Median total fibroid volume was 4.78 cm3 (IQR, 0.97-20.84 cm3) and the median volume of the largest fibroid was 4.64 cm3 (IQR, 0.83-18.23 cm3). Forty-four percent of women with fibroids had at least one intramural fibroid, compared to 42.3% with at least one subserosal and 14.5% with at least one submucosal fibroid. Twenty-one percent of women with fibroids had multiple fibroid types. Fibroid characteristics were similar when comparing women with preterm birth and those who delivered at term (Table 2). Fibroid presence was not associated with overall risk of preterm birth (adjusted RR, 0.88; 95% CI, 0.62–1.24). Neither maternal race nor age modified the association (p=0.56 and p=0.86, respectively). Fibroid number, volume, type, or location were not associated with preterm birth. We did not identify any combination of fibroid characteristics related to increased risk of preterm birth. When compared to women without fibroids, women with multiple intramural fibroids, intramural fibroids >3 cm in diameter, or multiple fibroids >3 cm in diameter were not at increased risk of preterm birth (analysis not shown).
Table 2.
Relationship between fibroid characteristics and preterm birth, Right from the Start, 2000–2012 (n = 4,622)
| Fibroid Characteristic | Preterm Births (n = 352) | Term Births (n = 4,270) | Crude RR | 95% CI | Adjusted RRa | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Fibroid Present | ||||||||
| No | 316 | 89.8 | 3,831 | 89.7 | 1.00 | Referent | 1.00 | Referent |
| Yes | 36 | 10.2 | 439 | 10.3 | 0.99 | 0.71–1.39 | 0.88 | 0.62–1.24 |
| Fibroids, no. | ||||||||
| 0 | 316 | 89.8 | 3,831 | 89.7 | 1.00 | Referent | 1.00 | Referent |
| 1 | 21 | 6.0 | 315 | 7.4 | 0.82 | 0.53–1.26 | 0.76 | 0.49–1.16 |
| ≥ 2 | 15 | 4.3 | 124 | 2.9 | 1.42 | 0.87–2.31 | 1.14 | 0.68–1.89 |
| Total Volumeb | ||||||||
| No fibroids | 316 | 89.8 | 3,831 | 89.7 | 1.00 | Referent | 1.00 | Referent |
| First quartile | 5 | 1.4 | 114 | 2.7 | 0.55 | 0.23–1.31 | 0.55 | 0.23–1.30 |
| Second quartile | 11 | 3.1 | 107 | 2.5 | 1.22 | 0.69–2.17 | 1.12 | 0.63–1.99 |
| Third quartile | 10 | 2.8 | 110 | 2.6 | 1.09 | 0.60–2.00 | 0.95 | 0.52–1.74 |
| Fourth quartile | 10 | 2.8 | 108 | 2.5 | 1.11 | 0.61–2.03 | 0.87 | 0.47–1.60 |
| Largest Volumec | ||||||||
| No fibroids | 316 | 89.8 | 3,831 | 89.7 | 1.00 | Referent | 1.00 | Referent |
| First quartile | 5 | 1.4 | 115 | 2.7 | 0.55 | 0.23–1.30 | 0.55 | 0.23–1.31 |
| Second quartile | 11 | 3.1 | 106 | 2.5 | 1.23 | 0.70–2.19 | 1.10 | 0.62–1.97 |
| Third quartile | 7 | 2.0 | 112 | 2.6 | 0.77 | 0.37–1.60 | 0.66 | 0.32–1.37 |
| Fourth quartile | 13 | 3.7 | 106 | 2.5 | 1.43 | 0.85–2.42 | 1.14 | 0.67–1.95 |
| Fibroid Typed | ||||||||
| Any submucosal | 7 | 2.0 | 62 | 1.5 | 1.33 | 0.65–2.71 | 1.09 | 0.53–2.23 |
| Any intramural | 15 | 4.3 | 193 | 4.5 | 0.95 | 0.57–1.56 | 0.81 | 0.49–1.35 |
| Any subserosal | 16 | 4.5 | 185 | 4.3 | 1.04 | 0.65–1.69 | 0.91 | 0.56–1.49 |
| Any pedunculated | 3 | 0.9 | 28 | 0.7 | 1.27 | 0.43–3.74 | 0.99 | 0.33–2.93 |
| Location d | ||||||||
| Any cervix | 6 | 1.7 | 64 | 1.5 | 1.12 | 0.52–2.44 | 1.03 | 0.47–2.23 |
| Any fundus | 16 | 4.5 | 172 | 4.0 | 1.12 | 0.69–1.81 | 0.93 | 0.57–1.52 |
| Any corpus | 21 | 6.0 | 242 | 5.7 | 1.05 | 0.69–1.60 | 0.90 | 0.58–1.39 |
Abbreviations: RR Risk ratio, CI Confidence interval
a Adjusted for maternal age and race/ethnicity
b Quartiles for total fibroid volume: < 0.97 cm3, 0.97–4.76 cm3, 4.77–20.84 cm3, > 20.84 cm3
c Quartiles for largest fibroid volume: < 0.82 cm3, 0.82–4.62 cm3, 4.63–18.18 cm3, > 18.18 cm3
d Columns do not add up to 100% because a participant could contribute to more than one category if she had multiple fibroids, each category is a separate model with women without fibroids as referent group
Preterm birth clinical subtype was known for 60.0% of cases (n=211). Most commonly, preterm birth was secondary to spontaneous preterm labor (n=83, 39.3%), followed by medically indicated delivery for maternal or fetal conditions (n=78, 37.0%), and preterm births after PPROM (n=50, 23.7%). We did not detect an association between fibroid presence and medically indicated preterm birth (adjusted RR, 0.92; 95% CI, 0.43–1.96) or spontaneous preterm birth (adjusted RR, 1.27; 95% CI, 0.76– 2.11; Table 3). Findings did not change when adjusted for prior preterm birth.
Table 3.
Relationship between fibroid status and preterm birth by subtype, Right from the Start, 2000–2012 (n = 4,622)
| Outcome | Preterm | Unadjusted RR | 95% CI | Adjusted RRa | 95% CI | Adjusted RR, Secondaryb | 95% CI |
|---|---|---|---|---|---|---|---|
| All preterm births | 352 | 0.99 | 0.71–1.39 | 0.88 | 0.62–1.24 | 0.93 | 0.66–1.30 |
| Spontaneous | 133 | 1.35 | 0.83–2.20 | 1.27 | 0.76–2.11 | 1.29 | 0.77–2.17 |
| Preterm labor | 83 | 1.19 | 0.62–2.29 | 1.31 | 0.66–2.59 | 1.43 | 0.73–2.82 |
| PPROM | 50 | 1.65 | 0.78–3.49 | 1.18 | 0.53–2.62 | 1.12 | 0.48–2.58 |
| Medically indicated | 78 | 1.00 | 0.48–2.06 | 0.92 | 0.43–1.96 | 1.02 | 0.48–2.18 |
a All analyses are from separate models comparing preterm birth (or preterm birth subtype) to 4,270 term births, adjusted for maternal age and race/ethnicity
b Secondary analysis adjusted for maternal age, race/ethnicity, and history of preterm birth
Fibroid presence or size was not associated independently with late preterm, early preterm, or very early preterm birth. However, the number of women with deliveries prior to 34 weeks of gestation was small, and therefore this cohort is inadequately powered to assess risk for early and very early preterm births.
Discussion
In this prospective, community-based pregnancy cohort with standardized imaging for fibroid characterization in the first trimester, we did not find evidence that fibroid presence, size, location, or number influences risk of preterm birth. Fibroids were not associated with any clinical subtype of preterm birth. If fibroids increase preterm birth risk, the effect is notably more modest than previous literature indicates.
Given the null association between fibroids and preterm birth, let us consider the confidence we have in these results. Participants had a research ultrasound to determine fibroid presence, size, location, and type in the first trimester. Imaging was performed by experienced clinical sonographers using a detailed protocol to systematically characterize fibroids. This is an improvement over studies depending on maternal self-report, which fails to capture up to 80% of fibroids [37, 38], or retrospective ultrasound databases, which rely on imaging not meant to uniformly detect or characterize fibroids, and are therefore prone to misclassification. More rigorous methods for fibroid classification in this study better capture exposure and account for the higher prevalence of fibroids observed in this cohort compared with other studies.
We used community-based recruitment methods to enroll a cohort more representative of the general population than clinic-based studies [39]; though we acknowledge that those who volunteer to participate in a study of pregnancy health may be more health-conscious than those who do not. Additionally, we recruited women prior to conception or in the first trimester to ensure standardized fibroid assessment in early pregnancy. While this results in more rigorous exposure classification, it also necessitates that participants identified pregnancy early. These two factors may lead to a lower risk cohort than the general population.
We excluded women who used reproductive technologies to conceive from this analysis. The association between fibroids and preterm birth may be underestimated if fibroid characteristics linked to infertility also drive risk of preterm birth. Nonetheless, fibroid presence, size, and type were not associated with time to pregnancy in this cohort [40]. We did not find that maternal age or race modified the association between fibroids and preterm birth. However, further questions about risk attributable to fibroids in the setting of other factors such as prior myomectomy, prior C-sections, or the use of assisted reproductive technologies should be explored.
In most studies about fibroids and preterm birth [3–8, 10–18], spontaneous and medically indicated preterm birth are treated as the same outcome. Proposed biological mechanisms for risk associated with fibroids are architectural in nature (fibroids prevent proper placentation, impair distensibility of the uterus, cause uterine irritability and preterm contractions, or lead to intrauterine crowding) and are more in line with how fibroids may contribute to spontaneous preterm birth. We endeavored to determine if distinct relationships exist between fibroid status and preterm birth subtypes. Though women were followed prospectively in this cohort until pregnancy outcome, the effort to determine the subtype of preterm birth (spontaneous versus medically indicated) was done retrospectively. Information concerning the birth was insufficient to confidently classify subtype in 40.0% of cases and precision of subtype-specific estimates was limited. Consistent with a prospective study about predictors of medically indicated preterm birth, we did not find evidence fibroids are associated with increased risk of this subtype after adjusting for maternal age and race [25]. However, Meis et al. study relied on ultrasound reports not standardized to assess fibroid status, resulting in possible misclassification of fibroid status as suggested by the low prevalence of detected fibroids in the study population (1.5%) [9]. Due to the small number of cases for individual preterm birth subtypes, we could not assess how fibroid number, size, location, and type related to specific subtypes. Future studies about the relationship between fibroid characteristics and specific preterm birth subtypes are warranted.
Conclusions
We did not find evidence fibroids contribute to preterm birth risk in this prospective study of more than four thousand women, nor did we detect an association between fibroids and any clinical preterm birth subtype. To abate undue anxiety among expectant mothers, we encourage a reassessment of classifying presence of fibroids as a risk factor for preterm birth among women with normal fertility.
Acknowledgements
We would like to thank all the women who made the study possible.
Abbreviations
- BMI
Body mass index
- CI
Confidence intervals
- IQR
Interquartile range
- LMP
Last menstrual period
- OR
Odds ratio
- RR
Risk ratio
- PPROM
Preterm premature rupture of membranes
- SAB
Spontaneous abortion
Authors’ contributions
Dr. Alexandra Sundermann designed and conducted the analysis and drafted the manuscript. Dr. Tiara Aldridge helped conceptualize the project, advised the analysis design, and contributed to drafting and editing the manuscript. As the principal investigator, Dr. Hartmann obtained funding, designed the cohort, accomplished data collection, and participated in developing the analysis and key revisions. Sarah Jones assisted in data preparation, management of data quality, and manuscript revision. Eric Torstenson prepared the dataset and revised the manuscript. Dr. Digna Velez Edwards refined the analytic design, supervised the analysis, and revised the manuscript. The authors read and approved the final manuscript.
Funding
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (F30HD094345 to A.C.S., R01HD043883, and R01HD049675), the American Water Works Association Research Foundation (award 2579), and the National Institute of General Medical Studies award for the Vanderbilt Medical- Scientist Training Program (T32GM007347 to A.C.S.). The publication was supported by a CTSA award from the National Center for Advancing Translational Sciences (UL1TR000445) for data management infrastructure in REDCap.
Availability of data and materials
The datasets and materials used in the study are available from the corresponding author (Dr. Hartmann email address) via concept proposal request to the study senior investigators. Additional information about requesting Right from the Start data can be found at https://rightfromthestartstudy.org/collaborate/.
Declarations
Ethics approval and consent to participate
This study has been IRB approved by Vanderbilt University Medical Center IRB (#070037) and performed in accordance with the principles expressed in the Declaration of Helsinki. All the subjects participating in the study provided written informed consent.
Consent for publication
The participating subjects have provided informed written consent for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Laughlin SK, Baird DD, Savitz DA, Herring AH, Hartmann KE. Prevalence of uterine leiomyomas in the first trimester of pregnancy: An ultrasound-screening study. Obset Gyncol. 2009;113:630–5. doi: 10.1097/AOG.0b013e318197bbaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: A systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008;198:357–66. doi: 10.1016/j.ajog.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 3.Chen YH, Lin HC, Chen SF, Lin HC. Increased risk of preterm births among women with uterine leiomyoma: A nationwide population-based study. Hum Reprod. 2009;24:3049–56. doi: 10.1093/humrep/dep320. [DOI] [PubMed] [Google Scholar]
- 4.Ciavattini A, Clemente N, DelliCarpini G, Di Giuseppe J, Giannubilo SR, Tranquilli AL. Number and size of uterine fibroids and obstetric outcomes. J Matern Fetal Neonatal Med. 2015;28:484–8. doi: 10.3109/14767058.2014.921675. [DOI] [PubMed] [Google Scholar]
- 5.Conti N, Tosti C, Pinzauti S, Tomaiuolo T, Cevenini G, Severi FM, et al. Uterine fibroids affect pregnancy outcome in women over 30 years old: Role of other risk factors. J Matern Fetal Neonatal Med. 2013;26:584–7. doi: 10.3109/14767058.2012.745504. [DOI] [PubMed] [Google Scholar]
- 6.Coronado GD, Marshall LM, Schwartz SM. Complications in pregnancy, labor, and delivery with uterine leiomyomas: A population-based study. Obstet Gynecol. 2000;95:764–9. doi: 10.1016/s0029-7844(99)00605-5. [DOI] [PubMed] [Google Scholar]
- 7.Davis JL, Ray-Mazumder S, Hobel CJ, Baley K, Sassoon D. Uterine leiomyomas in pregnancy: A prospective study. Obstet Gynecol. 1990;75:41–4. [PubMed] [Google Scholar]
- 8.Exacoustos C, Rosati P. Ultrasound diagnosis of uterine myomas and complications in pregnancy. Obstet Gynecol. 1993;82:97–101. [PubMed] [Google Scholar]
- 9.Girault A, Le Ray C, Chapron C, Goffinet F, Marcellin L. Leiomyomatous uterus and preterm birth: An exposed/unexposed monocentric cohort study. Am J Obstet Gynecol. 2018;219:410. doi: 10.1016/j.ajog.2018.08.033. [DOI] [PubMed] [Google Scholar]
- 10.Mollica G, Pittini L, Minganti E, Perri G, Pansini F. Elective uterine myomectomy in pregnant women. Clin Exp Obstet Gynecol. 1996;23:168–72. [PubMed] [Google Scholar]
- 11.Qidwai GI, Caughey AB, Jacoby AF. Obstetric outcomes in women with sonographically identified uterine leiomyomata. Obstet Gynecol. 2006;107:376–82. doi: 10.1097/01.AOG.0000196806.25897.7c. [DOI] [PubMed] [Google Scholar]
- 12.Rice JP, Kay MH, Mahony BS. The clinical significance of uterine leiomyomas in pregnancy. Am J Obstet Gynecol. 1989;160:1212–6. doi: 10.1016/0002-9378(89)90194-4. [DOI] [PubMed] [Google Scholar]
- 13.Roberts WE, Fulp KS, Morrison JC, Martin JN. The impact of leiomyomas on pregnancy. Aust N Z J Obstet Gynaecol. 1999;39:43–7. doi: 10.1111/j.1479-828X.1999.tb03442.x. [DOI] [PubMed] [Google Scholar]
- 14.Shavell VI, Thakur M, Sawant A, Kruger ML, Jones TB, Singh M, et al. Adverse obstetric outcomes associated with sonographically identified large uterine fibroids. Fertil Steril. 2012;97:107–10. doi: 10.1016/j.fertnstert.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Sheiner E, Bashiri A, Levy A, Hershkovitz R, Katz M, Mazor M. Obstetric characteristics and perinatal outcome of pregnancies with uterine leiomyomas. J Reprod Med. 2004;49:182–6. [PubMed] [Google Scholar]
- 16.Stout MJ, Odibo AO, Graseck AS, Macones GA, Crane JP, Cahill AG. Leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes. Obstet Gynecol. 2010;116:1056–63. doi: 10.1097/AOG.0b013e3181f7496d. [DOI] [PubMed] [Google Scholar]
- 17.Vergani P, Ghidini A, Strobelt N, Roncaglia N, Locatelli A, Lapinski RH, et al. Do uterine leiomyomas influence pregnancy outcome? Am J Perinatol. 1994;11:356–8. doi: 10.1055/s-2007-994554. [DOI] [PubMed] [Google Scholar]
- 18.Zhao R, Wang X, Zou L, Li G, Chen Y, Li C, et al. Adverse obstetric outcomes in pregnant women with uterine fibroids in China: A multicenter survey involving 112,403 deliveries. PLoS One. 2017;12(11):e0187821. [DOI] [PMC free article] [PubMed]
- 19.Vergani P, Locatelli A, Ghidini A, Andreani M, Sala F, Pezzullo JC. Large uterine leiomyomata and risk of cesarean delivery. Obstet Gynecol. 2007;109:410–4. doi: 10.1097/01.AOG.0000250470.78700.f0. [DOI] [PubMed] [Google Scholar]
- 20.Lam SJ, Best S, Kumar S. The impact of fibroid characteristics on pregnancy outcome. Am J Obstet Gynecol. 2014;211:395. doi: 10.1016/j.ajog.2014.03.066. [DOI] [PubMed] [Google Scholar]
- 21.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Division of vital statistics. Births: final data for 2014. Natl Vital Stat Rep. 2015;64:1–65. [PubMed] [Google Scholar]
- 22.Goldenberg RL, Culhane JF, Iams JD, Romero R. Preterm birth 1: Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Savitz DA, Blackmore CA, Thorp JM. Epidemiologic characteristics of preterm delivery: Etiologic heterogeneity. Am J Obstet and Gynecol. 1991;164:467–71. doi: 10.1016/S0002-9378(11)80001-3. [DOI] [PubMed] [Google Scholar]
- 24.Ananth CV, Vintzileos AM. Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med. 2006;19:773–82. doi: 10.1080/14767050600965882. [DOI] [PubMed] [Google Scholar]
- 25.Meis PJ, Goldenberg RL, Mercer BM, Iams JD, Moaward AH, Miodovnik M, et al. The preterm prediction study: Risk factors for indicated preterm births. Am J Obstet Gynecol. 1998;178:562–7. doi: 10.1016/S0002-9378(98)70439-9. [DOI] [PubMed] [Google Scholar]
- 26.Meis PJ, Michielutte R, Peters TJ, Wells HB, Sands RE, Coles EC, et al. Factors associated with preterm birth in Cardiff, Wales: Indicated and spontaneous preterm birth. Am J Obstet and Gynecol. 1995;173:597–602. doi: 10.1016/0002-9378(95)90288-0. [DOI] [PubMed] [Google Scholar]
- 27.Berkowitz GS, Blackmore-Prince C, Lapinski RH, Savitz DA. Risk factors for preterm birth subtypes. Epidemiology. 1998;9:279–85. doi: 10.1097/00001648-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Gimenez LG, Krupitzki HB, Momany AM, Gili JA, Poletta FA, Campana H, et al. Maternal and neonatal epidemiological features in clinical subtypes of preterm birth. J Matern Fetal Neonatal Med. 2016;29:3153–61. doi: 10.3109/14767058.2015.1118035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Della Rossa PA, Miglioli C, Caglioni M, Tiberio F, Mosser KHH, Vignotto E, et al. A hierarchial procedure to select intrauterine and extrauterine factors for methodological validation of preterm risk estimation. BMC Pregnancy Childbirth. 2021;16(21):306. doi: 10.1186/s12884-021-03654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Promislow JH, Makarushka CM, Gorman JR, Howards PP, Savitz DA, Hartmann KE. Recruitment for a community-based study of early pregnancy: The Right From The Start study. Paediatr Perinat Epidemiol. 2004;18:143–52. doi: 10.1111/j.1365-3016.2003.00546.x. [DOI] [PubMed] [Google Scholar]
- 31.Michels KA, Hartmann KE, Archer KR, Ye F, Velez Edwards DR. The relationship between total fibroid burden and first trimester bleeding and pain. Paediatr Perinat Epidemiol. 2016;30:115–23. doi: 10.1111/ppe.12256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartmann KE, Velez Edwards DR, Savitz DA, Jonsson-Funk ML, Wu P, Sundermann AC, et al. Prospective cohort of uterine fibroids and miscarriage risk. Am J Epidemiol. 2017;186:1–9. doi: 10.1093/aje/kwx062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao SK, Wu P, Jones SH, Torstenson ED, Hartmann KE, Velez Edwards DR. Association of uterine fibroids with birthweight and gestational age. Ann Epidemiol. 2020;50:35–40.e2. doi: 10.1016/j.annepidem.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michels KA, Velez Edwards DR, Baird DD, Savitz DA, Hartmann KE. Uterine leiomyomata and cesarean birth risk: A prospective cohort with standardized imaging. Ann Epidemiol. 2014;24:122–6. doi: 10.1016/j.annepidem.2013.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Howards PP, Schisterman EF, Heagerty PJ. Potential confounding by exposure history and prior outcomes: An example from perinatal epidemiology. Epidemiology. 2007;18:544–51. doi: 10.1097/EDE.0b013e31812001e6. [DOI] [PubMed] [Google Scholar]
- 36.Weinberg CR. Toward a clearer definition of confounding. Am J Epidemiol. 1993;137:1–8. doi: 10.1093/oxfordjournals.aje.a116591. [DOI] [PubMed] [Google Scholar]
- 37.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman J. High cumulative incidence of uterine leiomyoma in black and white women: Ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–7. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 38.Myers SL, Baird DD, Olshan AF, Herring AH, Schroeder JC, Nylander-French LA. Self-report versus ultrasound measurement of uterine fibroid status. J Womens Health. 2012;21:285–93. doi: 10.1089/jwh.2011.3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Savitz DA, Dole N, Kaczor D, Herring AH, Siega-Riz AM, Kaufman J, et al. Probability samples of area births versus clinic populations for reproductive epidemiology studies. Paediatr Perinat Epidemiol. 2005;19:315–22. doi: 10.1111/j.1365-3016.2005.00649.x. [DOI] [PubMed] [Google Scholar]
- 40.Johnson G, MacLehose RF, Baird DD, Laughlin-Tommaso SK, Hartmann KE. Uterine leiomyomata and fecundability in the Right from the Start study. Hum Reprod. 2012;27:2991–7. doi: 10.1093/humrep/des263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets and materials used in the study are available from the corresponding author (Dr. Hartmann email address) via concept proposal request to the study senior investigators. Additional information about requesting Right from the Start data can be found at https://rightfromthestartstudy.org/collaborate/.