Abstract
Background:
After discharge from an acute care hospitalization, cancer patients may choose to pursue rehabilitative care in a skilled nursing facility (SNF)
Objective:
To examine receipt of anti-cancer therapy, death, readmission, and hospice use of cancer patients who discharge to a SNF compared to those who discharge home or home with home health services in the 6 months following an acute care hospitalization.
Patients and Methods:
We conducted a population-based cohort study using the Surveillance, Epidemiology, and End Results (SEER)-Medicare database of patients with stage II - IV colorectal, pancreatic, urinary bladder, or lung cancer who had an acute care hospitalization between 2010–2013. A total of 58,770 cases were identified and patient groups of interest were compared descriptively using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Logistic regression was used to compare patient groups, adjusting for covariates.
Results:
Of patients discharging to SNF, 21%, 17%, and 2% went on to receive chemotherapy, radiation, and targeted chemotherapy, respectively, whereas the rates were 54%, 28%, and 6% for patients discharging to home. Fifty-six percent of patients discharging to SNF died within 6 months of their hospitalization compared to 36% discharging to home. Thirty-day readmission rates were 29% and 28% for patients discharging to SNF and home, respectively. Twelve percent of patients in hospice received less than 3 days of hospice care prior to their death regardless of their discharge location.
Conclusion:
Patients with cancer who discharge to a SNF are significantly less likely to go on and receive oncologic treatment of any kind and have higher mortality compared to patients who discharge home after an acute care hospitalization.
Discussion:
Further research is needed to understand and address patient goals of care prior to SNF discharge.
Introduction
Studies have shown a significant correlation between functional status and survival for patients with cancer.1,2,3 The functional decline associated with progressive cancer is prognostic for health events that severely limit mobility and also with acute care hospitalizations.4 After discharge from an acute care hospitalization, patients may choose to pursue rehabilitative care in a skilled nursing facility (SNF). SNF care is considered a transitional period - a place where patients who are too weak to discharge home can go to receive skilled nursing care and rehabilitative therapies. Patients who discharge to a SNF are typically older, more medically complex, and have higher hospital readmission rates than patients who are strong enough to discharge home.5,6,7
The use of institutional post-acute care has increased from 21% in 2000 to 26% in 2015, resulting in Medicare spending more than $59 billion for these services in 2015.8,9 SNF services are covered by Medicare Part A (hospital insurance) which provides payments to SNF’s for a set period of time to care for patients after a qualifying hospital stay. Importantly, the SNF is the only setting that Medicare reimburses for 24-hour care after an acute care hospitalization for patients who are not eligible for long term acute care or inpatient rehabilitation.
There are two important limitations for patients with cancer who discharge to a SNF. First, patients with cancer rarely receive chemotherapy while admitted to a SNF because infusion chemotherapy is considered an outpatient procedure and covered by Medicare Part B whereas SNF’s are covered by Medicare Part A. To provide chemotherapy, SNFs would have to absorb the cost of administration and treatment. Second, availability of palliative care (PC) consultation remains limited for patients in the SNF.10
We sought to understand clinical outcomes of patients with stage II - IV pancreatic, colorectal, lung, and bladder cancer who discharge to a SNF when compared to patients who discharge home or home with home services. These cancer types were selected because we anticipated that these patients would have high rates of hospital admission and re-admission and likely be candidates for SNF discharge, thus providing us with a robust cohort of patients for our analysis. We assessed health care utilization by examining rates of receipt of cancer directed therapy, 30-day readmission, death, and hospice use 6 months after an acute care hospitalization. We hypothesized that the majority of patients who are discharged to a SNF do not subsequently receive oncologic treatment, have higher mortality and readmission rates, and lower hospice use when compared to patients who discharge home or home with home healthcare.
Methods
Data Source
The data source was the Surveillance, Epidemiology and End Results (SEER)-Medicare database. The SEER program collects data from select cancer registries covering approximately 28% of the U.S. population; 93% of persons age 65 and older in the SEER files are matched to the Medicare enrollment file. Seventy-two to 76% of the Medicare population enrolled in Medicare Fee-for-Service (FFS) during the years of our study. For cases enrolled in Medicare FFS, the combined file provides detailed demographic and clinical information collected by cancer registries at the time of diagnosis, plus covered health care services received prior to diagnosis, during initial treatment, and over the course of follow-up for the duration of available claims. The database also includes a limited set of census tract and zip code-level socioeconomic variables.11
Sample Selection
We selected patients with colorectal, pancreatic, bladder, or lung cancer diagnosed from 2010 to 2013. We excluded records from patients with a subsequent primary tumor or other prior cancer diagnoses other than Stage 0 or Stage 1 breast or cervical cancer, or non-metastatic prostate cancer diagnosed in the three years prior to the tumor of interest (total sample size, N = 301,776, including 5,242 patients with one of the accepted prior tumors specified). Our analysis only included de novo cancers and did not include recurrent cancers as this information is not provided in the SEER-Medicare database. We further restricted to patients with American Joint Committee on Cancer, 7th Edition (AJCC) Stage Group II-IV tumors at diagnosis to obtain the patient sample with regional or advanced disease (N = 190,692).12,13
We identified the patient sample for which we have complete claims data by restricting to patients age 66 years and older at diagnosis (N = 150,679) and excluding patients diagnosed at autopsy as well as those with a missing diagnosis date (n = 127) or with negative survival time (n = 359). We included only patients who were continuously enrolled in Medicare FFS Parts A and B from 12 months prior to diagnosis through death or the end of the study follow-up, December 2014 (N = 91,568).
The study sample was further limited to patients with a paid claim for a short-term inpatient stay subsequent to diagnosis that did not end in death or discharge to hospice (N = 64,160). We assigned the first stay occurring in the month of diagnosis or later as the index inpatient stay. We required that the index stay occur by June 2014, with continuous enrollment in Medicare FFS Part A and Part B for at least 6 months after discharge or until death if before 6 months, to ensure adequate follow-up for all outcome measures (N = 63,697). Furthermore, removing discharge locations other than the 3 settings of interest (eg, inpatient residential facility, Medicare certified long term care hospital, transfer to another hospital) brought the total sample to 58,770 patients. Of these, 29% (n = 16,936) had a prior oncologic visit (established) and 71% percent (n = 41,834) had no prior oncologic visit (unestablished) (Figure 1). The Colorado Multiple Institutional Review Board and the Duke Institutional Review Board approved this study.
Figure 1.
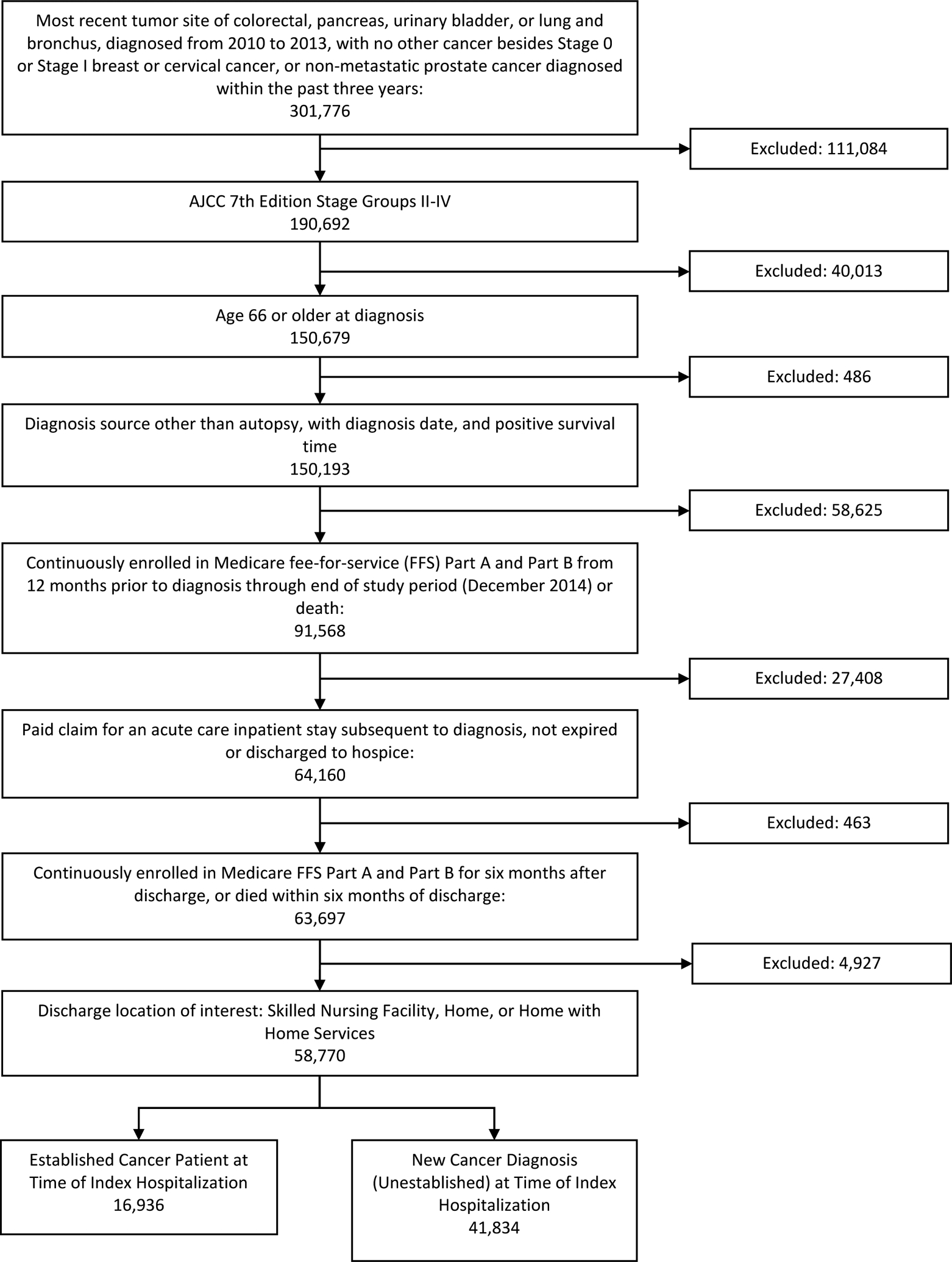
SEER-Medicare analysis sample derivation
Comparator Groups
Analyses were conducted among 3 comparison groups with discharge locations of interest: SNF, home, and home with home health service (N = 58,770). We defined a confirmed discharge to a SNF as the presence of a SNF claim with an admission date equal to the index discharge date. Discharges to home and to home with home health care were identified using the patient discharge status code reported on the inpatient claim.
Outcomes
The primary outcome was receipt of anti-cancer therapy following an inpatient hospitalization in the 6 months after discharge. Current Procedural Terminology (CPT) codes, Healthcare Common Procedure Coding System (HCPCS) codes, International Classification of Diseases, 9th Revision (ICD-9) procedure and diagnosis codes, and National Drug Codes (NDC) were used to identify treatment received, including radiation, chemotherapy, and targeted therapy. We included targeted therapy drugs approved by the Food and Drug Administration (FDA) for the tumor sites of interest that had specific HCPCS codes initiated prior to the December 2014. The selected drugs included bevacizumab, cetuximab, everolimus, panitumumab, ramucirumab, and ziv-aflibercept. Claims in the 6 months after discharge were used to obtain additional outcome measures: 30-day readmission, hospice use, and death. Hospice use was measured using the number of covered days of care reported on hospice claims in the 6 months following index discharge.
Control Variables
We used SEER variables to obtain patient demographics and tumor characteristics at diagnosis. We used claims to identify characteristics of the index inpatient stay, prior health conditions, health care services received as well as to generate the Charlson Comorbidity Index and identify specific conditions of interest using Chronic Conditions Data Warehouse algorithms. We also used treatment and other health care services received after diagnosis and prior to index admission including visits with an oncology specialist, prior radiation, chemotherapy, and targeted therapy, as covariates in the analysis.14
Statistical Analysis
The 3 patient groups of interest were compared descriptively using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. SEER-Medicare provides only the month of the cancer diagnosis but does not include date or setting in which the diagnosis was made. Patients with and without prior oncologist visits were considered separately in subsequent analyses to identify those patients with a known cancer diagnosis prior to index hospitalization from patients who were diagnosed with a new cancer at the time of index hospitalization. Subsequent cancer directed treatment, mortality, readmission, and hospice use were compared by discharge setting using chi-square tests. Logistic regression was used to compare patient groups, adjusting for covariates. Kaplan-Meier estimates were used to compare survival curves by patient group. For patients discharged to SNF, statistically significant predictors for the outcomes were identified using logistic regression and Cox proportional hazards regression. The regression models were developed using a random 50% subsample and validated on the remaining 50% subsample. Statistical significance was defined as p<0.05.
Results
Patient Characteristics
Our study population consisted of 58,770 people with stage II – IV colorectal (31%), lung (51%, with 77% non-small cell lung cancer), pancreatic (12%), or bladder cancer (6%) (Table 1). A total of 71% of patients were given a new cancer diagnosis at the time of index hospitalization (unestablished patients) whereas 29% of patients had a known cancer diagnosis before index hospitalization (established patients). Mean (SD) length of stay (LOS) for the index hospitalization was 6.9 (±SD5.8) for all patients. LOS was 5.0 (±SD3.8) days for patients discharging to home, 8.1 (±5.8) days for those discharging to home with home healthcare, and 10.6(±SD7.6) days for those discharging to a SNF.
Table 1.
Patient and Index Hospitalization Characteristics by Discharge Setting (n (%) or mean ± SD unless otherwise specified) – SEER-Medicare 2010–2013
| Characteristic | All | Home | Home Health | SNF |
|---|---|---|---|---|
| Total patients - N (% of the whole study sample 58770) | 58770 (100%) | 33057 (56%) | 13592 (23%) | 12121 (21%) |
| Male (vs. Female) | 29747 (50.6%) | 17770 (53.4%) | 6716 (49.4%) | 5261 (43.4%) |
| Age (years) | ||||
| Index Admission | 77.6 ± 7.1 | 76.2 ± 6.6 | 77.9 ± 7.0 | 81.0 ± 7.2 |
| Months between Diagnosis and Index Admission | 2.5 ± 3.8 | 2.6 ± 3.9 | 2.6 ± 3.7 | 2.4 ± 3.7 |
| Race | ||||
| White NH | 47668 (81.2%) | 26733 (81.0%) | 10826 (79.7%) | 10109 (83.4%) |
| Black NH | 4974 (8.5%) | 2697 (8.2%) | 1331 (9.8%) | 946 (7.8%) |
| Hispanic | 3070 (5.2%) | 1791 (5.4%) | 746 (5.5%) | 533 (4.4%) |
| Asian or Pacific Islander/American Indian/Alaska Native NH | 3002 (5.1%) | 1803 (5.5%) | 678 (5.0%) | 521 (4.3%) |
| Married or Partnered (vs. Non-married) | 29366 (50.0%) | 18547 (56.1%) | 6726 (49.5%) | 4093 (33.8%) |
| Census Tract Socioeconomic Status (SES) | ||||
| Median Income ($) | 61513.9 ± 25634.1 | 60509.0 ± 25300.2 | 62071.9 ± 26359.9 | 63635.6 ± 25566.1 |
| % of Residents below Poverty | 14.0 ± 9.3 | 14.3 ± 9.3 | 14.1 ± 9.3 | 13.2 ± 9.1 |
| % of Non-High School Grads | 14.4 ± 9.8 | 14.6 ± 9.9 | 14.6 ± 10.1 | 13.7 ± 9.5 |
| Charlson Comorbidity Index | ||||
| 0 | 19452 (33.1%) | 11848 (35.8%) | 4210 (30.1%) | 3394 (28.0%) |
| 1 | 16946 (28.8%) | 9879 (29.9%) | 3933 (28.9%) | 3134 (25.9%) |
| 2 | 9845 (16.8%) | 5288 (16.0%) | 2333 (17.2%) | 2224 (18.4%) |
| 3 or more | 12527 (21.3%) | 6042 (18.3%) | 3116 (22.9%) | 3369 (27.8%) |
| Year of Diagnosis | ||||
| 2010 | 15334 (26.1%) | 8601 (26.0%) | 3574 (26.3%) | 3159 (26.1%) |
| 2011 | 14812 (25.2%) | 8431 (25.5%) | 3358 (24.7%) | 3023 (24.9%) |
| 2012 | 14714 (25.0%) | 8270 (25.0%) | 3372 (24.8%) | 3072 (25.3%) |
| 2013 | 13910 (23.7%) | 7755 (23.5%) | 3288 (24.2%) | 2867 (23.7%) |
| Cancer Type & Stage | ||||
| Colorectal | 18472 (31.4%) | 9666 (29.2%) | 4239 (31.2%) | 4567 (37.7%) |
| Stage II | 7498 (40.6%) | 3941 (40.8%) | 1675 (39.5%) | 1882 (41.2%) |
| Stage III | 6528 (35.3%) | 3545 (36.7%) | 1474 (34.8%) | 1509 (33.0%) |
| Stage IV | 4446 (24.1%) | 2180 (22.6%) | 1090 (25.7%) | 1176 (25.8%) |
| Lung | 29792 (50.7%) | 17218 (52.1%) | 6823 (50.2%) | 5751 (47.5%) |
| Stage II | 3551 (11.9%) | 2139 (12.4%) | 834 (12.2%) | 578 (10.1%) |
| Stage III | 7634 (25.6%) | 4688 (27.2%) | 1655 (24.3%) | 1291 (22.5%) |
| Stage IV | 18607 (62.5%) | 10391 (60.4%) | 4334 (63.5%) | 3882 (67.5%) |
| Pancreas | 6897 (11.7%) | 4303 (13.0%) | 1531 (11.3%) | 1063 (8.8%) |
| Stage II | 2521 (36.6%) | 1507 (35.0%) | 613 (40.0%) | 401 (37.7%) |
| Stage III | 692 (10.0%) | 469 (10.9%) | 135 (8.8%) | 88 (8.3%) |
| Stage IV | 3684 (53.4%) | 2327 (54.1%) | 783 (51.1%) | 574 (54.0%) |
| Bladder | 3609 (6.1%) | 1870 (5.7%) | 999 (7.4%) | 740 (6.1%) |
| Stage II | 2000 (55.4%) | 1037 (55.5%) | 531 (53.2%) | 432 (58.4%) |
| Stage III | 639 (17.7%) | 335 (17.9%) | 196 (19.6%) | 108 (14.6%) |
| Stage IV | 970 (26.9%) | 498 (26.6%) | 272 (27.2%) | 200 (27.0%) |
| Health Care Utilization prior to Index Admission | ||||
| One or More SNF Stays | 5181 (8.8%) | 1279 (3.9%) | 800 (5.9%) | 3102 (25.6%) |
| Visit with Oncologist | 16936 (28.8%) | 9763 (29.5%) | 4351 (32.0%) | 2822 (23.3%) |
| Chemotherapy | 9584 (16.3%) | 5588 (16.9%) | 2529 (18.6%) | 1467 (12.1%) |
| Radiation | 6641 (11.3%) | 3652 (11.1%) | 1803 (13.3%) | 11.86 (9.8%) |
| Targeted Chemotherapy | 1131 (1.9%) | 669 (2.0%) | 281 (2.1%) | 181 (1.5%) |
| Index Hospital Characteristics | ||||
| Location | ||||
| Urban (vs. Rural) | 53137 (91.2%) | 29746 (90.1%) | 12401 (92.1%) | 10990 (90.7%) |
| Type | ||||
| Teaching (vs. Non-teaching) | 32107 (55.1%) | 17847 (54.5%) | 7767 (57.7%) | 6493 (53.6%) |
| Index Stay DRG (top 10 listed, *surgical) | ||||
| *330 MAJOR SMALL AND LARGE BOWEL PROCEDURES WITH CC | 7117 (12.2%) | 3704 (11.3%) | 1768 (13.1%) | 1645 (13.6%) |
| 181 RESPIRATORY NEOPLASMS WITH CC | 3441 (5.9%) | 2117 (6.4%) | 730 (5.4%) | 594 (4.9%) |
| 180 RESPIRATORY NEOPLASMS WITH MCC | 3196 (5.5%) | 1563 (4.7%) | 840 (6.2%) | 793 (6.6%) |
| *329 MAJOR SMALL AND LARGE BOWEL PROCEDURES WITH MCC | 2767 (4.7%) | 615 (1.9%) | 762 (5.6%) | 1390 (11.5%) |
| *331 MAJOR SMALL AND LARGE BOWEL PROCEDURES WITHOUT CC/MCC | 2477 (4.2%) | 1813 (5.5%) | 428 (3.2%) | 236 (2.0%) |
| *164 MAJOR CHEST PROCEDURES WITH CC | 2276 (3.9%) | 1399 (4.3%) | 623 (4.6%) | 254 (2.1%) |
| *167 OTHER RESPIRATORY SYSTEM O.R. PROCEDURES WITH CC | 1437 (2.5%) | 895 (2.7%) | 350 (2.6%) | 192 (1.6%) |
| *166 OTHER RESPIRATORY SYSTEM O.R. PROCEDURES WITH MCC | 1315 (2.2%) | 618 (1.9%) | 367 (2.7%) | 330 (2.7%) |
| 435 MALIGNANCY OF HEPATOBILIARY SYSTEM OR PANCREAS WITH MCC | 1276 (2.2%) | 798 (2.4%) | 283 (2.1%) | 195 (1.6%) |
| 375 DIGESTIVE MALIGNANCY WITH CC | 1258 (2.1%) | 898 (2.7%) | 180 (1.3%) | 180 (1.5%) |
Data were rarely missing (<1%, except SES variables ~4%).
P-values are not shown because all comparisons were highly significant due to the large sample size.
CC – complication or comorbidity; MCC – major complication or comorbidity
Patient Outcomes
Of SNF discharges, 21%, 17%, and 2% of SNF went on to receive chemotherapy, RT, and targeted chemotherapy, respectively, compared to 54%, 28%, and 6%, respectively, among home discharges. Furthermore, 56% of SNF discharges died within 6 months of their hospitalization compared to 36% of patients who discharged home (Figure 2a and 2b). Thirty-day readmission rates were 29% and 28% for SNF and home discharges, respectively and 12% of patients in hospice received less than 3 days of hospice care prior to their death regardless of their discharge location. Patients who had a major bowel surgery seemed more likely to require SNF care after hospitalization.
Figure 2a.
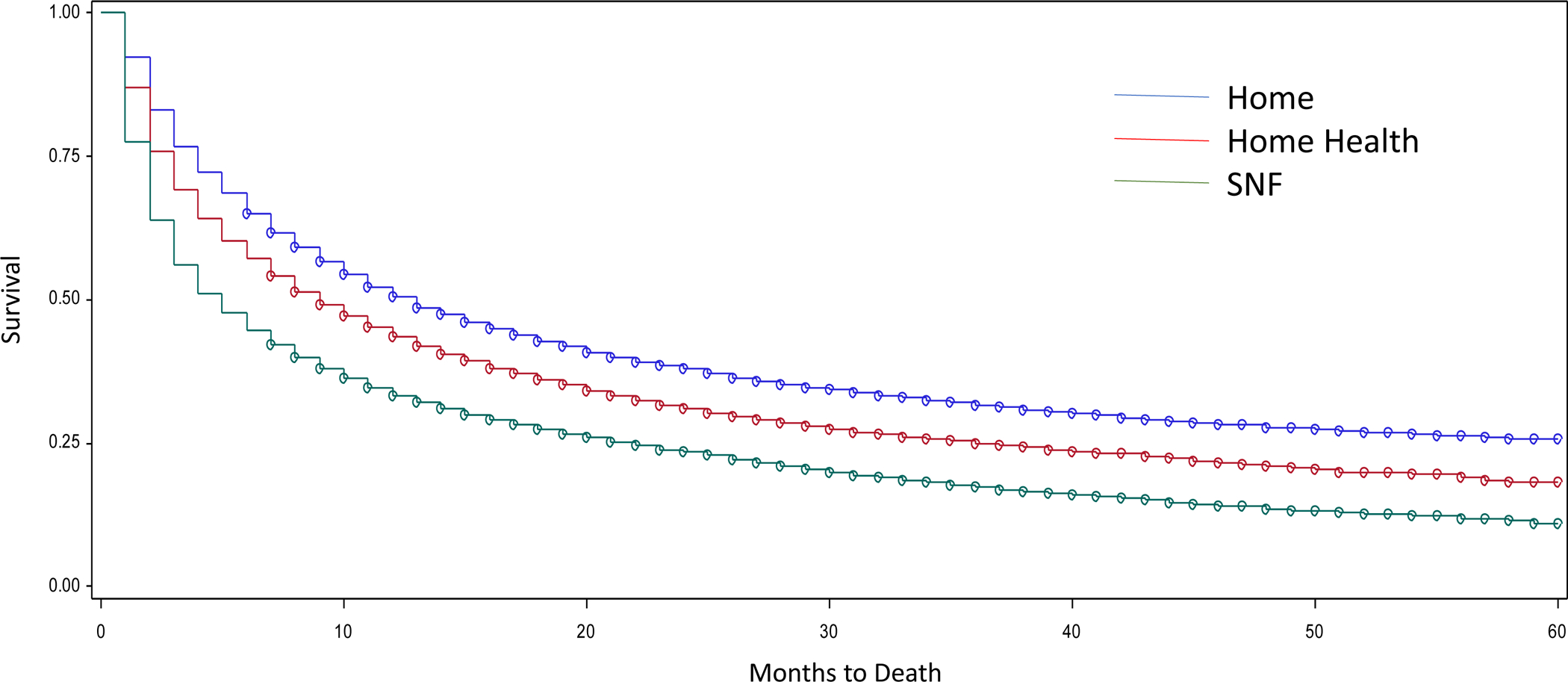
Kaplan Meier Survival Curve – Unestablished Cancer Patients
Figure 2b.
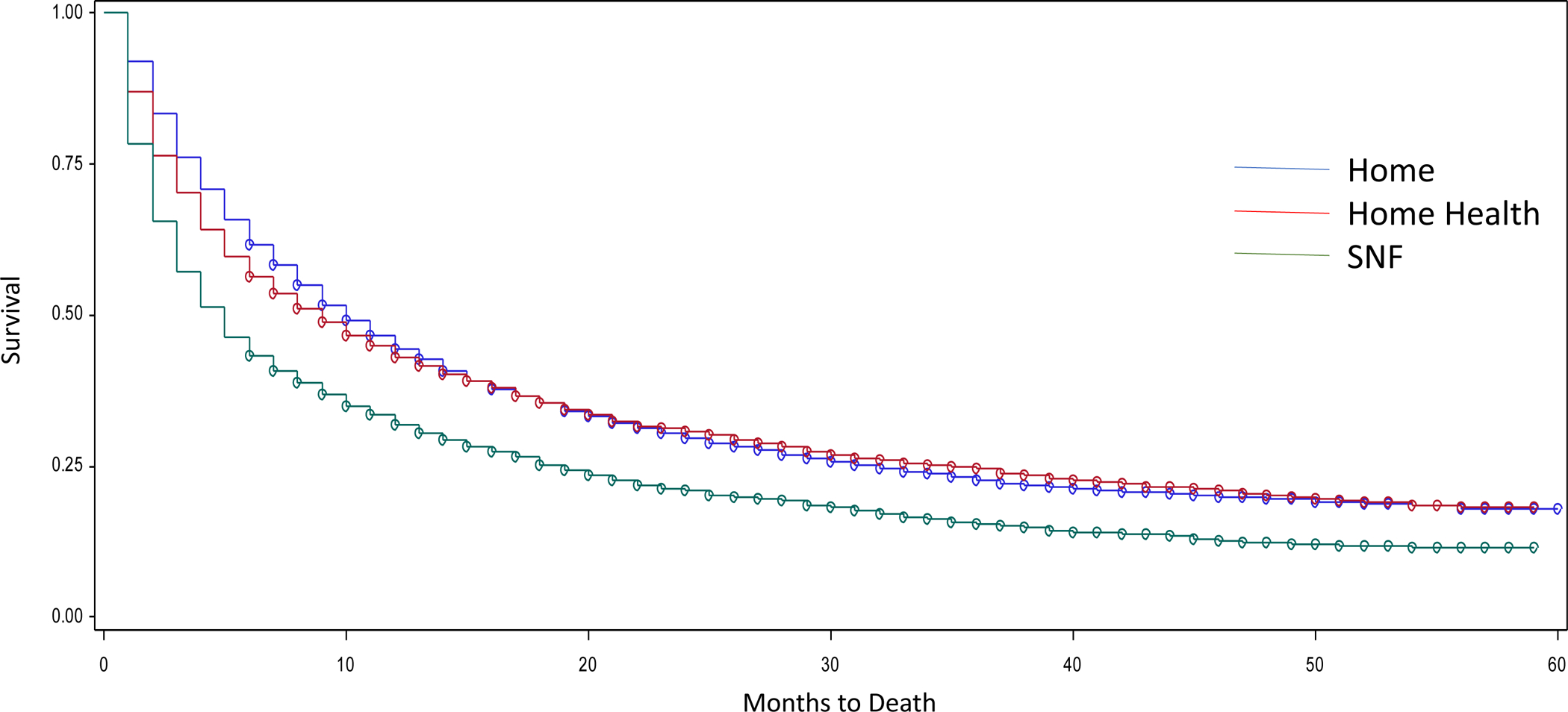
Kaplan Meier Survival Curve – Established Cancer Patients
A total of 29% of unestablished cancer patients who discharged to a SNF went on to receive any cancer treatment (chemotherapy, RT, targeted chemotherapy) compared to 60% of patients discharged home (Table 2).
Table 2.
Outcomes at 6 Months – Unestablished Cancer Patients
| Adjusted ± OR (95% CI) vs Home | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Home | Homecare | SNF | p-value | Homecare | Adjusted p-value | SNF | Adjusted p-value | |||
| N=41834 | N=23294 | N=9241 | N=9299 | |||||||
| Any Treatment | N=4116* | 13646 (59.5%) | 4530 (50.0%) | 2649 (28.8%) | <0.001 | 0.78 (0.73–0.82) | <0.001 | 0.40 (0.37–0.42) | <0.001 | |
| Any Chemotherapy Infusion | N=4121* | 11677 (50.9%) | 3592 (39.6%) | 1675 (18.2%) | <0.001 | 0.74 (0.70–0.79) | <0.001 | 0.32 (0.30–0.34) | <0.001 | |
| Radiation | N=4176* | 6279 (27%) | 2251 (24.4%) | 1490 (16%) | <0.001 | 0.94 (0.88–1.00) | 0.04 | 0.66 (0.62–0.71) | <0.001 | |
| Targeted Chemotherapy | N=4175* | 1265 (5.4%) | 448 (4.9%) | 194 (2.0%) | <0.001 | 0.89 (0.78–1.004) | 0.06 | 0.41 (0.34–0.48) | <0.001 | |
| Death 6 months following admission | 8178 (35.1%) | 3966 (42.9%) | 5141 (55.3%) | <0.001 | 1.36 (1.28–1.45) | <0.001 | 2.49 (2.31–2.67) | <0.001 | ||
| Hospice use 6 months following admission | N=1728** | 5159 (63.1%) | 2619 (66.0%) | 2706 (52.6%) | <0.001 | 1.14 (1.05–1.24) | 0.003 | 0.64 (0.59–0.70) | <0.001 | |
| Hospice LOS < 3 days | N=1048*** | 616 (11.9%) | 307 (11.7%) | 368 (13.6%) | 0.06 | 1.01 (0.86–1.17) | 0.95 | 1.22 (1.05–1.42) | 0.01 | |
| 30-day Readmission | 6693 (28.7%) | 2699 (29.2%) | 2688 (28.9%) | 0.69 | 1.00 (0.95–1.06) | 0.98 | 1.03 (0.97–1.09) | 0.37 | ||
Excludes few cases with data error where prior cancer treatment is indicated
Number of patients who died
Number of patients who received hospice before death
prior treatment (prior chemotherapy, prior radiation, and prior targeted chemotherapy; or prior any therapy for any treatment outcome), discharge year, cancer type and stage, grade, age at index admission, months between diagnosis and index admission, male, white NH, urban, index hospital region and characteristics, prior hypertension, prior diabetes, prior COPD, prior heart disease, prior stroke, prior cognitive disorder, index admission LOS, Charlson comorbidity index categories, per capita income, median income, percent of non-high school grads, percent of residents below poverty, married or partnered, prior depressive disorders, prior alcohol use disorder, prior drug use, prior tobacco use.
For patients with a known cancer diagnosis and receipt of prior treatment, 42% of those discharged to a SNF went on to receive any further cancer treatment compared with 74% of those discharged home. Table 3.
Table 3.
Outcomes at 6 Months – Established Cancer Patients
| Adjusted ± OR (95% CI) vs Home | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Home | Homecare | SNF | p-value | Homecare | Adjusted p-value | SNF | Adjusted p-value | |||
| N=16936 | N=9763 | N=4351 | N=2822 | |||||||
| Any Treatment | 0.72 (0.67–0.79) | <0.001 | 0.39 (0.35–0.43) | <0.001 | ||||||
| Prior Receipt | N=10648* | 4483 (73.5%) | 1772 (63.3%) | 736 (42.1%) | <0.001 | |||||
| Chemotherapy | 0.71 (0.66–0.77) | <0.001 | 0.34 (0.30–0.38) | <0.001 | ||||||
| Prior Receipt | N=8963* | 3615 (68.9%) | 1358 (57.7%) | 447 (32.9%) | <0.001 | |||||
| Radiation | 0.83 (0.76–0.91) | <0.001 | 0.66 (0.59–0.75) | <0.001 | ||||||
| Prior Receipt | N=6570* | 1496 (41.5%) | 553 (30.9%) | 299 (25.4%) | <0.001 | |||||
| Targeted Chemotherapy | 0.71 (0.58–0.85) | <0.001 | 0.44 (0.33–0.57) | <0.001 | ||||||
| Prior Receipt | N=1054* | 287 (45.6%) | 93 (35.6%) | 36 (22.1%) | <0.001 | |||||
| Death 6 months following admission | 3746 (38.4%) | 1902 (43.7%) | 1599 (56.7%) | <0.001 | 1.46 (1.34–1.59) | <0.001 | 2.51 (2.27–2.78) | <0.001 | ||
| Hospice use 6 months following admission | N=7247** | 2484 (66.3%) | 1231 (64.7%) | 907 (56.7%) | <0.001 | 0.93 (0.82–1.05) | 0.23 | 0.68 (0.59–0.78) | <0.001 | |
| Hospice LOS < 3 | N=4622*** | 255 (10.3%) | 123 (10.0%) | 122 (13.5%) | 0.02 | 0.94 (0.74–1.18) | 0.58 | 1.28 (0.999–1.63) | 0.0501 | |
| 30-day Readmission | 2403 (24.6%) | 1245 (28.6%) | 823 (29.2%) | <0.001 | 1.20 (1.10–1.31) | <0.001 | 1.20 (1.07–1.34) | 0.001 | ||
Number of patients who received cancer treatment before index hospitalization
Number of patients who died
Number of patients who received hospice before death
prior treatment (prior chemotherapy, prior radiation, and prior targeted chemotherapy; or prior any therapy for any treatment outcome), discharge year, cancer type and stage, grade, age at index admission, months between diagnosis and index admission, male, white NH, urban, index hospital region and characteristics, prior hypertension, prior diabetes, prior COPD, prior heart disease, prior stroke, prior cognitive disorder, index admission LOS, Charlson comorbidity index categories, per capita income, median income, percent of non-high school grads, percent of residents below poverty, married or partnered, prior depressive disorders, prior alcohol use disorder, prior drug use, prior tobacco use.
Predictors of SNF success for Established and Unestablished Cancer Patients
For unestablished patients, those with lung, pancreatic, and bladder cancer were more likely to go on to receive any further treatment compared to those with colorectal cancer. Unestablished patients with stage III cancer were more likely to receive future treatment compared with those with stage IV cancer patients. Both established and unestablished patients with stage II cancer were less likely to receive future oncologic treatment compared to those with stage IV cancer. Both established and unestablished patients with cognitive impairment were less likely to receive future treatment.
For all patients discharged to a SNF, stage II and III cancer were associated with a lower risk of death and longer time to death (measured in months), indicated by a lower hazard of death when compared to stage IV cancer. For established cancer patients, those who had received chemotherapy before their index hospitalization were less likely to die compared with those who had received no treatment before index admission (Table 4).
Table 4.
Predictors for SNF Success in Outcomes at 6 Months - Established Cancer Patients (OR (95% CI) unless otherwise specified)
| Variable | Any Treatment | Death | Hospice | Hospice LOS < 3 | 30-day Readmission | Months to Death HR* (95% CI) |
|---|---|---|---|---|---|---|
| N=1411 | N=1397 | N=805 | N=460 | N=1397 | N=1397 | |
| c=0.64 | c=0.75 | c=0.66 | c=0.57 | c=0.62 | ||
| Male (vs. Female) | 1.66 (1.30–2.11) | 1.22 (1.08–1.37) | ||||
| Age (years) at Index Admission | 0.96 (0.94–0.98) | 1.015 (1.01–1.024) | ||||
| Months between Diagnosis and Index Admission | 0.95 (0.93–0.97) | |||||
| White NH (vs. Other) | 1.54 (0.99–2.38) | |||||
| Married or Partnered (vs. Non-married) | ||||||
| Urban | 1.85 (1.15–2.98) | 1.27 (1.001–1.61) | ||||
| SES | ||||||
| Per Capita Income ($1000) | ||||||
| Median Income ($1000) | ||||||
| % of Residents below Poverty | ||||||
| % of Non-High School Grads | ||||||
| Charlson Comorbidity Index Categories | 1.16 (1.04–1.29) | |||||
| Cancer Type (vs. Colorectal) | ||||||
| Lung | 2.83 (2.05–3.92) | 1.32 (0.97–1.79) | 1.85 (1.53–2.22) | |||
| Pancreas | 3.55 (2.23–5.65) | 1.07 (0.68–1.69) | 2.36 (1.86–3.00) | |||
| Bladder | 1.66 (0.93–2.97) | 2.07 (1.26–3.41) | 1.2 (0.87–1.70) | |||
| Cancer Stage (vs. Stage IV) | ||||||
| Stage II | 0.60 (0.45–0.80) | 0.31 (0.22–0.42) | 0.74 (0.54–1.02) | 0.52 (0.44–0.61) | ||
| Stage III | 0.94 (0.73–1.22) | 0.33 (0.24–0.44) | 0.71 (0.53–0.94) | 0.55 (0.47–0.63) | ||
| Grade** (vs. 9) | ||||||
| 1 | 0.33 (0.17–0.64) | 0.54 (0.38–0.76) | ||||
| 2 | 0.55 (0.39–0.77) | 0.71 (0.59–0.85) | ||||
| 3 | 0.74 (0.54–1.002) | 0.87 (0.75–1.01) | ||||
| 4 | 1.28 (0.71–2.31) | 1.02 (0.75–1.40) | ||||
| Prior to Index Admission | ||||||
| One or More SNF Stays | ||||||
| Any Therapy | ||||||
| Chemotherapy | 0.67 (0.52–0.87) | |||||
| Radiation | 1.68 (1.28–2.20) | 1.18 (1.04–1.34) | ||||
| Targeted Chemotherapy | 2.34 (1.18–4.62) | |||||
| HTN | 0.74 (0.55–0.99) | 0.82 (0.72–0.94) | ||||
| Diabetes | ||||||
| COPD | 1.16 (1.02–1.32) | |||||
| Heart | ||||||
| Stroke | 0.47 (0.25–0.89) | |||||
| Cognitive | 0.44 (0.27–0.69) | 1.84 (1.17–2.88) | ||||
| Alcohol | 2.39 (1.23–4.63) | |||||
| Depression | 1.60 (1.08–2.38) | |||||
| Index Hospital | ||||||
| Region (vs. West) | ||||||
| Northeast | 1.98 (1.40–2.81) | |||||
| Midwest | 3.90 (2.21–6.88) | |||||
| South | 1.86 (1.20–2.88) | |||||
| Location: Urban (vs. Rural) | 2.01 (1.22–3.33) | 0.69 (0.53–0.91) | ||||
| Type: Teaching (vs. Non-teaching) | 0.76 (0.60–0.96) | 0.85 (0.76–0.96) | ||||
| LOS | 0.96 (0.94–0.99) | 0.92 (0.86–0.99) | 1.03 (1.01–1.05) | |||
| Discharge Year |
Hazard Ratio
Grade I: well differentiated; differentiated, NOS
Grade 2: moderately differentiated; moderately differentiated; intermediate differentiation
Grade 3: poorly differentiated; differentiated
Grade 4: undifferentiated; anaplastic
Grade 9: cell type not determined, not stated or not applicable
Discussion
This study describes post-acute care outcomes of patients with stage II – IV colorectal, lung, pancreatic, and bladder cancer discharged to a SNF after an acute care hospitalization. Data show that these patients are significantly less likely to go on and receive cancer treatment of any kind and are more likely to die within 6 months of discharge compared with patients discharged home. Only approximately one-fifth of patients discharged to a SNF received subsequent chemotherapy compared with slightly more than half of patients discharged home. This analysis also shows how ill this cancer population is - 42% of all patients who had an acute care hospitalization discharged to home, home with health care, and SNF had died within 6 months of discharge.
Although these findings are not unexpected, the magnitude of the difference in outcomes of patients who discharge to a SNF compared to those who discharge home is striking. This analysis of SEER Medicare data confirms previous research of SNF populations in general. Patients who discharge to a SNF are more frail, older, and have more comorbidities than those who discharge home. Thus, poorer outcomes in the SNF population of this study are not unexpected but rather most congruent with their projected outcomes based on their clinical morbidities. Although we attempted to adjust for patient-level differences, including hospital characteristics, the cohorts are inherently different, and the discharge location essentially serves as a surrogate for functional status. The intent of this study was to understand the impact of discharge location, as a surrogate for function, on subsequent rates of cancer directed treatment. The American Society of Clinical Oncology recommends against the use of chemotherapy in patients with solid tumors who have not benefited from prior treatment and who have an Eastern Cooperative Oncology Group (ECOG)15 performance status (PS) score of 3 or more.16 These findings suggest that if the intent of sending this patient population to a SNF is to recover functional status and receive cancer directed therapy, most patients will not realize this goal.
Discharging patients with cancer who have a poor prognosis to a SNF setting hinders the ability of patients to express their goals of care and participate in end of life planning due to limited access of palliative care in SNFs. Previous studies have shown that oncologists struggle with communicating prognosis and with saying “no” to continued chemotherapy treatment in patients with end stage cancer.17,18 This struggle likely contributes to the poor prognostic understanding and unrealistic expectations patients experience at the end of their life. The proportion of patients using short-term hospice services (3 days or less) decreased from 9.8% to 7.7%. Our study revealed that 13.6% and 11.9% of patients who discharged to SNF or home, respectively, had a hospice LOS < 3 days.19 These numbers are higher than national averages for both discharge locations (SNF and home). It is possible that the standard Medicare requirement to select either hospice or SNF care may lead to lower hospice enrollment. The Medicare Care Choices Model, allowing for concurrent hospice and cancer directed treatment, might increase hospice utilization in this population.20
This study reveals differences between patients with an established cancer diagnosis compared to those who were newly diagnosed with cancer. Patients with unestablished cancer were less likely to receive future oncologic treatment at all discharge locations compared with established cancer patients who had received prior oncologic treatment of any kind. We posit the functional decline that unestablished cancer patients experience is primarily driven by the malignancy itself while patients with established cancer and exposure to cancer directed therapy might be experiencing functional decline as a result of their treatment or a complication of treatment and thus might be more likely to regain functional strength to receive future cancer directed therapy after a SNF stay.
Results of this study should prompt consideration of the financial implications of discharging patients with cancer with functional decline to a SNF. Although readmissions were not statistically different between the discharge locations, 29% of patients were readmitted within 6 months of their acute care hospitalization. High hospital readmission rates from the post-acute care setting have become exceedingly problematic for hospitals and SNF’s, because they now receive financial penalties for these readmissions and lower quality metrics. This is largely driven by the Medicare Hospital Readmission Reduction Program and the increasing prevalence of bundled payments and shared-savings programs since the passage of the Patient Protection and Affordable Care Act.21,22 Feder, et al. studied hospital and SNF clinicians’ perceptions of goals of care discussions for patients discharged to a SNF and found that discordant goals of care among patients, family members, and clinicians were perceived to contribute to poor patient outcomes at SNF and to increased hospital readmissions.23
Limitations
Our study has several limitations. The SEER-Medicare data set is a secondary claims database that does not provide a measure of functional status or social support, which are both factors that might influence disposition after acute care hospitalization and the outcomes we measured. We do not know the goals of patients in discharging to a SNF. Regardless, CMS has set up a reimbursement infrastructure with the view that SNF’s are to serve a rehabilitative function. Our analysis of SEER-Medicare data from 2010–2013 is immediately prior to the increase in the use of immunotherapy – a treatment which might not have the same performance status requirements as traditional cytotoxic chemotherapy. Preliminary research has shown that older patients with an ECOG PS of 2 or higher had poor outcomes despite receipt of immunotherapy and that overall survival was primarily driven by a patient’s ECOG PS.24 Further research is needed to understand the relationship between immunotherapy and functional outcomes as these patient populations were under-represented in clinical trials involving those with immunotherapies.25 We note that patients with earlier stage disease might have received surgery as their primary treatment modality and might not be candidates for adjuvant treatment. Evaluating post-acute care outcomes of cancer patients undergoing primary surgical treatment of their malignancy is an important line of inquiry but beyond the scope of this paper. Lastly, future receipt of outpatient oral cancer directed therapy was not captured in this study as oral medications are covered by Medicare Part D and these claims were not analyzed.
Conclusion
Our study shows that the majority of patients with stage II - IV colorectal, lung, bladder, and pancreatic cancer who discharge to a SNF are less likely to receive cancer directed treatment and more likely to die compared to those who are functionally able to discharge home. Next steps include better understanding patients’ goals of care when discharging to a SNF and developing and implementing targeted interventions that improve Palliative Care delivery models to patients in the SNF setting.
Supplementary Material
Funding
This project is supported by the Palliative Care Research Cooperative Group funded by the National Institute of Nursing Research U24NR014637.
This project was supported by Population Health Shared Resources, University of Colorado Cancer Center, P30CA046934.
Footnotes
Disclosures
Authors Sarguni Singh, Megan Eguchi, Sung-Joon Min, and Stacy Fischer report no conflicts of interest.
References
- 1.Verweij NM, Schiphorst AH, Pronk A, et al. Physical performance measures for predicting outcome in cancer patients: a systematic review. Acta Oncol. 2016December;55(12)1386–1391. [DOI] [PubMed] [Google Scholar]
- 2.Studenski S, Perera S, Patel K. Gait speed and survival in older adults. JAMA 2011; 305:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stanaway FF, Gnjidic D, Blyth FM, et al. How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over. BMJ. 2011;343:d7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cesari M, Kritchevsky SB, Newman AB, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging, and Body Composition Study. J AM Geriatr Soc. 2009;57:251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke RE, Juarez-Colunga E, Levy C, et al. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med. 2015February;175(2):295–296. [DOI] [PubMed] [Google Scholar]
- 6.Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff Proj Hope. 2010February;29(1):57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA. 2014October15;312(15:1542–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werner R, Konetzka T. Trends in Post-Acute Care Use Among Medicare Beneficiaries 2000 to 2015. JAMA. 2018;319(15):1616–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Redberg R The Role of Post-Acute Care in Variation in the Medicare Program. JAMA Intern Med. 2015;175(6):1058. [DOI] [PubMed] [Google Scholar]
- 10.Lester PE, Stefanacci RG, Feuerman M. Prevalence and description of palliative care in US nursing homes: a descriptive study. Am J Hosp Palliat Care. 2016;33:171–177. [DOI] [PubMed] [Google Scholar]
- 11.Surveillance, Epidemiology, and End Results (SEER) Program; National Cancer Institute. Overview of the SEER Program. https://seer.cancer.gov/about/overview.html
- 12.National Cancer Institute, Division of Cancer Control and Population Sciences. SEER-Medicare: Medicare Enrollment & Claims Data. https://healthcaredelivery.cancer.gov/seermedicare/medicare/
- 13.National Cancer Institute, Division of Cancer Control and Population Sciences. SEER-Medicare: How the SEER & Medicare Data are Linked. https://healthcaredelivery.cancer.gov/seermedicare/overview/linked.html
- 14.Center for Medicare and Medicaid Services. Chronic Conditions Data Warehouse. https://www.ccwdata.org/web/guest/condition-categories
- 15.Eastern Cooperative Oncology Group. ECOG performance status. http://ecog-acrin.org/resources/ecog-performance-status.
- 16.Schnipper LE, Smith TJ, Raghavan D, et al. American Society of Clinical Oncology identifies give key opportunities to improve care and reduce costs: the top five list for oncology. J Clin Oncol. 2012;30(14):17175–1724. [DOI] [PubMed] [Google Scholar]
- 17.Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program—a positive alternative. N Engl J Med. 2012April12;366(15):1363–1366 [DOI] [PubMed] [Google Scholar]
- 18.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012March22;366(12):1075–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teno JM, Gozalo P, Trivedi AN, et al. Site of death, place of care and health care transitions among US Medicare beneficiaries, 2000 – 2015. JAMA 2018;320:264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Centers for Medicare & Medicaid Services. Medicare Care Choices Model enables concurrent palliative and curative care. J Pain Palliat Care Pharmacother 2015;29:401–403. [DOI] [PubMed] [Google Scholar]
- 21.Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program – a positive alternative. N Engl J Med 2012;366:1364–1366. [DOI] [PubMed] [Google Scholar]
- 22.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med 2012;366:1075–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feder SL, Britton MC, Chaudhry SI. “The Need to Have an Understanding of Why They’re Coming Here and What Outcomes Might Be.” Clinician Perspectives on Goals of Care for Patients Discharging from Hospitals to Skilled Nursing Facilities. J Pain Symptom Manage. 2018March;55(3):930–937. [DOI] [PubMed] [Google Scholar]
- 24.Muchnik E, Loh KP, Strawderman M, et al. Immune checkpoint inhibitors in real-world treatment of older adults with non-small cell lung cancer. J AM Geriatr Soc 2019;67:905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanesvaran R, Cordoba R, Maggiore R. Immunotherapy in Older Adults with Advanced Cancers: Implications for Clinical-Decision Making and Future Research. Am Soc Clin Oncol Educ Book. 2018May23;(38):400–414. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


