Abstract
There is a relative dearth of research on features of schizotypal personality in children, in part due to lack of instrumentation. This study tests 5 competing models of the factor structure of the self-report Schizotypal Personality Questionnaire for Children (SPQ-C) and examines its relationship with a family history of schizotypal personality disorder (SPD), child abuse, and stability over time. Hypotheses were tested on 454 11- to 12-year-old schoolchildren and their caregivers. Confirmatory factor analyses supported a 3-factor structure of the SPQ-C (cognitive-perceptual, interpersonal, and disorganized). Test-retest stability was relatively robust over 3 months (r = .67), 6 months (r = .64), and 12 months (r = .55), with acceptable internal reliabilities (r = .84 to .91). Regarding construct validity, children with a biological family history of SPD had higher scores on all 3 factors (d =.51). Abused children had higher schizotypy scores (d = .55). A genetic × environment interaction was observed, with schizotypy highest in those with both a family history of schizotypy and also child abuse. Findings are the first in the child schizotypy field to document a gene × environment interaction and the independence of child abuse from confounding genetic influences. Results support the utility of the SPQ-C in future family and clinical studies of schizotypal personality and provide an avenue for much-needed and neglected research into the early antecedents of child schizotypal personality.
Keywords: schizotypy, family history, abuse, children, cognitive-perceptual, interpersonal, disorganized
Introduction
Schizotypy is a multidimensional construct sitting on a continuum of psychosis and representing a risk factor for schizophrenia-spectrum disorders and full-blown psychosis.1,2 Despite progress on adult schizotypy,3 schizotypy studies on children are scarce, even though understanding the progression of schizotypy throughout childhood and into the adolescence could enhance our understating of the etiology of schizophrenia-spectrum disorders. Insufficient instrumentation may be one reason for this significant gap. This study examines a self-report instrument for assessing childhood schizotypy, the Schizotypal Personality Questionnaire for Children (SPQ-C), with the broader goal of stimulating future research on the early antecedents of schizotypal personality disorder (SPD).
The most comprehensive analysis of the factor structure of the adult Schizotypal Personality Questionnaire-Brief (SPQ-B) tested 5 models across 14 countries.4 Results supported both the original and modified 3-factor structure5,6 and also a new “bifactor” structure consisting of the original 3-factor model (cognitive-perceptual, interpersonal, and disorganized) with the addition of one general factor.4 These 3 factors reflect the classic triad of positive, negative, and disorganized symptoms frequently observed in psychosis.7 Based on these adult findings, and because one study using the SPQ-C with Spanish children confirmed this 3-factor structure,8 we hypothesized that this same 3-factor structure would be the best-fitting model in children.
A second issue concerns the stability of schizotypal personality. In contrast to studies reporting short-term test-retest reliability,9,10 very few studies on schizotypal personality have reported the stability of schizotypy over a year or longer. In adults, a 2-year test-retest reliability of the adult SPQ has been reported at .53,11 with 6-year stability for schizotypy being somewhat lower (.41).12 It has been argued that 75%–90% of subclinical psychotic features in the general population disappear over time,13 suggesting significant instability. This instability argument could be taken further with children who show greater plasticity and developmental change, an issue we examined in the current study.
We also sought to address 2 more substantive etiological issues spanning environment and genetics—child abuse and biological family history of SPD. Abuse is associated with the development of later psychotic symptoms at age 1214 and represents the risk factor most commonly associated with the persistence of schizotypy in adults.15 One large clinical study of individuals diagnosed with SPD found child trauma to be related to cognitive-perceptual and interpersonal, but not disorganized, features of schizotypy.16 Another study observed positive relationships between child abuse and positive, but not negative, symptoms in psychotic patients.17 Similarly, positive relationships between abuse and positive schizotypal features, but not disorganization, have been observed in nonclinical adults.18 Other trauma studies have found stronger effects for cognitive-perceptual19 and weaker effects for disorganization.20,21 With one exception,14 no study has assessed the role of abuse in relation to child schizotypy, a gap we aimed to fill.
Within the context of the vulnerability—stress model of schizotypy,2,13 a second etiological issue concerns relationships between the SPQ-C and family history of SPD. Adult schizotypy has a heritable basis and runs in families.22 If the SPQ-C is a valid indicator of child schizotypy, some relationships should be anticipated with a family history of SPD. Whether this is true for all aspects of schizotypy is less clear. The traditional perspective argues that negative schizotypy features have a somewhat stronger genetic link to schizophrenia.23,24 This proposition receives support from reviews and empirical studies,25–28 although discrepant findings exist.29,30 In contrast to this robust adult literature, there is no prior study on family history of SPD and schizotypy in children. Given this prior literature, we hypothesized that the interpersonal (negative) factor of the SPQ-C would be most related to the family history of SPD.
These issues are addressed in 11-year-old children. We hypothesized that a 3-factor cognitive-perceptual/interpersonal/disorganized model would best fit the data, that reliability of the SPQ-C would be adequate, but that stability would be moderate-to-low given developmental change and the instrument’s brevity. Schizotypy was hypothesized to be positively associated with child abuse and family history of SPD, while abuse would be more associated with positive schizotypy features. The interpersonal (negative) factor of the SPQ-C was hypothesized to be most related to a family history of SPD.
Methods
Participants
Full details of participants are given elsewhere.31 Briefly, 454 male and female English-speaking children aged 11–12 years from an urban community of Philadelphia were recruited. Inclusion criteria consisted of: 11–12 years of age; English-speaking; and absence of mental retardation, psychotic disorder, or pervasive developmental disorders. Written informed consent was obtained from the caregiver, with assent obtained from the child. Ethnic composition was as follows: Caucasian (12.4%), African American (79.9%), Latino (0.7%), Asian (0.5%), Native American (0.2%), Multiracial (5.1%), and Other (0.9%), with 0.2% declining to answer. Families were recruited using targeted mailings, flyers, advertisements, and personal referrals. The mean household monthly income of the participants was $2994.56 (SD = $3173.39). The sample was at moderate risk for psychopathology due to the urban catchment area and low income. Missing data details are provided in the online supplementary material. Ethical approval was obtained from IRB boards at the University of Pennsylvania and the Philadelphia Department of Health.
Schizotypal Personality Questionnaire-Child (SPQ-C)
Schizotypal personality was assessed using the self-report Schizotypal Personality Questionnaire-Child (SPQ-C). The SPQ-C is a downward extension of the adult Schizotypal Personality Questionnaire-Brief (SPQ-B),5 which in turn is a short form of the adult 74-item SPQ.32 Consisting of 22 yes-no self-report statements, the SPQ-C contains all items from the SPQ-B with relatively minor modification for use with children aged 9 and above (see supplementary material for a freely available copy of the instrument). It measures 3 main factors of schizotypy—cognitive-perceptual, interpersonal, and disorganized features6—together with a total score. Beginning support has been observed for its internal reliability and construct validity.10,21,33,34
Child Abuse
Past child abuse was assessed using a modification of the Conflict Tactics Scale (CTS),35 which has been prospectively validated on adults physically abused 20 years previously based on official court reports of child abuse.36 The instrument showed good discriminant and predictive validity.36 A dimensional measure of abuse was created consisting of verbal and physical abuse items, with a categorical measure based on those experiencing no abuse (N = 135) vs some abuse (N = 306). Internal reliability (omega) in this study was high (.87).
Family History of SPD
Family history of SPD was obtained from an interview with the primary caregiver by interviewers trained in semi-structured clinical interviews and blinded to SPQ-C scores. Diagnoses on first- and second-degree biological relatives of the child (mother-father, grandmother, and grandfather) were made using the Family History - Research Diagnostic Criteria (FH-RDC).37 Positive responses to questions were followed up with probe questions. Final consensus diagnoses were arrived at in consultation with the first author who was also blind to SPQ-C scores. Those whose parent or grandparent met criteria for DSM-IV SPD38 were assigned to the family history positive group (N = 58), with others assigned to the family history negative group (N = 293). Moderately good sensitivity and excellent specificity have been reported for this instrument.39 See supplementary table S2 for missing data analyses.
Statistical Analyses
Confirmatory factor analysis (CFA) using the weighted least squares means- and variance-adjusted weighted least squares (WLSMV) estimator for skewed dichotomous data was conducted in MPlus 7.4 for Mac.40 Five models were tested (see table 1): one factor (schizotypy total), 2 intercorrelated factors (positive and negative schizotypy), 3 intercorrelated factors (cognitive-perceptual, interpersonal, and disorganized),5 3 intercorrelated factors with 4 paranoid items cross-loading on cognitive-perceptual and interpersonal subscales,6 and a bifactor model4 with items loading on both one general factor and 3 latent factors (cognitive-perceptual, interpersonal, and disorganized).6 Standardized betas and 6 fit indices were reported for all models. Better fits are indicted by a higher (>.90) comparative fit index (CFI) and higher (>.90) Tucker-Lewis index (TLI) and lower (<.06) root mean squared error of approximation (RMSEA) and Akaike Information Criterion (AIC). McDonald’s omega (ω)41 was used to calculate internal reliability with 95% confidence intervals.
Table 1.
Fit Indices for the 5 Different Factor Models of the SPQ-C (N = 447)
| Model | χ 2 (df) | CFI | TLI | RMSEA (90% CI) | P | WRMR | AIC (χ 2 − 2df) |
|---|---|---|---|---|---|---|---|
| 1. Single factor | 445.682 (209) | .915 | .906 | .050 (.044–.057) | .457 | 1.231 | 27.682 |
| 2. Two factors Positive vs Negative | 432.866 (208) | .919 | .910 | .049 (.043–.056) | .573 | 1.211 | 16.866 |
| 3. Original 3 factorsa Cog, Int, and Dis | 348.109 (206) | .949 | .943 | .039 (.032–.046) | .995 | 1.066 | −63.891 |
| 4. Modified 3 factorsb Cog, Int, and Dis | 314.782 (202) | .959 | .953 | .035 (.028–.043) | 1.00 | 0.998 | −89.218 |
| 5. Bifactorc Cog, Int, Dis,General | 230.593 (187) | .984 | .981 | .023 (.010–.032) | 1.00 | 0.809 | −143.407 |
Correction for the attenuation of stability coefficients due to measurement error was conducted using Spearman’s correction for attenuation.42 Binary logistic regression was used to assess SPQ-C differences between abused and non-abused groups using the forward Wald stepwise selection method with entry testing based on the significance of the score statistic, with the Wald statistic used to test variable removal, and the Nagelkerke R2 statistic used as an effect size. Because prior work has shown that those scoring in the top 10% of the SPQ have high rates of SPD,11,32 we adopted this cut-point on the SPQ-C for logistic regression analyses.
To test the interaction between abuse and family history of SPD, binary logistic regression using the forward stepwise Wald method was used, with high/low schizotypy group as the dependent variable and abuse, family history, and their interaction term as predictors. Significant interactions were broken down using t-test comparisons. Odds ratios were derived from the exponentiation of the beta coefficient.
Results
Psychometric Properties of the SPQ-C
Factor Structure
Fit indices for the 5 models are given in table 1 (see supplementary material for factor loadings). All models gave acceptable fits, with RMSEA at .051 or below and both CFI and TLI above .90. Nevertheless, some models were better fits than others. The original and modified 3-factor models were indistinguishable from one another and were better fits than two- and one-factor models. The best-fitting model was the bifactor model4 consisting of the 3-factor model6 with one overarching general factor.
Factor Intercorrelations
Factor intercorrelations were as follows: cognitive-perceptual/interpersonal (r = .56), cognitive-perceptual/disorganized (r = .53), and interpersonal/disorganized (r = .47). Findings indicate overlapping shared variance but separable identities for the 3 factors.
Internal Reliability
Omega coefficients (and confidence intervals) are as follows: total score .93 (.924–.947), cognitive-perceptual .852 (.833–.897), interpersonal .845, (.825–.876), and disorganized .851 (.829–.888). Item-total correlations are as follows: total score (r = .30–.51), cognitive-perceptual (r = .27–.52), interpersonal (r = .27–.44), and disorganized (r = .33–.48).
Stability
Test-retest stability for the total SPQ-C score was relatively strong over 3 months (r = .67, P < .001), 6 months (r = .64, P < .001), and 12 months (.55, P < .001). Correcting for measurement error resulted in the following stability coefficients: 3 months (r = .80), 6 months (r = .76), and 12 months (r = .65). One-year stability coefficients were slightly lower for the subscales, ranging from .43 to .45 when uncorrected and .59 to .66 when corrected for measurement error attenuation (see supplementary material for further details).
Family History of SPD
Children with a family history of SPD had higher total SPQ-C scores than controls, with an effect size (Cohen’s d) of .51 (see table 2—upper). All 3 factors were associated with family history of SPD as follows: cognitive-perceptual (d = .46), interpersonal (d = .36), and disorganized (d = .47).
Table 2.
Schizotypy Scores and Group Comparisons in Those With and Without a Family History of Schizotypal Personality Disorder (Upper Half) and Those With and Without a History Of Child Abuse (Lower Half)
| Family History + (N = 58) | Family History − (N = 287) | t | P | d | |
|---|---|---|---|---|---|
| SPQ-C | |||||
| Total | 9.71 (5.18) | 7.24 (4.76) | 3.54 | .001 | .51 |
| Cognitive-perceptual | 3.26 (2.29) | 2.32 (2.03) | 3.16 | .002 | .46 |
| Interpersonal | 3.97 (2.23) | 3.21 (2.11) | 2.45 | .015 | .36 |
| Disorganized | 1.69 (1.63) | 2.58 (1.79) | 3.30 | .001 | .47 |
| Abused | Non-abused | t | P | d | |
| SPQ-C | |||||
| Total | 8.57 (4.86) | 5.99 (4.37) | 5.27 | .0001 | .55 |
| Cognitive-perceptual | 2.82 (2.11) | 1.83 (1.93) | 4.62 | .0001 | .48 |
| Interpersonal | 3.72 (2.14) | 2.81 (1.97) | 4.19 | .0001 | .44 |
| Disorganized | 2.01 (1.66) | 1.53 (1.52) | 3.95 | .0001 | .41 |
Binary logistic regression analyses indicated that disorganization was the best predictor of family history (Wald χ 2 = 9.93, df = 1, P = .002), after which there was only a trend for cognitive-perceptual (P = .099), and no effect for interpersonal (P = .24).
Child Abuse
Abused children had significantly higher total SPQ-C scores (d = .55, see table 2—lower). All 3 factors were associated with family history of SPD as follows: cognitive-perceptual (d = .48), interpersonal (d = .44), and disorganized (d = .41).
Binary logistic regression analyses indicated that the cognitive-perceptual factor was the best predictor of abuse (Wald χ 2 = 19.45, df = 1, P < .0001). The interpersonal factor improved model fit slightly (Wald χ 2 = 4.02, df = 1, P = .045), but the disorganized factor was nonsignificant (P = .13).
Total schizotypy scores correlated significantly (r = .31) with caregivers abusing their children. Schizotypy factors all correlated with abuse (r = .22 to .32). Linear regression using the stepwise method in which all 3 factors were entered as predictors of abuse indicated that cognitive-perceptual was primarily associated with abuse (F change = 49.28, df = 1, P < .0001), after which no other factor added to the prediction equation (P = .12). As such, both binary logistic regression and linear regression analyses converged on the primary finding of higher cognitive-perceptual scores in abused children.
Interaction Between Abuse and Family History of SPD
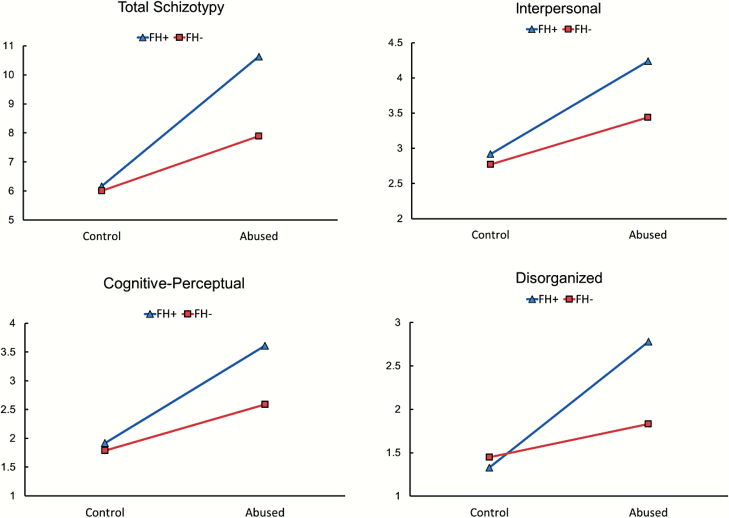
The interaction between abuse and family history of SPD in predicting schizotypy grouping was significant (Wald χ 2 = 6.03, df = 1, P = .014, odds ratio = 7.50). The moderating effect of family history of SPD on the abuse-schizotypy relationship is illustrated in figure 1. The highest SPQ-C scores were observed when abuse combined with a family history of SPD. Those with a family history of SPD had higher total SPQ-C scores when abuse was present (t = 3.46, df = 232, P = .001), but not when abuse was absent (t = 0.11, df = 105, P = .91). Taken together, abuse, family history of SPD, and their interaction explained 31.1% of the variance in schizotypy group membership (χ 2 = 24.32, df = 3, P < .0001), correctly classifying 71.0% of all cases.
Fig. 1.
Illustration of the interaction between child abuse and family history of SPD for total schizotypy and the 3 factors scores. FH+, family history positive; FH−, family history negative.
Analyses were repeated on the 3 SPQ-C factors. Interactions were significant for cognitive-perceptual (Wald χ 2 = 4.65, df = 1, P = .031, odds ratio = 3.91), interpersonal (Wald χ 2 = 4.44, df = 1, P = .035, odds ratio = 6.16), and disorganized (Wald χ 2 = 10.47, df = 1, P = .001, odds ratio = 7.12). Interactions are illustrated in figure 1, which show the highest schizotypy scores in those who were both abused and had a family history of SPD. Full details of these interactions are provided in the online supplementary material.
Can the Effect of Abuse Be Accounted for by Genetic Transmission of Schizotypy?
Logistic regression analyses were run to evaluate (a) the effect of abuse on schizotypy controlling for family history of SPD and (b) the effect of family history on schizotypy controlling for abuse. Abuse remained a significant predictor of total schizotypy after controlling for family history (Wald χ 2 = 10.36, df = 1, P = .001). Similarly, family history remained significant after controlling for abuse (Wald χ 2 = 4.91, df = 1, P = .027). Both processes acted as relatively independent predictors of schizotypy. The results for the 3 schizotypy factors converge on the same conclusions (see online supplementary material).
Discussion
This study aimed to address several substantive issues on childhood schizotypy. The SPQ-C factor structure mirrored that of the adult SPQ-B, reflecting cognitive-perceptual, interpersonal, and disorganized features. Adequate internal reliability was documented. Reasonable stability over 1 year was observed, establishing the trait nature of schizotypy captured by the instrument. Construct validity was documented in 2 ways, with both abuse and family history of SPD being associated with higher SPQ-C scores. Schizotypy was highest in children with both a family history of SPD and who also experienced abuse. Findings of this study are the first to document a gene × environmental interaction in relation to child schizotypy and suggest that the SPQ-C can be usefully employed either as a brief screen, a dimensional tool, or as a supplement to clinical interviewing to further prospective longitudinal research into the progression and course of schizotypy from childhood into adolescence and adulthood.
Psychometrics and Subdimensions of Childhood Schizotypy
Five competing factor structure models were tested. All provided acceptable fits, although models involving 3 factors produced better fits. Amongst these, the 3-factor model6 subsumed under a general factor (bifactor model) was the best-fitting model.4 This model has the advantage of parsimony and practicality—one single measure for broad investigations of the schizotypy construct and with 3 dimensions for more fine-grained analyses. The fact that CFA findings from the child SPQ parallel those observed with the adult SPQ4,43 both provides support for the factorial validity of the SPQ-C, and also the utility of both child and adult versions of the SPQ in future child-parent research.
Acceptable internal reliability for the SPQ-C was obtained. Reliability for the total scale score of .93 compares favorably to 2 prior studies reporting reliabilities of .8144 and .83.10 Subscale reliabilities are lower at .85 due to reduced item length (6–8) but are in the acceptable range, particularly since consistent item-total correlations were obtained for all 3 subscales (all r = .27 to .52). Furthermore, factor intercorrelations were in the anticipated range (r = .47 to .56).
An important conceptual question concerns whether there is value in considering subdimensions of schizotypy in developmental research.1 It is notable that the DSM throughout its development has ignored the fact that schizotypy has separable components. Some argue that prospective research has been overly focused on positive symptoms, bypassing the potential predictive role of negative schizotypal traits.45 Clinical developmental studies have shown that different dimensions of schizotypy interact,1 and that differential correlates of schizotypy factors exist.1,46 The 3 cognitive-perceptual, interpersonal, and disorganized subdimensions are repeatedly observed in CFAs of positive and negative symptoms of schizophrenia.7 Examining how these 3 substrates emerge in childhood, unfold in adolescence, and evolve as separable processes in adult schizophrenia could be a profitable model for future research. Conceivably, a greater focus on child schizotypy could provide more persuasive evidence than hitherto for greater recognition of these different processes and provide clinical utility for a multidimensional consideration.
Stability of Child Schizotypal Personality
We hypothesized that 1-year stability of child schizotypy would be low to moderate for several reasons, including childhood developmental change, scale brevity, and only modest prior findings on more developmentally stable adults using a longer SPQ (74 items).11 This hypothesis was only partially supported. Stability for total scores was somewhat higher than anticipated at .55, and correcting for measurement error it increased to .65, suggesting stability of schizotypy even in childhood. Two important caveats are that stability may be lower (a) during adolescence when peer influences prevail and (b) over longer time periods. Unlike some prior findings observing stronger stability for negative schizotypy11 and greater instability for cognitive-perceptual features,45 all 3 dimensions showed equivalent levels of stability (see supplementary material). Future child longitudinal research on stability could further address factors influencing the exacerbation and diminution of schizotypal symptoms over time.
Child Abuse and Family History
Construct validity for the SPQ-C was provided by child abuse being associated with higher total schizotypy scores. Regression analyses found the strongest effects for the cognitive-perceptual factor, after which interpersonal was minimally related, while disorganization was unrelated. Similar findings have been observed in prior studies.14,17,18,47 From a theoretical perspective, it has been hypothesized that cognitive-perceptual features reflect a form of schizotypy with an etiological foundation more in early psychosocial influences (including abuse) compared with other schizotypy factors.48 With some exceptions, findings on adult schizotypy have supported this prediction. The fact that similar findings are also obtained for children provides convergent validity for this child instrument.
Construct validity for the SPQ-C was also found with respect to biological family history of SPD. All 3 factors were associated with a family history of SPD. This suggests a genetic influence on schizotypal traits, although family history findings may best be considered as “quasi-genetic” as they also reflect environmental as well as genetic influences. We previously found that 70.5% of the developmental stability of the SPQ-C over 3 years can be explained by genetic influences, providing support for heritable influences on child schizotypy.34 We had hypothesized that negative features of schizotypy (ie, the interpersonal factor) would be most strongly related to family history. This hypothesis was not supported. Regression analyses indicated that disorganization had the strongest link to family history after which cognitive-perceptual was only marginally significant, while interpersonal was no longer significant. Because this study is the first to report on child schizotypy and family history of SPD, it is unclear whether they point to a developmental discontinuity with the adult literature, or alternatively reflect spurious findings, an issue requiring further resolution in child schizotypy studies.
Gene × Environment Interaction
The most striking finding in relation to construct validity concerns the interaction between abuse and family history of SPD. Schizotypy scores were highest when both risk factors were present, and this was true for all 3 factors (see figure 1). While such interactions have not been investigated in child schizotypy, studies of adult schizotypy do suggest gene × environmental effects. One Spanish study found that child abuse combined with carrying the brain-derived neurotrophic factor (BDNF) MET allele (negatively affecting brain growth) predisposed to increased psychotic-like experiences.49 Two other molecular genetic studies on adults have produced similar findings.50,51 Stronger effects were again found for disorganization, although interactions held for all 3 schizotypy factors. Current findings provide support for the construct validity of the SPQ-C and encourage further examination of which psychosocial risk factors interact with which genetic influences in predisposing to childhood schizotypy.
We found abuse and family history to operate as independent processes. In contrast, one adult study found only a small relationship between abuse and SPD, a relationship abolished after controlling for genetic influences. This led its authors to conclude that focusing on child trauma may not be a fruitful endeavor.52 Our contrasting findings are, however, consistent with a longitudinal study showing a link between childhood abuse and later psychotic-like experiences at age 12, even after controlling for genetic risk for psychosis.14 As such, we tentatively conclude that rather than representing an artifact of genetic influences, child abuse may be a genuine risk factor for child schizotypy.
From a theoretical perspective, findings on abuse and family history can be interpreted within the context of the vulnerability-stress model of schizotypy.2,13 Reviews of adolescent schizotypy have highlighted a neurodevelopmental framework whereby environmental “hits” during adolescence act on genetic predisposition to enhance vulnerability for schizophrenia-spectrum disorders.2 Regressing this adolescent model back to childhood, child abuse in the current study may represent the environmental “hit,” which acts on family history of schizotypy (genetic influence) to predispose to child schizotypy. Our findings can also be viewed within the psychosis proneness-persistence-impairment model of psychosis. This model argues that while genetic influences result in varying degrees of transitory psychotic experiences, persistence arises in the presence of environmental exposures (including abuse) interacting with genetic risk.13 How mechanistically gene-environment interactions like these explain the transition from trait schizotypy to psychotic outcome is much less clear, and resolution of this issue constitutes an important goal for future developmental schizotypy research.
Limitations and Conclusions
Limitations of this study need to be recognized. The sample was at moderate risk for psychopathology and is not representative of the general population. We did not have a diagnostic measure of child schizotypy for further validation of the SPQ-C. We only assessed 2 forms of abuse (physical and verbal), and as such similar findings may or may not be observed with emotional and sexual abuse. Schizotypy self-report reports are also subject to bias and we did not control for social desirability or employ an infrequency scale.
In conclusion, this study provides several new findings in the field of child schizotypy, encapsulating a gene × environmental interaction, child abuse as a risk factor independent of genetic influences, the influence of family history of SPD, and establishment of a bifactor model. It also provides further support for the utility of the SPQ-C in screening/assessing schizotypal features in children. Because this instrument can be completed in as little as 3 minutes, it can be easily incorporated into survey studies, family studies, and used as an adjunct to clinical assessment tools. The promise is that such instrumentation can provide a vehicle for researching the childhood antecedents of schizotypy on much larger populations than hitherto to enrich our understanding of the developmental underpinnings of schizophrenia-spectrum disorders and also provide longitudinal pointers for prevention/intervention studies.
Supplementary Material
Funding
This project was supported in part by grants to the first author from the National Institute of Child Health and Development (R01HD087485) and the Pennsylvania Department of Health (SAP# 4100043366).
References
- 1.Debbané M, Barrantes-Vidal N. Schizotypy from a developmental perspective. Schizophr Bull. 2015;41 (Suppl 2):S386–S395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fonseca-Pedrero E, Debbané M. Schizotypal traits and psychotic-like experiences during adolescence: an update. Psicothema 2017;29(1):5–17. [DOI] [PubMed] [Google Scholar]
- 3.Cohen AS, Chan RCK, Debbane M. Crossing boundaries in schizotypy research: an introduction to the special supplement. Schizophr Bull. 2018;44:S457–S459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fonseca-Pedrero E, Ortuño-Sierra J, Lucas-Molina B, et al. Brief assessment of schizotypal traits: a multinational study. Schizophr Res. 2018;197:182–191. [DOI] [PubMed] [Google Scholar]
- 5.Raine A, Benishay D. The SBQ-B: a brief screening instrument for schizotypal personality disorder. J Pers Disord. 1995;9(4):346–355. [Google Scholar]
- 6.Raine A, Reynolds C, Lencz T, Scerbo A, Triphon N, Kim D. Cognitive-perceptual, interpersonal, and disorganized features of schizotypal personality. Schizophr Bull. 1994;20(1):191–201. [DOI] [PubMed] [Google Scholar]
- 7.Tibber MS, Kirkbride JB, Joyce EM, et al. The component structure of the scales for the assessment of positive and negative symptoms in first-episode psychosis and its dependence on variations in analytic methods. Psychiatry Res. 2018;270:869–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fonseca-Pedrero E, Ortuno J, Paino M, Lemos-Giraldez S, Muniz J. Schizotypal experiences in adolescence: psychometric properties of schizotypal personality questionnaire-child. An de Psicol. 2015;31(2):414–421. [Google Scholar]
- 9.Wong KK, Freeman D, Hughes C. Suspicious young minds: paranoia and mistrust in 8-to 14-year-olds in the UK and Hong Kong. Br J Psychiatry. 2014;205(3):221–229. [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Wong KK, Dong F, Raine A, Tuvblad C. The Schizotypal Personality Questionnaire – Child (SPQ-C): psychometric properties and relations to behavioral problems with multi-informant ratings. Psychiatry Res. 2019;275:204–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stefanis NC, Vitoratou S, Ntzoufras I, Smyrnis N, Evdokimidis I, Stefanis CN. Psychometric properties of the Greek version of the Schizotypal Personality Questionnaire (SPQ) in young male obligatory conscripts: a two years test-retest study. Pers Individ Differ. 2006;41(7):1275–1286. [Google Scholar]
- 12.Venables PH, Raine A. The stability of schizotypy across time and instruments. Psychiatry Res. 2015;228(3):585–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. [DOI] [PubMed] [Google Scholar]
- 14.Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168(1):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Velikonja T, Velthorst E, McClure MM, et al. Severe childhood trauma and clinical and neurocognitive features in schizotypal personality disorder. Acta Psychiatr Scand. 2019;140(1):50–64. [DOI] [PubMed] [Google Scholar]
- 17.Heins M, Simons C, Lataster T, et al. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. 2011;168(12):1286–1294. [DOI] [PubMed] [Google Scholar]
- 18.Cicero DC, Kerns JG. Can disorganized and positive schizotypy be discriminated from dissociation? J Pers. 2010;78(4):1239–1270. [DOI] [PubMed] [Google Scholar]
- 19.Quidé Y, Cohen-Woods S, O’Reilly N, Carr VJ, Elzinga BM, Green MJ. Schizotypal personality traits and social cognition are associated with childhood trauma exposure. Br J Clin Psychol. 2018;57(4):397–419. [DOI] [PubMed] [Google Scholar]
- 20.Gong JB, Wang Y, Lui SSY, Cheung EFC, Chan RCK. Childhood trauma is not a confounder of the overlap between autistic and schizotypal traits: a study in a non-clinical adult sample. Psychiatry Res. 2017;257:111–117. [DOI] [PubMed] [Google Scholar]
- 21.Fung AL, Raine A. Peer victimization as a risk factor for schizotypal personality in childhood and adolescence. J Pers Disord. 2012;26(3):428–434. [DOI] [PubMed] [Google Scholar]
- 22.Siever LJ, Davis KL. The pathophysiology of schizophrenia disorders: perspectives from the spectrum. Am J Psychiatry. 2004;161(3):398–413. [DOI] [PubMed] [Google Scholar]
- 23.Gunderson JG, Siever LJ, Spaulding E. The search for a schizotype. Crossing the border again. Arch Gen Psychiatry. 1983;40(1):15–22. [DOI] [PubMed] [Google Scholar]
- 24.Torgersen S, Edvardsen J, Øien PA, et al. Schizotypal personality disorder inside and outside the schizophrenic spectrum. Schizophr Res. 2002;54(1-2):33–38. [DOI] [PubMed] [Google Scholar]
- 25.Calkins ME, Curtis CE, Grove WM, Iacono WG. Multiple dimensions of schizotypy in first degree biological relatives of schizophrenia patients. Schizophr Bull. 2004;30(2):317–325. [DOI] [PubMed] [Google Scholar]
- 26.Cohen AS, Emmerson LC, Mann MC, Forbes CB, Blanchard JJ. Schizotypal, schizoid and paranoid characteristics in the biological parents of social anhedonics. Psychiatry Res. 2010;178(1):79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarbox SI, Pogue-Geile MF. A multivariate perspective on schizotypy and familial association with schizophrenia: a review. Clin Psychol Rev. 2011;31(7):1169–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Webb CT, Levinson DF. Schizotypal and paranoid personality disorder in the relatives of patients with schizophrenia and affective disorders: a review. Schizophr Res. 1993;11(1):81–92. [DOI] [PubMed] [Google Scholar]
- 29.Kremen WS, Faraone SV, Toomey R, Seidman LJ, Tsuang MT. Sex differences in self-reported schizotypal traits in relatives of schizophrenic probands. Schizophr Res. 1998;34(1-2):27–37. [DOI] [PubMed] [Google Scholar]
- 30.Yaralian PS, Raine A, Lencz T, et al. Elevated levels of cognitive-perceptual deficits in individuals with a family history of schizophrenia spectrum disorders. Schizophr Res. 2000;46(1):57–63. [DOI] [PubMed] [Google Scholar]
- 31.Liu J, Richmond TS, Raine A, et al. The healthy brains and behavior study: objectives, design, recruitment, and population coverage. Int J Methods Psychiatr Res. 2013;22(3):204–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raine A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophr Bull. 1991;17(4):555–564. [DOI] [PubMed] [Google Scholar]
- 33.Raine A, Fung AL, Lam BY. Peer victimization partially mediates the schizotypy-aggression relationship in children and adolescents. Schizophr Bull. 2011;37(5):937–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ericson M, Tuvblad C, Raine A, Young-Wolff K, Baker LA. Heritability and longitudinal stability of schizotypal traits during adolescence. Behav Genet. 2011;41(4):499–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Straus MA. Measuring intra-family conflict and violence – the Conflict Tactics (CT) scales. J Marriage Fam. 1979;41(1):75–88. [Google Scholar]
- 36.Widom CS, Shepard RL. Accuracy of adult recollections of childhood victimization .1. Childhood physical abuse. Psychol Assess. 1996;8(4):412–421. [Google Scholar]
- 37.Andreasen NC, Rice J, Endicott J, Reich T, Coryell W. The family history approach to diagnosis. How useful is it? Arch Gen Psychiatry. 1986;43(5):421–429. [DOI] [PubMed] [Google Scholar]
- 38.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 39.Li G, Silverman JM, Smith CJ, et al. Validity of the family history method for identifying schizophrenia-related disorders. Psychiatry Res. 1997;70(1):39–48. [DOI] [PubMed] [Google Scholar]
- 40.Muthen LK, Muthen BO. Mplus User’s Guide. 6th ed. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 41.McDonald R. Test Theory: A Unified Treatment. Lawrence Earlbaum Associates. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- 42.Spearman C. The proof and measurement of association between two things. Am J Psychol. 1904;15:72–101. [PubMed] [Google Scholar]
- 43.Fonseca-Pedrero E, Debbané M, Ortuño-Sierra J, et al. The structure of schizotypal personality traits: a cross-national study. Psychol Med. 2018;48(3):451–462. [DOI] [PubMed] [Google Scholar]
- 44.Wong KK, Raine A. Peer problems and low self-esteem mediate the suspicious and non-suspicious schizotypy-reactive aggression relationship in children and adolescents. J Youth Adolesc. 2019;48(11):2241–2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Debbane M, Badoud D, Balanzin D, Eliez S. Broadly defined risk mental states during adolescence: disorganization mediates positive schizotypal expression. Schizophr Res. 2013;147(1):153–156. [DOI] [PubMed] [Google Scholar]
- 46.Meller T, Schmitt S, Stein F, et al. Associations of schizophrenia risk genes ZNF804A and CACNA1C with schizotypy and modulation of attention in healthy subjects. Schizophr Res. 2019;208:67–75. [DOI] [PubMed] [Google Scholar]
- 47.Velikonja T, Fisher HL, Mason O, Johnson S. Childhood trauma and schizotypy: a systematic literature review. Psychol Med. 2015;45(5):947–963. [DOI] [PubMed] [Google Scholar]
- 48.Raine A. Schizotypal personality: neurodevelopmental and psychosocial trajectories. Annu Rev Clin Psychol. 2006;2:291–326. [DOI] [PubMed] [Google Scholar]
- 49.Alemany S, Arias B, Aguilera M, et al. Childhood abuse, the BDNF-Val66Met polymorphism and adult psychotic-like experiences. Br J Psychiatry. 2011;199(1):38–42. [DOI] [PubMed] [Google Scholar]
- 50.Cristóbal-Narváez P, Sheinbaum T, Rosa A, et al. The interaction between childhood bullying and the FKBP5 gene on psychotic-like experiences and stress reactivity in real life. PLoS One. 2016;11(7):e0158809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Savitz J, van der Merwe L, Newman TK, Stein DJ, Ramesar R. Catechol-o-methyltransferase genotype and childhood trauma may interact to impact schizotypal personality traits. Behav Genet. 2010;40(3):415–423. [DOI] [PubMed] [Google Scholar]
- 52.Berenz EC, Amstadter AB, Aggen SH, et al. Childhood trauma and personality disorder criterion counts: a co-twin control analysis. J Abnorm Psychol. 2013;122(4):1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.