Sir,
Serotonin syndrome (SS) is a drug-induced clinical phenomenon caused by increased serotonergic activity in the central nervous system (CNS) and characterized by a triad of cognitive impairment, autonomic hyperactivity, and neuromuscular abnormalities.[1] Several serotonergic drugs are available in clinical practice, and they are used for numerous clinical indications.[1,2] So, there is a possibility that clinical symptoms of SS may mimic the clinical features of preexisting disease, for which serotonergic drugs have been started. Herein, we are reporting two cases of SS, which mimicked the underlying preexisting syndrome.
CASE 1
A 34-year-old man had a 3-year history of bipolar disorder. Three years ago, he had the first depressive episode that started gradually, characterized by irritability, diminished interest in routine activities, social withdrawal, loss of appetite, lack of energy, poor concentration, and insomnia. He had his first manic episode one year back. The patient was noncompliant for medications and had received various antidepressants and hypnotics over the last 3 years. Fluoxetine and amitriptyline had been started 2–3 weeks back for his recent relapse of depressive symptoms. The drugs were gradually titrated, amitriptyline from 10 mg to 25 mg, and fluoxetine from 10 mg to 20 mg. However, he developed increased activity, over-talkativeness, disturbed sleep, anger, agitation, and tremulousness all over the body over 5–7 days. He was brought to the emergency department in an agitated state. A diagnosis of an episode of mania was made and olanzapine was added. There was some improvement in over-talkativeness, anger, and sleep over 2 days. However, the tremulousness of the body got aggravated and the patient noted a difficulty in walking. The patient was referred to our neurology department. Physical examinations revealed tachycardia (116 beats/min), hypertension (158/96 mmHg), and diaphoresis. Neurological examinations revealed coarse tremor, hypertonia, brisk tendon reflex, inducible clonus at the ankles, flexor plantar response, and incoordination in all four limbs. The presence of neuromuscular hyperactivity (tremor, clonus, hyperreflexia) and a history of proserotonergic drugs ingestion raised a possibility of SS and the patient fulfilled the Hunter serotonin toxicity criteria.[1,3] Twelve mg loading dose of cyproheptadine was administered immediately, followed by 2 mg every 2 h. Fluoxetine and amitriptyline were discontinued. We continued olanzapine as it may be effective in SS.[1] Neuroimaging and biochemical parameters were normal. Agitation, tremor, and incoordination started to improve within 12 h and subsided completely in 3 days. Pulse and blood pressure returned to normal in 24 h. There were no diaphoresis and clonus after 24 h. Deep tendon reflex became normal in 48 h. The dose of cyproheptadine was rescheduled to 8 mg three times a day after 24 h. No physical abnormalities were detected on the fourth day. Cyproheptadine was withdrawn after 2 weeks. Olanzapine was continued for his bipolar disorder. Follow-up until 9 months was uneventful.
CASE 2
A 47-year-old male had a history of chronic obstructive lung disease (COPD). He had been prescribed an antibiotic (amoxicillin) and cough syrup (containing dextromethorphan) for his recent onset sore throat, cough, fever, and malaise. A combination of acetaminophen and tramadol was added for fever and myalgia. Although the patient got some relief in sore throat and cough, there was no improvement in fever and myalgia. His condition deteriorated with increasing fever and the development of new symptoms, like agitation, irritability, and disturbed sleep. He was brought to the emergency department. Physical examination revealed tachycardia (126/min), hypertension (156/98 mmHg), fever (102.6°F), and diaphoresis. A diagnosis of exacerbation of COPD was made. All investigations were normal and it included: Biochemical parameters, CSF examination, and neuroimaging. Serological testing for herpes simplex virus, human immunodeficiency virus, hepatitis B virus, malarial parasites, and Mycobacterium tuberculosis were negative. Initially, he was treated with intravenous fluids, antibiotics, and ondansetron. However, the patient did not respond to treatment and gradually became less communicative and drowsy. At this point, a neurology consultation was taken. We noted profuse sweating, tremor, generalized stiffness, hyperreflexia, and clonus at the ankles. As he fulfilled the Hunter criteria for SS, cyproheptadine was started in the dosages similar to the previous case. Dextromethorphan, tramadol, and ondansetron were discontinued. The patient became alert in 12 h. Fever and diaphoresis subsided in 24 h. Tremor, stiffness, and clonus disappeared in the 2 days. Follow-up until 3 months was uneventful.
DISCUSSION
SS is a highly under-diagnosed condition.[1] Manifestations may be wrongly attributed to another cause.[1] Physicians may not be aware of the different aspects of SS.[4] There are more than 50 drugs that may cause SS.[1,5] Several drugs with serotonergic properties are not classified or marketed as serotonergic agents (such as tramadol, ondansetron, dextromethorphan, and linezolid).[2] Physicians do not consider the possibility of SS with such drugs. Case-2 was not on classical serotonergic drugs. He was on dextromethorphan and tramadol for cough and bodily pain, and later on, injectable ondansetron was added. These all three drugs are serotonergic agents and may cause SS alone or in combination with others. SS is classically described in patients with psychiatric disorders. However, recent observations/case studies have expanded the underlying disorders where patients can develop SS.[5,6]
SS is an iatrogenic, drug-induced clinical syndrome. So, it usually develops over some preexisting disease or syndrome. Figure 1 explains the interrelation between the symptom complex of preexisting disease and symptom complex of SS. A few clinical features of the SS spectrum may overlap with the preexisting disease and it may appear as a deterioration of the preexisting disease. In some cases, the clinical features of SS may be entirely different from the pre-existing disease. However, even the development of any new symptoms in any particular condition is frequently labeled as aggravation or exacerbations of the underlying disease and they are frequently dismissed as a drug-related syndrome.
Figure 1.
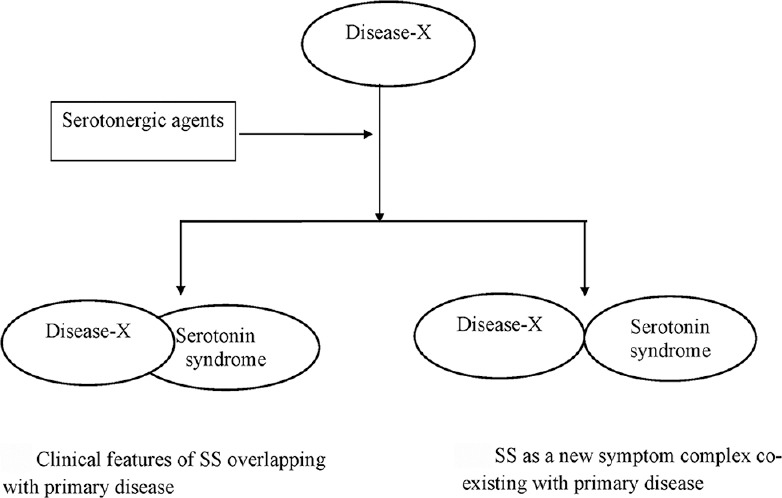
Interrelation between clinical features of serotonin syndrome with preexisting primary disease
The cognitive abnormalities of SS (insomnia, anxiety, agitation, etc.) may mimic the symptom complex of mania.[7] In case-1, the symptom complex of SS mimicked with the preexisting disease (manic phase of bipolar disorder). In case- 2, SS was initially diagnosed as the aggravation or complications of respiratory tract infection. We presume that fever in the early stage was because of exacerbation of COPD. However, later on, fever was the part of SS as it responded promptly to cyproheptadine. So, in these two cases, a few clinical features of SS were, in fact, the extension of the preexisting symptoms for which serotonergic drugs had been started. Such clinical situations may be noted in various other clinical scenarios. The most common indication to use serotonergic agents (SSRI) is a behavioral or psychiatric disorder.[1,2] Therefore, the cognitive impairment of SS may be overlapped with the preexisting psychiatric disorder. Nausea and vomiting are the part of autonomic manifestation in SS.[2,3] However, various antiemetic agents (including ondansetron, granisetron, and metoclopramide) may cause SS.[1] Linezolid is a serotonergic agent that is used for various bacterial infections (presenting as fever or febrile encephalopathy).[1] However, SS may have fever with or without encephalopathy.
Serotonergic neurons in the CNS modulate wakefulness, behavior, thermoregulation, muscular tone, sexual behavior, nociception, and voiding functions.[1] Peripheral serotonin receptors modulate vascular tone and gastrointestinal motility.[1] Therefore, a large number of symptoms may be present in SS and it may overlap with the preexisting clinical syndrome.
SS is mostly caused by an overdose of a single serotonergic agent or the concomitant use of 2 or more serotonergic agents. However, few cases have reported the SS caused by a normal or low dose of a single serotonergic agent. Our both patients received a therapeutic dose of serotonergic agents. Serotonergic drugs are metabolized by the cytochrome P450 family of enzymes. Impaired activity of cytochrome P450 enzymes may decrease the metabolism of certain serotonergic drugs, suggesting an increased tendency to develop SS. Such patients can be subjected for genetic polymorphism testing of cytochrome P450 by restriction fragment length polymorphism assay (RFLP).[8]
With this case reports, we suggest that any patient on any serotonergic agent, if develops any new symptoms, or there is an aggravation of the preexisting symptoms, should be examined for the presence of SS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112–20. doi: 10.1056/NEJMra041867. [DOI] [PubMed] [Google Scholar]
- 2.Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ. 2014;348:g1626. doi: 10.1136/bmj.g1626. [DOI] [PubMed] [Google Scholar]
- 3.Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The hunter serotonin toxicity criteria: Simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635–42. doi: 10.1093/qjmed/hcg109. [DOI] [PubMed] [Google Scholar]
- 4.Prakash S, Rathore C, Rana K. Knowledge, attitude, and practice (KAP) Study on Serotonin Syndrome Among Neuro Physicians. Ann Indian Acad Neurol. 2020;23:638–43. doi: 10.4103/aian.AIAN_603_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prakash S, Rathore C, Rana KK, Dave A, Joshi H, Patel J. Refining the clinical features of serotonin syndrome: A prospective observational study of 45 patients. Ann Indian Acad Neurol. 2019;22:52–60. doi: 10.4103/aian.AIAN_344_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedavally S, Fugate JE, Rabinstein AA. Serotonin syndrome in the intensive care unit: Clinical presentations and precipitating medications. Neurocrit Care. 2014;21:108–13. doi: 10.1007/s12028-013-9914-2. [DOI] [PubMed] [Google Scholar]
- 7.Isbister GK, Buckley NA, Whyte IM. Serotonin toxicity: A practical approach to diagnosis and treatment. Med J Aust. 2007;187:361–5. doi: 10.5694/j.1326-5377.2007.tb01282.x. [DOI] [PubMed] [Google Scholar]
- 8.Piatkov I, Mann G, Jones T, McLean M, Gunja N. Serotonin toxicity and cytochrome p450 poor metaboliser genotype patient case. J Investig Genomics. 2017;4:1–5. [Google Scholar]


