Abstract
Background
Residents may learn how to perform advance care planning (ACP) through informal curriculum. Task-based instructional designs and recent international consensus statements for ACP provide opportunities to explicitly train residents, but residents' needs are poorly understood.
Objective
We assessed residents' training needs in ACP at the Geneva University Hospitals in Geneva, Switzerland.
Methods
Qualitative data were collected and analyzed iteratively between December 2017 and September 2019. Transcripts were coded using both a deductive content analysis based on the 4-Component Instructional Design (4C/ID) model and an inductive thematic analysis.
Results
Out of 55 individuals contacted by email, 49 (89%) participated in 7 focus groups and 10 individual interviews, including 19 residents, 18 fellows and attending physicians, 4 nurses, 1 psychologist, 1 medical ethics consultant, 3 researchers, and 3 patients. Participants identified 3 tasks expected of residents (preparing, discussing, and documenting ACP) and discussed why training residents in ACP is complex. Participants described knowledge (eg, prognosis), skills (eg, clinical and ethical reasoning), and attitudes (eg, reflexivity) that residents need to become competent in ACP and identified needs for future training. In terms of the 4C/ID, these needs revolved around: (1) learning tasks (eg, workplace practice, simulated scenarios); (2) supportive information (eg, videotaped worked examples, cognitive feedback); (3) procedural information (eg, ACP pocket-sized information sheet, corrective feedback); and (4) part-task practice (eg, rehearsal of communication skills, simulation).
Conclusions
This study provides a comprehensive description of tasks and competencies to train residents in ACP.
Objectives
To assess residents' training needs in advance care planning using the 4-Component Instructional Design model.
Findings
Participants identified 3 tasks (preparing, discussing, documenting) and described a complex set of knowledge, skills, and attitudes expected of residents in advance care planning.
Limitations
The study took place in the Geneva University Hospitals (Switzerland) and focused primarily on physicians' perspectives.
Bottom Line
Educators in graduate medical education may use the proposed competency framework and skills hierarchy to develop innovative trainings in advance care planning.
Introduction
A recent international consensus defined advance care planning (ACP) as “the ability to enable individuals to define goals and preferences for future medical treatment and care, to discuss these goals and preferences with family and health care providers, and to record and review these preferences if appropriate.”1 ACP aims to ensure that people receive care that is medically appropriate and consistent with their personal values, which is an ethical imperative and improves patient safety and quality of care.1–4 Health care professionals need to be trained in ACP because they are often unprepared to discuss ACP with patients.5–7 Training is especially needed for resident physicians. In Switzerland, residents are typically patients' main interlocutors for ACP in the hospital setting and serve as liaison with other health care professionals caring for a patient.8–10 Given the absence of ACP curriculum standards, internationally and nationally, training in ACP has traditionally been implicit.11–14 Thus, residents' needs for training in ACP are poorly understood.
ACP is a complex process. It occurs within and outside of health care facilities, involves multiple stakeholders (patients, relatives, and health care professionals), and requires regular updates.1–4 ACP encompasses both oral and written communication. It includes goals of care discussions with patients and their relatives (and documentation of these discussions) and decisions about the end of life that can be written by patients (such as advance directives), physicians (such medical orders for scope of treatment and do-not attempt cardiopulmonary resuscitation orders [DNACPR]), and other members of the health care team (such as care plans).15,16 Given the complexity of ACP, scholars and policy makers have highlighted that training residents in ACP is critical.13,14,16 The recent international consensus on ACP1 provides a timely opportunity to develop such training.
Developing and implementing ACP training for residents, however, is difficult. First, the ACP-related tasks expected of residents in daily practice are ill-defined because ACP has traditionally been left to the informal curriculum.11–14 Research on related tasks has, to date, focused on training residents for breaking bad news, discussing CPR code status, or talking about advance care plans.14,17 Second, ACP requires a complex set of knowledge, skills, and attitudes5,18 that residents need to develop.11,14 Trainings published so far focused on specific aspects of ACP such as palliative care, end-of-life decision-making, or communication,11,12,14,19 but we still need a comprehensive and explicit ACP competency-based curriculum. Third, existing and limited ACP trainings were not informed by task-based instructional designs,20,21 though such designs may support integrated learning and transfer of complex competencies, such as ACP, into clinical practice. These considerations point to important research gaps that need to be filled to support residents in learning ACP. Furthermore, they suggest that innovative instructional design methods would be helpful in supporting residents' complex learning in ACP.
The aim of our study was to assess residents' training needs in ACP at the Geneva University Hospitals in Switzerland to inform the development of a training program. Specifically, we sought to address the following research questions: (1) What are the real-life tasks expected of residents when performing ACP with hospitalized patients? (2) What are the competencies needed by residents to perform these tasks? and (3) How can we support residents in the complex learning of these competencies?
Methods
Setting
This exploratory qualitative study took place at Geneva University Hospitals, in the French-speaking part of Switzerland, which includes 8 hospitals, with 1600 beds in 8 departments. There are approximately 750 residents in graduate medical education training in different specialties. Of note, in addition to Swiss residents, the hospitals have a long record of training residents from other European countries, especially from France, Belgium, Greece, Italy, and Portugal, which have different approaches to end-of-life decisions, DNACPR policies, and ACP.9,22
National guidelines support patients' empowerment and proxies' involvement in shared decision-making.10 Hospital guidelines recommend to discuss CPR with patients in goals of care discussions prior to document a DNACPR order, unless CPR is deemed futile near the end of life.10 However, previous studies conducted in Geneva have suggested that ACP is still underused and that residents experience difficulties with communication and decision-making during ACP.8–10
Conceptual Framework
We used the definition of ACP as a framework and included code status discussions about DNACPR orders, goals of care discussions, medical decisions regarding the overall treatment plan, and documentation in electronic health records.1,4 We focused on residents' training needs in ACP in the hospital.
We adopted the lens of task-centered learning, an approach underpinning several instructional design models, such as the first principles of instruction and the 4-Component Instructional Design (4C/ID).20,21 In this approach, learners progress in learning complete tasks that are increasingly complex. They receive tailored guidance that diminishes as they gain more experience, and they learn through real-world practice to support complex learning.23,24 Complex learning refers to “integrating knowledge, skills, and attitudes, coordinating qualitatively different constituent skills, and often transferring of what is learnt in the school or training setting to daily life and work setting.”24 Among the most renowned task-centered instructional design methods, we chose the 4C/ID because it offers practical guidance on 4 main components to be elaborated: (1) the learning tasks (authentic whole-task experiences organized in simple-to-complex classes with variability); (2) the supportive information (supporting the learning and performance of nonrecurrent skills, such as mental models and cognitive feedback); (3) the corrective or “just-in-time” information (supporting the learning and performance of recurrent skills, such as information displays and corrective feedback); and (4) the part-task practice (additional practice for selected recurrent skills to be automated).21,24 In addition, the 4C/ID allows for the involvement of all relevant stakeholders in needs assessment and to adapt training to the context.21,24
Data Collection
To illuminate residents' training needs in ACP, we used a qualitative research design to explore meanings and tasks associated with ACP in our setting.25 We conducted focus groups and individual interviews with the main stakeholders involved in ACP in various departments of the hospitals and with researchers in the field of ACP in the French-speaking part of Switzerland. We collected and analyzed the data iteratively between December 2017 and September 2019. As residents' training in ACP has traditionally been implicit,11–14 and as residents need to discuss ACP with the interprofessional health care team,8–10 our needs assessment included multiple stakeholders involved in ACP. We recruited participants using purposive sampling of residents, fellows, attending physicians, nurses, and other members of the health care team, researchers with expertise on ACP, and members of the “Patients-as-Partners” program (developed at the hospitals to promote patient advocacy in care, research, and health professions education).26 Involving members from the program in this study enabled us to elicit patient perspectives without interviewing hospitalized patients.
We conducted physician-only and interprofessional focus groups to understand the participants' perspectives on ACP, which enabled us to collect rich and contrasted data. However, focus groups require participants to feel at ease and speak freely with one another. To protect focus group dynamics, we conducted individual interviews with participants who had higher levels of seniority and with participants from the Patients-as-Partners program. We contacted participants by email with up to 2 reminders. Out of the 55 individuals we contacted, 51 agreed to participate, but 2 were not able to attend focus groups, resulting in 49 participants in this study (89%). We conducted focus groups in dedicated rooms close to participants' workplaces and interviews in the location of participants' choice, usually their offices. For both focus groups and interviews, we used a discussion guide based on the 4C/ID components (provided as online supplementary data).21,24,27 We designed questions following principles of cognitive task analysis: participants first described recent ACP experiences, then were asked to explore mental models and cognitive strategies by discussing or drawing diagrams on a paper board.28,29
Data Analysis
Three researchers who did not work with study participants conducted the interviews and focus groups—an intensivist in a geriatric emergency department with a background in public health and qualitative research (T.F.), a medical sociologist with experience in qualitative research (N.B.), and a research assistant in medical education (A.R.). We audiotaped and transcribed all focus group and interview data. We uploaded anonymized transcripts into Dedoose software for qualitative analysis (SocioCultural Research Consultants LLC, Manhattan Beach, CA).30 We coded the data using 2 complementary approaches: deductively using content analysis with an a priori coding framework to identify the components of the 4C/ID, and inductively using thematic analysis to unveil potential themes beyond the deductive coding framework.25 Two authors (T.F., N.B.) independently coded 2 interviews and 2 focus groups to develop an initial coding framework; 3 authors (T.F., N.B., A.R.) then coded the subsequent transcripts using this framework, which was consensually revised with the other researchers when new codes were integrated. The Standards for Reporting Qualitative Research guided our research design, data collection, and analysis.31
According to Swiss law, the Geneva Ethics Committee waived a complete review for this study. We provided participants with a letter summarizing the aim of the study and asked for their written consent to participate in the study.
Results
We conducted 7 focus groups (median duration 68 minutes, IQR 54–78) and 10 individual interviews (45 minutes, IQR 40–54). As Table 1 shows, we involved 49 participants: 19 residents, 18 senior physicians, 4 nurses, 1 psychologist, 1 medical ethics consultant, 3 researchers, and 3 patients. Table 1 displays the participants' characteristics. Table 2 displays the 3 themes and codes with selected quotations detailed in the following sections. In brief, participants described 3 tasks expected of residents and discussed why training residents in ACP is complex. They identified knowledge, skills, and attitudes that residents need to integrate to become competent in ACP. They described the current training and identified priority needs for future training.
Table 1.
Characteristics of Participants in Focus Groups and Interviews
| Participants | Residents (n = 19) | Senior Physicians (n = 18) | Allied Health Care Professionalsa (n = 6) | Researchers (n = 3) | Patients as Partners (n = 3) |
| Median age (IQR) | 28 (27–29.8) | 46 (39.8–51.5) | 48 (46–52) | 43 (42–46) | 62 (59–63.5) |
| Female-to-male ratio | 13:6 | 11:7 | 6:0 | 2:1 | 0:3 |
| Departments/unitsb Residents: rotations Senior physicians, allied health care professionals, researchers: work positions | General internal medicine (16) Rehabilitation (1) Geriatrics (7) Emergency (6) Palliative care (3) Intermediary care unit (2) Anesthesiology (1) | Internal medicine (7) Family medicine (4) Rehabilitation (1) Geriatrics (3) Palliative care (2) ICU (1) Emergency (1) Surgery (1) | Bioethics (1) Emergency (1) Hospital direction (1) Pain management (1) Palliative care (1) | Geriatric (2) Internal medicine (2) Palliative care (2) | Cardiology (1) Oncology (2) Oncology surgery (1) |
| Median years of experience (IQR) | 2 (1.25–4) | 19 (11.5–22.8) | 27 (25–31) | 16 (8–22) | N/A |
| Initial training in Switzerland ratioc | 11:8 | 15:3 | 3:3 | 2:1 | N/A |
| Other | France (3) Portugal (2) Czech Republic (1) Greece (1) Italy (1) | France (2) Belgium (1) | France (3) | Germany (1) | N/A |
| Involved in focus groups (FG) | 17 (3 FG) | 16 (2 FG) | 3 (1 FG) | 3 (1 FG) | 0 |
| Involved in individual interviews | 2 | 2 | 3 | 0 | 3 |
Abbreviation: N/A, not applicable.
Allied health care professionals included 4 nurses, 1 psychologist, and 1 medical ethics consultant.
Some participants practiced (rotations or work position) in more than one department/unit at the time of the study; patients as partners had been hospitalized and were followed up for chronic conditions in these departments.
MD for residents and physicians, Bachelor's for nurses, MSc for researchers.
Table 2.
Themes, Codes, Descriptions, and Representative Quotes
| Themes and Codes | Code Descriptions and Quotes |
| Theme 1: ACP Real-Life Tasks Expected of Residents | |
| Preparing | Gathering and evaluating available information And then residents further distinguish: Was this code status changed compared to the last hospitalization? Since a lot of patients are readmitted in the system […], I find it shocking to know that if code status was determined on a previous hospitalization, some people don't discuss it again at readmission. (A researcher, FG) That is what's really problematic to me, you constantly have to question yourself: “Is the code status still relevant or do we need to rediscuss it?” (A geriatrics resident, FG) |
| Discussing | With patients and/or relatives and with other caregivers A good example would be a 90-year-old patient with few comorbidities, but who tells us: “I don't want to be resuscitated.” We need to be able to hear them out, I mean, that's the whole point of having these discussions, especially when patients are doing well and can make decisions for themselves. (A geriatrics physician, Interview) I think first of all we need to discuss with the family, to get a better idea of the patient that we have in front of us. Because the acute problem could have completely changed the patient due to confusion. The patient may usually be a lot more autonomous and… I mean, we need to get an accurate picture… (A geriatrics resident, FG) We realized that surgeons, some surgeons, had a different understanding of it. When we labeled a patient NTBR, some surgeons thought it meant no surgery. (An internal medicine physician, FG) |
| Documenting | Recording goals of care discussions using appropriate formats As physicians, we tend to focus on some sort of checklist that we have in our mind, we want patients to answer yes or no to mechanical ventilation, to cardiopulmonary resuscitation, to intensive care, etc. (A geriatrics physician, Interview) If you want the code status to be systematically recorded, you need a protocol… I mean, how do we know whether or not residents will record it? I'm pretty sure that people started using NTBR because there was a checkbox about it somewhere. A mandatory checkbox. (An internal medicine physician and a surgeon, FG) |
| Tasks complexity | Determinants of complexity in ACP-related tasks as experienced by participants I think that the boundaries of what we need to do can be vague… I mean, I find it hard because sometimes we have to say: “Okay, this time I'm in charge, I get to make the decision since I'm the physician.” And other times, we have situations where the patients alone get to decide and there's nothing we can do about it. I struggle with that, especially when I don't know the patients very well. (An internal medicine resident, FG) Being respectful of patient choices does not mean telling them: “You're the patient so you're on your own to make decisions.” (A medical ethics consultant, Interview) When you start as a resident, you may have never worked in the ICU. That makes it difficult to tell patients what exactly could happen. I find it a little too hard for first-year residents. (An emergency medicine resident, FG) We've had young residents who had never experienced death, either in their family or through their clinical experience, and who had not had their ICU rotation yet… (A nurse, FG) |
| Patient safetya | Impact on patient safety or quality of care There's is a clear deficiency there: we write down decisions, but we don't explain why we made those decisions. When you're on call at 2 am and you see in the patient's file that there is a written order to withhold treatments, you have no idea whether it actually applies to your current situation. And that represents a major risk. (A physician, Interview) The tool to record [NTBR order], it's a box to tick, but when people do not speak the same language, it does not mean the same to them. This is what I was most concerned about… As he mentioned, NTBR in France means end-of-life care... And we have quite a lot of French physicians here at HUG, so it can get confusing! [Laughing] What a horrible misunderstanding! (An intensivist and an internal medicine physician, FG) I would say that in France, those questions did not come up because we used to call the intensivist saying: “I have a critical patient, what should we do?” They were the ones whether or not to admit patients to the ICU. Then, we would simply call relatives to tell them: “Here is the plan.” (An internal medicine resident, FG) |
| Theme 2: Residents' Needed Competencies in ACP | |
| Knowledge | Knowledge expected of residents in ACP, including prerequisite knowledge We are not good at evaluating patients' prognosis, we are not good at assessing their quality of life. Yet I think that these factors are crucial to having a good discussion. (A physician, FG) Some situations sometimes get labeled as palliative care, typically that would be a patient with terminal cancer. That is straightforward and we don't have problems with these. However, it can be challenging to detect that a patient with advanced dementia is also in a palliative care situation. (A geriatrics physician, Interview) |
| Skills | Skills expected of residents in ACP-related tasks, including recurrent and non-recurrent skills in the 4C/ID model I would tell residents: “Don't try to determine what type of doctor you are then always behave the same with all your patients. Your patients need you to adapt to them, to their needs, to the situation.” (A consultant, Interview) I tend to think that the priority is to have a conversation with the patient, to know what they expect us to do for them. In that way, I am not shocked when a patient tells me: “I am 80 years old, I am doing great, but I do not want to be resuscitated if anything happened to me.” (A resident, FG) I think you can influence a patient's answer by the way you frame the question. (A resident, Interview) |
| Attitudes | Attitudes expected of residents in ACP and goals of care, including empathy, respect, and reflexivity I could tell that there were 2 important dimensions… First, I guess, is the technical part: doctors need to have medical knowledge. And then, there's the dimension of being with another human being. They need to be able to have a human connection, to humanize the conversation… Getting the patients on board, involving them, making sure they remain positive and constructive despite possible bad news or diagnoses that are difficult for them … (A patient, Interview) I would say that one competency that is really needed is empathy. I mean, discussing ACP can be a violent experience for patients who get here, so we need to be able to have this conversation without making it too difficult for patients. (A geriatrics physician, Interview) Every caregiver must be self-reflective and wonder: how do I view medicine? How do I cope with…? I mean, there's a certain feeling of helplessness or failure... (A rehabilitation physician, Interview) If I ever got one of the diseases that I sometimes see in the neuro-ICU, even though I don't have any health issues at the moment, I think about it and there are things that I would refuse… But I've been saying that for years, I really should write down my advance directives [laughs]. (An ICU physician, FG) |
| Theme 3: Supporting Residents' Training in ACP | |
| Existing training | Description of existing training in ACP, including learning tasks in the 4C/ID model – You just learn it on the spot, you watch others do it and you learn from them, you decide what you like and what you don't like in what they do… – See one, do one, then you're in! [Laughs] (2 internal medicine residents, FG) – Can you remember… Has anyone observed you for that competency, and has anyone ever given you feedback on that? (Interviewer) – No, never! Never! [laughs] (2 geriatrics residents, FG-4) It's true that when I was in that situation, at the beginning, I wondered: “which words should I use? How am I going to explain that?” Well, I just looked it up in the literature and that's how I learnt. (A nurse, FG) |
| Training needs | Description of training needs, including suggestions for learning tasks and part-task practice in the 4C/ID model It would be useful to have an interactive hour, once every 3 months or so, where we could discuss how to… Where attendings could tell us: “Here's an idea for how to discuss code status with a patient.” (An internal medicine resident, FG) Interprofessional training is also super important because that's a good way to learn about what others can do. Because that's not always very obvious, and we can support each other play different roles at different times. When we need to decide, it obviously is physicians' responsibility. But for everything that comes before and after that decision, support, readjustments, we could perhaps find a way to better work hand in hand? (A nurse, FG) |
| Simulation | Simulation in existing training and suggestions for future training, including ideas for scenarios and assessment Simulated patients would be great. But the problem is that if you want to train 90 residents with simulated patients, you'll need an army of SPs! And I don't think that residents are that bad at role plays, so they could easily just put themselves in their patients' shoes to learn how to have code status discussions. (An internal medicine physician, FG) Developing simulations with simulated patients would be great. However, practically speaking, it means that you're slowly training a small number of people. I like (Physician)'s idea of making everyone watch a video of an intensivist talking about code status with their patient, that would be easy to do. (An ICU physician, FG) |
Abbreviations: ACP, advance care planning; FG, focus group; NTBR, not to be resuscitated; 4C/ID, 4-Component Instructional Design; AD, advance directives; DNACPR, do not attempt cardiopulmonary resuscitation.
Codes identified inductively through thematic analysis.
Real-Life Tasks Expected of Residents
We identified 3 main task classes related to ACP for residents in the hospital: preparing, discussing, and documenting ACP. Preparing ACP involved gathering and evaluating prior ACP information (eg, advance directives or surrogate decision-maker) from diverse locations (eg, patient medical files at the hospital, nursing home, or family medicine physician office). It required residents to distinguish between simple and complex ACP situations, to determine the urgency, and to identify individuals to involve in the discussion. Discussing ACP involved different tasks depending on who participated in the conversation. Residents had to inform patients and their relatives about diagnosis and prognosis, explore end-of-life preferences, and ideally agree on realistic goals of care. They also had to discuss complex situations with their supervisors and other members of the health care team, such as primary care providers, nurses, or psychologists. Documenting ACP involved filling out a form in patients' electronic health records. At the time of the study, this meant checking 2 boxes (CPR/DNACPR order, discussed with patient “Yes/No”) and documenting the goals of care in a free text box. Supervisors stressed that documenting the form upon admitting a patient and updating it throughout hospitalization were important for patient safety and were elements of a physician's ethical duty to respect patient preferences. These tasks ranged from simple to complex, depending on a series of factors detailed in Table 3. The perceived level of complexity influenced the way residents reasoned, communicated, and made decisions. In simple situations (eg, elderly patients with dementia for whom palliative care was already initiated), residents tended to determine patients' code status by themselves with no or limited discussion with the patients and to leave what had previously been documented unchanged in the medical record. In contrast, in complex situations with a potential risk to patient safety (eg, older patients with life-threatening emergencies for whom intensive care may not be beneficial or even harmful), residents tended to work more collaboratively with patients and relatives and to call for help from senior physicians or palliative care consultants.
Table 3.
Advance Care Planning in Geneva University Hospitals: Tasks Expected of Residents and Their Determinants of Complexity
| Tasks | Factors of Complexity | Easy | Intermediate | Complex |
(1) Preparing ACP This includes:
|
Patient's medical file | Patient with past medical file:
|
Patient with past medical file:
|
New patient, no medical file |
| DNACPR orders/goals of care | Prior DNACPR orders/goals of care, clear + recent | No prior DNACPR orders/goals of care | Prior DNACPR orders/goals of care + inconsistent information | |
| Advance directives | Clear + recent AD | Clear but outdated | Unclear or inconsistent with other ACP sources | |
| Outcome and prognosis: level of uncertainty | Good outcome clearly expected (eg, young patient with no comorbidity admitted for planned surgery) Comorbidities with expected trajectory of care Poor outcome clearly expected (eg, elderly patient with dementia in terminal palliative care) Evidence available (eg, prognostic score, epidemiological data) | Comorbidities: none or few Conflicting evidence | Outcome: unclear No or conflicting evidence regarding the benefit of intensive care with a risk of futile care and delayed palliative care | |
| (2) Discussing ACP This includes: (a) Goals of care discussion with one patient | Time available to discuss | Hours to days | Minutes to hours | No time, or within minutes |
| Level of emergency | No emergency | Potentially life-threatening | Life-threatening emergency | |
| Cognitive functions | No impairment | Mild impairment | Unknown | |
| Patient's preferences regarding end of life | Clear preferences Preferences consistent with comorbidities and prognosis | Unclear preferences or does not know | Clear preferences, but considered inconsistent by physicians (eg, CPR preference viewed as futile) | |
| Prior ACP discussions | Prior discussions Patient aware of ACP, ready and willing to discuss | No prior discussion | ||
| Language and culture | No language barrier No cultural barrier | No language barrier Cultural barrier | Language barrier + cultural barrier with the risk of divergent views between patients' preferences and caregivers' recommendations | |
| (b) Goals of care discussion with relative(s) for patients unable to communicate (eg, dementia or confusion) | Relationship | Spouse, sibling Living daily with the patient | Family member or friend, with regular contacts | Loose relationship, no regular or close contact |
| Number of relatives Level of agreement | One legal surrogate or one relative | Several relatives agreeing on patient's end-of-life preference | No relative Several relatives with conflict | |
| Awareness of patient's end-of-life preferences | Aware and clear, based on opened and explicit discussions on end-of-life topics | Aware but unclear assumptions based on indirect information (eg, meaning of life, values, projects) | Unaware No prior discussions No indirect information | |
| Language and culture | No language barrier No cultural barrier | No language barrier Cultural barrier | Language barrier + Cultural barrier | |
| (c) Goals of care discussion with other(s) health care professional(s) More senior physician (eg, fellow, attending), consultant (eg, surgeon), family medicine physician, nurse, other professional(s) | Setting | In-hospital: same team Ambulatory care: one network Shared electronic medical file | In-hospital: different teams Ambulatory: no structured network for collaboration | In-hospital or ambulatory: lack of collaboration, conflicts No shared patient medical file associated with communication gap during transition of care |
| Timing of discussion Interlocutor reachable | During regular working hours Easily reachable | Off-hours Not reachable | ||
| Communication between resident and other professionals | Face-to-face communication Standardized communication (eg, ISBAR) | Communication by phone | Unstructured communication Conflict or authority gradient | |
| Interprofessional collaboration | Interprofessional meetings Involvement of palliative care team | No voice for nurses | Intra-team conflict | |
| (3) Documenting ACP | Hospital policy and guidelines | Computerized medical file Dedicated space to record ACP Local guidelines defining terms, acronyms, and concepts for DNACPR orders and goals of care | Ambiguous interpretation of DNACPR acronym Lack of standardized terms to document goals of care No dedicated space to document patients' narratives | |
| Advance directives | Standardized acronyms/terms Boxes and text format | Unclear acronyms and terms with potential risk for patient safety (eg, ambiguous goals of care associated with futile treatments) Boxes to be checked and that lack narrative information regarding patients' values and preferences |
Abbreviations: ACP, advance care planning; AD, advance directives; DNACPR, do not attempt cardiopulmonary resuscitation; ISBAR, Identity, Situation, Background, Assessment, Recommendation (mnemonics for handover); NTBR, not to be resuscitated (at the time of the study, this acronym was used instead of DNACPR in the Geneva University Hospitals).
Residents' Competencies in ACP
Competencies for residents to discuss ACP with hospitalized patients included knowledge, skills, and attitudes (Box). Residents needed knowledge about the legal and ethical principles used for ACP in Switzerland, which was often new to foreign residents. In addition, residents had to grapple with uncertainty and unclear information as to patients' status and prognosis. Residents also mentioned they needed deeper knowledge in palliative care, especially in life-threatening situations.
Box Advance Care Planning: Residents' Needed Competencies
Knowledge
-
▪
Ethical principles
-
○
Autonomy and decision-making, futility
-
○
-
▪
End-of-life legal framework in the context of Switzerland
-
○
Advance directives, surrogate appointment, assisted suicide
-
○
-
▪
Advance care planning
-
○
Terminology and acronyms, definition, and conceptual framework
-
○
International and Swiss consensus statements
-
○
Difference between ACP, AD, and DNACPR orders
-
○
-
▪
Prognosis and benefit/risks in:
-
○
Resuscitation for in-hospital cardiac arrest
-
○
Frequent ICU admissions (eg, acute respiratory failure, septic shock)
-
○
End-of-life course of frequent chronic diseases (eg, dementia, COPD, CKD)
-
○
-
▪
Evidence-based palliative care
-
○
Best practices in goals of care conversations
-
○
Palliative options in life-threatening emergencies (eg, pain control, sedation)
-
○
Skills
-
▪
Reasoning skills
-
○
Assessing patient's ability to discuss ACP (eg, cognitive decline or confusion)
-
○
Integrating clinical and ethical reasoning to justify decisions
-
○
Making decisions regarding when and with whom to discuss ACP
-
○
-
▪
Communication skills, with patients and relatives
-
○
Using a structured yet flexible format
-
○
Tailoring the information and avoiding jargon
-
○
Listening and identifying patients' needs and cues
-
○
Avoiding influencing patients' decisions
-
○
-
▪
Communication skills, with colleagues and interprofessional team
-
○
Using a structured format for oral handovers (eg, ISBAR)
-
○
Using appropriately DNACPR orders and goals of care forms in electronic health records
-
○
Handling conflicts
-
○
Attitudes
-
▪
Empathy
-
▪
Respect patient's willingness to be involved or not in the decision-making process
-
▪
Intercultural open-mindedness
-
▪
Reflexivity regarding
-
○
Self-perceived confidence and competency to proceed without supervision
-
○
Personal values and experience regarding disease, handicap, and end of life
-
○
The potential biases in goals of care discussions
-
○
Emotional impact of ACP
-
○
Abbreviations: ACP, advance care planning; AD, advance directives; DNACPR, do not attempt cardiopulmonary resuscitation; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; ISBAR, identity, situation, background, assessment, recommendation (mnemonics for handover).
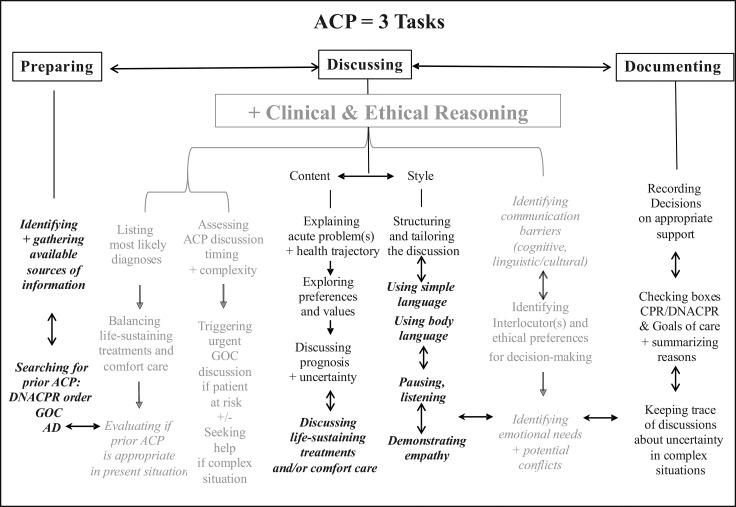
In terms of skills, residents needed skills in reasoning and communication (Box and Figure). Residents needed clinical reasoning skills to evaluate whether patients were able to have a conversation and make decisions, to establish diagnosis and prognosis, and to prescribe treatments. They also needed ethical reasoning skills to assess the extent to which patients or relatives wanted to be involved in ACP. Intertwined with clinical and ethical reasoning, residents needed decision-making skills to evaluate existing prior ACP, to initiate new discussions when needed, and to know when to refer to supervisors if the situation became too complex, for example with older patients with uncertain prognosis in life-threatening emergency conditions. Residents needed excellent communication skills to address critical points with patients and relatives (eg, diagnosis, prognosis, treatments, and patients' preference), to listen to patient needs, and to demonstrate empathy.
Figure.
Skills Hierarchy of Resident Competencies for Advance Care Planning
Abbreviations: ACP, Advance care planning; AD, advance directives; DNACPR, do not attempt cardiopulmonary resuscitation; GOC, goals of care.
Note: Black color: 3 ACP-related tasks; gray color: dual clinical and ethical reasoning skills; Roman font: non-recurrent skills; italic and bold: recurrent skills; double arrows: simultaneous relationship; horizontal simple arrow: temporal relationship; vertical simple arrow: prerequisite relationship.
In terms of attitudes, residents needed be empathetic and tactful. They were also expected to be reflexive of how their own opinions and values influenced their approach to ACP and end-of-life care, as these represent sensitive topics. During focus groups, we noticed that participants often used humor when discussing these topics, suggesting their emotional involvement.
Supporting Residents' Training in ACP
Participants identified developing competencies required for ACP as important learning objectives, although they described this as an educational challenge. Residents in our study reported learning ACP by shadowing more senior physicians. They also regretted not receiving any feedback from supervisors on how they managed ACP, which made them feel uncertain about what needed improvement. Some residents mentioned reading about ACP in their free time and attending workshops organized by the institution (eg, on breaking bad news, ethics).
All participants believed that residents' training in ACP was critical, particularly as residents were often left in charge of ACP even though most experienced participants acknowledged that it had taken them years to feel confident in managing complex ACP situations. Participants also noted that there were important barriers to overcome to develop residents' training in ACP. These barriers included limited time for learning, the high number of residents, the short duration of rotations, and the limited training of supervisors themselves. However, participants also believed that ACP training could be integrated into existing learning activities. Such activities included a patient-physician relationship module at the undergraduate level, a role-play for internal medicine residents at the postgraduate level, and a workshop on clinical supervision at the faculty development level. Another suggestion was to embed an introduction to ACP within an existing e-learning module on CPR, compulsory for every new health care professional at the hospitals.
In terms of educational strategies, many participants noted that simulation and role-play may be fruitful. In particular, they imagined a e-learning module with videotaped simulated goals of care discussions prior to a 2-hour practice session with role-play.
Discussion
This qualitative study increased our understanding of current practices and training needs for residents in ACP; it revealed that residents perform 3 main task classes regarding ACP, namely preparing, discussing, and documenting ACP. To perform these tasks, this study showed that residents needed complex sets of skills and attitudes that include clinical and ethical reasoning. Finally, this study outlined suggestions for designing an innovative training in ACP using a whole-task instructional design.
Our proposed ACP skills hierarchy diagram (Figure) provides a hierarchical description of all constituent skills and their relationships24 and fits well in competency-based residency programs endorsed worldwide, notably in Canada, the United States, and Switzerland.32–34 This visual representation of our skills hierarchy can be used by instructional designers to guide the development of learning tasks, as well as by clinical supervisors and residents to share a common mental model of the skills to be integrated in the complex learning of ACP.20,21 Our finding that residents need to acquire knowledge on disease prognosis and palliative care management is consistent with 2 reviews of the literature.11,14 This need can be addressed through integration of palliative medicine and geriatrics competencies into postgraduate curricula.35 Additionally, our skills hierarchy is helpful for including clinical and ethical reasoning into ACP postgraduate training.11,36,37 In line with previous research,38,39 our study shows that residents often struggle to integrate clinical and ethical reasoning because they tend to be taught in isolation. Research has suggested that learning ethical and clinical reasoning skills in a more integrated way requires a shared theoretical framework, assuming a balance between deductive (top down) and inductive (bottom up) reasoning.40
Residents and senior physicians reported experiences of learning ACP-related tasks on the job through role modeling and informal curriculum rather than through formal trainings. This echoes the literature in Switzerland and in other settings.8,9,14 Participants suggested that simulated role-play and clinical supervision could be starting points to improve the training, and that e-learning modules, journal clubs, and ACP guidelines or pocket-sized information sheets may be helpful. Some of these strategies are already described in the literature.19,41 However, they are typically used during one-time training and focus on tasks at a single point in time, such as code status discussions, goals of care conversations, or breaking bad news.17,42,43 We suggest that a whole-task approach is more consistent with the most recent approach to ACP, which promotes the integration of discussions and documentation of goals of care regularly updated along the ACP process.5,15,16 In addition, a whole-task instructional design is expected to support residents' complex learning in ACP.20,21 We provide suggestions for how to develop such an ACP training for learners in graduate medical education using the 4C/ID framework in the online supplementary data.
This study has several limitations. Due to time and budget constraints, we were limited in our ability to triangulate data collection methods. We conducted focus groups and semistructured interviews because we wanted to explore participants' perceptions of and experiences with ACP, but we did not conduct field observations.31 Our understanding of participants' behaviors and interactions during ACP-related tasks was limited from what they described, which may be different from what they actually do in real life. Another limitation of this study is that it focused primarily on physicians' perspectives. We attempted to involve patients' perspectives by interviewing members of the Patients-as-Partners program, but we still have limited insights into patients' needs, which may differ from professionals' needs and be relevant to residents' training in ACP.43 Similarly, although we included one interprofessional focus group, we are still limited in understanding other health care professionals' potential role in training residents in ACP.44
Future research could delve deeper into how residents perform ACP with patients by using ethnographic observations, which would allow to address underexplored phenomena in ACP such as barriers to patients' involvement in the decision-making process.42,43,45 Furthermore, as we undertook this study to develop a program to train residents in ACP, we will conduct further research on the implementation and evaluation of the program.
Conclusions
In line with recent international consensus statements on ACP, this study provided a comprehensive description of tasks and competencies to train residents in ACP. It proposed a competency framework and a skills hierarchy for educators in graduate medical education to develop innovative trainings in ACP using the 4C/ID model.
Supplementary Material
Acknowledgments
The authors would like to thank all research participants for their involvement in the focus groups and individual interviews; members of the UDREM at the University of Geneva School of Medicine, members of the Interprofessional Simulation Center, and members of the Institute of Primary Care at the Geneva University Hospitals for their help in designing and conducting the study; the academic and administrative staff of the Master of Health Profession Education program at Maastricht University and the Association for Medical Education in Europe for a research scholarship granted to Dr Fassier; and the Swiss National Science Foundation for its Postdoctoral Fellowship grant for Dr Bochatay.
Footnotes
Funding: Dr Fassier was awarded a research scholarship from the Association for Medical Education in Europe, and Dr Bochatay was supported by the Swiss National Science Foundation Postdoctoral Fellowship under grant P2GEP1_184139.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–e551. doi: 10.1016/S1470-2045(17)30582-X. [DOI] [PubMed] [Google Scholar]
- 2.Heyland DK, Ilan R, Jiang X, You JJ, Dodek P. The prevalence of medical error related to end-of-life communication in Canadian hospitals: results of a multicentre observational study. BMJ Qual Saf. 2016;25(9):671–679. doi: 10.1136/bmjqs-2015-004567. [DOI] [PubMed] [Google Scholar]
- 3.Allison TA, Sudore RL. Disregard of patients' preferences is a medical error: comment on “failure to engage hospitalized elderly patients and their families in advance care planning.”. JAMA Intern Med. 2013;173(9):787. doi: 10.1001/jamainternmed.2013.203. [DOI] [PubMed] [Google Scholar]
- 4.Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage. 2017;53(5):821–832.e1. doi: 10.1016/j.jpainsymman.2016.12.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994. doi: 10.1001/jamainternmed.2014.5271. [DOI] [PubMed] [Google Scholar]
- 6.Sudore RL, Heyland DK, Barnes DE, et al. Measuring advance care planning: optimizing the advance care planning engagement survey. J Pain Symptom Manage. 2017;53(4):669–681.e8. doi: 10.1016/j.jpainsymman.2016.10.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fassier T, Valour E, Colin C, Danet F. Who am I to decide whether this person is to die today? Physicians' life-or-death decisions for elderly critically ill patients at the emergency department–ICU interface: a qualitative study. Ann Emerg Med. 2016;68(1):28–39.e3. doi: 10.1016/j.annemergmed.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 8.Pautex S, Gamondi C, Philippin Y, et al. Advance directives and end-of-life decisions in Switzerland: role of patients, relatives and health professionals. BMJ Support Palliat Care. 2018;8(4):475–484. doi: 10.1136/bmjspcare-2014-000730. [DOI] [PubMed] [Google Scholar]
- 9.Becerra M, Hurst SA, Junod Perron N, Cochet S, Elger BS. ‘Do not attempt resuscitation' and ‘cardiopulmonary resuscitation' in an inpatient setting: factors influencing physicians' decisions in Switzerland. Gerontology. 2011;57(5):414–421. doi: 10.1159/000319422. [DOI] [PubMed] [Google Scholar]
- 10.Hurst SA, Becerra M, Perrier A, Perron NJ, Cochet S, Elger B. Including patients in resuscitation decisions in Switzerland: from doing more to doing better. J Med Ethics. 2013;39(3):158–165. doi: 10.1136/medethics-2012-100699. [DOI] [PubMed] [Google Scholar]
- 11.Gorman TE, Ahern SP, Wiseman J, Skrobik Y. Residents end-of-life decision making with adult hospitalized patients: a review of the literature. Acad Med. 2005;80(7):622–633. doi: 10.1097/00001888-200507000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Redman M, Pearce J, Gajebasia S, Johnson M, Finn G. Care of the dying: a qualitative exploration of foundation year doctors' experiences. Med Educ. 2017;51(10):1025–1036. doi: 10.1111/medu.13358. [DOI] [PubMed] [Google Scholar]
- 13.Levy D, Strand J, McMahon GT. Evaluating residents' readiness to elicit advance care plans. J Grad Med Educ. 2015;7(3):364–368. doi: 10.4300/JGME-D-14-00542.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kottewar SA, Bearelly D, Bearelly S, Johnson ED, Fleming DA. Residents' end-of-life training experience: a literature review of interventions. J Palliat Med. 2014;17(6):725–732. doi: 10.1089/jpm.2013.0353. [DOI] [PubMed] [Google Scholar]
- 15.Sinuff T, Dodek P, You JJ, et al. Improving End-of-Life Communication and Decision Making: The Development of a Conceptual Framework and Quality Indicators J Pain Symptom Manage . 20154961070–1080. 10.1016/j.jpainsymman.2014.12.007 [DOI] [PubMed] [Google Scholar]
- 16.Fritz Z, Slowther A-M, Perkins GD. Resuscitation policy should focus on the patient, not the decision. BMJ. 2017 doi: 10.1136/bmj.j813. j813. [DOI] [PMC free article] [PubMed]
- 17.Szmuilowicz E, Neely KJ, Sharma RK, Cohen ER, McGaghie WC, Wayne DB. Improving residents' code status discussion skills: a randomized trial. J Palliat Med. 2012;15(7):768–774. doi: 10.1089/jpm.2011.0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mullick A, Martin J, Sallnow L. An introduction to advance care planning in practice. BMJ. 2013 doi: 10.1136/bmj.f6064. 347:f6064. [DOI] [PubMed]
- 19.Chung H-O, Oczkowski SJW, Hanvey L, Mbuagbaw L, You JJ. Educational interventions to train healthcare professionals in end-of-life communication: a systematic review and meta-analysis. BMC Med Educ. 2016;16(1):131. doi: 10.1186/s12909-016-0653-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vandewaetere M, Manhaeve D, Aertgeerts B, Clarebout G, Van Merriënboer JJG, Roex A. 4C/ID in medical education: how to design an educational program based on whole-task learning: AMEE Guide No. 93. Med Teach. 2015;37(1):4–20. doi: 10.3109/0142159X.2014.928407. [DOI] [PubMed] [Google Scholar]
- 21.Dolmans DHJM, Wolfhagen IHAP, Van Merriënboer JJG. Twelve tips for implementing whole-task curricula: how to make it work. Med Teach. 2013;35(10):801–805. doi: 10.3109/0142159X.2013.799640. [DOI] [PubMed] [Google Scholar]
- 22.Gysels M, Evans N, Meñaca A, et al. Culture and end of life care: a scoping exercise in seven European countries. PLoS ONE. 2012;7(4):e34188. doi: 10.1371/journal.pone.0034188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Francom GM, Gardner J. What is task-centered learning? TechTrends. 2014;58(5):27–35. doi: 10.1007/s11528-014-0784-z. [DOI] [Google Scholar]
- 24.Van Merriënboer JJG, Kirschner PA. Ten Steps to Complex Learning A Systematic Approach to FourComponent Instructional Design 2nd ed. London, UK: Routledge; 2012. [Google Scholar]
- 25.Braun V, Clarke V. Successful Qualitative Research A Practical Guide for Beginners. New York, NY: SAGE; 2013. [Google Scholar]
- 26.Nestel D, Kneebone R. Perspective: authentic patient perspectives in simulations for procedural and surgical skills. Acad Med. 2010;85(5):889–893. doi: 10.1097/ACM.0b013e3181d749ac. [DOI] [PubMed] [Google Scholar]
- 27.Stalmeijer RE, McNaughton N, Van Mook WNKA. Using focus groups in medical education research: AMEE Guide No. 91. Med Teach. 2014;36(11):923–939. doi: 10.3109/0142159X.2014.917165. [DOI] [PubMed] [Google Scholar]
- 28.Dionne-Odom JN, Willis DG, Bakitas M, Crandall B, Grace PJ. Conceptualizing surrogate decision making at end of life in the intensive care unit using cognitive task analysis. Nursing Outlook. 2015;63(3):331–340. doi: 10.1016/j.outlook.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schubert CC, Denmark TK, Crandall B, Grome A, Pappas J. Characterizing novice-expert differences in macrocognition: an exploratory study of cognitive work in the emergency department. Ann Emerg Med. 2013;61(1):96–109. doi: 10.1016/j.annemergmed.2012.08.034. [DOI] [PubMed] [Google Scholar]
- 30.Dedoose. Qualitative Data Analysis Software. 2021 https://www.dedoose.com/ Accessed April 20.
- 31.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 32.CanMEDS. Frank JR, Snell L, Sherbino J, Boucher A. CanMEDS 2015 Physician Competency Framework. Royal College of Physicians and Surgeons of Canada. 2021 http://www.canmeds.royalcollege.ca/en/framework Accessed April 20.
- 33.ISFM. Institut suisse pour la formation médicale postgraduée et continue. 2021 https://www.fmh.ch/fr/formation-isfm/formation-postgraduee.html Accessed April 20.
- 34.Frank JR, Snell L, Englander R, Holmboe ES, on behalf of the ICBME Collaborators Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568–573. doi: 10.1080/0142159X.2017.1315069. [DOI] [PubMed] [Google Scholar]
- 35.Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17(3):316–324. doi: 10.1111/j.1553-2712.2010.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaldjian LC, Weir RF, Duffy TP. A clinician's approach to clinical ethical reasoning. J Gen Intern Med. 2005;20(3):306–311. doi: 10.1111/j.1525-1497.2005.40204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaldjian LC. Teaching practical wisdom in medicine through clinical judgement, goals of care, and ethical reasoning. J Med Ethics. 2010;36(9):558–562. doi: 10.1136/jme.2009.035295. [DOI] [PubMed] [Google Scholar]
- 38.Eckles RE, Meslin EM, Gaffney M, Helft PR. Medical ethics education: where are we? Where should we be going? A review. Acad Med. 2005;80(12):1143–1152. doi: 10.1097/00001888-200512000-00020. [DOI] [PubMed] [Google Scholar]
- 39.Doukas DJ, Kirch DG, Brigham TP, et al. Transforming educational accountability in medical ethics and humanities education toward professionalism. Acad Med. 2015;90(6):738–743. doi: 10.1097/ACM.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 40.Edwards I, Delany C. Clinical Reasoning in the Health Professions 3rd ed. Amsterdam, Netherlands: Elsevier; 2008. Ethical reasoning; pp. 279–289. [Google Scholar]
- 41.Roze des Ordons A, Kassam A, Simon J. Goals of care conversation teaching in residency—a cross-sectional survey of postgraduate program directors. BMC Med Educ. 2017;17(1):6. doi: 10.1186/s12909-016-0839-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shah K, Swinton M, You JJ. Barriers and facilitators for goals of care discussions between residents and hospitalised patients. Postgrad Med J. 2017;93(1097):127–132. doi: 10.1136/postgradmedj-2016-133951. [DOI] [PubMed] [Google Scholar]
- 43.You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015;175(4):549. doi: 10.1001/jamainternmed.2014.7732. [DOI] [PubMed] [Google Scholar]
- 44.Vedel I, Ghadi V, Lapointe L, Routelous C, Aegerter P, Guirimand F. Patients', family caregivers', and professionals' perspectives on quality of palliative care: a qualitative study. Palliat Med. 2014;28(9):1128–1138. doi: 10.1177/0269216314532154. [DOI] [PubMed] [Google Scholar]
- 45.Roze des Ordons AL, Sharma N, Heyland DK, You JJ. Strategies for effective goals of care discussions and decision-making: perspectives from a multi-centre survey of Canadian hospital-based healthcare providers. BMC Palliat Care. 2015;14(1):38. doi: 10.1186/s12904-015-0035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.