Abstract
Hidradenitis suppurativa (HS) is a chronic and often debilitating inflammatory condition characterized by frequent nodules, abscesses, sinus tracts, and scars impacting the intertriginous areas. Many patients with HS often report limited treatment success and symptom coverage with conventional therapies. Recent studies have reported the widespread use of complementary and alternative medicine (CAM) among patients with HS. In this study, our aim was to examine current physician practice patterns, opinions, and comfort with recommending CAM. Our results indicate that provider comfort and opinions on CAM varied based on the provider’s experiences, demographics, and the CAM modality itself. Overall, nearly two-thirds (n=30, 61.2%) of respondents agreed that CAM and conventional medicine were more effective together than either alone. Meanwhile, 44.9% (n=22) of respondents routinely recommend CAM while 64.6% (n=31) of respondents reported that they are routinely asked about CAM. The majority (n=41, 83.7%) of respondents indicated a lack of scientific evidence in the medical literature as a barrier to recommending CAM along with efficacy concerns (n=34, 69.4%) and ability to recommend reputable CAM products (n=32, 65.3%) and practitioners (n=32, 65.3%). Future investigations are warranted to establish a better understanding of the efficacy and benefit of CAM methods in conjunction with conventional methods.
Keywords: hidradenitis suppurativa, complementary medicine, alternative medicine, physician perspectives, survey
Introduction
Hidradenitis suppurativa (HS) is an often-debilitating disease characterized by painful abscesses, nodules and sinus tracts. Conventional treatments have limited success in managing HS symptoms, and a recent survey found that 84.2% of HS patients reported using complementary and alternative medicine (CAM) for their HS.1 The National Center for Complementary and Integrative Health (NCCIH) defines CAM as health practices that are utilized outside of current methods of conventional medicine or that may have origins outside of the usual Western practice.2 The most reported CAM methods utilized by HS patients include dietary changes, turmeric, and magnesium sulfate (Epsom salt) bath followed by dietary supplements including zinc, vitamin D, vitamin C, vitamin B12, and fish oil.1 The North American clinical management guidelines for HS list zinc, vitamin D, brewer’s yeast avoidance, and dairy avoidance as potential alternative interventions, but with insufficient evidence to support routine use.3 Despite widespread patient utilization of CAM, there remains a paucity of literature examining healthcare provider opinions of CAM for HS. We aimed to examine physician practice patterns, comfort, and opinion in recommending CAM.
Materials and Methods
An anonymous e-questionnaire was distributed to HS provider listservs sponsored by the United States and Canadian HS Foundations between March-May 2020 using RedCap. CAM methods reported in the previously noted survey study of CAM usage among HS patients were divided into five categories (e.g. mind/body interventions, bathing techniques, supplement-based practices, cultural/traditional medicine, and dietary modifications) and comfort levels in each group were assessed using Likert scale questions.1 Provider opinions of CAM was also assessed using Likert scale responses to various statements. Associations between provider characteristics and Likert scale questions were assessed using Spearman’s correlation coefficient (rs). P-values<0.05 were considered statistically significant. Statistical analyses were performed using SPSS V25 (Armonk, NY).
Results
Forty-nine physician respondents were included (mean age, 45.5 [SD=12.5] years, 27 males [55.1%]). The majority (n=45, 91.8%) were dermatologists, four (8.2%) were surgeons. Forty-four (89.8%) were attending dermatologists, three (6.1%) were residents; two (4.1%) unspecified. On average, participants had 12.7 years of experience (SD=11.6, range 1–46) with an average clinic volume of 37.1 (SD=35.8, range 3–200) HS patients per month. The majority practiced in academic settings (n=37, 75.5%) and directed a HS specialty clinic (n=36, 73.5%).
Respondents with higher monthly HS patient volumes were significantly more likely to believe that conventional medicine (rs=0.40, p=0.01) or that CAM (rs=0.46, p=0.001) are successful at treating HS. HS clinic directors were significantly more likely to agree that CAM is successful (rs =0.35, p=0.01). Academicians (rs=0.37, p=0.01) and HS clinic directors (rs=0.38, p=0.007) were significantly more likely to agree that CAM should be covered by insurance whereas those who have been an attending for longer were significantly less likely to agree (rs=−0.40, p=0.01).
Thirty-one respondents (64.6%) reported their patients routinely ask about CAM, while 22 (44.9%) routinely recommend CAM (Fig. 1). Thirty-six respondents (73.5%) felt comfortable discussing CAM as an adjunctive treatment, whereas only six (12.2%) felt comfortable discussing CAM as a primary treatment. HS clinic directors were significantly more likely to be comfortable discussing CAM as a primary treatment (rs=0.29, p=0.04).
Figure 1.
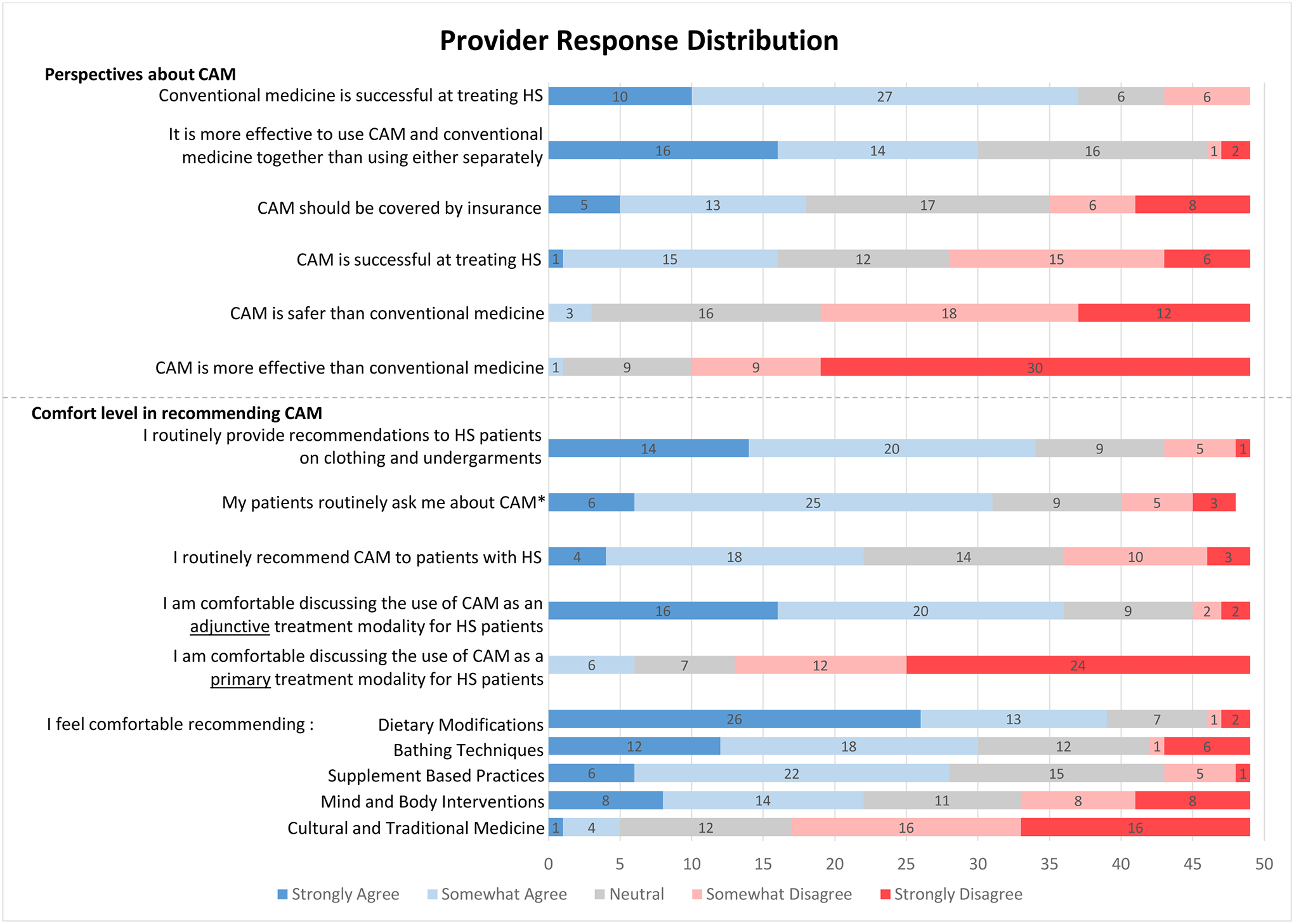
Provider response distribution
*Missing one respondent
Female respondents (rs=0.29, p=0.04) and those with higher monthly HS patient volumes (rs=0.33, p=0.02) were significantly more likely to be comfortable recommending dietary modifications. Respondents who have been an attending for longer were significantly less likely to be comfortable recommending bathing techniques (rs=−0.33, p=0.03). HS clinic directors were significantly more likely to be comfortable with recommending mind-and-body interventions (rs=0.45, p=0.001). No other demographic variables significantly correlated with comfort in treatment modalities or agreement with certain statements.
The most notable barrier to advising CAM was lack of scientific evidence in the medical literature (n=41, 83.7%), followed by efficacy concerns (n=34, 69.4%), ability to recommend reputable CAM products (n=32, 65.3%) and practitioners (n=32, 65.3%), costs to patients (n=23, 46.9%), safety concerns (n=22, 44.9%), and time constraints (n=9, 18.4%).
Discussion/Conclusion
Our study found that nearly half of respondents (44.9%) routinely recommend CAM and the majority (64.6%) are routinely asked about CAM. Most respondents believe that conventional medicine (75.5%) is successful at treating HS, while only 32.7% believe that CAM is successful. Despite minimal support for using CAM alone, 61.2% of respondents reported that CAM and conventional medicine are more effective together than either alone.
To the best of our knowledge, this is the first study to examine CAM for HS from the provider perspective. CAM has been mentioned in several HS guidelines and are highlighted in the North American HS management guidelines.3,4 Battlefield acupuncture is another form of CAM that has demonstrated benefit in pain management and contributed to a reported 77% reduction in injectable opioid use.5 The comfort level among HS providers in recommending dietary changes and bathing techniques parallels the high utilization of these CAM modalities among patients.1
The lack of scientific evidence (83.7%) and efficacy concerns (69.4%) were among the most reported barriers to advising CAM. In similar studies examining dermatologists’ perspectives on CAM, results revealed interest and optimism in the potential benefits of CAM prohibited by limitations in scientific support and education.6,7 In light of both patient and physician interest in CAM, further studies are needed to examine the safety and efficacy of CAM methods.
The limitations of this study include small sample size and the lack of inclusion of non-HS specialists.
CAM practice and comfort level among HS providers are varied and modality-dependent. The lack of well-designed studies precludes confidence in recommending CAM. Future investigations should evaluate the benefit and safety of CAM methods to maximize treatment outcomes for patients impacted by this debilitating disease.
Acknowledgements
We would like to thank our HS colleagues for participating in this study. Special thanks to Ms. Pamela Belfer from the Canadian HS Foundation for her administrative support.
Statistical analyses for this research was supported by NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
Funding Sources
No funding was received for this study.
Footnotes
Conflict of Interest Statement
VYS is a stock shareholder of Learn Health and has served as an advisory board member, investigator, and/or received research funding from Sanofi Genzyme, Regeneron, AbbVie, Eli Lilly, Novartis, SUN Pharma, LEO Pharma, Pfizer, Galderma, Menlo Therapeutics, Burt’s Bees, GpSkin, Altus Labs and Skin Actives Scientific. RA has served as an advisory board member and/or consultant for AbbVie, Janssen, Eli Lilly, Leo Pharma and Hidramed solutions. AA received honoraria as a consultant, speaker, or advisory board participant from AbbVie, Actelion, Celgene, Galderma, GSK, Janssen, Leo Pharma, Novartis, Sanofi2Genzyme, and Bausch; received grants from AbbVie; and was a research investigator with AbbVie, Aristea, Asana, Boehringer-Ingelheim, Bristol-Myers Squibb, Dermavant, Eli Lilly, Genetech, Glenmark, Incyte, Infla Rx, Janssen, Kyowa, Kymera,Leo Pharma, Merck Serono, Novartis, Pfizer, Regeneron, Roche, UCB, Xoma, and Xenon. IH has served as an advisory board member, investigator, and/or research funding from AbbVie, Pfizer Inc., Bayer, Lenicura, Incyte, UCB, HS Foundation, Boehringer Ingelheim. MAL has served on the advisory boards for Abbvie, Janssen, and Viela Bio, and consulted for Almirall, BSN, Incyte, Janssen, Kymera, and XBiotech. MP is a consultant and/or investigator for AbbVie, Eli Lilly, Novartis, UCB, Trifecta clinical, chemocentryx, and Pfizer. There were no incentives or transactions, financial or otherwise, relevant to this manuscript. KNP, EKC, TRG, JMF, and JLH have no conflicts of interest to declare relevant to this manuscript.
References
- 1.Price KN, Thompson AM, Rizvi O, et al. Complementary and Alternative Medicine Use in Patients With Hidradenitis Suppurativa. JAMA Dermatol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medicine NLo. Complementary and Alternative Medicine. In: Bethesda, MD: 2018: https://www.ncbi.nlm.nih.gov/books/NBK518811/. [Google Scholar]
- 3.Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Journal of the American Academy of Dermatology. 2019;81(1):76–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. Journal of the European Academy of Dermatology and Venereology. 2015;29(4):619–644. [DOI] [PubMed] [Google Scholar]
- 5.Narla S, Price KN, Sachdeva M, et al. Proceeding report of the fourth Symposium on Hidradenitis Suppurativa Advances (SHSA) 2019. J Am Acad Dermatol. 2020. [DOI] [PubMed] [Google Scholar]
- 6.Renzi C, Mastroeni S, Paradisi M, Mazzotti E, Pasquini P. Complementary and alternative medicine: knowledge and attitudes among dermatologists. Acta Derm Venereol. 2009;89(6):642–644. [DOI] [PubMed] [Google Scholar]
- 7.AlGhamdi KM, Khurrum H, Asiri Y. The welcoming attitude of dermatologists towards complementary and alternative medicine despite their lack of knowledge and training. Saudi Pharmaceutical Journal. 2017;25(6):838–843. [DOI] [PMC free article] [PubMed] [Google Scholar]


