Abstract
Clinical trials investigating cardiovascular safety of dipeptidyl peptidase-IV inhibitors (DPP-4i) among patients with cardiovascular and renal disease rarely recruit patients with renal impairment, despite associations with increased risk for major adverse cardiovascular events (MACE). We investigated the risk of MACE associated with the use of DPP-4i among these high-risk patients. Using a new-user, retrospective, cohort design, we analyzed 2010–2015 IBM MarketScan Commercial Claims and Encounters for patients with diabetes, comorbid with cardiovascular disease and/or renal impairment. We compared time to first MACE for DPP-4i versus sulfonylurea and versus metformin. Of 113,296 individuals, 9146 (8.07%) were new DPP-4i users, 17,481 (15.43%) were new sulfonylurea users, and 88,596 (78.20%) were new metformin users. Exposure groups were not mutually exclusive. DPP-4i was associated with lower risk for MACE than sulfonylurea (aHR 0.84; 95% CI 0.74, 0.93) and similar risk for MACE to metformin (aHR 1.07; 95% CI [1.04, 1.16]). DPP-4i use was associated with lower risk for MACE compared to sulfonylureas and similar risk for MACE compared to metformin. This association was most evident in the first year of therapy, suggesting that DPP-4i is a safer choice than sulfonylurea for diabetes treatment initiation in high-risk patients.
Subject terms: Epidemiology, Drug development, Endocrine system and metabolic diseases
Introduction
Diabetes afflicts nearly 26 million people in the United States and is associated with considerable morbidity, mortality, and health care spending1,2. This statistic becomes especially concerning given that many patients with diabetes later develop diabetic complications such as diabetic retinopathy, diabetic ketoacidosis, and peripheral vascular disease. Additionally, patients with diabetes also often suffer from cardiovascular disease3. As such, patients and providers are left with a host of considerations for managing both the symptoms of diabetes and the associated comorbidities.
One important class of medicines to treat type 2 diabetes are the dipeptidyl peptidase-IV inhibitors (DPP-4i), which act by slowing the breakdown of glucagon-like peptide-1 (GLP-1), inhibiting glucagon release and increasing insulin release4. Since they were introduced in 2006, four DPP-4i have been approved by the FDA for stand-alone use or as part of fixed-dose combination products, and they rank third in utilization after metformin and sulfonylurea with 8% of antidiabetic drug prescriptions5.
DPP-4i were initially believed to be protective against major adverse cardiovascular events (MACE), evidenced through pre-market clinical trials6. Given high rates of cardiovascular disease among patients with diabetes7,8, as well as longstanding regulatory interest in the potential adverse cardiovascular events associated with diabetes treatments9, evidence of such a cardioprotective effect was of high regulatory, clinical and market importance. However, despite this early evidence from pre-market clinical pharmacology studies, postmarketing surveillance reports10,11 and data from Phase 4 clinical trials12–14 suggested a possible harmful association with MACE, specifically heart failure.
We examined the association between DPP-4i therapy and cardiovascular events using a large commercial claims database. We focused on individuals at elevated baseline risk, including those with history of cardiovascular disease as well as those with renal impairment, comparing the rates of adverse cardiovascular events among DPP-4i new users with that of metformin and sulfonylurea. The inclusion of individuals with renal impairment reflected increased regulatory interest in understanding cardiovascular risk in this patient population as evidenced in the two latest clinical trials studying the association of DPP-4i and cardiovascular outcomes15,16. Additionally, the results of the Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus Thrombolysis in Myocardial Infarction 53 (SAVOR-TIMI 53) trial showed that an elevated urinary albumin to creatinine ratio was independently associated with increased risk for MACE17. We were interested in this elevated risk population, because if a discernable effect were present, it could mean additional cardiovascular risk from DPP-4i therapy for a population already at high susceptibility to cardiovascular events.
Results
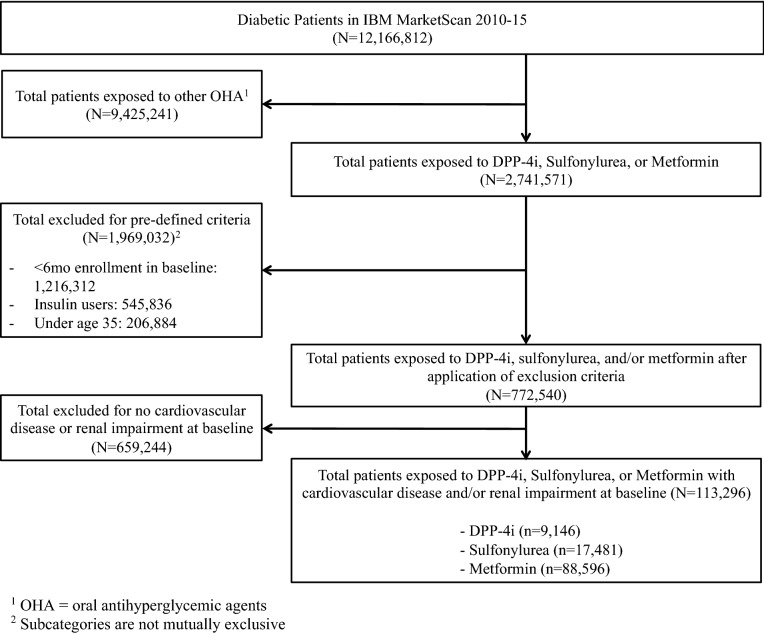
We identified 12,166,812 individuals with diabetes from 2010 to 2015. After applying our inclusion and exclusion criteria, there were a total of 113,296 individuals in our cohort (Fig. 1). Of these, 9146 (8.07%) were new users of DPP-4i, 17,481 (15.43%) initiated sulfonylureas, and 88,596 (78.20%) started metformin. Three percent of included individuals were new users of both DPP-4i and metformin, and 1524 (1.72%) were new users of both sulfonylureas and metformin.
Figure 1.
Cohort derivation and sample attrition after applying inclusion and exclusion criteria for retrospective cohort.
Table 1 depict the demographic and clinical characteristics of DPP-4i users and their counterparts. For example, more sulfonylurea users (60.40%) were male compared to DPP-4i (58.51%) or metformin (52.17%) users. Approximately half of individuals in each exposure group had a cumulative exposure to the treatment of interest less than or equal to 6 months (DPP-4i: 54.05%; sulfonylureas: 56.28%; metformin: 53.65%). There were also several differences in baseline comorbidities, and corresponding medication use, between exposure groups. For example, rates of cardiovascular disease were higher among users of metformin than their counterparts, while kidney disease was more prevalent among users of sulfonylureas (17.22%) and DPP-4i (15.00%) than metformin (7.07%). Differences between users of DPP-4i, sulfonylurea, and metformin were not statistically significant after application of propensity score weighting.
Table 1.
Baseline demographics and medical characteristics.
| DPP-4i (n = 9146) | Sulfonylureas (n = 17,481) | Metformin (n = 88,596) | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Male sex | 5351 | 58.51 | 10,559 | 60.40 | 46,224 | 52.17 |
| Age, years | ||||||
| 35–44 | 877 | 9.59 | 2066 | 11.82 | 11,755 | 13.27 |
| 45–54 | 2815 | 30.78 | 5147 | 29.44 | 29,238 | 33.00 |
| 55–64 | 5454 | 59.63 | 10,268 | 58.74 | 47,603 | 53.73 |
| Cumulative exposure, months | ||||||
| < 6 months | 4943 | 54.05 | 9838 | 56.28 | 47,534 | 53.65 |
| 6–12 months | 2580 | 28.21 | 4326 | 24.75 | 23,869 | 26.94 |
| 12–18 months | 848 | 9.27 | 1665 | 9.52 | 8713 | 9.83 |
| > 18 months | 775 | 8.47 | 1652 | 9.45 | 8480 | 9.57 |
| Comorbidities in baseline | ||||||
| Cardiovascular disease | 8187 | 89.51 | 15,359 | 87.86 | 84,138 | 94.97 |
| Kidney disease (chronic and acute) | 1372 | 15.00 | 3011 | 17.22 | 6263 | 7.07 |
| Cerebrovascular disease | 1574 | 17.21 | 2931 | 16.77 | 14,391 | 16.24 |
| Ischemic heart disease | 3926 | 42.93 | 7374 | 42.18 | 35,242 | 39.78 |
| Hypertension | 7501 | 82.01 | 13,902 | 79.53 | 68,723 | 77.57 |
| Eye disease | 3149 | 34.43 | 5289 | 30.26 | 28,809 | 32.52 |
| Renal diseasea | 4029 | 44.05 | 7243 | 41.43 | 34,718 | 39.19 |
| Acute renal failure | 465 | 5.08 | 1126 | 6.44 | 2118 | 2.39 |
| Neuropathy | 1320 | 14.43 | 2270 | 12.99 | 12,573 | 14.19 |
| Nephropathy | 559 | 6.11 | 1330 | 7.61 | 2455 | 2.77 |
| aDCSI score | ||||||
| 0 | 5813 | 63.56 | 11,326 | 64.79 | 61,295 | 69.18 |
| 1 | 1203 | 13.15 | 2055 | 11.76 | 10,806 | 12.20 |
| 2 | 1358 | 14.85 | 2738 | 15.66 | 11,290 | 12.74 |
| 3 + | 772 | 8.44 | 1362 | 7.79 | 5205 | 5.87 |
| Dual exposures | ||||||
| Sulfonylureas | 0 | 0.00 | 0 | 0.00 | 1,524 | 1.72 |
| Metformin | 3451 | 37.73 | 1524 | 8.72 | 0 | 0.00 |
| DPP-4 inhibitors | 0 | 0.00 | 0 | 0.00 | 3451 | 3.90 |
| Concomitant baseline medications | ||||||
| ACE inhibitors | 2022 | 22.11 | 3643 | 20.84 | 20,522 | 23.16 |
| Angiotensin II receptor blockers | 2380 | 26.02 | 3346 | 19.14 | 18,410 | 20.78 |
| Antidepressants | 2132 | 23.31 | 3378 | 19.32 | 24,832 | 28.03 |
| Antiplatelets | 2871 | 31.39 | 4729 | 27.05 | 28,182 | 31.81 |
| Asthma medication | 4599 | 50.28 | 7531 | 43.08 | 48,709 | 54.98 |
| Benzodiazepines | 1842 | 20.14 | 2905 | 16.62 | 20,485 | 23.12 |
| Beta blockers | 2832 | 30.96 | 5208 | 29.79 | 28,437 | 32.10 |
| Blood thinners and anticoagulants | 496 | 5.42 | 820 | 4.69 | 4924 | 5.56 |
| Calcium channel blockers | 1507 | 16.48 | 2762 | 15.80 | 13,754 | 15.52 |
| Cardioselective beta blockers | 940 | 10.28 | 1632 | 9.34 | 7767 | 8.77 |
| Diuretics | 1737 | 18.99 | 3016 | 17.25 | 19,258 | 21.74 |
| Nitrates | 807 | 8.82 | 1342 | 7.68 | 7924 | 8.94 |
| Peripheral neuropathic treatments | 688 | 7.52 | 944 | 5.40 | 6867 | 7.75 |
| Statins | 4699 | 51.38 | 7484 | 42.81 | 41,933 | 47.33 |
| Thiazide diuretics | 1875 | 20.50 | 3335 | 19.08 | 21,306 | 24.05 |
aDCSI adapted diabetes complications severity index.
aIncludes diseases of kidneys, ureters, and bladders; inclusive of acute renal failure.
The median follow-up for the primary outcome was 160 days (interquartile range (IQR) 92–296 days) and there was no statistically significant difference in time-to-event distributions across the therapeutic classes examined. After propensity score weighting and adjusting for baseline demographics, clinical characteristics, and concomitant medications, the incidence rate for the primary outcome was statistically significantly less (30.20 per 1000 person-years) among new users of DPP-4i compared to sulfonylureas (Table 2). There was a non-statistically significant increase in the incidence rate for the primary outcome among new users of DPP-4i compared to sulfonylureas (91.25 per 1000 person-years vs. 79.46 per 1000 person-years). Among the secondary outcomes, the incidence rate for heart failure was statistically significantly less (4.07 per 1000 person-years vs. 7.56 per 1000 person-years) for new users of DPP-4i compared to sulfonylurea. The incidence rates for the secondary outcomes were not statistically significantly different between DPP-4i and metformin.
Table 2.
Incidence rates of primary composite outcome, acute myocardial infraction, stroke, and heart failure among new users of DPP-4 inhibitors, sulfonylureas, and metformin.
| Outcome, n | DPP-4 inhibitors | Sulfonylureas | Metformin |
|---|---|---|---|
| Primary composite outcome1 | 510 | 1301 | 4781 |
| Total person years | 5578 | 10,696 | 57,134 |
| Rate per 1000 person years | 91.25 | 121.63 | 79.46 |
| Median [IQR] observation time, days | 160 [92, 286] | 144 [75, 288] | 163 [93, 300] |
| Rate difference (95% CI)2 | – | − 30.20 [− 40.47, − 19.89] | 7.75 [− 0.45, 15.96] |
| Acute myocardial infarction | 54 | 132 | 450 |
| Total person years | 5898 | 11,487 | 60,159 |
| Rate per 1000 person years | 9.16 | 11.49 | 7.06 |
| Median [IQR] observation time, days | 167 [98, 297] | 161 [90, 308] | 172 [100, 314] |
| Rate difference (95% CI)2 | – | − 2.34 [− 5.45, 0.80] | 1.68 [− 0.91, 4.22] |
| Stroke | 141 | 268 | 1202 |
| Total person years | 5839 | 11,380 | 59,592 |
| Rate per 1000 person years | 24.15 | 23.55 | 20.17 |
| Median [IQR] observation time, days | 167 [97, 295] | 159 [90, 305] | 171 [99, 311] |
| Rate difference (95% CI)2 | – | 0.60 [− 4.31, 5.47] | 3.98 [− 0.19, 8.14] |
| Heart failure | 24 | 87 | 240 |
| Total person years | 5912 | 11,512 | 60,277 |
| Rate per 1000 person years | 4.06 | 7.56 | 3.98 |
| Median [IQR] observation time, days | 168 [98, 298] | 161[90,308] | 172 [100, 314] |
| Rate difference (95% CI)2 | – | − 3.50 [− 5.78, − 1.21] | 0.08 [− 1.64, 1.82] |
IQR interquartile range.
1Primary composite outcome includes myocardial infarction, cardiac arrest, coronary artery bypass, coronary angioplasty, heart failure, stroke, inpatient death.
2Incidence rate difference per 1000 person-years.
Bold values indicate statistically significant results.
After propensity score weighting and adjustment for baseline demographics, clinical characteristics, and concomitant medications, there was a statistically significant association between new use of DPP-4i and the primary outcome of MACE compared to sulfonylurea (adjusted hazard ratio (aHR) 0.84, 95% confidence interval (CI) 0.74–0.93). However, there was no statistically significant difference in risk of MACE among users of DPP-4i as compared with metformin (aHR 1.07, 95% CI 0.98–1.16) (Table 3). There were no statistically significant differences between sexes in the association between new use of DPP-4i and the primary outcome compared to sulfonylurea or metformin (Additional File 1, Supplementary Appendix 3).
Table 3.
Hazard ratios for the association between DPP-4 inhibitor use and primary composite outcome, acute myocardial infraction, stroke, and heart failure compared to sulfonylureas and metformin.
| Reference drug | Hazard ratios for DPP-4 inhibitors use | |||
|---|---|---|---|---|
| Primary composite outcomec | Acute myocardial infarction | Stroke | Heart failure | |
| Sulfonylureas | ||||
| HR (95% CI)a | 0.77 [0.69, 0.93] | 0.81 [0.56, 1.07] | 1.03 [0.84, 1.34] | 0.59 [0.35, 0.89] |
| aHR (95% CI)a | 0.84 [0.74, 0.93] | 0.95 [0.72, 1.40] | 1.08 [0.89, 1.35] | 0.71 [0.35, 1.09] |
| Metformin | ||||
| HR (95% CI)a | 0.98 [0.87, 1.08] | 1.13 [0.92, 1.53] | 1.12 [0.98, 1.34] | 0.94 [0.62, 1.41] |
| aHR (95% CI)b | 1.07 [0.98, 1.16] | 1.32 [0.96, 1.81] | 1.16 [0.98, 1.42] | 1.19 [0.81, 1.81] |
aPropensity score weighting only.
bPropensity score weighting and demographics, comorbidities, and concomitant medications as regressors and stratifiers.
cPrimary composite outcome includes myocardial infarction, cardiac arrest, coronary artery bypass, coronary angioplasty, heart failure, stroke, inpatient death.
Bold values indicate statistically significant results.
There was a statistically significant association for heart failure in the propensity score weighted analysis comparing DPP-4i to sulfonylurea (HR 0.59, 95% CI 0.35–0.89); however, after adjusting for potential confounders, the association was attenuated and no longer statistically significant. DPP-4i was also not statistically significantly associated with acute myocardial infarction when compared to sulfonylureas (aHR 0.95, 95% CI 0.72–1.40) or metformin (aHR 1.32, 95% CI 0.96–1.81), nor was there a statistically significant association between DPP-4i and stroke when compared to sulfonylureas (aHR 1.08, 95% CI 0.89–1.35) or metformin (aHR 1.16, 95% CI 0.98–1.42).
When comparing the association between DPP-4i and the primary outcome by cumulative exposure strata, there were differences from the overall effect. In the comparison between new users of DPP-4i and sulfonylurea, the adjusted hazard ratio for the primary outcome was statistically significant for a cumulative exposure of < 6 months (aHR 0.85, 95% CI 0.71–0.93) and 6–12 months (aHR 0.76, 95% CI 0.70–0.93). However, statistical significance was not evident for cumulative exposure 12–18 months and > 18 months. This suggests that the overall aHR might be driven by differences in MACE risk seen in the first year after initial exposure. There were no differences between the overall and cumulative exposure stratum specific adjusted hazard ratios for MACE between new users of DPP-4i and metformin (Table 4).
Table 4.
Hazard ratios for the association between DPP-4 inhibitor use and primary composite outcome, stratified by cumulative exposure.
| Reference drug | Hazard ratios for DPP-4 inhibitors use | ||
|---|---|---|---|
| Nref | NDPP-4i | Hazard ratio [95% CI] | |
| Sulfonylureas | |||
| aHRa | 17,481 | 9146 | 0.84 [0.74, 0.93] |
| Cumulative exposure < 6 months | 9838 | 4943 | 0.85 [0.71, 0.93] |
| Cumulative exposure 6–12 months | 4326 | 2580 | 0.76 [0.70, 0.93] |
| Cumulative exposure 12–18 months | 1665 | 848 | 0.80 [0.90, 1.11] |
| Cumulative exposure > 18 months | 1652 | 775 | 0.98 [0.92, 1.11] |
| Metformin | |||
| aHRa | 88,596 | 9146 | 1.07 [0.98, 1.16] |
| Cumulative exposure < 6 months | 47,534 | 4943 | 1.10 [0.85, 1.14] |
| Cumulative exposure 6–12 months | 23,869 | 2580 | 1.05 [0.92, 1.11] |
| Cumulative exposure 12–18 months | 8713 | 848 | 0.97 [0.90, 1.12] |
| Cumulative exposure > 18 months | 8480 | 775 | 1.16 [0.87, 1.13] |
Primary composite outcome includes myocardial infarction, cardiac arrest, coronary artery bypass, coronary angioplasty, heart failure, stroke, inpatient death.
aPropensity score weighting and demographics, comorbidities, and concomitant medications as regressors and stratifiers.
Bold values indicate statistically significant results.
Results of analyses excluding individuals with acute renal failure (sulfonylureas: aHR 0.83, 95% CI 0.17–0.86; metformin: aHR 1.08, 95% CI 1.01–1.19) showed qualitatively similar results to those including these individuals (sulfonylureas: aHR 0.84, 95% CI 0.74–0.93; metformin: aHR 1.07, 95% CI 0.98–1.16). Similarly, results were not sensitive to changes in the latency period after the last dose of exposure for the primary analysis results, nor did they differ substantively when lagging the latency period by 7-days or 30-days (Additional File 1, Supplementary Appendix 4).
Discussion
In this longitudinal study of commercial claims data for individuals with diabetes, having also cardiovascular disease and renal impairment, new use of DPP-4i was associated with a lower risk for MACE compared to sulfonylureas, and a comparable risk compared to metformin. This difference was most evident in the first year of use. New use of DPP-4i was not shown to be associated with the following individual components of MACE: heart failure, stroke, or acute myocardial infarction. These results contribute to the body of evidence examining the association of DPP-4i and MACE in individuals at higher risk for cardiovascular events.
Overall, our results corroborated those of previous clinical trials and observational studies of cardiovascular safety of DPP-4i. Our results showed no increased risk for MACE with the use of DPP-4i similar to the conclusions in the three completed clinical trials comparing DPP-4i and placebo12,13,18. However, unlike these trials our study population consisted of a high-risk group of individuals with established cardiovascular disease and renal impairment in a real-world setting with multiple comorbidities and concomitant medications. Additionally, our study allowed us to compare DPP-4i to other available therapies, namely sulfonylureas and metformin, showing a decreased risk for MACE when compared to sulfonylureas.
Three notable observational studies provide additional context to our results. First, a 2015 administrative claims study using the Taiwan National Health Insurance Research Database of individuals with diabetes and chronic kidney disease admitted for acute myocardial infarction also showed no increased risk for MACE when comparing individuals on sitagliptin to those not on sitagliptin19. Expanding on this approach, our study design included individuals with a multitude of cardiovascular conditions at baseline, making our results more generalizable to high-risk individuals with diabetes. The second study of 127,555 individuals which used the Italian Nationwide OsMed Health-DB database showed decreased risk in hospitalization for heart failure risk associated with DPP-4i compared to sulfonylurea (HR 0.78; 95% CI 0.62–0.97)20. This suggests that the increased risk for MACE in our comparison might be driven by differences in risk for heart failure. This is partially evident in the statistically significant unadjusted hazard ratio for heart failure as a secondary outcome (Table 3). Finally, a study of Medicare patients with diabetes compared cardiovascular risk of DPP-4i to sulfonylurea and thiazolidinediones and found no increased risk in individuals over age 6521. While our study was limited to a patient population under age 65, this study shows that our results are similar to those found in a study of older patients.
A major strength of our study was the identification of a high-risk cohort through the use of a large administrative database. The results of the SAVOR TIMI-53 trial showed that renal impairment was independently associated with adverse cardiovascular outcomes, even after adjusting for cardiovascular risk factors17. As such, our decision to restrict the study cohort to individuals with diabetes, comorbid with cardiovascular disease and renal impairment allowed us to hone in on a patient population identified by FDA as more appropriate for the study of this drug-event association. In a 2008 Guidance for Industry9, regulators noted that such patients are often excluded from pre-approval clinical trials, and recommended studies of the association between oral antihyperglycemic agents and MACE should include high-risk patients.
Our study also had several limitations. First, we included individuals using multiple therapies of interest (e.g., both DPP-4i and sulfonylureas) at baseline. While this may have led to potential misclassification, their exclusion would have resulted in a much smaller and less generalizable sample22. Second, our new-user design did not account for time-varying hazards for MACE, although the cumulative exposure stratified analysis suggested that the differences in risk of MACE between DPP-4i and sulfonylureas were most evident during the first year of exposure. Third, our analyses are subject to potential informative censoring due to a change in exposure status. However, our results were insensitive to the lagged latency period after the last day of exposure, and since most events occurred within the first year of exposure, extending the latency period past 30-days would have been unlikely to have changed our results and could have potentially led to misclassification. Finally, due to limitations in the administrative claims data, we were unable to assess mortality outside of the inpatient setting as a component of the primary composite outcome or as a competing risk. However, it is unlikely that death outside of the inpatient setting would occur more frequently in one exposure group than another in this cohort, potentially leading to biased results.
Our results provide evidence of decreased risk for MACE when comparing DPP-4i versus sulfonylurea in a commercially insured patient population with diabetes, comorbid with cardiovascular disease and renal impairment in the United States. Additionally, we found that there was no difference in risk of MACE for these individuals when comparing DPP-4i and metformin. Further studies are needed to determine differences in risk for individual components of the composite outcome, particularly heart failure. Finally, the decreased risk seen with DPP-4i use compared to sulfonylurea is more likely due to cardiovascular risk associated with sulfonylurea rather than protective effects of DPP-4i, as there was no difference in effect between DPP-4i and metformin, which carries little cardiovascular risk.
Methods
Study design and data source
We conducted a population-based, retrospective cohort study with a new-user design using data from IBM MarketScan Commercial Claims and Encounters from January 2010 through December 2015. MarketScan houses linked paid claims and encounter data from approximately 350 payers, covering more than 25 million individuals annually. The data consists of de-identified individual-level healthcare utilization data including demographic characteristics and information on inpatient and outpatient medical services and pharmacy claims issued.
Cohort derivation
We identified individuals with type 2 diabetes as those with at least one prescription for an oral antihyperglycemic agent and either hemoglobin A1c greater than 6.5% twice, fasting glucose greater than 126 mg/dL twice on different days, random glucose > 200 mg/dL twice on different days, one inpatient diagnosis of diabetes (ICD-9(10) codes: 250x (E11.9), 357.2 (E11.42), 366.41 (E11.36), 362.01–362.07 (E11.3*)) or outpatient diagnosis for diabetes (ICD-9(10) codes: 250x (E11.9), 366.41 (E11.36), 362.01–362.07 (E11.3*)) twice on different days. We included individuals if they received at least one prescription for an FDA-approved DPP-4i, sulfonylurea, or metformin (Additional File 1, Supplementary Appendix 1). We assigned an index date as the date of first filled prescription for one of these products. The baseline period was defined as the six-month period preceding this. We used International Classification of Diseases, 9th and 10th Revisions (ICD-9/10) codes from inpatient and outpatient records to identify those with a history of cardiovascular disease and/or renal impairment (chronic kidney disease or acute renal failure) for inclusion into the study.
We excluded individuals based on: (1) no continuous medical or pharmacy enrollment in the six-month baseline period; (2) below the age of 35; (3) insulin use at baseline; (4) end-stage renal disease in the baseline period; (5) less than 12-weeks of exposure to index treatment; or (6) treatment with oral antihyperglycemic agents in the 6-month baseline period. We followed individuals until the first of the following occurrences: (1) 14-days after the last date of exposure; (2) switch to or addition of anti-hyperglycemic treatment that was not DPP-4i, sulfonylurea, or metformin; (3) end in medical or pharmacy enrollment; (4) first date of either a major adverse cardiovascular event; or (5) study end date of 31 December 2015.
Definition of exposure
We assigned individuals to an exposure group based on their first prescription of DPP-4i, sulfonylurea, or metformin. In the event of multiple drug class prescriptions on the index date, individuals were counted in all relevant exposure groups. Due to the large number of individuals on multiple antihyperglycemic agents, particularly metformin in combination with other drug classes, dropping these individuals would have resulted in a considerably smaller sample size, reducing statistical power as well as the generalizability of our results.
Definition of outcome
We defined our primary composite outcome as the first of any of the following events: myocardial infarction, cardiac arrest, coronary artery bypass graft, coronary angioplasty, heart failure, and stroke. We did not examine all-cause mortality outside of the inpatient setting as an outcome, because information on these deaths were not available for our dataset. Our secondary outcomes were acute myocardial infarction, stroke, and heart failure. We used validated algorithms to identify myocardial infarction23, cardiac arrest24, coronary artery bypass graft23, coronary angioplasty23, heart failure25, and stroke26.
Definition of covariates
We used the peer-reviewed literature19,27–29, clinical guidelines30–34 and expert opinion9,35 in order to identify key covariates of interest. We assessed possible confounding due to patient age and sex; cardiovascular risk factors including hypertension and hypercholesterolemia, diabetic complications, diabetic severity at baseline as measured by the Adjusted Diabetes Comorbidities Severity Index (aDCSI)36–38, and other common comorbidities such as cerebrovascular disease, ischemic heart disease, asthma, and rheumatoid arthritis. Comorbidities coded under ICD-9 were identified using the Clinical Classification Software (CCS) developed by the Agency for Healthcare Research and Quality39. Additionally, we used National Drug Codes to assess for possible confounding due to concomitant medications including statins, angiotensin converting enzymes (ACE) inhibitors, platelet aggregation inhibitor, calcium channel blockers, angiotensin II receptor blockers, beta-blockers, diuretics, nitrates, and inhaled corticosteroids.
Propensity score
We used the Toolkit for Weighting and Analysis of Nonequivalent Groups (twang) package developed by the RAND Corporation40 to compute the propensity scores and associated weights used in the analysis to balance the covariates between exposure groups. To do so, we identified all available covariates without an association to the exposure that were associated to the primary outcome in order to increase precision41 (Additional File 1, Supplementary Appendix 2). Next, we used generalized boosted regression models to optimize the selection of covariates for the propensity score calculation, allowing for propensity scores estimation in the presence of multiple exposure groups. We used the standardized mean difference (SMD) to measure balance of covariates before and after weighting. Propensity score weighting reduced the SMD from a maximum of 0.23 to less than 0.01. We used the average treatment effect on the treated (ATT) propensity score weights to estimate the treatment effect of DPP-4i.
Statistical analysis
We identified a baseline period of 6 months prior to the first filled prescription of the exposure group. Using chi-square statistics for categorical covariates and the Kruskal–Wallis test for continuous covariates, we compared differences at baseline between new users of DPP-4i, sulfonylurea, and metformin. We used exact Poisson tests to compare absolute differences in incidence rates for the primary and secondary outcomes for new users of DPP-4i compared to those of sulfonylurea and metformin. Additionally, we checked for differences in duration of exposure to treatment distributions using a Kolmogorov–Smirnov test. Using the propensity score weights described above, we calculated weighted crude and adjusted Cox proportional hazards for the association between new use of DPP-4i and the primary and secondary outcomes compared to new use of sulfonylureas and metformin. For the adjusted hazard ratios, we included indicators for age, sex, baseline comorbidities, and concomitant medications. Additionally, we checked for covariates that violated the proportional hazards assumption by plotting the scaled Schoenfeld residuals. These covariates were added to the Cox proportional hazards model as stratifying variables. We also used spline intervals every 6 months to address potential violations of the proportional hazard assumption. Finally, we included an indicator variable for individuals included in multiple exposure groups and an indicator variable for cumulative exposure, which was defined as the number of days exposed to the exposure group drug. We stratified the analysis by the cumulative exposure variable. All analyses were conducted in R, version 3.3.3.
Sensitivity analyses
To check the robustness of our results, we first assessed possible sensitivity of our results to the latency of the period after drug discontinuation. We followed individuals for 14-, 7-, and 30-days after the last day of exposure to drug. Next, we recalculated the primary analysis without individuals with acute renal failure to determine whether our results were sensitive to the inclusion of those individuals. Finally, we compared the association of DPP-4i and the primary outcome between cumulative exposure strata and sex strata to assess possible effect modification.
The study was exempted from review by a Johns Hopkins Institutional Review Board, and all research was performed in accordance with relevant guidelines/regulations. Our study utilized commercial claims data through IBM Marketscan Research Databases. As such, we did not obtain informed consent. This was in accordance with local laws and regulations, and aligned with the terms of use from IBM Marketscan Research Databases.
Ethics approval
The study was exempted from review by a Johns Hopkins Institutional Review Board.
Supplementary Information
Author contributions
S.B., G.A., J.S., M.M. and S.E. contributed to the development of the research question and the writing of this manuscript. S.B., J.W., H.C. and O.M. contributed to the derivation of the cohort for this study. All authors contributed to the analysis plan and interpretation of results. Analysis was conducted by S.B. and reviewed by all authors.
Funding
This work was supported in part through the Johns Hopkins Center of Excellence in Regulatory Science and Innovation (U01FD004977-03), the National Heart, Lung, and Blood Institute of the National Institutes of Health (T32HL139426), and the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK120518). The funding sources had no role in the design and conduct of the study, analysis or interpretation of the data, and preparation or final approval of the manuscript prior to publication.
Data availability
The data that support the findings of this study are available from IBM MarketScan Research Databases but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of IBM MarketScan Research Databases.
Competing interests
Dr. Alexander is Chair of FDA’s Peripheral and Central Nervous System Advisory Committee, has served as a paid advisor to IQVIA, is a co-founding Principal and equity holder in Monument Analytics, a health care consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation, and serves on OptumRx’s National P&T Committee. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. All other authors have no conflict of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-95687-z.
References
- 1.Centers for Disease Control and Prevention. Diabetes 2014 Report Card. https://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf (2014).
- 2.Schmittdiel JA, et al. Prescription medication burden in patients with newly-diagnosed diabetes: A surveillance, prevention, and management of diabetes mellitus (SUPREME-DM) study. J. Am. Pharm. Assoc. 2014;54:374–382. doi: 10.1331/JAPhA.2014.13195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grundy SM, et al. Prevention conference VI: Diabetes and Cardiovascular Disease: executive summary: Conference proceeding for healthcare professionals from a special writing group of the American Heart Association. Circulation. 2002;105:2231–2239. doi: 10.1161/01.CIR.0000013952.86046.DD. [DOI] [PubMed] [Google Scholar]
- 4.Garber AJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2017 executive summary. Endocr. Pract. 2017;23:207–238. doi: 10.4158/ep161682.cs. [DOI] [PubMed] [Google Scholar]
- 5.Hampp C, Borders-Hemphill V, Moeny DG, Wysowski DK. Use of antidiabetic drugs in the U.S., 2003–2012. Diabetes Care. 2014;37:1367–1374. doi: 10.2337/dc13-2289. [DOI] [PubMed] [Google Scholar]
- 6.Chen XW, et al. Clinical pharmacology of dipeptidyl peptidase 4 inhibitors indicated for the treatment of type 2 diabetes mellitus. Clin. Exp. Pharmacol. Physiol. 2015;42:999–1024. doi: 10.1111/1440-1681.12455. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association Cardiovascular disease and risk management: Standards of medical care in diabetes-2018. Diabetes Care. 2018;41:S86–S104. doi: 10.2337/dc18-S009. [DOI] [PubMed] [Google Scholar]
- 8.Abdul-Ghani M, et al. Cardiovascular disease and type 2 diabetes: Has the dawn of a new era arrived? Diabetes Care. 2017;40:813–820. doi: 10.2337/dc16-2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Food and Drug Administration. Guidance for Industry: Diabetes Mellitus — Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes. (2008).
- 10.Scheen AJ. Safety of dipeptidyl peptidase-4 inhibitors for treating type 2 diabetes. Expert Opin. Drug Saf. 2015;14:505–524. doi: 10.1517/14740338.2015.1006625. [DOI] [PubMed] [Google Scholar]
- 11.Baksh SN, McAdams-DeMarco M, Segal JB, Alexander GC. Cardiovascular safety signals with dipeptidyl peptidase-4 inhibitors: A disproportionality analysis among high-risk patients. Pharmacoepidemiol. Drug Saf. 2018 doi: 10.1002/pds.4437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White WB, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N. Engl. J. Med. 2013;369:1327–1335. doi: 10.1056/NEJMoa1305889. [DOI] [PubMed] [Google Scholar]
- 13.Scirica BM, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N. Engl. J. Med. 2013;369:1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 14.Green JB, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 2015 doi: 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 15.Rosenstock J, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: The CARMELINA Randomized Clinical Trial. JAMA. 2018 doi: 10.1001/jama.2018.18269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenstock J, et al. Effect of linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: The CAROLINA Randomized Clinical Trial. JAMA. 2019;322:1155–1166. doi: 10.1001/jama.2019.13772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scirica BM, et al. Cardiovascular outcomes according to urinary albumin and kidney disease in patients with type 2 diabetes at high cardiovascular risk: Observations from the SAVOR-TIMI 53 trial. JAMA Cardiol. 2018;3:155–163. doi: 10.1001/jamacardio.2017.4228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green JB, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 2015;373:232–242. doi: 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 19.Chen DY, et al. Sitagliptin and cardiovascular outcomes in diabetic patients with chronic kidney disease and acute myocardial infarction: A nationwide cohort study. Int. J. Cardiol. 2015;181:200–206. doi: 10.1016/j.ijcard.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 20.Fadini GP, et al. Risk of hospitalization for heart failure in patients with type 2 diabetes newly treated with DPP-4 inhibitors or other oral glucose-lowering medications: A retrospective registry study on 127,555 patients from the Nationwide OsMed Health-DB Database. Eur. Heart J. 2015;36:2454–2462. doi: 10.1093/eurheartj/ehv301. [DOI] [PubMed] [Google Scholar]
- 21.Gokhale M, et al. No increased risk of cardiovascular events in older adults initiating dipeptidyl peptidase-4 inhibitors vs therapeutic alternatives. Diabetes Obes. Metab. 2017;19:970–978. doi: 10.1111/dom.12906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Packer M. Worsening heart failure during the use of DPP-4 inhibitors: Pathophysiological mechanisms, clinical risks, and potential influence of concomitant antidiabetic medications. JACC Heart Fail. 2018;6:445–451. doi: 10.1016/j.jchf.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Youngson E, et al. Defining and validating comorbidities and procedures in ICD-10 health data in ST-elevation myocardial infarction patients. Medicine. 2016;95:e4554. doi: 10.1097/md.0000000000004554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hennessy S, et al. Validation of diagnostic codes for outpatient-originating sudden cardiac death and ventricular arrhythmia in Medicaid and Medicare claims data. Pharmacoepidemiol. Drug Saf. 2010;19:555–562. doi: 10.1002/pds.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saczynski JS, et al. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol. Drug Saf. 2012;21(Suppl 1):129–140. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang TE, Lichtman JH, Goldstein LB, George MG. Accuracy of ICD-9-CM codes by hospital characteristics and stroke severity: Paul Coverdell National Acute Stroke Program. J. Am. Heart Assoc. 2016 doi: 10.1161/jaha.115.003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shih CJ, Chen HT, Kuo SC, Ou SM, Chen YT. Cardiovascular outcomes of dipeptidyl peptidase-4 inhibitors in elderly patients with type 2 diabetes: A Nationwide Study. J. Am. Med. Dir. Assoc. 2015 doi: 10.1016/j.jamda.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Kannan S, et al. Risk of overall mortality and cardiovascular events in patients with type 2 diabetes on dual drug therapy including metformin: A large database study from the Cleveland Clinic. J. Diabetes. 2015 doi: 10.1111/1753-0407.12301. [DOI] [PubMed] [Google Scholar]
- 29.Patorno E, et al. Observational studies of the association between glucose-lowering medications and cardiovascular outcomes: Addressing methodological limitations. Diabetologia. 2014;57:2237–2250. doi: 10.1007/s00125-014-3364-z. [DOI] [PubMed] [Google Scholar]
- 30.Alberti KG, et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/circulationaha.109.192644. [DOI] [PubMed] [Google Scholar]
- 31.Fox CS, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association. Diabetes Care. 2015;38:1777–1803. doi: 10.2337/dci15-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waugh N, et al. Newer agents for blood glucose control in type 2 diabetes: Systematic review and economic evaluation. Health Technol. Assess. (Winchester, England) 2010;14:1–248. doi: 10.3310/hta14360. [DOI] [PubMed] [Google Scholar]
- 33.Go AS, et al. Heart disease and stroke statistics–2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Arterioscler. Thromb. Vasc. Biol. 2004;24:e13–e18. doi: 10.1161/01.atv.0000111245.75752.c6. [DOI] [PubMed] [Google Scholar]
- 35.Fonarow GC. Diabetes medications and heart failure: Recognizing the risk. Circulation. 2014;130:1565–1567. doi: 10.1161/circulationaha.114.012883. [DOI] [PubMed] [Google Scholar]
- 36.Glasheen WP, Renda A, Dong Y. Diabetes complications severity index (DCSI)-update and ICD-10 translation. J. Diabetes Complic. 2017;31:1007–1013. doi: 10.1016/j.jdiacomp.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 37.Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted diabetes complications severity index in claims data. Am. J. Manage. Care. 2012;18:721–726. [PubMed] [Google Scholar]
- 38.Young BA, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am. J. Manage. Care. 2008;14:15–23. [PMC free article] [PubMed] [Google Scholar]
- 39.Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-10-PCS. Healthcare Cost and Utilization Project (HCUP). http://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp (2017).
- 40.Ridgeway, G. M. D., Morral, A. R., Burgette, L. F. & Griffin, B. A. Toolkit for Weighting and Analysis of Nonequivalent Groups (TWANG) Website http://www.rand.org/statistics/twang (2014).
- 41.Brookhart MA, et al. Variable selection for propensity score models. Am. J. Epidemiol. 2006;163:1149–1156. doi: 10.1093/aje/kwj149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from IBM MarketScan Research Databases but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of IBM MarketScan Research Databases.