Abstract
Objective:
College is a high-risk period for the initiation and escalation of problem alcohol use. College students with attention-deficit/hyperactivity disorder (ADHD) are at particularly high risk for experiencing alcohol-related negative consequences relative to typically-developing peers. Despite this, the best therapeutic approach for addressing alcohol problems in college students with ADHD has not been identified. Behavioral activation (BA) may augment effects of gold-standard college drinking interventions (i.e., brief motivational intervention; BMI) for students with ADHD who are engaging in problem drinking.
Method:
113 college students with ADHD (M age = 19.87, SD = 1.44; 49.1% male) were randomized to either BMI+BA or BMI plus supportive counseling (BMI+SC). Both groups received ADHD psychoeducation delivered in MI style. Outcomes were assessed using the Brief Young Adult Alcohol Consequences Questionnaire, Daily Drinking Questionnaire, Barkley Functional Impairment Scale, and Beck Depression Inventory.
Results:
There were no significant differences in outcomes for the sample as a whole; in both conditions, participants showed significant reductions in their alcohol-related negative consequences, alcohol use, and depressive symptoms at 1- and 3- month follow-ups. Exploratory moderation analyses revealed that participants with elevated depressive symptoms at baseline evidenced greater reductions in alcohol-related negative consequences in the BMI+BA condition compared to BMI+SC at the 3-month follow-up. Those low in depressive symptoms evidenced greater reductions of alcohol-related negative consequences in BMI+SC compared to BMI+BA.
Conclusions:
For college students with ADHD who reported elevated baseline depressive symptoms, inclusion of BA with BMI resulted in significantly greater decreases in alcohol-related negative consequences, compared to BMI+SC.
Keywords: ADHD, College Students, Behavioral Activation, Motivational Interviewing, Alcohol
College is a high-risk developmental period for the initiation and escalation of problem alcohol use, setting the stage for post-college drinking and lifelong alcohol-related negative consequences (Arria et al., 2016). Developmental models of alcohol use progression identify an activating environment interacting with individual vulnerabilities as one pathway leading to the onset of alcohol use disorders (Tarter, Vanyukov, & Kirisci, 2008). These models support the importance of identifying and intervening with high-risk subgroups who are especially vulnerable to alcohol problems during college (Johnston et al., 2014).
College students with attention-deficit/hyperactivity disorder (ADHD) represent one such high risk group. Approximately 2–8% of college students in the U.S. are affected by ADHD, a disorder characterized by developmentally inappropriate symptoms of inattention, hyperactivity, and impulsivity (Weyandt & DuPaul, 2008). Beyond these core symptoms, individuals with ADHD tend to prioritize immediately-reinforcing activities, even when doing so confers risk and jeopardizes longer-term goals (Dreschler et al., 2008). College students with ADHD may therefore choose to drink due to alcohol’s immediately-reinforcing qualities (Bowirrat & Oscar-Berman, 2005), despite negative impacts on academics and social-emotional functioning. Moreover, the precipitous decline in parental monitoring during college may further increase ADHD-related impairment across domains of functioning, including health-risk behaviors such as alcohol misuse (Meaux, et. al., 2009). Individuals with ADHD may struggle with resisting temptations to drink, leading to more compulsive patterns of drinking that are less sensitive to the academic contingencies (e.g., tests, homework) that may serve to modulate drinking among other students. Furthermore, when students with ADHD drink, their difficulties with impulsivity and planning may lead to greater alcohol problems, including fights, accidents, and risky sexual behavior.
Indeed, a diagnosis of ADHD is associated with increased risk for alcohol use disorder (Rooney et al., 2015), with a prior study showing that 47% of college students with ADHD meet DSM-IV criteria for lifetime alcohol abuse and 23% meet criteria for lifetime alcohol dependence, compared to 17% and 10% of non-ADHD college students, respectively. Relative to their typically-developing peers, students with ADHD are also more likely to experience alcohol-related negative consequences, even when reporting the same overall amount of alcohol consumption as their non-ADHD peers. For example, college students with ADHD more frequently vomit from drinking, experience memory loss, get injured when drinking, and have difficulties stopping a drinking episode (Baker, Prevatt, & Proctor, 2012; Rooney et al., 2012).
Intervention for College Students with ADHD who are Heavy Drinkers
Despite increased risk for alcohol-related negative consequences in students with ADHD, no research has been conducted to determine the best approach for reducing risk in this population. Brief motivational intervention (BMI) is a gold standard approach for college drinking, more broadly (Tanner-Smith & Lipsey, 2015). BMI consists of personalized alcohol feedback (e.g., amount and frequency of alcohol consumption, estimated blood alcohol level, negative consequences associated with use) and normative comparisons (i.e., how much the student believes his/her same-aged peers drink compared to normative data) using motivational interviewing (MI) techniques to spotlight discrepancies in the student’s actual versus ideal alcohol use (Walters & Neighbors, 2005). BMI is a cost-effective, time-limited, evidence-based approach resulting in short- and long-term reductions in problem alcohol use in young adults (Tanner-Smith & Lipsey, 2015).
Though BMI has generally been found to be efficacious in reducing problem alcohol use in college students, this approach shows limited effects for students with elevated impulsivity and poor self-regulation (Carey, Henson, Carey, & Maisto, 2007; Ewing et al., 2009), both hallmark traits of ADHD. Given the unique constellation of symptoms associated with ADHD (e.g., poor execution and follow through) and common co-occurring concerns in this population (e.g., depression), it is likely necessary to modify BMI to maximize outcomes in college students with ADHD. Efforts to optimize intervention for high-risk populations are consistent with a growing body of research supporting the addition of other therapeutic elements (e.g., cognitive-behavioral therapy) to standard BMI (Pedrelli et al., 2019). Recognizing the high rates of alcohol-related negative consequences in college students with ADHD (Rooney et al., 2012; White & Hingson, 2013) and poor response to BMI associated with core characteristics of ADHD (Ewing et al., 2009), this line of research is of utmost clinical importance.
Behavioral activation (BA) is a theoretically-plausible approach to augment effects of BMI for students with ADHD engaging in problem drinking for many reasons. BA is thought to target reward deficits, a construct associated with ADHD and problem alcohol use. In part, alcohol use is theorized to become problematic when individuals fail to engage in enjoyable, substance-free activities (Murphy et al., 2012). BA is based on the theory that increasing engagement in pleasurable and/or goal-directed activities in line with one’s values increases contact with environmental rewards and decreases engagement in unhealthy behaviors (Lejuez et al., 2011). As applied to alcohol intervention, BA entails helping patients monitor activities, identify goals and values, increase engagement with pleasurable and/or goal-directed substance-free activities, decrease engagement in maladaptive behaviors, and address barriers to experiencing positive reinforcement from their environments (Dimidjian, Barrera, Martell, Muñoz, Lewinsohn, 2011). These intervention components are ideal for addressing reward deficits that underlie both ADHD and alcohol use (Furukawa et al., 2014; Joyner et al., 2016).
Beyond increasing access to substance-free reward, BA may address core ADHD dysfunctions by helping students schedule and participate in value-driven, substance-free activities across multiple life areas (e.g., engaging in valued substance-free activities with friends; studying; exercising; getting more sleep). BA emphasizes breaking down and scheduling small “steps” toward a larger goal using a calendar system or mobile app. This process involves enlisting help from important people in one’s life to achieve goals, which is particularly relevant during college when parental supports are reduced and more time is spent with peers. Given this focus, BA may be an important therapeutic component in helping college students with ADHD – a disorder typified by poor self-regulation and difficulties in goal attainment (Barkley, 2006) – break down, organize, and systematically work towards substance-free goals. In this regard, BA may address broader academic and social impairments associated with ADHD.
In line with this possibility is research highlighting the trans-diagnostic potential of BA (Vujanovic et al., 2017). The idiographic and flexible nature of BA allows treatment to target a client’s needs, which may be particularly relevant in ADHD. This is because ADHD is a heterogeneous disorder with substantial individual differences in symptom profiles and associated comorbidities. Most notably, there is high comorbidity among ADHD and depression, with one study indicating that approximately 60% of students with ADHD report a history of major depression vs. 11.5% of non-ADHD students (Rooney et al., 2015). Depressive symptoms, in particular, are shown to increase risk for alcohol-related negative consequences in college samples (Dennhardt & Murphy, 2011), to partially account for the relation between ADHD and substance use (Tarter et al., 2008; Yoshimasu et al., 2016), and predict poor response to standard BMI (Murphy et al., 2012). Recognizing that BA is an evidence-based treatment for depression (Reynolds et al., 2011), and depression interferes with BMI efficacy, the addition of BA to BMI may optimize alcohol intervention for students with ADHD and depressive symptoms.
The Present Study
Despite elevated risk for alcohol-related negative consequences and alcohol use disorders in students with ADHD, no studies have systematically evaluated BMI in this population, nor have any existing ADHD intervention studies targeted alcohol-related negative consequences. It is important to target negative consequences in alcohol intervention, beyond simply focusing on overall rates of drinking, given that alcohol use is normative in college and is associated with some positive outcomes (e.g., increased social connection; Ham & Hope, 2003). Moreover, prior research demonstrates that despite not drinking more than their peers, college students with ADHD experience more alcohol-related negative consequences (Rooney et al., 2012; 2015).
The present study aimed to develop and test a novel intervention using a randomized controlled trial design. Both groups received ADHD psychoeducation delivered in MI style as well as BMI. The novel intervention included BA (hereafter referred to as BMI+BA; Vasko et al., 2019), compared to an alternative treatment condition consisting of standard BMI and supportive counseling (SC; hereafter referred to as BMI+SC). This design is optimal for a rigorous experimental evaluation of the addition of BA in alcohol intervention, as we compare our novel intervention to an “already-established treatment” (Chambless, 1998). We hypothesized that BMI+BA would result in greater reductions in the alcohol-related negative consequences (the primary outcome), compared to BMI+SC. As secondary outcomes, we predicted that BMI+BA would also result in greater reductions in overall amount of alcohol use, depressive symptoms and overall functional impairment than BMI+SC, given that BA is an evidence-based treatment for depression that focuses on breaking down and scheduling substance-free reinforcing activities and increasing environmental supports to follow through on planned activities.
An ancillary aim was to explore moderators of treatment response, to begin to determine for whom more intensive treatment (BMI+BA) is warranted. More specifically, we explored whether baseline depressive symptoms moderated outcomes such that participants with higher baseline depressive symptoms would evidence greater improvements in alcohol consequences in the BMI+BA condition (Murphy et al., 2012). BA may be especially advantageous for college students with ADHD who are also experiencing elevated depressive symptoms at baseline, given that BA aims to increase engagement in goal-directed and substance-free rewarding activities (Reynolds et al., 2011). We thus hypothesized that students in the BMI+BA condition would show fewer alcohol-related negative consequences in the context of higher baseline depression.
Method
Participants
The sample consisted of 113 college students at the University of Maryland, College Park (49.1% male). The average age of participants was 19.87 years (SD=1.44). Sample demographic characteristics are presented in Table 1. As depicted in Table 1, a large proportion of participants presented with comorbid mood, anxiety, or substance use disorders in addition to ADHD. Eligibility for the clinical trial (AA022133; PI Chronis-Tuscano) required that participants: (1) met DSM-5 criteria for ADHD, (2) had elevated levels of problem drinking as defined by an Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993) score of 7 or greater for males or 5 or greater for females (DeMartini & Carey, 2012), (3) reside on or off campus, away from their parents, and (4) were not currently participating in (or were willing to suspend) psychotherapy for ADHD that would interfere with the study until completion of study treatment. Bipolar disorder, psychosis, or suicidal thoughts/behaviors characterized by imminent risk and/or requiring immediate treatment were exclusionary.
Table 1.
Demographic and Diagnostic Characteristics
| BMI+BA (n = 55) | BMI+SC (n = 58) | |
|---|---|---|
|
| ||
| Age | M = 19.76, SD = 1.32 | M = 19.97, SD = 1.53 |
| Sex | ||
| Male | 26 (47.3%) | 30 (51.7%) |
| Female | 29 (52.7%) | 28 (48.3%) |
| Ethnicity | ||
| Hispanic/Latino | 7 (12.7%) | 6 (10.3%) |
| Not Hispanic/Latino | 48 (87.3%) | 52 (89.7%) |
| Race | ||
| White/Caucasian | 47 (85.5%) | 50 (86.2%) |
| Black/African American | 5 (9.1%) | 4 (6.9%) |
| Asian | 2 (3.6%) | 2 (3.4%) |
| More than one race | 1 (1.8%) | 2 (3.4%) |
| ADHD Diagnosis | ||
| IA Presentation | 15 (27.3%) | 20 (34.5%) |
| HI Presentation | 1 (1.8%) | 0 (0.0%) |
| Combined Presentation | 39 (70.9%) | 38 (65.5%) |
| Current ADHD medication | 38 (69.1%) | 39 (67.2%) |
| DSM-5 diagnoses | ||
| Current | ||
| MDD | 5 (9.1%) | 3 (5.2%) |
| Mania | 0 (0.0%) | 0 (0.0%) |
| PDD | 4 (7.3%) | 2 (3.4%) |
| Any Anxiety Disorder | 16 (29.1%) | 16 (27.6%) |
| AUD | 20 (36.4%) | 21 (36.2%) |
| CUD | 17 (30.9%) | 16 (27.6%) |
| Lifetime | ||
| MDD | 22 (40.0%) | 25 (43.1%) |
| Mania | 1 (1.9%) | 1 (1.7%) |
| PDD | 5 (9.1%) | 5 (8.6%) |
| Any Anxiety Disorder | 19 (34.5%) | 23 (39.7%) |
| AUD | 26 (47.3%) | 25 (43.1%) |
| CUD | 22 (40.0%) | 22 (37.9%) |
Note. BMI= brief motivational interviewing; BA= behavioral activation; SC= supportive counseling; IA = Inattentive; HI = Hyperactive; MDD = Major Depressive Disorder; PDD = Persistent Depressive Disorder; Any Anxiety Disorder = The presence of any of the following disorders: Panic Disorder, Social Anxiety Disorder, Generalized Anxiety Disorder, or Obsessive-Compulsive Disorder; AUD = Alcohol Use Disorder; CUD = Cannabis Use Disorder.
Procedures
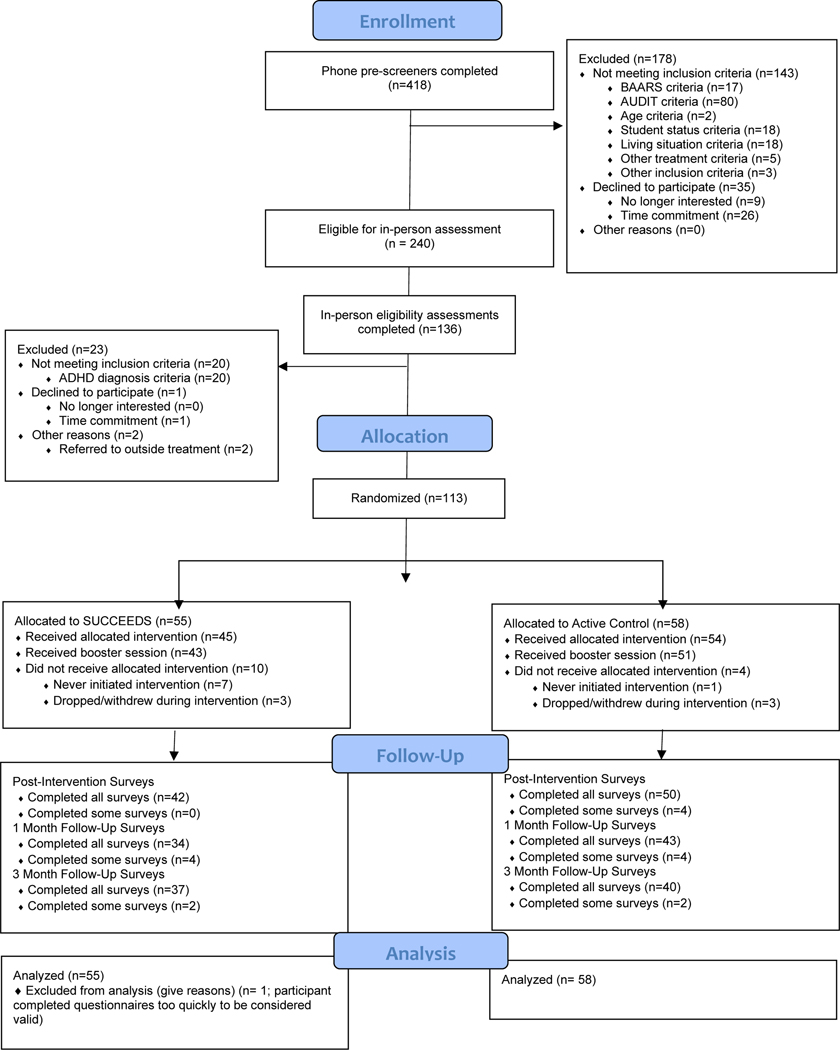
Participants were recruited through flyers, campus listservs, referrals from campus services (e.g., University Counseling Center, Accessibility and Disability Services, Student Health Center), and an online university survey pool (SONA) at a large, public university. Recruitment materials advertised a brief program to help college students with ADHD “lead a healthier lifestyle.” This was to avoid students being deterred by a study focused on reducing alcohol use, as college drinking norms and risk perceptions may interfere with treatment seeking behavior and views of problem drinking (Napper, Grimaldi, & LaBrie, 2015). Interested students were contacted to complete a telephone screen by trained research staff. In the screen, students were consented and administered the Barkley Adult ADHD Rating Scale (BAARS; Barkley, 2011a) to obtain a measure of current ADHD symptoms, and the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, De La Fuente, & Grant, 1993) to measure levels of alcohol misuse. To be invited for a baseline assessment, students had to endorse of 3 or more ADHD symptoms on the BAARS (as a preliminary screener for a possible ADHD diagnosis) and have an elevated score on the AUDIT (i.e., score of 7 or greater for males or 5 or greater for females; DeMartini & Carey, 2012). See CONSORT diagram (Figure 1).
Figure 1.
Consort Diagram
At baseline, students were administered background information interviews, the Adult ADHD Clinical Diagnostic Scale (ACDS; Kessler et al., 2010) semi-structured diagnostic interview to assess past and present ADHD symptoms, and modules of the Structured Clinical Interview of DSM-5 (SCID; First, Williams, Karg, & Spitzer, 2016) to determine a current or past diagnosis of comorbid psychopathology (i.e., mood or substance use disorders). Assessors were advanced-undergraduate, masters-, doctoral-level and postdoctoral trainees. Rigorously-trained and supervised research staff administered diagnostic interviews, and each case was reviewed with an expert panel including 2 Ph.D.’s. Final diagnoses were made based on expert consensus.
Participants were also administered a battery of questionnaires, including self-report of ADHD symptoms and impairment via the BAARS and Barkley Functional Impairment Scale (BFIS; Barkley, 2011b), in addition to other outcome variables. When permission was obtained from participants (n = 70), parent-report of current and childhood ADHD symptoms using the BAARS and BFIS was obtained for the purpose of ADHD diagnosis. Results from the ACDS, BAARS, and BFIS self- and parent-reports were synthesized using the “or rule” to arrive at a diagnosis of ADHD (Shemmassian & Lee, 2012). Given that a threshold of 3 symptoms endorsed on the BAARS was used as initial screening for eligibility via telephone, 20 participants completed a baseline assessment where a diagnosis of ADHD was not reached and they were thus ineligible to continue (see Figure 1). Of the 113 participants, 61.9% of (n=70), had collateral parent report at baseline. Of the 70 participants with parent report, only 2.86% (n=2) required parental report to meet ADHD diagnostic criteria; the remaining 97.15% met ADHD criteria based on self-report alone. Additionally, 75.2% of participants (n=85) reported a previous diagnosis of ADHD. Randomization to treatment condition was stratified based on gender, baseline alcohol use disorder, and current ADHD medication status. All procedures received IRB approval including the participant payments (i.e., receiving compensation for completing measures at baseline, post-treatment, 1-month follow-up, and 3-month follow-up time points). Participants did not pay to receive the treatment.
Interventions
Participants were randomized to one of two treatment conditions: BMI+BA or BMI+ SC. In both conditions, treatment was delivered in 5 sessions over 7 weeks to match groups for therapist contact. Sessions 1 through 4 were conducted in-person for approximately 60 minutes and Session 5 consisted of a brief (i.e., approximately 20-minute) telephone check-in conducted two weeks after the last in-person session. The same team of therapists delivered both conditions to control for potential therapist effects. See Table 2 for the breakdown of session content.
Table 2.
Key Session Components by Week Across Treatment Conditions
| Session # | Week # | BMI+BA | BMI+SC |
|---|---|---|---|
| 1 | 1 | - ADHD Psychoeducation - Personalized ADHD symptom and impairment feedback - Introduction to Activity Monitoring - Introduction of Values |
- ADHD Psychoeducation - Personalized ADHD symptom and impairment feedback - Introduction of journaling |
| 2 | 2 | - Decisional balance - Personalized alcohol use and consequences feedback - Review of Activity Monitoring |
- Decisional balance - Personalized alcohol use and consequences feedback - Review of journaling |
| 3 | 3 | - Introduction to BA and LAVA - Substance-free activity scheduling |
- Generate discussion topic list - Supportive counseling - Review journaling |
| 4 | 5 | - Review/troubleshoot activity completion - Scheduling substance-free activities - Incorporating assists |
- Review/troubleshoot journaling - Supportive counseling |
| 5 | 7 | - Review/troubleshoot activity completion and use of assists - Scheduling substance-free activities - Reflect on SUCCEEDS program |
- Review/troubleshoot journaling - Supportive counseling - Reflect on time in treatment |
Note. ADHD= attention-deficit/hyperactivity disorder; BA= behavioral activation; BMI= brief motivational intervention for alcohol use; SC= supportive counseling; LAVA= life areas, values, and activities.
BMI+BA.
BMI+BA included 1 session of ADHD psychoeducation delivered in an MI style, 1 session of alcohol-focused BMI (including personalized alcohol feedback and goal-setting), and 2 sessions of BA adapted for ADHD. During BA, students discussed their values (e.g., being a reliable friend or a good student) and substance-free activities were scheduled in accordance with those values (e.g., call high school friends weekly, reading textbook for 30 minutes nightly). Lastly, a telephone check-in was conducted two weeks after the final in-person session. See Vasko et al. (2019) for additional intervention details.
BMI+SC.
The alternative control condition also consisted of 3 components: 1 session of ADHD psychoeducation (delivered in MI style), 1 session of alcohol-focused BMI (including personalized alcohol feedback and goal-setting), and 3 sessions of supportive counseling (Hill, 2014). During the latter three sessions, the therapist assumed a supportive facilitative role (e.g., reflective listening) and did not prohibit conversation about psychological issues (e.g., ADHD, alcohol use, depression), but did not initiate conversation on these topics. Therapists engaged empathically without providing cognitive-behavioral skills to address problem areas. This SC approach was utilized in prior BA studies (e.g., Reynolds et al., 2011).
Treatment Fidelity.
Twenty percent of sessions (n = 90) were randomly selected to be coded by independent evaluators (i.e., 9 recordings were randomly selected for each of the 5 sessions in the 2 conditions; all therapists were represented). Independent evaluators consisted of 2 graduate-level and 1 advanced undergraduate-level students. The treatment developers coded a subset of sessions to serve as an answer key by which independent evaluators were tested against during training. Independent evaluators were able to code sessions for fidelity only after having been determined reliable during the training process (k>.8). Within BMI+BA and BMI+SC, 98.9% and 100% of the main points were covered across sessions, respectively, indicating that therapists implemented BMI and ADHD psychoeducation with fidelity and used BA in the BMI+BA condition only. Fidelity assessments confirmed that no BA content was delivered BMI+SC.
Measures
Diagnostic Measures
Adult ADHD Clinical Diagnostic Scale (ACDS; Kessler et al., 2010).
The ACDS is a semi-structured interview that assesses the presence of ADHD symptomology during the past 6 months (current) and in childhood (before the age of 12).
Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993).
The AUDIT is a 10-item brief assessment for excessive drinking and related impairment (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). Test-retest reliability has been shown to be satisfactory in a general population sample with an intra-class correlation coefficient of 0.84 (Park, Sher, & Krull, 2008). The internal consistency in the current sample was .80.
Barkley Adult ADHD Self-Report Scale (BAARS; Barkley 2011a).
The BAARS includes 18 DSM-5 ADHD symptoms on a 4-point Likert scale, with higher scores indicating higher levels of ADHD symptoms. Three versions of the BAARS were utilized: self-report of current symptoms, parent-report of current symptoms, parent-report of childhood symptoms. The BAARS has demonstrated strong t-test reliability and internal consistency (αs .80 - .90) in a large nationally representative sample of adults (Barkley, 2011a). Alphas for the BAAARS current and childhood symptoms ranged from .79 - .93 across self-report and parent-report in this study.
Structured Clinical Interview for DSM-5 (SCID; First et al., 2016).
The SCID is a semi-structured diagnostic interview used to assess past and current DSM-5 mood, alcohol and substance use, and psychosis diagnoses. The interrater reliability averaged across all disorders presented in Table 1 (current and lifetime) in this study was .98 (range: .91–1.00).
Primary Outcome Measure
Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler, Strong, & Read, 2005).
This abbreviated Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Kahler, Strong, & Colder, 2006) utilizes 24 items measuring negative consequences of drinking, and is effective at discriminating severity of alcohol-related negative consequences (Kahler et al., 2005). It has strong convergent validity and test-retest reliability (Kahler, Hustad, Barnett, Strong, & Borsari, 2008). Internal consistency of BYAACQ in this sample was .87.
Secondary Outcome Measures
Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985).
The DDQ asks participants to report how many drinks they consumed each day in the past week. The current study used total number of weekly drinks, which has been shown to be a reliable indicator of alcohol misuse (Borsari, Neal, Collins, & Carey, 2001).
Barkley Functional Impairment Scale (BFIS, Barkley, 2011b).
The BFIS measures ADHD-associated impairment in 15 domains (e.g., daily responsibilities, social relationships-friends/family, community activities, education, dating, money management, sexual relations, self-care). These domains are averaged to derive an overall impairment score, which was used in the current study. The BFIS is valid measure of impairment and has high test-retest reliability (Barkley et al., 2011b). The internal consistency for the total score in the current study was .88.
Beck Depression Inventory (BDI; Beck, Brown, & Steer, 1996).
The BDI is a 21-item self-report measure that assesses depressive symptoms during the past 2-weeks on a 4-point Likert scale. The BDI is a widely-used, reliable, and valid measure (Storch, Roberti, & Roth, 2004). The internal consistency in the current study was .92.
Data Analysis
We calculated Cohen’s d effect sizes (Cohen, 1988) to examine magnitude of change across post-treatment, 1-month follow-up, and 3–month follow-up time points as stipulated in the study’s a-priori aims. The between-group effect sizes estimating the 95% bootstrap confidence intervals were conducted using the bootES package in R (Kirby & Gerlanc, 2013). The between group effect sizes were estimated by first calculating the within-subjects change effects (e.g., change from baseline to Session 4). The contrast score was treated as a dependent variable and between contrast analyses were performed (Kirby & Gerlanc, 2013). These analyses illustrate the degree to which the within-subjects’ effects vary between the two treatment groups.
The primary outcome variable was alcohol-related negative consequences as measured on the BYAACQ (clinicaltrials.gov; NCT02829970). Additional outcomes included self-reported total weekly drinks, depressive symptoms, and functional impairment measured via the DDQ, BDI, and BFIS, respectively. Analyses examining total alcohol related negative consequences included total weekly drinks (DDQ) included as a covariate. Given that the intent-to-treat sample is repeated measures, we used linear mixed models (LMM; also referred to as multilevel models; West, 2009) for analyses. 1 We estimated LMM using full-restricted maximum likelihood estimator (REML). We selected the unstructured covariance matrix because it fully captures the correlation structure among latent growth factors (e.g., latent intercept and slope) without any presumed constraints, thereby thoroughly accounting for correlations between repeated measures. LMM uses all available data on each participant (in line with the intent to treat approach) and allows for more flexible estimation of the correlation of repeated measures. The within-cluster correlations accounts for participants’ random deviations from model estimations varying in structured patterns across measures. The LMM approach does not assume equal correlations across repeated outcomes measures, thus, allowing us to thoroughly model within-cluster correlations across measurement times (Muth et al., 2016).
To model main effects of treatment condition, we specified fixed and random effects of time in the LMM using time and treatment group as predictors. Specifically, we used treatment by time interactions to examine group differences in growth rates of change for outcome measures. Of note, all statistical analyses included sex as a covariate given documented sex-differentiated drinking patterns (Wilsnack, Wilsnack, & Wolfgang Kantor, 2013). Females were coded as the reference group (0 = female, 1 = male). ADHD medication status was not correlated with any of the variables in the model and therefore was not included. The alpha of .05 was set to represent statistical significance. We allowed random intercept and slope for time to vary across individuals. We also explored a priori cross-level interactions for depression as a baseline moderator on the primary outcome measure, alcohol-related negative consequences.
Results
Comparison of Treatment Conditions
Alcohol Related Negative Consequences (BYAACQ).
The LMM examining alcohol-related negative consequences yielded a significant effect of time (p <.01), suggesting that alcohol-related negative consequences decreased over time across both treatment conditions. No statistically significant differences were evident between BMI+BA and BMI+SC in alcohol-related negative consequences (p = .10) and growth rate (time x treatment) between the two groups at 1-month (p=.65) or 3-month follow-ups (p =.70). Effect sizes (Table 3) were slightly larger for participants in BMI+BA relative to the BMI+SC on the BYAACQ, though they were not statistically significantly different. Parameter estimates are reported in Table 4.
Table 3.
Means (SD) and Effect Sizes (d) for Outcomes
| Baseline | Post | 1-M FU | 3-M FU | ||
|---|---|---|---|---|---|
| BYAACQ | BMI+BA | 7.02 (5.02) | 6.57 (4.97) | 4.89 (3.54) | 5.92 (5.60) |
| N | 50 | 42 | 36 | 37 | |
| d | -- | .09 | .48 | .21 | |
| BMI+SC | 5.42 | 5.49 | 4.15 | 4.78 | |
| N | 57 | 51 | 46 | 40 | |
| d | -- | .12 | .31 | .15 | |
| DDQ | BMI+BA | 16.10 | 12.64 | 11.47 | 10.94 |
| N | 49 | 42 | 36 | 37 | |
| d | -- | 0.31 | 0.47 | 0.56 | |
| BMI+SC | 13.75 | 9.49 | 7.15 | 8.63 | |
| N | 57 | 50 | 45 | 40 | |
| d | -- | 0.40 | 0.77 | 0.58 | |
| BDI | BMI+BA | 14.76 (11.80) | 10.60 (11.35) | 9.25 (11.35) | 8.47 (9.43) |
| N | 50 | 51 | 46 | 40 | |
| d | -- | .37 | .47 | .58 | |
| BMI+SC | 12.28 (10.39) | 9.92 (10.50) | 7.71 (8.52) | 8.02 (8.84) | |
| N | 49 | 42 | 36 | 38 | |
| d | -- | .22 | h | .43 |
Note. Effect sizes reflect change from baseline for those individuals completing each follow-uptime point; all effect sizes were not significantly different between treatment conditions; SD= standard deviation; 1-M FU= 1-Month Follow-Up; 3-M FU= 3-Month Follow-up; d= within group effect size from baseline; small effect (d=.2); medium effect (d=.5); large effect (d=.8); BYAACQ= Brief Young Adult Alcohol Consequences Questionnaire; DDQ= Daily Drinking Questionnaire; BDI = Beck Depression Inventory.
Table 4.
Linear Mixed Model Parameter Estimates: Predicting Symptom Reduction Across Treatment
| Outcome Variable | Est | SE | t | Sig | 95% CI Low | 95% CI High |
|---|---|---|---|---|---|---|
|
| ||||||
|
BYAACQ
| ||||||
| Intercept | 5.64 | .38 | 14.83 | p<.001 | 4.89 | 6.38 |
| Time | −.36 | .14 | −2.59 | p<.01 | −.64 | −.09 |
| Sex | −1.21 | .76 | −1.59 | p=.12 | −1.59 | .17 |
| Treatment Group | 1.28 | .76 | 1.68 | p=.10 | −.21 | 2.77 |
| Time*Treatment | −.11 | .28 | −.38 | p=.70 | −.66 | .44 |
|
| ||||||
|
DDQ
| ||||||
| Intercept | 11.24 | 0.71 | 15.77 | p<.001 | 9.84 | 12.64 |
| Time | −0.48 | 0.14 | −3.38 | p<.001 | −0.76 | −0.20 |
| Sex | −5.05 | 1.43 | −3.54 | P<.001 | −7.84 | −2.26 |
| Treatment Group | 4.12 | 1.43 | 2.88 | p=.005 | 1.31 | 6.92 |
| Time*Treatment | 0.12 | 0.29 | 0.43 | p=.67 | −0.44 | 0.68 |
|
| ||||||
|
BDI
| ||||||
| Intercept | 10.67 | .85 | 12.46 | p<.001 | 8.96 | 12.31 |
| Time | −.74 | .09 | −7.82 | p<.001 | −.92 | −.55 |
| Sex | 2.04 | 1.71 | 1.20 | p=.23 | −1.30 | 5.38 |
| Treatment Group | 1.69 | 1.71 | .99 | p=.33 | −1.67 | 5.04 |
| Time*Treatment | −.30 | .19 | −1.61 | p=.11 | −.67 | .07 |
|
| ||||||
|
BFIS
| ||||||
| Intercept | 3.94 | .29 | 13.60 | p<.001 | 3.38 | 4.51 |
| Time | .12 | .11 | 1.13 | p=.26 | .009 | .34 |
| Sex | .87 | .58 | 1.50 | p=.14 | −.27 | 2.00 |
| Treatment Group | −.61 | .58 | −1.05 | p=.30 | −1.74 | .53 |
| Time*Treatment | −.27 | .22 | −1.24 | p=.22 | −.71 | .16 |
Note. Sex reference groups = women (0); Treatment reference group = Active Control; SE= standard error; Sig= significance; CI = confidence interval; BYAACQ= Brief Young Adult Alcohol Consequences Questionnaire; DDQ= Daily Drinking Questionnaire; BDI = Beck Depression Inventory; BFIS= Barkley Functional Impairment Scale.
Alcohol Use (DDQ).
The LMM DDQ model revealed significant mean differences between BMI+BA and BMI+SC at baseline (p <.005), such that participants in the BMI+BA condition reported drinking more at baseline than those in the BMI+SC condition. There was an effect of time (p <.001), which suggests that DDQ decreased over time in both conditions (see Table 3). In the BMI+SC group, students reported decreases in number of weekly drinks from baseline to 3-month follow-up from approximately 14 to 9. Effect size estimates are presented in Table 3 and indicate similar effects on weekly drinks at 3-month follow-up. No difference in growth rate between groups was evident (p = .68). See Table 4.
Depressive Symptoms (BDI).
The LMM examining depressive symptoms yielded a significant effect of time (p <.001), suggesting that BDI decreased over time across both treatment conditions. Effect size estimates are presented in Table 3 and indicate relatively stronger effects on depressive symptoms for participants in the BMI+BA condition relative to those in the BMI +SC condition. No statistically significant differences were evident between BMI+BA and BMI+SC in depressive symptoms (p = .33) and in growth rate (time x treatment) between the two groups (p =.11). Parameter estimates are reported in Table 4.
Functional Impairment (BFIS).
The LMM examining functional impairment showed a non-significant effect of time (p <.26), such that functional impairment did not decrease over time in either condition. Effect size estimates are presented in Table 3 and indicate similar effects across conditions. No significant differences in means across time points (p = .30) or growth rates (p =.22) were evident between BMI+BA and BMI+SC (see Table 4).
Moderation Analyses
Depressive Symptoms (BDI).
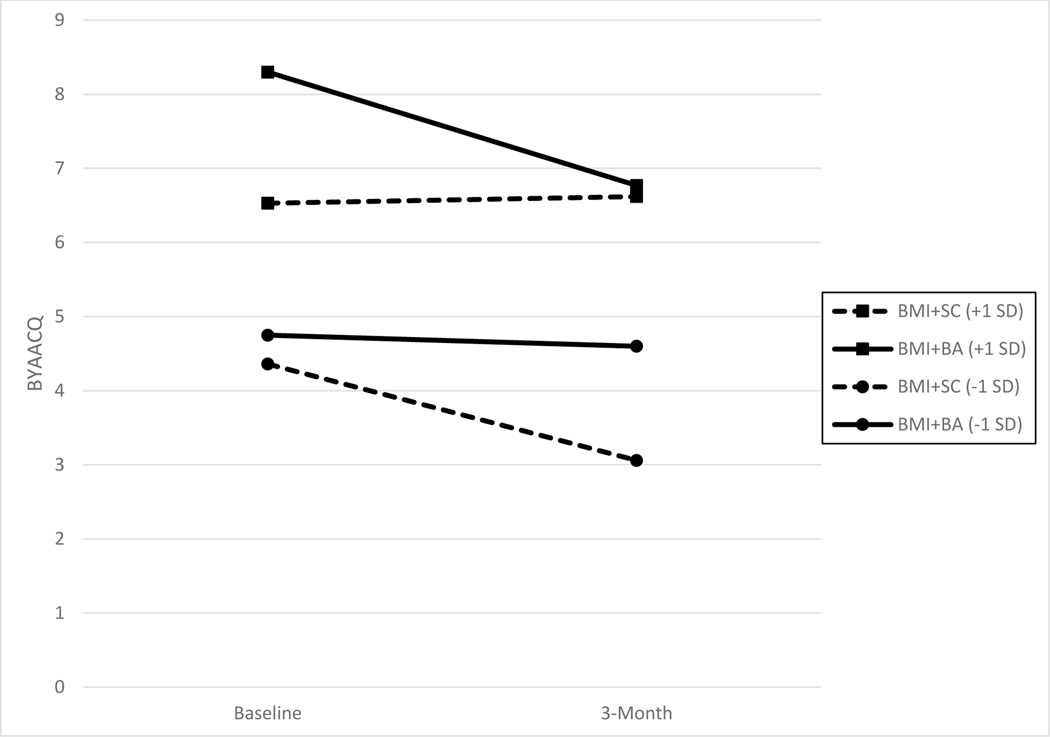
In exploratory moderation analyses, there was a significant interaction between treatment, time, and baseline depressive symptoms on alcohol-related negative consequences (the primary outcome variable) three months following treatment, controlling for alcohol use (i.e., DDQ; Table 5). As depicted in Figure 2, there were significant treatment effects, such that participants who reported more baseline depressive symptoms evidenced greater reductions in alcohol-related negative consequences over time following BMI+BA compared to participants in the BMI+SC group (B = −0.03, SE = 0.02, p < 0.05). Follow-up simple slope analyses probing this interaction effect revealed that individuals in the BMI+BA condition experienced more reductions in BYAACQ than those in BMI+SC condition at higher levels of baseline depressive symptoms (1SD or greater above the average), but not at average or lower levels. Conversely, individuals in the BMI+SC condition experienced more reductions in BYAACQ relative to those in the BMI+SC condition at lower levels of baseline depressive symptoms (1 SD or less below the average) but not at average or higher levels. Significant moderation was not observed at the 1-month follow-up period.
Table 5.
Summary of Three-way Interaction between Treatment, Time and Moderator on BYAACQ
| Moderator | Est | SE | t | Sig | 95% CI Low | 95% CI High |
|---|---|---|---|---|---|---|
|
| ||||||
|
BDI
| ||||||
| Intercept | 5.28 | .43 | 12.15 | p<.001 | 4.43 | 6.14 |
| Time | −.31 | .19 | −1.62 | p=.11 | −.68 | .07 |
| Sex | −.41 | .67 | .61 | p=.54 | −1.72 | .90 |
| Treatment Group | .56 | .65 | 1.34 | p=.18 | −.71 | 1.82 |
| DDQ | .19 | .04 | 5.31 | p<.001 | .12 | .26 |
| BDI | .13 | .03 | 4.27 | p<.001 | .06 | .18 |
| Time*Treatment | −.02 | .28 | −.06 | p=.95 | −.56 | .53 |
| Time*Treatment*BDI | −.03 | .02 | −1.99 | p<.05 | −.10 | −.005 |
Note. Sex reference groups = women (0); Treatment reference group = Active Control; SE= standard error; Sig= significance; CI = confidence interval; BYAACQ= Brief Young Adult Alcohol Consequences Questionnaire; DDQ = Daily Drinking Questionnaire; BDI = Beck Depression Inventory.
Figure 2.
Moderation Effects for Alcohol-Related Negative Consequences by Depressive Symptoms (BDI)
Note. BDI= Beck Depressive Inventory; BYAACQ= Brief Young Adult Alcohol Consequences Questionnaire; BMI= brief motivational intervention for alcohol use; BA= behavioral activation; SC= supportive counseling; SD= standard deviation.
Discussion
This is the first study to evaluate alcohol intervention approaches with a high-risk subpopulation of heavy drinkers with ADHD, a group who may require a more intensive and comprehensive approach to reduce problematic alcohol use than a standard single session of BMI. We examined the efficacy of BMI+BA relative to BMI+SC at reducing alcohol-related negative consequences among college students with ADHD over a 3-month follow-up period. Additional outcomes (i.e., total weekly drinks, depressive symptoms, functional impairment) were also examined between groups over time, given the theoretical links between BA and these outcomes (e.g., engaging in enjoyable and important activities to increase mood; identifying, planning, and executing observable, goal-directed activities). Exploratory moderation analyses were used to examine for whom BMI+BA produces greater reductions in alcohol-related negative consequences relative to BMI+SC.
There were no significant differences in outcomes for the sample as a whole; in both conditions, students reported significant reductions in both alcohol use and alcohol-related negative consequences from baseline to 3-month follow-up (and 1-month follow-up). Indeed, BMI is a gold-standard alcohol intervention for college students, more broadly (Tanner-Smith & Lipsey, 2015). Our results highlight the importance of BMI in alcohol intervention, perhaps especially with the addition of ADHD psychoeducation delivered in MI style with personalized feedback. Psychoeducation delivered in MI style may be especially effective in illuminating problem areas for many college students with ADHD and is consistent with emerging college ADHD interventions unselected for drinking behaviors, which include ADHD psychoeducation as a foundational intervention component (Anastopolus & King, 2015). Our results expand upon prior intervention work among college students with ADHD by showing that, on average, students with ADHD benefit from BMI + ADHD psychoeducation and either supportive counseling (i.e., establishing and discussing student-led topics) or BA. Prior research, has indicated that single sessions of BMI result in small effect size changes in alcohol use and alcohol-related problems (e.g., Murphy et al., 2015; Tanner-Smith & Lipsey, 2015). With the addition of BA (or SC), we found small effects on negative alcohol consequences and medium effects on alcohol use at 3-month follow-up. Our effect sizes may have been slightly larger than traditional BMI because of the addition of ADHD psychoeducation (delivered in MI style) as well as the addition of BA or SC.
Both BMI+BA and BMI+SC produced changes over time in depressive symptoms across 3-month follow-up, with larger effect sizes in the BMI+BA condition. Indeed, it is surprising that there were not significant differences in depressive symptom reduction across groups given that BA is an evidence-based intervention for depression that targets environmental reward which is theorized to be deficient in depressed individuals (Reynolds et al., 2011). It may be that the dose of BA provided in the BMI+BA program (i.e., two, 1-hour sessions plus a follow-up phone call) was simply not intensive enough to statistically outperform the active control condition (i.e., use of daily diaries, establishing student-led topics without specific use of cognitive-behavioral skills). In the spirit of brief interventions for alcohol use and related negative consequences (which typically consist of only 1 assessment and 1–2 intervention sessions; Carey et al., 2016), BA within the BMI+BA condition was delivered over the course of only 2 intervention sessions and a brief call (see Table 2). This dosage is substantially less than traditional evidence-based BA treatments for depression, which typically involve 10–12 sessions (Lejuez, Hopko, Acierno, Daughters, & Pagoto, 2011). Many treatments for college students with ADHD last 8–12 weeks (Anastopoulos & King, 2015; Solanto et al., 2018) to yield sustained, meaningful change in areas of impairment and emotional well-being. Given that ADHD is a chronic condition with multi-domain impairments (Weyandt & DuPaul, 2008), characterized by performance deficits and poor follow-through, it may be that additional BA sessions would result in stronger effects of BMI+BA on depression. Taken together, this preliminary finding suggests that, on average, short-term interventions with either BA or SC may be beneficial for this higher-risk comorbid population (Pedrelli et al., 2019).
Unexpectedly, neither treatment produced significant changes in ADHD-related functional impairment. At baseline, many participants self-reported low levels of impairment, despite their descriptions during ADHD assessments of impairment, corroborated by parents and transcript data (e.g., repeating classes). It is very possible that the MI-enhanced ADHD psychoeducation in both conditions (see Vasko et al., 2019) increased participants’ awareness of their areas of difficulty. Given that functional impairment data were collected via self-report only, students may have been more cognizant of their difficulties after the MI-delivered ADHD psychoeducation. It is also possible that the MI-delivered ADHD psychoeducation itself was a powerful treatment component; however, given the design of the current study to rigorously evaluate the addition of BA, we cannot isolate effects of MI-delivered psychoeducation alone.
In an effort to maximize available resources and make treatments as efficient as possible, it is important to examine for whom more intensive approaches are warranted. The exploratory moderation analyses suggested that the addition of BA may be clinically indicated for college students with ADHD who presented at baseline with elevated levels of depressive symptoms. Students with elevated baseline depressive symptoms demonstrated greater reductions in their alcohol-related negative consequences at 3-month follow-up (but not 1-month follow-up data) if they received BMI+BA. Conversely, college students with ADHD who reported low depressive symptoms at baseline saw greater reductions in alcohol-related negative consequences in BMI+SC compared to BMI+BA. Indeed, studies have demonstrated that depressive symptoms predict poorer response to BMI interventions (Dennhardt & Murphy, 2011) and adaptations to BMI that address coping skills and enhance substance-free reward may be especially important among those with elevated baseline depressive symptoms (Murphy et al., 2019; Murphy et al., 2012; Pedrelli et al., 2019). Given that comorbid ADHD and depression is associated with more impairment than either disorder alone (Chronis-Tuscano et al., 2010), it may be important to also evaluate levels of depressive symptoms at intake to identify students who could benefit from a more intensive intervention (i.e., BMI+BA) to reduce alcohol-related negative consequences.
Strengths, Limitations, and Future Directions
This is the very first study to: (1) investigate an intervention specifically designed to reduce problem drinking in college students with ADHD, (2) integrate BMI, MI-delivered ADHD psychoeducation, and BA in alcohol intervention, and (3) explore clinically-meaningful treatment moderators to identify for whom BMI+BA is warranted (i.e., treatment personalization). Prior research shows that students with self-regulation difficulties and high levels of impulsivity (i.e., core characteristics of ADHD) are less likely to respond to standard BMI (Carey et al., 2007; Ewing et al., 2009), supporting the importance of developing interventions that include additional elements for students with ADHD. Additionally, the current study was executed under a rigorous experimental design with a gold-standard comparison intervention (BMI+SC) to understand whether the addition of brief BA outperforms SC.
The results of this RCT need to be considered in the context of its limitations. This was a treatment development study and consequently sample size was relatively small, but consistent with others (e.g., Pedrelli et al., 2019). A larger sample would allow us to expand upon and replicate treatment moderators observed in the current sample. In the spirit of treatment efficiency, it may be the case that not all students with ADHD engaging in problem drinking require intervention beyond BMI, psychoeducation, and supportive counseling, which employs key helping skills shown to evoke behavior change (Hill, 2009). Another limitation is that the BA+BMI group reported higher levels of depressive symptoms at baseline than the BMI+SC; this reduction could represent a regression toward the mean. Future trials should attempt replicate our findings and explore this possibility.
Additionally, in subsequent trials, a wider range of assessment methods should be employed; ecological momentary assessment may provide proximal reports of alcohol-related negative consequences, mood symptoms, activity scheduling/completion, illuminating the unfolding of these behaviors over time. Although we coded sessions for fidelity (including for the absence of BA in the BMI+SC condition), it may also be helpful for future studies to employ cross-coding of sessions (i.e., independent evaluators who are blind to treatment condition and code with the other treatment condition’s content checklist). A limitation of the current study is that may have cross-contamination may have occurred during fidelity checking. Additionally, outcome data were collected via self-report, only. Given the sensitive nature of the study (e.g., underage drinking), parent data were only collected at baseline to confirm ADHD diagnoses and consent to contact parents was not required for participation. Parents’ corroboration of ADHD symptoms and impairment is recommended for assessing individuals with ADHD, when possible, (Barkley, 2006) but becomes increasingly difficult as youth age into emerging adulthood; few studies have followed this recommendation when assessing college students with ADHD (Dvorsky, Langberg, Molitor, & Bourchtein, 2016). Additionally, this was an NIAAA-funded study focused on drinking behavior and therefore we did not want to require parent participation. In this study we requested that participants grant permission to contact their parents about their ADHD symptoms, but did not exclude students who did not feel comfortable doing so. We were very conservative in our assessment approach. Diagnoses were made based on expert team consensus (including two licensed clinical psychologists) using a semi-structured diagnostic interview and student and (when available) parent rating scales assessing current/childhood ADHD symptoms and cross-domain impairment. Additionally, the majority of participants reported a previous diagnosis of ADHD during their assessment. Still, the lack of parent report on all participants could have impacted our ability to accurately capture symptoms and impairment. Future research should continue to attempt to obtain parent ratings of ADHD symptoms while maintaining the confidentiality of students in the study. Individuals with ADHD often have difficulty reporting on their own impairment (Sibley et al., 2012), so additional impairment outcomes, perhaps corroborated by parents or other significant others, would bolster findings. Longer follow-up assessments to assess sustained effects should also be considered, especially given that students with ADHD are at for persistent patterns of heavy drinking and poor follow-through with interventions (Tarter et al., 2008).
This study included students from a single 4-year, large, public university. Larger, more diverse samples at more than one university should be recruited to assess generalizability. Future work should also examine BMI+BA in community colleges (i.e., 2-year institutions), as well as among youth who do not pursue post-secondary schooling. Youth with ADHD are less likely to attend a 4-year institution vs. vocational/community colleges (Kuriyan et al., 2013). Implementing a BMI+BA in a broader array of educational settings would therefore be an important extension of this work to enhance generalizability.
It may also be beneficial for studies to investigate the effects of BMI+BA on other risk behaviors. For example, youth with ADHD are more likely to engage in risky sexual behavior, be involved in an early pregnancy, and have higher levels of drug-related impairment relative to their non-ADHD peers (Huggins, Rooney, Chronis-Tuscano, 2015; Meinzer et al., 2017; Rooney et al., 2012). BMI+BA may address other hazardous behaviors via personalized feedback on actual vs. ideal behaviors (BMI; Walters & Neighbors, 2005) and by replacing health risk behaviors with goal-directed substance-free behaviors (Lejuez et al., 2011).
Additional expansions of the current findings include elucidating why individuals receiving intervention make behavior change and for who. Consistent with foundational theories of substance misuse (e.g., behavioral economics), additional research should evaluate mechanisms of change in treatment. It is possible that engagement in goal-directed activities and access to substance-free reward across treatment may lead to reductions in problem alcohol use, depressive symptoms, or other negative outcomes (Murphy et al., 2019). Future research should also include finer-grained alcohol-related outcomes. It is currently unknown whether certain intervention components in ADHD lead to increased use of protective behavioral strategies or other cognitive-behavioral skills designed to reduce alcohol problems, and whether such effects are sustained over time (Magil et al., 2017). Additionally, given sex differences in both ADHD symptom presentation and alcohol use (Geisner, Larimer, & Clayton, 2004; Levy, Hay, Bennett, & McStephen, 2004), it would be beneficial for a future, larger randomized controlled trial to examine whether there are differences in treatment effects based on participant sex.
Though the current study controlled for therapist contact by implementing supportive counseling as a control comparison to behavioral activation, the current study did not examine whether BMI+SC or BMI+BA differed from BMI alone. Additionally, all participants received ADHD psychoeducation in MI style which could have bolstered the impact of both treatment conditions. This could have important implementation implications; traditional BMI is typically brief (e.g., 1–2 sessions) compared to the 4 session + brief check-in format that was employed in the BMI+SC and BMI+BA conditions. Should BMI alone result in equivalent improvements in alcohol-related negative consequences for all or subgroups of college students with ADHD, its implementation could aid in conserving mental health resources on college campuses.
Another important direction for future research involves evaluating the utility of supplementing the existing BMI+BA intervention with additional content to increase gains over time. This could come in several forms. For instance, the number of BA sessions could be increased to examine whether a higher “dose” of BA produces high magnitude and sustained effects on these outcomes, consistent with our findings that students with more depressive symptoms benefited the most from BMI+BA. Alternatively, technology could be employed to provide individualized between-session reminders regarding scheduled activities to address performance deficits that characterize individuals with ADHD. For example, prior work has used personalized text messaging in relation to alcohol use (Teeters, Soltis, & Murphy, 2018). Providing between session reminders of individuals’ alcohol-related and goals and BA content may be especially salient for college students with ADHD given difficulties executing skills acquired in treatment (Barkley, 1997). Lastly, future studies should consider implementation of BMI+BA within the infrastructure of university (i.e., health centers or specialty ADHD clinics) and/or community clinics. In line with dissemination efforts to have existing systems adopt and sustain evidence-based treatments (Brown et al., 2017), relying on current campus resources could increase access to care for college students with ADHD.
Public Health Significance Statement.
College students with ADHD are at increased risk for alcohol-related negative consequences and alcohol use disorders. Brief motivational interventions (BMI), considered the gold standard college alcohol intervention, are less effective for students with ADHD characteristics. In this randomized controlled trial, we found no group differences in outcomes for the sample as a whole. However, analyses revealed that BMI plus behavioral activation and ADHD psychoeducation was more effective than standard BMI for college students with ADHD who had elevated depressive symptoms at baseline.
Acknowledgments
This research was supported by a grant from NIAAA (R34 AA022133; PI: Chronis-Tuscano).
Footnotes
There were 6 participants with no baseline data (i.e., participant was administered a diagnostic interview but did not complete the baseline questionnaires). Analyses were conducted without those participants and all results remained consistent. Additionally, a logistic regression examined group differences on demographic variables between participants who dropped out of the study prior to receiving any treatment and those who completed at least one session. There were no significant differences between groups.
References
- Anastopoulos AD, DuPaul GJ, Weyandt LL, Morrissey-Kane E, Sommer JL, Rhoads LH, … & Gudmundsdottir BG (2018). Rates and patterns of comorbidity among first-year college students with ADHD. Journal of Clinical Child & Adolescent Psychology, 47(2), 236–247. doi: 10.1080/15374416.2015.1105137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastopoulos AD & King KA (2015). A cognitive-behavior therapy and mentoring program for college students with ADHD. Cognitive and Behavioral Practice, 22(2), 131–151. 10.1016/j.cbpra.2014.01.002 [DOI] [Google Scholar]
- Arria AM, Caldeira KM, Allen HK, Vincent KB, Bugbee BA, & O’Grady KE (2016). Drinking like an adult? Trajectories of alcohol use patterns before and after college graduation. Alcoholism: Clinical and Experimental Research, 40(3), 583–590. doi: 10.1111/acer.12973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor T, Higgins-Biddle J, Saunders J, & Monteiro M. (2001). AUDIT: The alcohol use disorders identification test. Guide-lines for use in primary care. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Baker L, Prevatt F, & Proctor B. (2012). Drug and alcohol use in college students with and without ADHD. Journal of Attention Disorders, 16(3), 255–263. Doi: 10.1177/1087054711416314 [DOI] [PubMed] [Google Scholar]
- Barkley RA (2006). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (3rd ed.). New York: Guilford. [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. [DOI] [PubMed] [Google Scholar]
- Barkley RA (2011a). Barkley Adult ADHD Rating Scale–IV (BAARS-IV). New York, NY: Guilford Press. [Google Scholar]
- Barkley RA (2011b). Barkley functional impairment scale (BFIS). New York: Guilford Press. [Google Scholar]
- Beck AT, Brown G & Steer RA (1996). Beck Depression Inventory II Manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Borsari, Neal, Collins, & Carey (2001).
- Bowirrat A & Oscar-Berman M. (2005). Relationship between dopaminergic neurotransmission, alcoholism, and reward deficiency syndrome. Neuropsychiatric Genetics, 132B, 29–37. Doi: 10.1002/ajmg.b.30080 [DOI] [PubMed] [Google Scholar]
- Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Collins LM, Naihua Duan N, Mittman BS, Wallace A, Tabak RG, Ducharme L, Chambers DA, Neta G, Wiley T, Landsverk J, Cheung K, & Cruden G. (2017). An overview of research and evaluation designs for dissemination and implementation. Annual Review of Public Health, 38, 1–22. 10.1146/annurev-publhealth-031816-044215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2007). Which heavy drinking college students benefit from a brief motivational intervention? Journal of Consulting and Clinical Psychology, 75, 663. 10.1037/0022-006X.75.4.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, & Hollon SD (1998). Defining empirically supported therapies. Journal of consulting and clinical psychology, 66(1), 7. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, & Lahey BB (2010). Very early predictors of adolescent depression and suicide attempts in children and adolescents with attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 67(10), 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychological bulletin, 112(1), 155. [DOI] [PubMed] [Google Scholar]
- Collins, Parks, & Marlatt (1985).
- DeMartini KS, & Carey KB (2012). Optimizing the use of the AUDIT for alcohol screening in college students. Psychological Assessment, 24(4), 954–963. 10.1037/a0028519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennhardt AA, & Murphy JG (2011). Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors, 25(4), 595–604. doi: 10.1037/a0025807 [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Barrera M Jr, Martell C, Munoz RF, & Lewinsohn PM (2011). The origins and current status of behavioral activation treatments for depression. Annual Review of Clinical Psychology, 7, 1–38. 10.1146/annurev-clinpsy-032210-104535 [DOI] [PubMed] [Google Scholar]
- Dvorsky MR, Langberg JM, Molitor SJ, & Bourchtein E. (2016). Clinical utility and predictive validity of parent and college student symptom ratings in predicting an ADHD diagnosis. Journal of Clinical Psychology, 72(4), 401–418. 10.1002/jclp.22268 [DOI] [PubMed] [Google Scholar]
- Ewing SWF, LaChance HA, Bryan A, & Hutchison KE (2009). Do genetic and individual risk factors moderate the efficacy of motivational enhancement therapy? Drinking outcomes with an emerging adult sample. Addiction Biology, 14, 356–365. doi: 10.1111/j.1369-1600.2009.00149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JB, Karg RS, & Spitzer RL (2016). Structured clinical interview for DSM-5 disorders: SCID-5-CV clinician version. American Psychiatric Association Publishing. [Google Scholar]
- Furukawa E, Bado P, Tripp G, Mattos P, Wickens JR, Bramati IE, Alsop B, Meireles Ferreira F, Lima D, Tovar-Moll F, Sergeant JA, & Moll J. (2014). Abnormal striatal BOLD responses to reward anticipation and reward delivery in ADHD. PLOS ONE, 9(2), e89129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, & Neighbors C. (2004). The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors, 29(5), 843–848. 10.1016/j.addbeh.2004.02.024 [DOI] [PubMed] [Google Scholar]
- Ham LS & Hope DA (2003). College students and problematic drinking: A review of the literature. Clinical Psychology Review, 23(5), 719–759. doi: 10.1016/S0272-7358(03)00071-0 [DOI] [PubMed] [Google Scholar]
- Hill CE (2014). Helping skills: Facilitating exploration, insight and action (4th Ed). Washington, DC: American Psychological Asoociation. [Google Scholar]
- Huggins SP, Rooney M, Chronis-Tuscano A. (2015). Risky secual behavior among college students with ADHD: Is the mother-child relationship protective? Journal of Attention Disorders, 19(3), 240–250. 10.1177/1087054712459560 [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Miech RA (2014). Monitoring the Future National Survey Results on Drug Use, 1975–2013. Volume 2, College Students & Adults Ages 19–55. Institute for Social Research. [Google Scholar]
- Joyner KJ, Pickover AM, Soltis KE, Dennhardt AA, Martens MP, & Murphy JG (2016). Deficits in access to reward are associated with college student alcohol use disorder. Alcoholism: Clinical and Experimental Research, 40(12), 2685–2691. DOI: 10.1111/acer.13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, & Read JP (2005). Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcoholism: Clinical and Experimental Research, 29(7), 1180–1189. 10.1097/01.ALC.0000171940.95813.A5 [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad J, Barnett NP, Strong DR, & Borsari B. (2008). Validation of the 30-day version of the brief young adult alcohol consequences questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs, 69(4), 611–614. 10.15288/jsad.2008.69.611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Adler LA, Barkley RA, Chatterji S, Faraone SV, . . . Van Brunt DL (2010). Structure and diagnosis of adult ADHD: Analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Archives of General Psychiatry, 67(11), 1168–1178. 10.1001/archgenpsychiatry.2010.146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyan AB, Pelham WE, Molina BSG, Waschbusch DA, Gnagy EM, … Kent K,M (2013). Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology, 41(1), 27–41. doi: 10.1007/s10802-012-9658-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, & Pagoto SL (2011). Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification, 35, 111–161. doi: 10.1177/0145445510390929 [DOI] [PubMed] [Google Scholar]
- Levy F, Hay DA, Bennett KS, & McStephen M. (2005). Gender differences in ADHD subtype comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry, 44(4), 368–376. 10.1097/01.chi.0000153232.64968.c1 [DOI] [PubMed] [Google Scholar]
- Magill M, Colby SM, Orchowski L, Murphy JG, Hoadley A, Brazil LA, & Barnett NP (2017). How does brief motivational intervention change heavy drinking and harm among underage young adult drinkers? Journal of Consulting and Clinical Psychology, 85, 447–458. doi: 10.1037/ccp0000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaux JB, Green A, & Broussard L. (2009). ADHD in the college student: A block in the road. Journal of Psychiatric and Mental Health Nursing, 16(3), 248–256. 10.1111/j.1365-2850.2008.01349.x [DOI] [PubMed] [Google Scholar]
- Meinzer MC, LeMoine KA, Howard AL, Stehli A, Arnold LE, Hechtman L, … & Swanson JM (2017). Childhood ADHD and involvement in early pregnancy: mechanisms of risk. Journal of attention disorders. doi: 1087054717730610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Borsari B, Witkiewitz K, & Meshesha LZ (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology, 87(7), 657–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, & Martens M. (2012). A randomized controlled trial of a behavioral economic supplement to a brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology, 80(5), 876–886. Doi: 10.1037/a0028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Yurasek AM, Skidmore JR, Martens MP, MacKillop J, & McDevitt-Murphy ME (2015). Behavioral economic predictors of brief alcohol intervention outcomes. Journal of Consulting and Clinical Psychology, 83, 1033–1043. 10.1037/ccp0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muth C, Bales KL, Hinde K, Maninger N, Mendoza SP, & Ferrer E. (2016). Alternative models for small samples in psychological research: applying linear mixed effects models and generalized estimating equations to repeated measures data. Educational and psychological measurement, 76(1), 64–87. 10.1177/0013164415580432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Grimaldi EM, & LaBrie JW (2015). Parents’ and students’ perceptions of college alcohol risk: The role of parental risk perception in intentions to communicate about alcohol. Addictive behaviors, 42, 114–118. 10.1016/j.addbeh.2014.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park A, Sher KJ, & Krull JL (2008). Risky drinking in college changes as fraternity/sorority affiliation changes: A person-environment perspective. Psychology of Addictive Behaviors, 22, 219–229. doi: 10.1037/0893-164X.22.2.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, & Colder CR (2006). Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of Studies on Alcohol, 61(1), 169–177. 10.15288/jsa.2006.67.169 [DOI] [PubMed] [Google Scholar]
- Reynolds EK, MacPherson L, Tull MT, Baruch DE, & Lejuez CW (2011). Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: Depression and alcohol outcomes. Journal of Counseling Psychology, 58, 555–564. doi: 10.1037/a0024634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooney M, Chronis-Tuscano A, & Yoon Y. (2012). Substance use in college students with ADHD. Journal of Attention Disorders, 16, 221–234. doi: 10.1177/1087054710392536 [DOI] [PubMed] [Google Scholar]
- Rooney M, Chronis-Tuscano A & Huggins SL (2015). Disinhibition mediates the relationship between ADHD and problematic alcohol use in college students. Journal of Attention Disorders, 19(4), 313–327. doi: 10.1177/1087054712459885 [DOI] [PubMed] [Google Scholar]
- Rooney M, Chronis-Tuscano A & Huggins SL (2015). Disinhibition mediates the relationship between ADHD and problematic alcohol use in college students. Journal of Attention Disorders, 19(4), 313–327. doi: 10.1177/1087054712459885 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, & Grant M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction, 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Shemmassian SK, & Lee SS (2012). Comparing four methods of integrating parent and teacher symptom ratings of attention-deficit/hyperactivity disorder (ADHD). Journal of Psychopathology and Behavioral Assessment, 34(1), 1–10. doi: 10.1007/s10862-011-9262-5 [DOI] [Google Scholar]
- Sibley MH, Pelham WE, Gnagy EM, Waxmonsky JG, Waschbusch DA, Derefinko KJ….Kuriyan AB (2012). When diagnosing ADHD in young adults emphasize informant reports, DSM items, and impairment. Journal of Consulting and Clinical Psychology, 80(6), 1052–1061. doi: 10.1037/a0029098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solanto MS & Scheres A. (2018, November). Cognitive-Behavioral Intervention: Executive Function in College Students With ADHD. Symposium presented at the annual meeting of the Association for Behavioral and Cognitive Therapies, Washington, DC. [Google Scholar]
- Storch EA, Roberti JW, Roth DA (2004). Factor structure, concurrent validity, and internal consistency of the Beck Depression Inventory- Second Edition in a sample of college students. Depression and Anxiety, 19(3), 187–189. 10.1002/da.20002 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substante Abuse Treatment, 51,1–18. doi: 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Vanyukov M, & Kirisci L (2008). Etiology of substance use disorder: Developmental perspective. In Kaminer Y & Bukstein OG (Eds.), Adolescent substance abuse: psychiatric comorbidity and high-risk behaviors. New York: Routledge. [Google Scholar]
- Teeters KB, Soltis KE, & Murphy JG (2018). A mobile phone-based brief intervention with personalized feedback and text messaging is associated with reductions in driving after drinking among college drinkers. Journal of Studies on Alcohol and Drugs, 79(5), 710–719. 10.15288/jsad.2018.79.710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasko JM, Meinzer MC, Murphy JG, Oddo LE, McCauley KL, Rooney ME, Lejuez CW, & Chronis-Tuscano A. (2019). Brief intervention to reduce problem drinking in college students with ADHD. Cognitive and Behavioral Practice, 26(3), 506–521. 10.1016/j.cbpra.2019.02.003 [DOI] [Google Scholar]
- Walters ST & Neighbors C. (2005). Feedback interventions for college alcohol misuse: What, why and for whom? Addictive Behaviors, 30(6). 1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West SG (2009). Alternatives to randomized experiments. Current Directions in Psychological Science, 18(5), 299–304. 10.1111/j.14678721.2009.01656.x [DOI] [Google Scholar]
- Weyandt LL, & DuPaul GJ (2008). ADHD in college students: Developmental findings. Developmental Disabilities Research Reviews, 14, 311–319. doi: 10.1002/ddrr.38 [DOI] [PubMed] [Google Scholar]
- White A & Hingsonm R. (2013). The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Research: Current Reviews, 35(2), 201–218. [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Wilsnack RW, & Wolfgang Kantor L. (2013). Focus on: Women and the costs of alcohol use. Alcohol Research: Current Reviews, 35(2), 219–228. [PMC free article] [PubMed] [Google Scholar]
- Yoshimasu K, Barbaresi WJ, Colligan RC, Voigt RG, Weaver AL, & Katusic SK (2016). Mediating and moderating role of depression, conduct disorder or ADHD in developing adolescent substance use disorders: A population-based study. PloS one, 11(6), e0157488. 10.1371/journal.pone.0157488 [DOI] [PMC free article] [PubMed] [Google Scholar]