Abstract
Background:
Individuals affected by disasters are at risk for adverse mental health sequelae. Individuals living in the US Gulf Coast have experienced many recent major disasters, but few studies have explored the cumulative burden of experiencing multiple disasters on mental health.
Objective:
The objective of this study was to evaluate the relationship between disaster burden on mental health.
Methods:
We used data from 9,278 Gulf Long-term Follow-up Study participants who completed questionnaires on perceived stress, anxiety, depression, and post-traumatic stress disorder (PTSD) in 2011-2013. We linked 2005-2010 county-level data from the Spatial Hazard Events and Losses Database for the United States, a database of loss-causing events, to participant’s home address. Exposure measures included total count of loss events as well as severity quantified as property/crop losses per capita from all hazards. We used multilevel modeling to estimate odds ratios (OR) and 95% confidence intervals (CI) for each exposure-outcome relationship.
Results:
Total count of loss events was positively associated with perceived stress (ORQ4:1.40, 95% CI:1.21-1.61) and was inversely associated with PTSD (ORQ4:0.66, 95% CI 0.45-0.96). Total duration of exposure was also associated with stress (ORQ4:1.16, 95% CI 1.01-1.33) but not with other outcomes. Severity based on cumulative fatalities/injuries was associated with anxiety (ORQ4:1.31, 95% CI 1.05-1.63) and stress (ORQ4:1.34, 95% CI 1.15-1.57), and severity based on cumulative property/crop losses was associated with anxiety (ORQ4:1.42, 95% CI:1.12-1.81), depression (ORQ4:1.22, 95% CI:0.95-1.57) and PTSD (ORQ4:1.99, 95% CI:1.44-2.76).
Significance:
Higher natural hazard burden above and beyond individual disasters may increase risk for multiple adverse mental health outcomes.
Introduction
Natural hazards (1) such as floods, hurricanes and wildfires pose a significant threat to human health and productivity. Disasters resulting from these hazards cause tens of thousands of fatalities and affect hundreds of millions of people each year (2). In 2017, natural hazards affected an estimated 25 million Americans, or around 8% of the population, and led the Federal Emergency Management Agency (FEMA) to support 137 presidential disaster declarations and provide over $7.2 billion in public and individual assistance to address immediate housing and infrastructure needs (3). In addition to direct damages such as the immediate effects on human life and property, natural hazards can also cause broader indirect economic consequences, such as the disruption of trade and manufacturing (4).
Direct negative health consequences include personal physical injuries, whereas indirect adverse health consequences include witnessing the death or injury of a friend or family member (5). Additionally, traumatic experiences during and after a disaster from stressors such as fear of death, economic uncertainty, loss of life and/or property, and others may provoke symptoms of post-traumatic stress disorder (PTSD) (6). Individuals with PTSD are also at risk of developing secondary mental health disorders such as anxiety and depression (7).
Previous epidemiological studies have demonstrated positive associations between hurricanes (8-10), earthquakes (11), floods (7), fires (12), and heat waves (13), and mental health conditions such as PTSD and depression. Exposure to Hurricane Harvey in 2017 was found to be associated with PTSD, with 46% of participants meeting screening thresholds for PTSD (8). Similarly, studies of evacuees from the 2016 wildfires in the Fort McMurray area of Canada demonstrated significant incidence of PTSD, depression and insomnia (14). Although these singular events point to a relationship between mental health and disaster impacts, few studies have analyzed the impact of multiple disasters due to natural hazards across a defined geographic region such as the Gulf of Mexico and over a sustained period of time.
The Gulf region of the United States has been affected by multiple severe natural hazards (15) in the past two decades. The region is particularly susceptible to hurricanes, including major disasters such as Hurricanes Katrina (2005), Rita (2005), Gustav (2008), and Ike (2008), with damages from each hurricane exceeding billions of dollars (16). The Gulf region has also endured several standalone flooding events, droughts, thunderstorms, tornadoes and wind events. Although the acute health impacts from these large-scale events are relatively well understood, much less is known about the lasting mental health impacts across the region. The objective of this study is to assess the relationship between natural hazard burden and adverse mental health outcomes among residents living in the Gulf states.
Methods
Study Design and Population
The Gulf Long-term Follow-up Study (GuLF Study) is a large prospective cohort of 32,608 adults who trained for and/or participated in oil spill response and clean-up following the 2010 Deepwater Horizon disaster (17,18) (Figure S1). At enrollment (March 2011 – March 2013), participants completed a structured telephone interview on demographics, lifestyle and health. A subset of 11,193 English and Spanish-speaking participants living in the Gulf coast states (eastern Texas, Louisiana, Mississippi, Alabama and Florida) completed a home visit between May 2011 – May 2013, which included an interview on health and lifestyle factors, and mental health screening questionnaires.
Of the 11,193 home visit participants, 430 participants were missing information for at least one covariate. A further 1,240 participants did not provide responses for at least one mental health questionnaire, and we were unable to link natural hazard data by home address for 174 additional participants, yielding a primary analytic sample size of 9,349 (Figure 1).
Figure 1:
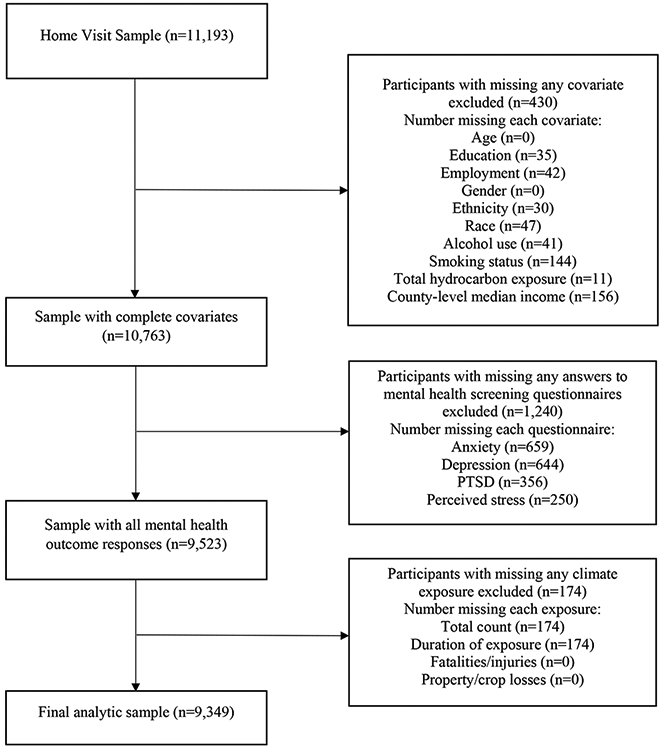
Study population selection criteria
Ethical Approval
This research was approved by the Institutional Review Board of the National Institute of Environmental Health Sciences. Written informed consent was obtained from all participants completing the home visit.
Mental Health Outcomes
Perceived Stress
We screened for perceived stress using a four-item version of the Perceived Stress Scale (19). Participants were asked how often, within the last month, they felt that they were losing control over their lives, felt that difficulties were piling up beyond their coping abilities, had confidence in their abilities to handle personal problems, or felt that things were going their way. For the first two questions, responses ranged from 0 (never) to 4 (very often), and for the last two questions responses ranged from 0 (very often) to 4 (never). We classified participants with a composite score (sum of items) of 9 or higher as being stressed per Cohen et al. (19).
Anxiety
Participants were screened for anxiety using the Generalized Anxiety Disorder 7-item (GAD-7) scale to identify probable cases of generalized anxiety disorder (GAD) (20). We asked participants if, over the previous two weeks, they experienced feeling nervous, anxious or on edge, not being able to stop or control worrying, worrying too much about different things, having trouble relaxing, being restless and unable to sit still, becoming easily annoyed or irritable, or feeling afraid as if something awful might happen. For each question, responses ranged from 0 (never) to 3 (nearly every day). Responses from each question were summed to provide a final score, and we classified participants with scores of 10 or greater as having anxiety per Spitzer et al. (20).
Depression
Participants were screened for depression using the Patient Health Questionnaire-8 (PHQ8) scale, validated for use in epidemiologic studies (21). We asked participants, over the past two weeks, how often they had little interest in doing things, felt down or depressed, had trouble with sleep or slept too much, felt tired or had low energy, had poor or increased appetite, felt bad about themselves, had trouble concentrating on things, or were moving too slowly or too quickly. Responses ranged from 0 (no days) to 14 (every day). Responses were summed, and we classified scores of 10 days or greater as having depression per Kroenke et al. (21).
Post-Traumatic Stress Disorder
Participants were screened for PTSD using the Primary Care PTSD (PC-PTSD) scale (22). Participants were asked if, within the past month and related to a specific past event, they experienced nightmares, went out of their way to avoid similar situations, were constantly on guard, or felt numb or detached from their surroundings. Responses were coded as 0 (no) or 1 (yes) and summed. We classified participants with scores of 3 or greater as having PTSD per Prins et al. (22).
Distress
A subset of 7,766 participants provided information on distress, so we analyzed this as a secondary outcome. Participants were screened for distress using the Kessler-6 Psychological Distress Scale (K6), a scale developed to identify cases of serious mental illness that impact functional ability (23). We asked participants if, over the previous 30 days, they felt nervous, hopeless, restless or fidgety, depressed, like everything was an effort, or worthless. Responses for each question ranged from 0 (none of the time) to 4 (all of the time). Responses were added into a total score, and we classified participants with scores of 13 or greater as being distressed per Kessler et al. (23).
Natural Hazard Burden
The Spatial Hazard Events and Losses Database for the United States (SHELDUS) is a database of loss-causing natural hazard events in the United States dating back to 1960 (24). SHELDUS 18.1 data provides county-level characteristics of United States hazard events including the event start and end dates, hazard type (e.g. hurricane, flooding event etc.), duration of event, and direct losses from the event such as per capita fatalities, injuries, absolute property, and absolute crop losses in US dollars. In the United States, a county or parish is a defined administrative subdivision of a state, and the sizes of counties vary significantly across and within states. For this study, we used data encompassing events from January 1, 2005 to December 31, 2010 affecting any county within the Gulf states of Florida, Alabama, Mississippi, Louisiana and Texas associated with any type of natural hazard. Potential biases included in loss data are discussed elsewhere (25).
The overall approach we used for the exposure assessment was to sum losses across all events affecting each county between 2005-2010 reported in the SHELDUS database including: 1) total count of loss events; 2) total duration in days across all events; 3) total fatalities/injuries per capita during the exposure period; and 4) total property/crop losses per capita during the exposure period.” We then linked this data to participant residential addresses at the time of enrollment. Counts for each type of loss were then categorized in quartiles for analysis.
For the total count and total duration exposure measures, we screened out minor loss events (e.g. from a severe thunderstorm) and focused solely on county-level events characterized as Billion Dollar events (26) using SHELDUS’ Major Disasters search functionality. We combined fatalities and injuries, for which per capita-adjusted values were provided in SHELDUS. We separately calculated property losses per capita and crop losses per capita, by dividing raw values for each provided in SHELDUS by county population as provided in the 2010 American Community Survey 5-year estimates (27). We then combined the calculated property and crop per capita losses. For each metric of natural hazard burden, we created quartiles within our sample distribution, with the lowest quartile serving as the reference group (Table 1).
Table 1:
Exposure definitions
| Name | Definition | Quartile Distributions | |||
|---|---|---|---|---|---|
| Quartile 1 (1-24%) |
Quartile 2 (25- 49%) |
Quartile 3 (50- 74%) |
Quartile 4 (75- 100%) |
||
| Total Count | Total number of billion-dollar events from 2005-2010 | 1-5 | 6 | 7-11 | 12-73 |
| Duration of Exposure | Total duration of exposure to all billion-dollar events from 2005-2010 in days | 1-9 | 10-13 | 14-16 | 17-570 |
| Fatalities/Injuries | Total fatalities and injuries per capita due to hazard events in 2005-2010 | 0-4.70 | 4.70-6.42 | 6.44-14.60 | 14.93-528.49 |
| Property/Crops | Total property and crop losses per capita in dollar amounts due to hazard events in 2005-2010 | $5-$875 | $886-$2,241 | $2,286-$17,135 | $17,247-$272,961 |
| Monetized Score | Values of $4 million were assigned to each fatality and $600,000 to each injurya. Dollar amounts for fatalities per capita, injuries per capita, property losses per capita and crop losses per capita were added together, and participants were categorized into quartiles per losses in dollar amounts. | $12-$7,394,288 | $7,793,602-$18,154,956 | $18,257,898-$39,466,709 | $40,609,909-$1,115,979,402 |
| N (%) | |||||
| Level 0 (0) | Level 1 (1-2) | Level 2 (2-3) | |||
| Cumulative Score | For each participant, a score of one was assigned if they were categorized in the top quartile for each individual parameter of severity: fatalities per capita, injuries per capita, property losses per capita, crop losses per capita | 3514 (38) | 5407 (58) | 428 (5) | |
Hahn, Daniel J., Emmanuelle Viaud, and Ross B. Corotis. 2017. “Multihazard Mapping of the United States.” ASCE-ASME Journal of Risk and Uncertainty in Engineering Systems, Part A: Civil Engineering 3 (3): 04016016. https://doi.org/10.1061/AJRUA6.0000897.
Additionally, we created two scores incorporating individual severity metrics using the raw data provided by SHELDUS. First, we assigned participants a score of 1 for each instance of being in the highest quartile of: aggregated fatalities per capita, injuries per capita, property losses per capita, and crop losses per capita. Scores were summed into a ‘Cumulative Score (0-4)’characterized as: Level 0 (score of 0), Level 1 (scores of 1-2), and Level 2 (scores of 3-4). The lowest category (Level 0) served as the reference group. Second, we assigned a value of $4 million to a fatality and $600,000 to an injury, per a previous paper using SHELDUS data (28). Participants were then categorized into quartiles of a ‘Monetized Score’ according to their total loss in dollar amounts, and the lowest quartile served as the referent group.
Statistical Analyses
We calculated descriptive statistics of study sample characteristics by quartiles of exposure. We assessed the relationship between natural hazard burden and mental health outcomes using a multilevel modeling approach with generalized estimating equations as described by Hubbard et al (29). We used multilevel modeling to simultaneously examine the effects of group-level and individual-level variables on individual-level outcomes, given that our exposures were at the county-level while health outcomes were individual. We used generalized estimating equations as the health outcomes of residents in the same neighborhood may be correlated and violate assumptions of independence in linear regression models (30). We accounted for these potential spatial correlations of outcomes at the county-level using a repeated statement. We estimated crude and adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) for each quartile or level compared to the lowest as the referent group.
For adjusted models, we identified potential confounders using a directed acyclic graph (Figure S2) (31). We considered individual-level characteristics, obtained via enrollment questionnaire: age (years), sex (male, female), race (white, black, other), ethnicity (Hispanic, non-Hispanic), smoking status (heavy current smoker, light current smoker, former smoker, never smoker), alcohol use (current drinker, former drinker, never drinker), educational attainment (< high school/equivalent, high school diploma/General Educational Development test, some college/2-year degree, ≥ 4-year college graduate) and employment status (working now, looking for work/unemployed, other). We also adjusted by individual-level ordinal estimates of total hydrocarbon exposure, as a proxy for oil spill exposure (32) as well as county-level median household income, obtained from the 2010 American Community Survey 5-year estimates by the U.S. Census Bureau (33) and categorized into quartiles per our sample distribution.
As PTSD has been most strongly associated with individual disaster events in the prior literature (5), we conducted additional analyses to better understand associations between natural hazard burden and PTSD. Based on prior literature on racial and occupational health disparities (34), we assessed the potential for effect-measure modification by race and oil spill cleanup work exposures using stratification (white, non-white) and restriction to a sub-cohort of oil-spill workers (N=7,456). We additionally stratified participants by median home visit date (before or after July 8, 2012) to assess the impact of response date on associations with PTSD as an effect-measure modifier.
Statistical Analysis System (SAS, Cary, NC) version 9.4 was used to conduct all statistical analyses.
Results
Sample population characteristics are shown by natural hazard exposure metrics (total count of events, total duration, fatalities/injuries per capita, property/crop losses per capita, cumulative score, monetized score) quartiles (<25th percentile, 25th-49th percentile, 50th-74th percentile, >75th percentile) (Tables S1, S2 and S3). Participants living in the highest vs. lowest quartile of loss event counts were less likely to be white (48% vs. 60%) and less likely to be a college graduate (14% vs. 22%) (Table S1). Participants living in the highest compared to lowest quartile for property/crop losses per capita were also less likely to be white (56% vs. 64%) and less likely to be a college graduate (11% vs. 22%) (Table S2).
In the primary analytic sample, total natural disaster event count was not clearly associated with anxiety, depression or PTSD. Odds ratios decreased with increasing quartiles, as compared to the lowest quartile. However, total count appeared to be associated with perceived stress in a suggestive dose-dependent manner (ORQ2 vs Q1 1.21, 95% CI 1.04-1.42; ORQ3 vs Q1 1.24, 95% CI 1.06-1.45; ORQ4 vs Q1 1.40, 95% CI 1.21-1.61; Table 2). Total duration of exposure was also not clearly associated with anxiety, depression or PTSD, with protective point estimates; however, duration was associated with stress, (ORQ4 vs Q1 1.16, 95% CI 1.01-1.33).
Table 2:
Estimated odds ratio (OR) associations between natural hazard burden and mental health outcomes (N=9,349)*
| Mental Health Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Anxiety (GAD) | Depression (PHQ8) | PTSD | Stress (Cohen) | ||||||
| Prevalence (N, %) | 2173 (23%) | 1469 (16%) | 486 (5%) | 2556 (28%) | |||||
| Natural Hazard Burden Exposure |
Quartile N (%) |
Cases | OR (95% CI) | Cases. | OR (95% CI) | Cases. | OR (95% CI) | Cases. | OR (95% CI) |
| Total Counta | |||||||||
| Quartile 1 | 1755 (19) | 354 | REF | 251 | REF | 82 | REF | 392 | REF |
| Quartile 2 | 2391 (26) | 618 | 1.26 (0.93, 1.70) | 448 | 1.17 (0.90, 1.52) | 153 | 1.17 (0.78, 1.78) | 703 | 1.21 (1.04, 1.42) |
| Quartile 3 | 2458 (26) | 606 | 1.19 (0.93, 1.52) | 402 | 1.05 (0.81, 1.35) | 160 | 1.30 (0.95, 1.78) | 667 | 1.24 (1.06, 1.45) |
| Quartile 4 | 2745 (29) | 622 | 0.88 (0.66, 1.16) | 388 | 0.86 (0.66, 1.13) | 95 | 0.66 (0.45, 0.96) | 820 | 1.40 (1.21, 1.61) |
| Duration of Exposurea | |||||||||
| Quartile 1 | 2471 (26) | 592 | REF | 427 | REF | 144 | REF | 620 | REF |
| Quartile 2 | 2105 (23) | 457 | 0.87 (0.68, 1.11) | 342 | 0.86 (0.68, 1.08) | 94 | 0.85 (0.60, 1.20) | 565 | 1.11 (0.93, 1.32) |
| Quartile 3 | 2711 (29) | 733 | 1.05 (0.81, 1.37) | 441 | 0.84 (0.64, 1.11) | 163 | 1.31 (0.81, 2.12) | 882 | 1.31 (1.16, 1.48) |
| Quartile 4 | 2062 (22) | 418 | 0.91 (0.72, 1.15) | 279 | 0.81 (0.65, 1.00) | 89 | 0.85 (0.57, 1.27) | 515 | 1.16 (1.01, 1.33) |
| Fatalities/Injuries per Capita | |||||||||
| Quartile 1 | 2134 (23) | 440 | REF | 302 | REF | 91 | REF | 459 | REF |
| Quartile 2 | 2852 (31) | 676 | 0.86 (0.65, 1.13)b | 424 | 0.84 (0.65, 1.08) | 138 | 0.97 (0.55, 1.72) | 892 | 1.32 (1.16, 1.51) |
| Quartile 3 | 2133 (23) | 546 | 1.16 (0.86, 1.57)b | 393 | 1.26 (0.94, 1.68) | 140 | 1.23 (0.82, 1.83) | 633 | 1.28 (1.06, 1.55) |
| Quartile 4 | 2230 (24) | 538 | 1.31 (1.05, 1.63)b | 370 | 1.20 (0.95, 1.51) | 121 | 1.28 (0.87, 1.88) | 598 | 1.34 (1.15, 1.57) |
| Property/Crop Damage per Capita | |||||||||
| Quartile 1 | 1550 (17) | 313 | REF | 236 | REF | 50 | REF | 376 | REF |
| Quartile 2 | 2662 (28) | 602 | 0.99 (0.78, 1.25)b | 365 | 0.79 (0.62, 1.00)b | 93 | 0.95 (0.68, 1.33)b | 782 | 1.17 (0.96, 1.42) |
| Quartile 3 | 2784 (30) | 645 | 1.17 (0.91, 1.51)b | 443 | 0.96 (0.75, 1.23)b | 167 | 1.60 (1.15, 2.22)b | 718 | 1.10 (0.82, 1.21) |
| Quartile 4 | 2353 (25) | 640 | 1.42 (1.12, 1.81)b | 445 | 1.22 (0.95, 1.57)b | 180 | 1.99 (1.41, 2.81)b | 706 | 1.19 (0.93, 1.52) |
| Cumulative Scorec | |||||||||
| Level 0 | 3514 (38) | 782 | REF | 502 | REF | 146 | REF | 1050 | REF |
| Level 1 | 5407 (58) | 1275 | 1.31 (1.07, 1.60)b | 895 | 1.35 (1.12, 1.63)b | 304 | 1.51 (1.14, 2.00)b | 1391 | 0.98 (0.83, 1.17) |
| Level 2 | 428 (5) | 143 | 1.88 (1.43, 2.47)b | 92 | 1.66 (1.24, 2.21)b | 40 | 1.99 (1.44, 2.76)b | 141 | 1.29 (1.03, 1.62) |
| Monetized Scored | |||||||||
| Quartile 1 | 2665 (29) | 572 | REF | 413 | REF | 120 | REF | 655 | REF |
| Quartile 2 | 1710 (18) | 379 | 0.92 (0.70, 1.22)b | 257 | 0.88 (0.66, 1.16) | 113 | 1.38 (0.93, 2.03) | 415 | 1.06 (0.87, 1.28)b |
| Quartile 3 | 2848 (30) | 744 | 1.11 (0.84, 1.46)b | 477 | 1.02 (0.72, 1.42) | 134 | 0.99 (0.63, 1.56) | 917 | 1.27 (1.07, 1.50)b |
| Quartile 4 | 2126 (23) | 505 | 1.28 (1.02, 1.60)b | 342 | 1.13 (0.88, 1.44) | 123 | 1.36 (0.90, 2.05) | 595 | 1.28 (1.07, 1.54)b |
Adjusted for age, education, employment, sex, race, ethnicity, alcohol use, smoking, total hydrocarbon exposure, and county-level median income
Incorporates NCEI-designated Billion-Dollar Disasters only
Linear Regression Test for Trend, P < 0.05
For each participant, a score of one was assigned if they were categorized in the top quartile for each individual exposure parameter of severity: fatalities per capita, injuries per capita, property losses per capita, crop losses per capita. Level 0 = score of 0, Level 1 = scores of 1-2, Level 2 = scores of 3-4
Values of $4 million were assigned to each fatality and $600,000 to each injury. Dollar amounts for fatalities per capita, injuries per capita, property losses per capita and crop losses per capita were added together, and participants were categorized into quartiles per losses in dollar amounts.
Among individual metrics of severity, fatalities/injuries was associated with anxiety (ORQ2 vs Q1 0.86, 95% CI 0.65-1.13; ORQ3 vs Q1 1.16, 95% CI 0.86-1.57; ORQ4 vs Q1 1.31, 95% CI 1.05-1.63) and perceived stress (ORQ2 vs Q1 1.32, 95% CI 1.16-1.51; ORQ3 vs Q1 1.28, 95% CI 1.06-1.5; ORQ4 vs Q1 1.34, 95% CI 1.15-1.57), with point estimates increasing with increasing quartiles, and suggestively associated with depression and PTSD (Table 2). Property/crop losses was associated with anxiety (ORQ2 vs Q1 0.99, 95% CI 0.78-1.25; ORQ3 vs Q1 1.17, 95% CI 0.91-1.51; ORQ4 vs Q1 1.42, 95% CI 1.12-1.81) and PTSD (ORQ2 vs Q1 0.97, 95% CI 0.55-1.72; ORQ3 vs Q1 1.23, 95% CI 0.82-1.83; ORQ4 vs Q1 1.28, 95% CI 0.87-1.88) in a dose-dependent manner, and suggestively associated with depression and perceived stress (Table 2).
With derived scores of severity, the Cumulative Score was associated with all four mental health outcomes: for anxiety (ORL1 vs L0 1.31, 95% CI 1.07-1.60; ORL2 vs L0 1.88, 95% CI 1.43-2.47), depression (ORL1 vs L0 1.35, 95% CI 1.12-1.63; ORL2 vs L0 1.66, 95% CI 1.24-2.21), PTSD (ORL1 vs L0 1.51, 95% CI 1.14-2.00; ORL2 vs L0 1.99, 95% CI 1.44-2.76) and perceived stress (ORL1 vs L0 0.98, 95% CI 0.83-1.17; ORL2 vs L0 1.29, 95% CI 1.03-1.62). Point estimates increased with increasing quartiles for anxiety, depression and PTSD. The Monetized Score was associated with anxiety (ORQ2 vs Q1 0.92, 95% CI 0.70-1.22; ORQ3 vs Q1 1.11, 95% CI 0.84-1.46; ORQ4 vs Q1 1.28, 95% CI 1.02-1.60) and perceived stress (ORQ2 vs Q1 1.06, 95% CI 0.87-1.28; ORQ3 vs Q1 1.27, 95% CI 1.07-1.50; ORQ4 vs Q1 1.28, 95% CI 1.07-1.54) in a dose-dependent manner, and was suggestively associated with depression and PTSD. (Table 2).
With distress, we observed inverse associations with total count and duration of exposure, and positive associations with metrics of severity. Levels 1 and 2 of the Cumulative Score were associated with distress (N=7,766, ORL1 vs L0 1.40, 95% CI 1.16-1.69; ORL2 vs L0 1.61, 95% CI 1.24-2.10; Table S4). In analyses stratified by race, the magnitude of association between property/crop losses per capita and PTSD was stronger among white participants (ORQ4 vs Q1 2.84, 95% CI 1.85-4.37) than among non-white participants (ORQ4 vs Q1 1.24, 95% CI 0.74-2.09; Table 3). When restricting to oil spill response and cleanup workers (N=7,456), associations with PTSD were similar to those found in the broader analytic sample (Table S5). In analyses stratified by the median home visit date, no significant differences were observed in magnitudes of association with PTSD in earlier response vs. later response participants (Table S6).
Table 3:
Estimated odds ratio (OR) associations between natural hazard burden and PTSD (PC-PTSD ≥ 3) stratified by race*
| Non-White (N=4,224) | White (N=5,125) | |||||
|---|---|---|---|---|---|---|
| Prevalence (N, %) | 272 (7%) | 214 (4%) | ||||
| Natural Hazard Burden Variable | Quartile N (%) | Cases | OR (95% CI) | Quartile N (%) | Cases | OR (95% CI) |
| Total Counta | ||||||
| Quartile 1 | 703 (17) | 50 | REF | 1052 (21) | 32 | REF |
| Quartile 2 | 1088 (26) | 102 | 1.23 (0.76, 1.99) | 1303 (25) | 51 | 1.10 (0.70, 1.75) |
| Quartile 3 | 1000 (24) | 69 | 0.97 (0.64, 1.47) | 1458 (28) | 91 | 1.93 (1.16, 3.21) |
| Quartile 4 | 1433 (34) | 55 | 0.60 (0.36, 0.98) | 1312 (26) | 40 | 0.92 (0.55, 1.51) |
| Duration of Exposurea | ||||||
| Quartile 1 | 993 (24) | 94 | REF | 1478 (29) | 50 | REF |
| Quartile 2 | 811 (19) | 50 | 0.77 (0.50, 1.17) | 1294 (25) | 44 | 0.89 (0.54, 1.46) |
| Quartile 3 | 1515 (36) | 88 | 0.97 (0.58, 1.64) | 1196 (23) | 75 | 1.91 (1.10, 3.32) |
| Quartile 4 | 905 (21) | 44 | 0.74 (0.46, 1.21) | 1157 (23) | 45 | 1.20 (0.66, 2.21) |
| Fatalities/Injuries per Capita | ||||||
| Quartile 1 | 841 (20) | 50 | REF | 1293 (25) | 41 | REF |
| Quartile 2 | 1661 (39) | 90 | 0.94 (0.47, 1.87) | 1191 (23) | 48 | 1.07 (0.70, 1.64) |
| Quartile 3 | 898 (21) | 74 | 0.92 (0.53, 1.58) | 1235 (24) | 66 | 2.11 (1.25, 3.54) |
| Quartile 4 | 824 (20) | 62 | 1.14 (0.73, 1.76) | 1406 (27) | 59 | 1.40 (0.85, 2.31) |
| Property/Crop Damage per Capita | ||||||
| Quartile 1 | 558 (13) | 29 | REF | 992 (19) | 21 | REF |
| Quartile 2 | 1295 (31) | 49 | 0.77 (0.45, 1.31) | 1367 (27) | 44 | 1.18 (0.75, 1.86)c |
| Quartile 3 | 1327 (31) | 103 | 1.42 (0.84, 2.38) | 1457 (28) | 64 | 1.73 (1.13, 2.64)c |
| Quartile 4 | 1044 (25) | 95 | 1.24 (0.74, 2.09) | 1309 (26) | 85 | 2.84 (1.85, 4.37)c |
| Cumulative Scored | ||||||
| Level 0 | 1904 (45) | 90 | REF | 1610 (31) | 56 | REF |
| Level 1 | 2142 (51) | 171 | 1.62 (1.20, 2.20) | 3265 (64) | 133 | 1.38 (0.93, 2.05)c |
| Level 2 | 178 (4) | 15 | 1.44 (0.88, 2.36)b | 250 (5) | 25 | 3.12 (1.73, 5.63)bc |
| Monetized Scoree | ||||||
| Quartile 1 | 1152 (27) | 74 | REF | 1513 (30) | 46 | REF |
| Quartile 2 | 700 (17) | 52 | 0.87 (0.46, 1.63) | 1010 (20) | 61 | 2.20 (1.53, 3.17) |
| Quartile 3 | 1537 (36) | 88 | 0.80 (0.45, 1.42) | 1311 (26) | 46 | 1.03 (0.68, 1.57) |
| Quartile 4 | 835 (20) | 62 | 0.98 (0.58, 1.66) | 1291 (25) | 61 | 1.72 (1.10, 2.69) |
Adjusted for age, education, employment, sex, ethnicity, alcohol use, smoking, total hydrocarbon exposure, and county-level median income
Incorporates NCEI-designated Billion-Dollar Disasters only
Significant interaction between exposure and race (Wald interaction test P < 0.05)
Linear Regression Test for Trend, P < 0.05
For each participant, a score of one was assigned if they were categorized in the top quartile for each individual exposure parameter of severity: fatalities per capita, injuries per capita, property losses per capita, crop losses per capita. Level 0 = score of 0, Level 1 = scores of 1-2, Level 2 = scores of 3-4
Values of $4 million were assigned to each fatality and $600,000 to each injury. Dollar amounts for fatalities per capita, injuries per capita, property losses per capita and crop losses per capita were added together, and participants were categorized into quartiles per losses in dollar amounts.
Discussion
Among GuLF Study participants, we found consistently positive associations between natural hazard Cumulative Score and five measures of mental health impact (perceived stress, distress, depression, anxiety and PTSD). We also observed generally positive associations between these mental health outcomes and the Monetized Score, as well as each score’s individual components (fatalities/injuries, property/crop losses). These associations were seen after adjustments for individual-level and county-levels, as well as past and current mental health treatment. The two crude hazard exposure metrics – total count of loss events and duration of exposure – were only positively associated with stress and inconsistently or even inversely associated with other adverse mental health outcomes. Associations were generally strongest for PTSD. In analyses stratified by race, although baseline prevalence of PTSD was higher among non-white compared to white participants (7% vs. 4%), we found higher magnitudes of association between hazard burden and PTSD in white vs. non-white participants. Associations were similar among oil spill cleanup workers as compared to the overall study cohort.
This study uniquely evaluated multiple dimensions of overall natural hazard burden with multiple mental health outcomes. Previous studies found that individual natural disasters are most strongly associated with PTSD incidence (5). Schwartz et al. found that overall exposure to Hurricane Sandy in 2012 was associated with anxiety (OR 1.08, 95% CI 1.04-1.14), depression (OR 1.09, 95% CI 1.04-1.14) and PTSD (OR 1.32, 95% CI 1.23-1.40) among a sample of New York residents (9). Lieberman-Cribbin et al. found that self-reported flooding exposure during Hurricane Sandy was associated with anxiety (OR 1.5, 95% CI 1.1-1.9), depression (OR 1.7, 95% CI 1.3-2.2) and PTSD (OR 2.5, 95% CI 1.8-3.4) (10). Fergusson et al. found similar results for anxiety (OR 1.08, 95% CI 0.95-1.23), depression (OR 1.10, 95% CI 0.95-1.27) and PTSD (OR 1.25, 95% CI 0.93-1.68) in relation to earthquake exposure in 2010-2011 among residents of the Canterbury region of New Zealand (35), and Stellman et al. found an increased risk (OR 1.66, 95% CI 1.21-2.28) of PTSD with the loss of a family member from the 9/11 attacks on New York City (Stellman et al. 2008), a man-made disaster. We also found that exposure to natural hazards is associated most strongly with PTSD. As Goldmann et al. note, PTSD is the only mental health disorder where an experienced traumatic event is required for diagnosis, and therefore PTSD is the most likely disorder to appear immediately following a disaster (34). However, isolated mental health disorders are rare, and PTSD is itself a risk factor for secondary mental health outcomes such as anxiety and depression (37).
Neria et al. suggest that cumulative exposure severity, defined either as the magnitude of personal exposure to a single hazard event or as exposure to multiple hazard events in one location, is associated with higher risk of mental health pathology in a dose-dependent manner (5). Harville et al. studied women in the US Gulf region following the Deepwater Horizon disaster, and found that the risk of developing mental health disorders in participants who have experienced multiple hurricanes is higher than among those who experienced less hurricanes (38). Similarly, we found that severity as defined by two severity scores of hazard burden is associated with adverse mental health in a linear fashion. However, we also found that measures of total count of loss events and duration of exposure appeared protective, and that magnitudes of association were stronger among white vs. non-white participants. It is possible that hazard events over time may lead to the development of personal resilience and/or social support, such that participants living in certain areas or within certain social and cultural communities may be able to recover faster from hazard events . This result could also indicate that aggregate impact measures, like the cumulative and monetized scores we consider, are better indicators of adverse hazard exposures than the number and duration of hazard events.
Previous studies using the GuLF Study population found associations between working on the oil spill and depression and PTSD (40,41). Similarly, Rung et al. (2016) found associations with both physical and economic exposure to the oil spill and depression and mental distress among a population-based sample of women living in southern coastal Louisiana parishes (42). In our primary analyses, despite adjusting for oil spill response and cleanup exposures, we found associations between natural hazard exposure and various mental health outcomes including PTSD. Additionally, results from a sensitivity analysis restricted to oil spill response and cleanup workers were broadly similar to our primary results, suggesting that exposures to natural and man-made hazards are independently associated with mental health pathologies. The severity of exposure to oil spills may contribute to cumulative severity from natural hazards and affect mental health in a dose-dependent fashion, as Harville et al. (2018) have suggested (38), however we did not see this in our study.
Overall, our study findings indicate that natural hazard burden, above and beyond single hazard events, contributes to mental health burden, especially for PTSD. Primary hypothesized mechanisms explaining this link include experiences of trauma during a hazard event (34), secondary stressors such as economic difficulties and problems with personal relationships after a hazard event (7), and long-term impairments in cognitive functioning (43). While the majority of victims of a natural hazard will not develop psychopathology (6), and while mental health burden following a disaster decreases over time as personal resilience increases for some (44), climate change is expected to increase the severity of hazard events of all types (45) and may increase the prevalence and magnitude of mental health pathologies in the future.
Strengths of our study include the use of all loss-causing county-level natural hazard events and thus the ability to assess mental health impacts of repeat exposure to major loss events from natural hazards. The large sample size with detailed information on sociodemographic, lifestyle and health factors, as well as oil spill exposures, allowed for control of potential confounding. Participants in our sample were exposed to multiple hazards from 2005 to 2010, including four major hurricanes as well as flooding and tornado events among others, providing variability of exposure within our distribution. We also used validated screening questionnaires for perceived stress, anxiety, depression and PTSD, allowing us to identify participants at risk of different mental health pathologies.
A primary concern in our study is that possible reverse causation may play a role such that participants who have poor mental health cluster in counties at risk of natural hazards. A longitudinal design would better support a causal hypothesis. While comprehensive, SHELDUS is a database of only loss-causing hazard events reported to the National Weather Service. SHELDUS is highly likely to underreport direct losses and does not include events which did not cause any direct monetary or human losses (25). SHELDUS also only includes direct losses caused by hazard events and does not consider indirect losses such as disruptions in productivity due to illness or infrastructure damage. In this study, we used county-level data from SHELDUS and did not estimate or obtain individual-level hazard exposures. We aggregated events occurring from 2005-2010 by county from SHELDUS. By linking this county-level data to our participants using home address, we, in effect, assume that participants moved to their county of residence prior to 2005 and resided at their provided address until their home visit interviews which were conducted sometime between 2011-2013. We cannot account for variability in exposures within counties. County-level exposure data may induce misclassification of exposure, however this is the most comprehensive data available for disasters from natural hazard events across such a large region. Our population generally has lower socioeconomic status, with lower average household incomes compared to regional and national averages, so our findings may not be broadly generalizable.
Additionally, major disasters such as Hurricane Katrina result in signification migration of certain populations away from impacted areas (46). Our study results may be affected by selection bias given that persons who do not have the ability to move or who are better able to adapt to the situation may be differentially at risk of mental health effects than those who were able to leave. Furthermore, those who remain may have been the least affected physically or financially by the disaster. Unfortunately, we do not have the data appropriate for assessing the presence or magnitude of this bias and cannot predict that direction of bias due to competing factors affecting migration.
The assessment of natural hazard burden and objective measures of mental health contributes to the growing body of evidence suggesting that natural disasters collectively are associated with significant burden of multiple mental health outcomes. Future studies should elucidate the indirect economic effects of mental health pathology due to natural hazards, particularly in relation to productivity losses, and should consider incorporating non-loss causing hazard events as well as regular climate variations in analyses.
Supplementary Material
Acknowledgments
Funding: This work was supported by the NIH Common Fund and the Intramural Research Program of the National Institutes of Health, the National Institute of Environmental Health Sciences [ZIA ES 102945]
Footnotes
Conflict of Interest: none declared.
References
- 1.Desai B, Maskrey A, Peduzzi P, De Bono A, Herold C. Making Development Sustainable: The Future of Disaster Risk Management, Global Assessment Report on Disaster Risk Reduction. 2015. [cited 2020 Nov 9]; Available from: https://archive-ouverte.unige.ch/unige:78299
- 2.McGlade J, Bankoff G, Abrahams J, Cooper-Knock S, Cotecchia F, Desanker P, et al. Global Assessment Report on Disaster Risk Reduction 2019. 2019;
- 3.FEMA. FEMA reflects on historic year [Internet]. 2017. [cited 2020 Feb 6]. Available from: https://www.fema.gov/news-release/2017/12/29/fema-reflects-historic-year
- 4.Lazzaroni S, van Bergeijk PAG. Natural disasters’ impact, factors of resilience and development: A meta-analysis of the macroeconomic literature. Ecol Econ. 2014November1;107:333–46. [Google Scholar]
- 5.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008April;38(4):467–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norris FH, Tracy M, Galea S. Looking for resilience: Understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009June1;68(12):2190–8. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez A, Black J, Jones M, Wilson L, Salvador-Carulla L, Astell-Burt T, et al. Flooding and Mental Health: A Systematic Mapping Review. PLoS ONE [Internet]. 2015. April 10 [cited 2020 Jan 27];10(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4393088/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz RM, Tuminello S, Kerath SM, Rios J, Lieberman-Cribbin W, Taioli E. Preliminary Assessment of Hurricane Harvey Exposures and Mental Health Impact. Int J Environ Res Public Health [Internet]. 2018. May [cited 2020 Jan 27];15(5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5982013/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwartz RM, Sison C, Kerath SM, Murphy L, Breil T, Sikavi D, et al. The impact of Hurricane Sandy on the mental health of New York area residents. Am J Disaster Med. 2015October1;10(4):339–46. [DOI] [PubMed] [Google Scholar]
- 10.Lieberman-Cribbin W, Liu B, Schneider S, Schwartz R, Taioli E. Self-Reported and FEMA Flood Exposure Assessment after Hurricane Sandy: Association with Mental Health Outcomes. PLoS ONE [Internet]. 2017. January 27 [cited 2020 Jan 27];12(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5271356/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yabe H, Suzuki Y, Mashiko H, Nakayama Y, Hisata M, Niwa S-I, et al. Psychological Distress After the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant Accident: Results of a Mental Health and Lifestyle Survey Through the Fukushima Health Management Survey in Fy2011 and Fy2012. Fukushima J Med Sci. 2014;60(1):57–67. [DOI] [PubMed] [Google Scholar]
- 12.Laugharne J, Watt GV de, Janca A. After the fire: the mental health consequences of fire disasters. Curr Opin Psychiatry. 2011January;24(1):72–7. [DOI] [PubMed] [Google Scholar]
- 13.Hansen A, Bi P, Nitschke M, Ryan P, Pisaniello D, Graeme T. The Effect of Heat Waves on Mental Health in a Temperate Australian City. Environ Health Perspect. 2008October1;116(10):1369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belleville G, Ouellet M-C, Morin CM. Post-Traumatic Stress among Evacuees from the 2016 Fort McMurray Wildfires: Exploration of Psychological and Sleep Symptoms Three Months after the Evacuation. Int J Environ Res Public Health [Internet]. 2019. May [cited 2020 Feb 6];16(9). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6540600/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gall M, Cutter S. 2005 Events and Outcomes: Hurricane Katrina and Beyond. In 2019. p. 191–217. [Google Scholar]
- 16.Blake ES, Landsea CW, Gibney EJ. NOAA Technical Memorandum NWS NHC-6. :49. [Google Scholar]
- 17.Kwok RK, Engel LS, Miller AK, Blair A, Curry MD, Jackson WB, et al. The GuLF STUDY: A Prospective Study of Persons Involved in the Deepwater Horizon Oil Spill Response and Clean-Up. Environ Health Perspect. 2017April1;125(4):570–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Engel LS, Kwok RK, Miller AK, Blair A, Curry MD, McGrath JA, et al. The Gulf Long-Term Follow-Up Study (GuLF STUDY): Biospecimen Collection at Enrollment. J Toxicol Environ Health A. 2017;80(4):218–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen S Perceived stress in a probability sample of the United States. In: The social psychology of health. Thousand Oaks, CA, US: Sage Publications, Inc; 1988. p. 31–67. (The Claremont Symposium on Applied Social Psychology). [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med. 2006May22;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009April1;114(1):163–73. [DOI] [PubMed] [Google Scholar]
- 22.Prins A, Ouimette P, Kimerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC–PTSD): development and operating characteristics. Prim Care Psychiatry. 2004January1;9(1):9–14. [Google Scholar]
- 23.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for Serious Mental Illness in the General Population. Arch Gen Psychiatry. 2003February1;60(2):184–9. [DOI] [PubMed] [Google Scholar]
- 24.CEMHS. The Spatial Hazard Events and Losses Database for the United States, Version 18.1 [Internet]. Arizona State University: Phoenix, AZ; 2019. Available from: http://www.sheldus.org [Google Scholar]
- 25.Gall M, Borden KA, Cutter SL. When Do Losses Count? Bull Am Meteorol Soc. 2009June1;90(6):799–810. [Google Scholar]
- 26.Smith AB, Matthews JL. Quantifying uncertainty and variable sensitivity within the US billion-dollar weather and climate disaster cost estimates. Nat Hazards. 2015July;77(3):1829–51. [Google Scholar]
- 27.“About the Survey.” The United States Census Bureau. September 26, 2019. https://www.census.gov/programs-surveys/acs/about.html. [Google Scholar]
- 28.Hahn DJ, Viaud E, Corotis RB. Multihazard Mapping of the United States. ASCE-ASME J Risk Uncertain Eng Syst Part Civ Eng. 2017September;3(3):04016016. [Google Scholar]
- 29.Hubbard AE, Ahern J, Fleischer NL, Laan MV der, Lippman SA, Jewell N, et al. To GEE or Not to GEE: Comparing Population Average and Mixed Models for Estimating the Associations Between Neighborhood Risk Factors and Health. Epidemiology. 2010July;21(4):467. [DOI] [PubMed] [Google Scholar]
- 30.Ramezani N Analyzing Correlated Data in SAS®. 2017;13. [Google Scholar]
- 31.Greenland S, Pearl J, Robins J. Causal Diagrams for Epidemiologic Research. Epidemiology. 1999January;10(1):37–48. [PubMed] [Google Scholar]
- 32.Stewart PA, Stenzel MR, Ramachandran G, Banerjee S, Huynh T, Groth C, et al. Development of a Total Hydrocarbon Ordinal Job-Exposure Matrix for Workers Responding to the Deepwater Horizon Disaster: The GuLF STUDY. J Expo Sci Environ Epidemiol. 2018May;28(3):223–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.US Census Bureau. 2006-2010 ACS 5-year Estimates [Internet]. 2010. [cited 2020 Jan 23]. Available from: https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2010/5-year.html
- 34.Goldmann E, Galea S. Mental Health Consequences of Disasters. Annu Rev Public Health. 2014;35(1):169–83. [DOI] [PubMed] [Google Scholar]
- 35.Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a Major Disaster on the Mental Health of a Well-Studied Cohort. JAMA Psychiatry. 2014September1;71(9):1025–31. [DOI] [PubMed] [Google Scholar]
- 36.Stellman JM, Smith RP, Katz CL, Sharma V, Charney, LaVallee RA, et al. Enduring Mental Health Morbidity and Social Function Impairment in World Trade Center Rescue, Recovery, and Cleanup Workers: The Psychological Dimension of an Environmental Health Disaster. Environ Health Perspect. 2008September1;116(9):1248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMillan GP, Lapham S. Effectiveness of Bans and Laws in Reducing Traffic Deaths. Am J Public Health. 2006November1;96(11):1944–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harville EW, Shankar A, Dunkel Schetter C, Lichtveld M. Cumulative effects of the Gulf oil spill and other disasters on mental health among reproductive-aged women: The Gulf Resilience on Women’s Health study. Psychol Trauma Theory Res Pract Policy. 2018;10(5):533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. J Pers Soc Psychol. 2010December1;99(6):1025. [DOI] [PubMed] [Google Scholar]
- 40.Kwok RK, McGrath JA, Lowe SR, Engel LS, Jackson WB, Curry MD, et al. Mental health indicators associated with oil spill response and clean-up: cross-sectional analysis of the GuLF STUDY cohort. Lancet Public Health. 2017December1;2(12):e560–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lowe S, Kwok R, Payne J, Engel L, Galea S, Sandler D. Why Does Disaster Recovery Work Influence Mental Health?: Pathways through Physical Health and Household Income. Am J Community Psychol. 2016December;58(3–4):354–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rung AL, Gaston G, Oral E, Robinson WT, Fontham E, Harrington DJ, et al. Depression, Mental Distress, and Domestic Conflict among Louisiana Women Exposed to the Deepwater Horizon Oil Spill in the WaTCH Study. Environ Health Perspect. 2016September1;124(9):1429–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKinzie AE. In their own words: disaster and emotion, suffering, and mental health. Int J Qual Stud Health Well-Being [Internet]. 2018. March 1 [cited 2020 Jan 27];13(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5844051/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pietrzak RH, Tracy M, Galea S, Kilpatrick DG, Ruggiero KJ, Hamblen JL, et al. Resilience in the Face of Disaster: Prevalence and Longitudinal Course of Mental Disorders following Hurricane Ike. PLoS ONE [Internet]. 2012. June 26 [cited 2020 Jan 30];7(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3383685/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Intergovernmental Panel on Climate Change. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; 2012. 593 p. [Google Scholar]
- 46.Myers CA, Slack T, Singelmann J. Social vulnerability and migration in the wake of disaster: the case of Hurricanes Katrina and Rita. Popul Environ. 2008;29(6):271–291. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


