Abstract
Background:
Telemedicine and telemonitoring have become invaluable tools in managing chronic diseases, such as heart failure (HF). With the recent pandemic, telemedicine has become the preferred method of providing consultative care.
Local Problem:
This rapid paradigm shift from face-to-face (F2F) consultations to telemedicine required a collaborative approach for successful implementation while maintaining quality of care. The processes for conducting a telemedicine visit for HF patient are not well defined or outlined.
Method:
Using a collaborative practice model and nurse practitioner led program, technology was leveraged to manage the high-risk HF population using virtual care (consultation via phone or video-to-home) with two aims: first to provide ongoing HF care using available telemedicine technologies or F2F care when necessary and, second, to evaluate and direct those needing urgent/emergent level of care to emergency department (ED).
Intervention:
The process was converted into an intuitive algorithm that describes essential elements and team roles necessary for execution of a successful HF consultation.
Results:
Following the algorithm, nurse practitioners conducted 132 visits, yielding 100% success in the conversion of F2F appointments to telemedicine, with 3 patients referred to ED for care. The information obtained through telemedicine consultation accurately informed decision for ED evaluation with resultant admission.
Conclusion:
Collaborative team-based approach delineated in the algorithm facilitated successful virtual consultations for HF patients and accurately informed decisions for higher level of care.
Keywords: COVID-19, heart failure algorithm, heart failure consultation, nurse practitioner, quality of care, team-based virtual care, telemedicine, video-to-home
Introduction
Telemedicine and telemonitoring have revolutionized the delivery of health care. Telemonitoring technologies have been commonly used for the management of chronic diseases such as hypertension, diabetes, and heart failure (HF). Sensor telemonitoring technologies and enrollment in telehealth programs for heart failure patients have shown mixed results toward reduction of morbidity and mortality (Koehler et al., 2010). Sensor monitoring technologies use algorithm-based parameters in monitoring physiological data, such as blood pressure (BP), heart rate, weight, and saturation, to identify high-risk responses that require intervention. Traditionally, these data have been used as an adjunct to a consultative face-to-face (F2F) visit, but what happens when F2F visits cannot be undertaken?
The current COVID-19 pandemic has spurred a paradigm shift in the delivery of cardiac consultation for HF patients, from a traditional F2F to virtual care. Although this change has been forcibly and rapidly introduced, it is likely to result transform future delivery of consultative care. There is minimal data available addressing the essential elements necessary to execute consultations with HF patients via telephone or video-based modalities (i.e., VA Video Connect, FaceTime, Doximity, Google Duo, and other accepted video conference platforms). Therefore, the initial roll out and blueprint of these elements that ultimately became an algorithm was formulated and incepted for the management of HF patients at US Department of Veteran Affairs (VA).
Patients with heart failure diagnosis were identified by the Centers for Disease Control and Prevention (2020) as being in the highest “at-risk” category during the COVID-19 pandemic who could suffer a deterioration of status without continuity of care. Using a collaborative practice model and a nurse practitioner (NP)-led program, an intuitive algorithm (Figure 1) was formulated leveraging available resources and technology to provide virtual consultations to HF patients.
Figure 1.
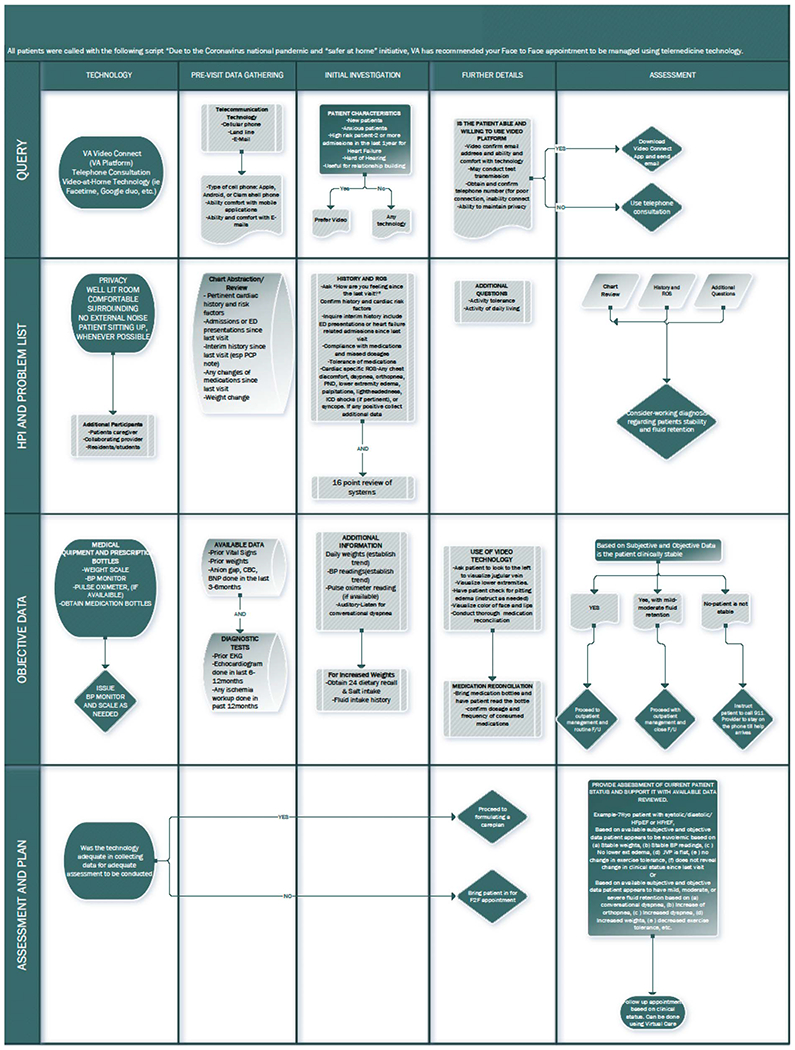
Telemedicine guided heart failure algorithm during COVID-19.
Background
There has been a national trend over many decades to integrate video consultation as a platform for health care delivery. This trend is fueled by both institutions and policymakers, although uptake has been limited (Eysenbach et al., 2020; Institute of Medicine, 2001). Drivers for this change are both the patients and providers. Patients are keen to have an alternate solution for F2F visits due to the benefits of reduced time to travel, ability to remain in the comfort of their home, and increased access to providers. Providers, including NPs, are motivated to integrate telehealth into their practice because this may result in increased compliance with attendance.
VA experience with video-to-home technology
The technology to provide video consultations at home within the VA system is known as VA Video Connect. VA Video Connect is a secure VA platform, using video-to-home modality to deliver health care principally directed to those needing primary care and mental health services. More than 99,000 veterans used the VA VA Video Connect app, in fiscal year 2019, resulting in 294,000 virtual appointments (U.S Department of Veteran Affairs, 2019). Patient satisfaction of their overall care at the VA significantly increased with the addition of telemedicine services (Slightam et al., 2020). Providers agreed that telemedicine could improve patient care especially by increasing access and decreasing wait times (Driessen et al., 2018). Lack of training in the areas of available platforms, safety assessments, patient/provider relationships, confidentiality, and computer/systems software were barriers identified by providers (Baird et al., 2018; Seuren et al., 2019).
Not only have providers reported satisfaction with telemedicine but patients have as well. Veterans were shown to report positive satisfaction for receiving their care with VA issued tablets, without any correlation with age, income, health literacy, distance from the closest VA, or prior technology use. Veterans were open to video care as an alternative to in-person care. This demonstrates that telehealth may be beneficial for many different types of veterans and is associated with a high level of satisfaction (Slightam et al., 2020).
Nurse practitioner role in heart failure management
Nurse practitioners have been shown to deliver high-quality care that is noninferior to physician colleagues, with no difference in performance measures between physicians and advanced practice providers (Virani, et al, 2015). A protocol-driven allied health clinic (consisting of an APN who specialized in HF and a clinical pharmacist) decreased 30-day hospital readmissions for HF by 44.3% (Donaho et al, 2015). Nurse practitioners are therefore poised and motivated in transitioning patients from F2F to virtual care.
Methods
An initial interdisciplinary workgroup of NPs, telemedicine cardiologists, and the associate chief of cardiology was established to brainstorm patient management strategies for successful virtual HF consultation. There was an initial discussion to identify the goals, available vs required resources, and key stakeholders essential for each consultation to be successful. Additionally, clinical elements necessary for HF consultation, availability for consultation with a cardiologist, and management of emergent/urgent issues were discussed. As a result of the brainstorming sessions, the workgroup was expanded to include the clerical staff and the telemedicine director.
Workgroup meetings were initially conducted weekly for 4 weeks, then reduced to every other week once communication lines, and expectations were established. Initial paper notes and flow diagram were later changed to HF algorithm included in this article.
Patient characteristics
Heart failure patients included those with either diastolic or systolic HF with one or more hospital admissions or emergency department (ED) presentations for HF in the past year or HF patients who have had difficulty with titration of guideline-directed medical therapy with the need for closer follow-up. Patients were contacted regarding their interest in telemedicine consultation; they reported the following: (a) uncomfortable with technology, (b) did not know or have an email address, (c) could not download “apps,” or (d) did not have a laptop or personal computer with video capability. These patients received assistance from clinicians, clerical staff, and their caregivers in undergoing telephone or video-to-home visits.
Provider characteristics
Providers included four NPs with an average of 12.75 ± 6.76 years of NP experience. All NPs completed required telehealth training. An attending cardiologist was available for consultation, and patients were contacted with collaborative recommendations after visit completion.
Heart failure consultation: Operational elements
The involvement of the clerical staff, clinicians, patients, caregivers, and attending cardiologists are essential in conducting a successful telemedicine visit. Steps for a successful consultation begins with overcoming logistical challenges of appointment set up, previsit chart review and preparation, HF-specific subjective and objective data collection, and Lastly assessment and plan.
Appointment logistics/staff roles
Clerical staff.
On initial query, the cardiology clerk identifies the following information: (a) type of phone (Android, flip-phone/clamshell phone, or iPhone/iPad), (b) ability to download applications on their devices, and (c) having an email address and/or comfort with email usage. The patient is offered a consultation modality based on the technology available to the patient. A test transmission is recommended for a patient who has never used video-to-home and would be using this modality for the first time. A back-up telephone number is essential if a video connection experiences technical difficulties. Additional information obtained by the clerk includes presence of a functional weight scale and BP monitor. Patients are instructed to obtain their weights and BP readings the morning of their visit.
Clinician.
Patients are prescreened by the clinician for appropriateness of telemedicine care. This involves chart review of the patient’s clinical status to identify characteristics that may determine patient’s suitability for video versus phone visit. Face-to-face visits may be more appropriate for patients who are highly anxious, high risk with two or more hospitalizations in the past 3 months, hard of hearing, or is an initial visit that is crucial for foundational relationship building. Once the patient has been scheduled for their chosen modality, a weight scale and BP monitor can be mailed, if appropriate. A clinician must ensure the availability and functionality of the telemedicine equipment being used; audio via computers and an external camera mounted on the monitor should be tested prior to the visit. Any individual that may have a role in the patient’s care, such as a caregiver or additional providers (attending/residents) can be invited to attend the consultation using a video link connected to patient’s appointment.
Caregiver.
Caregivers are essential in assisting the patient with technology-related challenges, obtaining vital signs, and facilitating appointments. Caregivers can also participate in the appointment by checking for lower extremity edema and assisting with patient positioning for assessment of jugular venous pressure (JVP).
Data collection
Previsit.
To be prepared for the virtual appointment, a clinician must collect relevant data pertinent to the visit. A chart review can be conducted to obtain further information regarding cardiac history and associated comorbidities. A chart biopsy can also be done to obtain supplemental information, including interim hospitalizations and ED visits for HF, medical care provided since last visit relevant to HF, medication changes, weight and BP trends, laboratory data (chem panel, complete blood count, beta-natriuretic peptide level) preferably done in the last 3 months, and prior diagnostic studies, such as electrocardiogram, echocardiogram, and any workup.
During visit.
A vigilant review of the environmental factors along with pertinent subjective and objective data collection elements can lead to sound decision making to inform the care plan. Environmental factors that are important to address during the visit include privacy, adequate lighting, noise reduction, comfortable surroundings, and safety of the patient. It is preferable to have the patient seated during the interview.
Subjective
Once all participants have joined the meeting and have been introduced, history should include comparison of the patient’s past clinical status to current status, since the last visit. It is important to ask an open-ended question. This encourages a patient to reflect on their overall health and can guide further query. The clinician performs a cardiac specific and 16-point review of systems, including implantable cardioverter defibrillator-initiated shocks. Any positive findings during review of system warrants additional query. During the interview, the provider listens and observes for the presence of conversational dyspnea. Video visits offer the additional benefit of visualizing medication bottles for medication reconciliation. Assessment of functional capacity and activity tolerance can include questions, such as walking distance, ability to climb a flight of stairs (provided patient has access to stairs), carrying groceries, walking briskly, and the like. These answers can better inform New York Heart Association classification for each patient.
Objective
Video technology can be used to evaluate the patient’s overall demeanor, breathing effort, facial color (pallor/cyanosis), presence of lower extremity edema, and JVP. If using a mobile phone or tablet, presence of lower extremity edema can be assessed by asking patients to move the camera toward their legs, and JVP can be examined by having them turn their neck to the left or right side. A clinician may guide the proximity of the camera to allow for clear visualization of the area. Caregiver assistance, if available, is important for this step. Additional data collection includes current weight, BP, oxygen saturation, and 24-hour dietary recall to assess for salt intake and average total fluid intake.
Assessment/plan
Based on available subjective and objective data, a determination of the patient’s HF stability can be formulated. The clinician must reflect and evaluate whether the selected modality (phone or video-to-home), patient interview, and available data are satisfactory toward formulating a reasonable and adequate care plan. If the answer is yes, then care plan can be implemented. If answer is no, then the patient should be recommended to present for a F2F appointment for further care. Continuation of current medical therapy with consideration for titration of goal-directed medical therapy may be pursued in clinically stable patients. Patients with mild-to-moderate fluid retention can be managed through adjustment of medications with emphasis on diuretics. Daily weights, BP monitoring, and follow-up laboratory tests are helpful to evaluate a patient’s response to diuresis. Home health consultation may be used for in-home laboratory draw. This is especially important for patients without access to transportation. If the patient is found to have advanced NYHA class III-IV HF, they should be advised to contact ED or 911 for assistance. In the event of a 911 dispatch, the provider continues to remain on the call with the patient until arrival of emergency services.
Barriers
The encountered barriers were centered around logistics, resistance to technology, and training. These were discussed at the weekly workgroup meetings, with an ongoing effort toward overcoming them. Provider hesitation with usage of technology was addressed through completion of mandatory courses offered by the VA and conducting a provider-to-provider mock video call. There was a steep learning curve because the use/integration of telemedicine has not been a part of formal education and training. Self-education and continuing education resources continue to be used in fulfilling these deficits. For geographical areas that had inadequate internet/cellular connection or dropped video calls, telephone consultation became the primary virtual care modality.
During the first two weeks, usage of video-to-home technology was <5%, owing to providers proactively making phone calls, to preempt F2F encounters, and due to lack of familiarity and comfort with the technology. In the third week, the clerical staff was used to call patients and offer video-to-home technology for consultation. It was later identified that the clerical staff were not comfortable with the usage of telemedicine technology and therefore could not describe or advocate for it. Similar to the approach in teaching the providers, a mock video call was made with the clerical staff to familiarize them with log in and equipment usage. In retrospect, this was the critical step that resulted in patient acceptance and increased scheduling of video-to-home visits.
Data review
Data were collected at end of each week for eight weeks. The data included the number of (a) total completed HF consultations, (b) modality used for each consultation, (c) face-to-face visits, (d) referred to ED/911 calls, and (e) no show/canceled appointment. Each NP also reported the percent of patients where video-to-home technology was used to deliver care. Nurse providers provided care to a total of 132 HF patients, with 100% conversion of F2F appointments to telemedicine with zero no-show rate starting the third week. During this time, there was an increase of video-to-home visits to 24% (Figure 2). No appointments were converted from telemedicine to F2F.
Figure 2.
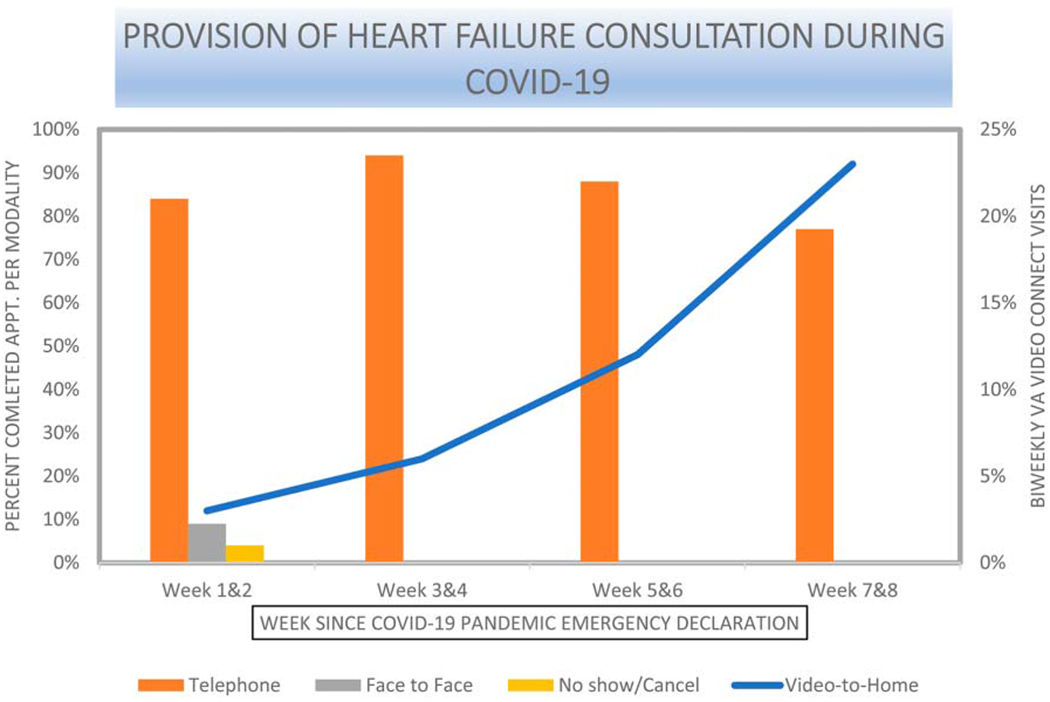
Consultation modalities. Figure represents percent usage of telephone, face-to-face, and video-to-home modalities for care delivery to HF patient. Patients were managed virtually starting week 3 onward with an increase of Video-to Home modality over time. HF = heart failure.
Lessons Learned
COVID-19 is ongoing as is our telemedicine HF care. Telemedicine provided a platform for conducting HF visits. These visits were meaningful, and value was added when video technology was used. The initial 2 weeks were spent bracing with the reality of a pandemic. Telephone visits were used predominantly due to unfamiliarity and lack of comfort with technology. Over time, there was an increase in utilization of video-to-home technology. A collaborative effort between clerical staff, clinicians, and caregivers provided foundational success toward integration and transition to telemedicine care. During the first four weeks, there was an increased reliance on home health consults for laboratory draws. The telemedicine platform and algorithm guided data collection to provide optimal HF management. Information obtained through telemedicine accurately informed decision making for patients who needed higher levels of care, prompting ED evaluation that led to hospital admission.
Implications for nurse practitioner practice
Nurse practitioners are at the forefront of patient care, providing both direct and indirect longitudinal care for chronically ill patients with a diagnosis of HF. Nurse practitioners across the nation working collaboratively with physician cardiologists are making critical clinical decisions regarding HF care for these patients. Since the COVID-19 pandemic emerged, NPs have been propelled to find innovative ways to deliver care. Leveraging existing technology provides an avenue toward delivering meaningful value-added consultation. Nurse practitioners frequently manage HF clinics and supervise the care provided. Therefore, it is well suited to incorporate the intuitive algorithm that delineates each team member’s role clearly in conducting successful consultation appointments for HF patients. Having an overall understanding of every team member’s role is crucial toward patient engagement.
In conclusion, when following the outlined process, telemedicine was found to provide an adequate platform for delivery of HF consultation and to the point studied, a reliable determinant of patients needing emergency/hospital level care.
Footnotes
Competing Interests: The authors report no conflicts of interest.
References
- Baird MB, Whitney L, & Caedo CE (2018). Experiences and attitudes among mental health advanced practice nurses in the use of telemental health: Results of an online survey. Journal of the American Psychiatric Nurses Association, 24, 235–240. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (30 June 2020). Frame-work for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. In Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, https//:www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. [Google Scholar]
- Centers for Disease Control and Prevention. People who are at higher risk for severe illness. In Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. [Google Scholar]
- Donaho EK, Hall AC, Gass JA, Elayda MA, Lee VV, Paire S, & Meyers DE (2015). Protocol-driven allied health post-discharge transition clinic to reduce hospital readmissions in heart failure. Journal of the American Heart Association, 4, e002296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driessen J, Chang W, Patel P, Wright RM, Ernst K, & Handler SM (2018). Nursing home provider perceptions of telemedicine for providing specialty consults. Telemedicine Journal and E-health: The Official Journal of the American Telemedicine Association, 24, 510–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G, Stommel W, McKinstry B, Seuren LM, Wherton J, Greenhalgh T, Cameron D, A’Court C, & Shaw SE (2020). Physical examinations via video for patients with heart failure: Qualitative study using conversation analysis. Journal of Medical Internet Research, 22, e16694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Quality of Health Care in America (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press. [PubMed] [Google Scholar]
- Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, Boll H, Kim SS, Koehler K, Lücke S, Honold M, Heinze P,Schweizer T, Braecklein M, Kirwan BA, Gelbrich G, Anker SD, &T. I. M-H. F. Investigators (2010).Telemedical interventional monitoring in heart failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: Study design. European Journal of Heart Failure, 12, 1354–1362. [DOI] [PubMed] [Google Scholar]
- Seuren LM, Wherton J, Greenhalgh T, Cameron D, A’Court C, & Shaw SE (2020). Physical examinations via video for patients with heart failure: Qualitative study using conversation analysis. Journal of Medical Internet Research, 22, e16694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slightam C, Gregory AJ, Hu J, Jacobs J, Gurmessa T, Kimerling R, Blonigen D, & Zulman DM (2020). Patient perceptions of video visits using Veterans Affairs telehealth tablets: Survey study. Journal of Medical Internet Research, 22, e15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veteran Affairs. (November 22,2019). VA reports significant increase in Veteran use of telehealth services. Office of Public and Intergovernmental Affairs. US Department of Veterans Affairs. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5365. [Google Scholar]
- Virani SS, Maddox TM, Chan PS,Tang F, Akeroyd JM, Risch SA, Oetgen WJ, Deswal A, Bozkurt B, Ballantyne CM, & Petersen LA (2015). Provider type and quality of outpatient cardiovascular disease care: Insights from the NCDR PINNACLE registry. Journal of the American College of Cardiology, 66,1803–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]


