Highlights
-
•
Behavioral economic-based interventions have been suggested to increase uptake in CRC screening programmes.
-
•
This study tested the effectiveness of six behavioral economic-based messages in two field trials.
-
•
None of the messages increased screening participation.
1. Introduction
Colorectal cancer (CRC) screening has proven to be an effective way of detecting cancer at an early stage (Wagner et al., 1991, Frazier et al., 2000). However, as screening is not mandated, participation rates vary drastically globally and are often below-recommended levels (McGregor et al., 2007, Klabunde et al., 2015, Karsa et al., 2008, Basu et al., 2018, Hirst et al., 2018). In order to be effective, CRC screening programs need to achieve and maintain high participation. There is, thus, an interest in studying reasons for suboptimal screening uptake, in order develop interventions to make CRC screening more accessible. Non-participation is thought to be caused by low knowledge about the screening program, among other factors (Power et al., 2009). Low uptake rates may, therefore, indicate that individuals do not fully understand the purpose and goal of screening programs. (Weitzman et al., 2001)
A recent systematic review found that pre-notification letters, primary care endorsement, tailored reminders and telephone contact, in addition to usual invitation, can all lead to higher participation rates (Duffy et al., 2017). While these interventions are effective at improving overall uptake, they have only partially been adopted, due to a lack of evidence supporting their cost-effectiveness (for example, telephone reminders are not recommended by the European Union Committee for Quality Assurance in Bowel Cancer Screening, as they are not considered cost-effective) (von Karsa et al., 2013). As such, there is growing interest in the search for new low-cost interventions, such as those which involve enhancing existing invitation materials through the use of insights from behavioral economics (von Karsa et al., 2013, Purnell et al., 2015, Barnes et al., 2016, Schwartz et al., 2017, Stoffel et al., 2019, Bakr et al., 2020, Huf et al., 2020, Stoffel et al., 2021) These approaches build on the concept that the screening decision is influenced by the way in which the choice is presented, and are potentially cost-neutral, as they only involve manipulating the presentation and content of the invitation materials (Purnell et al., 2015, Schwartz et al., 2017, Stoffel et al., 2019, Bakr et al., 2020, Huf et al., 2020, Stoffel et al., 2021, Mehta et al., 2017, Mehta et al., 2018, Stoffel et al., 2019, Stoffel et al., 2020).
To date, studies conducted in the context of CRC screening have mostly analyzed the framing of existing information in invitation letters, such as relative and absolute risk (Howard and Salkeld, 2009) and gain vs. loss-framed messages (Meyerowitz and Chaiken, 1987, Myers et al., 1991, Ferrer et al., 2012). Only a few studies have investigated the effect of adding additional information, mainly on social norms. (Schwartz et al., 2017, Stoffel et al., 2019, Bakr et al., 2020, Huf et al., 2020, Sieverding et al., 2010, Stoffel et al., 2019, von Wagner et al., 2019) Furthermore, several of these studies measured the effect on intention rather actual behavior, limiting the generalizability of their findings (Howard and Salkeld, 2009, Ferrer et al., 2012, Sieverding et al., 2010, Stoffel et al., 2019, von Wagner et al., 2019). Finally, little is therefore known about the effect of using other messages, derived from behavioral economics, communicating information about the costs and benefits of CRC screening on screening uptake.
In this study, we set out to test whether messages, derived from behavioral economics, can increase participation in the context of the Cypriot pilot program for CRC screening, which invited residents, aged 50–69 years, to complete a Fecal Immunochemical Test (FIT) (Farazi, 2014;8:389., Ponti et al., 2017). The screening pilot was initiated by Ministry of Health in 2013 and aimed at reaching the international benchmark for acceptable participation set out by the European guidelines for quality assurance in CRC screening (i.e. 65%), as it is imperative for screening programs to achieve and maintain high participation in order to be effective and cost-effective (Ponti et al., 2017). Although there is no data from the first pilot round available, there is a strong public health mandate in Cyprus to optimize screening invitations through the use of low cost, evidence-based approaches to make screening accessible for everyone.
2. Methods
2.1. Study design
We performed two randomized controlled trials (RCTs) between 2013 and 2014. The first RCT (‘Trial 1′) was a seven-arm RCT in which individuals were randomly allocated to receive the standard invitation letter, with one of six additional behavioral economics-based messages included, or the standard invitation letter with no manipulation (i.e. control). The second RCT (‘Trial 2′) was a two-arm RCT, in which individuals were randomly allocated to receive either the standard invitation letter with the most efficacious message from the first RCT, or the standard invitation letter with no manipulation (i.e. control). The primary aim of the first RCT was to identify the most efficacious message, which was then tested the second RCT with more participants per trial arm.
2.2. Setting
Trial 1 was conducted as part of the second round of the Cypriot CRC screening pilot, which was conducted in the urban area of Aradippou between October and December 2013. 1Trial 2 was conducted as part of the third round of the Cypriot CRC screening pilot, which was conducted in the rural villages of Meneou, Dromolaxia, and Kiti, between May and October 2014.2
2.3. Participants
In both trials, participants were residents, aged between 50 and 69 years, who were invited for CRC screening as part of Cypriot CRC screening pilot.
2.4. Invitation procedure
Participants were invited for CRC screening as per usual care. Participants received an invitation letter (with or without the inclusion of a behavioral message, depending on whether they had been randomly allocated to one of the intervention conditions, or the control), an information leaflet, and a small tube for collecting the stool sample. Participants who received an invitation were instructed to use the tube to collect a small sample of their stool and return it in a sealed plastic bag to their nearest health center. Participants then received their test results by mail. Anyone with an abnormal result was invited for further investigation (e.g. colonoscopy).
2.5. Randomization
Participants were randomized individually by a computer using a pseudorandom number generator. Participants in Trial 1 were randomized (1:1:1:1:1:1:1 ratio) to receive either the standard invitation letter, or, a modified invitation letter with an additional component based on one of six behavioral economics principles, namely: social responsibility, anticipated regret, account effect, benefit of early detection, scarcity effect and social norms. In Trial 2, participants were randomized (1:1 ratio) to receive either the standard invitation, or, a modified version of the standard invitation, containing the behavioral message found to be most efficacious in Trial 1.
2.6. Intervention design
English translations for the six behavioral messages are presented in Table 1. The intervention message was presented in the third paragraph of the invitation letter, had an average length of 61 words (SD 7.31), was entirely highlighted in bold and underlined.3
Table 1.
Messages used in Trial 1 (translated from Greek).
| Message | |
|---|---|
| Social responsibility | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. Developing colorectal cancer is likely to have a substantial physical and emotional impact on your life. However, it is not just you who would suffer; typically, family and friends suffer with you. Participate now, not only for your own health but also to prevent your family and your friends from going through the suffering with you. After all, they deserve it! |
| Anticipated regret | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. Without participating in the screening program now, you might find out too late that you have colorectal cancer. Patients with an early diagnosis have much higher survival rates. Later cancer diagnoses can be physically and mentally more painful as the cancer might be more difficult to cure. Participate now and avoid regretting the decision later! |
| Account effect | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. You can participate in this screening program now. Remember that although the participation is free, you and others have financed this program through your taxes. Participate now, not only for your own health but also to not waste your tax money. |
| Benefit of early detection | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. Testing increases the chance that the cancer is detected in an early stage so that you could profit from early treatments. Your participation in the program reduces the risk of detecting colon cancer at an advanced stage. |
| Scarcity effect | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. The current program is only available to people who live in the area of ____. Furthermore, the program will end at the end of this year. Don't wait and risk regretting passing up on the opportunity of free screening. Hurry up and participate in the program. |
| Social norms | The Ministry of Health has started a colorectal cancer screening program to reduce the number of victims in Cyprus. The program has started to be successfully implemented in the other regions of _____, where a large number of people have already participated in the program. Follow their lead and participate in the program! |
The behavioral messages were developed together with stakeholders in the screening program and highlighted either the benefit of participating in the screening program or the costs of non-participation. The messages were mainly negatively framed as previous studies found that loss framed health messages may be more persuasive than gain framed messages (O’keefe and Jensen, 2006).
2.7. Social responsibility message
The first intervention featured a social responsibility message, which highlighted that a CRC diagnosis does not only affect their own quality of life, but also those of their family, as a result of physical and psychological changes (Cotrim and Pereira, 2008). This intervention was based on the theory of planned behavior, which states that the intention to perform a specific behavior is determined by salient beliefs about the benefits and costs of such behavior (Ajzen, 1991). Studies suggest that individuals are not aware of the costs of non-attendance and mainly care about the opportunity cost of participation (Rothman et al., 1993, Myers et al., 1997, Rothman and Salovey, 1997). Additionally, as low awareness of the benefits of screening is often found among individuals who do not attend screening (Garcia et al., 2011), highlighting them and the cost of non-attendance could potentially improve individual attitudes about CRC screening and increase uptake (Power et al., 2009, Purnell et al., 2015, Cox and Cox, 2001). Knowing more about the cost of cancer for the social environment and cost of non-attendance in terms of late diagnosis may provide a powerful motivation to participate in cancer screening (Champion and Skinner, 2008). Additionally, individuals may underestimate the consequences of having cancer by not thinking about its impact on their close social environment (Bell, 1982).
2.8. Anticipated regret
The second intervention included an anticipated regret message and was inspired by studies that suggest that emotional experiences, such as regret, following a decision can promote behavior change and modify the evaluation about potential outcomes of participating in CRC screening. (Abraham and Sheeran, 2004). Anticipated regret refers to the expected post-behavioral negative emotional experience of not performing a behavior that would positively contribute to one's personal goals, such as participating in CRC screening to stay healthy. Anticipated regret has been studied within the context of the theory of planned behavior and has shown to an important determinant of intention formation (Ajzen, 1991, Abraham and Sheeran, 2004 May). Several studies have manipulated anticipated regret for increasing intention to engage in health behaviors (O'Carroll et al., 2011 Mar, Sheeran et al., 2014 Mar, Conner et al., 2015 Jun). Following this literature, the second intervention communicated that late CRC diagnosis may involve more difficult treatments, so that they should participate now to benefit from early diagnosis and not regret the decision later. The theoretical underpinning for this intervention is similar to that of the social responsibility message, the key difference being that is focuses on the consequences of their own quality of life.
2.9. Account effect
The third behavioral message was based on the accounting effect and the sunk cost effect and stated that the screening program was financed through taxes and that they should also participate to not waste their tax payments. It assumes that individuals may neglect the financial opportunity costs of non-participation believing that the price of non-participation is zero, even though they have already paid their participation through taxes. The account effect predicts that individuals may perceive the decision to get screened in the context of the earlier payment of the taxes (Tversky, 1981), while the sunk cost effect foresees that individuals would be more likely to get screened if they knew that they had already invested money, in form of taxes, beforehand (Arkes and Blumer, 1985).
2.10. Benefit of early detection
The fourth behavioral messages focused on the benefit of cancer screening in terms of early detection. The message built on the ostrich effect, which states that individuals may not want to participate in cancer screening to avoid receiving information on potential health problems. (Beeker et al., 2000, Greiner et al., 2005, Karlsson et al., 2009, Panidi, 2015) Thus, highlighted the advantage of early over late diagnosis in terms of medical treatments could reduce the negative feeling about cancer screening. Differently to the anticipated regret message, this message did not mention the consequences of non-participation.
2.11. Scarcity effect
The fifth intervention was directly inspired by commodity theory and stated that the screening invite was restricted. Specifically, the message focused on the time-limited and local character of the current CRC screening pilot.4 Individuals, who randomly received the scarcity message, were told that they should accept the exclusive screening invite. The message builds in previous research which suggests that perceived scarcity may enhance the value of the medical service (BROCK, 1968). Experiments have shown that people perceive products which are scarce because of limited availability as costlier and more appealing as products that are abundantly available (Verhallen, 1982, Verhallen and Robben, 1994) A recent US study found that a behavioral intervention, which also featured implied scarcity, increased CRC screening (Bakr et al., 2020). Similar to our study, they implied scarcity by the unique opportunity of receiving a FIT kit (“you have been selected”).
2.12. Social norms
The sixth intervention used social norms to communicate that a large number of people participated in the first round. The idea of social norms messages is to provide individuals a standard behavior for CRC screening from which they do not want to deviate (Schultz et al., 2007). The message communicated both descriptive and injunctive norms. The descriptive norms followed previous studies on social norms that used verbal quantifiers, such as a large number of people, to communicate relatively low uptake below 50% (Stoffel et al., 2019, Schwartz et al., 2017, Stoffel et al., 2019). The injunctive norms part, which refer to the perceived approval of the behavior stated that they should follow the lead of those who participated (Schultz et al., 2007).
2.13. Blinding
The researchers randomized participants, and were so not blinded to the treatment that subjects received. As the intervention was a letter, it was not possible to blind participants to the treatment they received, either. However, participants did not know they were subjects in a randomized controlled trial, minimizing the influence of demand characteristics.
2.14. Outcome measures
In both trials, the primary outcome was participation (i.e. return of a completed FIT kit) within each experimental condition, eight weeks after sending out the screening invitation.
2.15. Sample size
Due to the exploratory nature of the first trial, no formal sample size was calculated beforehand. Differently, sample size for the second field trial was calculated prior to data collection based on estimates obtained from the first trial, so that it was sufficiently powered to detect differences of at least 4% in participation, between the experimental condition and the control, with a power of 80% and an alpha value of 0.05. (Cohen, 1988).
2.16. Data analysis
We compared screening participation across the experimental condition according to an intention-to-treat (ITT) and a per-protocol (PP) basis. The PP analysis excluded individuals whose invitation material was undeliverable and therefore returned to the Ministry of Health and recorded on the study database. Data on gender and age was only available for the PP analysis. While we used multivariate logistic regressions with age and gender as covariates for the PP analysis, we used Chi-square tests of independence for the ITT analysis, due to the lack of information about gender and age. All statistical analysis was conducted with Stata/SE version 15.1 (StataCorp LP, College Station, TX).
2.17. Ethics
The study protocol was approved by the ethics committee of the Cyprus Ministry of Health.
3. Results
3.1. Trial 1 – ITT analysis
In total, 3212 eligible men and women were randomized to one of the seven conditions. Overall screening participation was 20.2% and 19.9% in the control condition. The ITT analysis (Table 2) indicates that while screening participation of four messages (benefit of early detection 22.2%, social responsibility 20.7%, account effect 20.4% and social norms 20.2%) were higher, and of two messages (anticipated regret 19.3% and scarcity 18.9%) lower than in the control, there were no significant differences between any of the experimental conditions and the control (χ2 (6, N = 3212) = 1.934, p = 0.926).
Table 2.
Screening participation in the intention to treat and the per protocol analysis.
| Intention to treat analysis |
Per protocol analysis |
|||
|---|---|---|---|---|
| Uptake (%) | p-value | Uptake (%) | p-value | |
| Trial 1 | ||||
| Control | 19.91 | 0.926 | 20.35 | 0.937 |
| Social responsibility | 20.70 | 21.11 | ||
| Anticipated regret | 19.26 | 19.87 | ||
| Account effect | 20.35 | 20.85 | ||
| Benefit of early detect. | 22.15 | 22.70 | ||
| Scarcity | 18.86 | 19.41 | ||
| Social norms | 20.22 | 20.81 | ||
| Trial 2 | ||||
| Control | 18.68 | 0.857 | 20.59 | 0.879 |
| Social responsibility | 18.93 | 20.83 | ||
p value refers to Chi Square test of independence.
3.2. Trial 1 – PP analysis
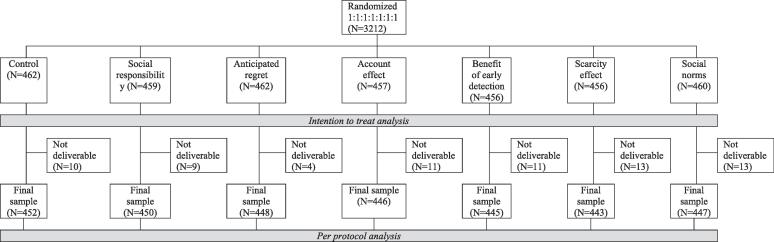
After excluding 81 participations who didn’t receive the invitation, 3131 men and women were eligible for inclusion in the PP analysis (see Fig. 1). Table 1 in the supplementary files shows that 51.2% of the study participants were male (N = 1604), 58.7% aged between 50 and 59 years old (N = 1837) and that there were no statistically significant differences between the groups in terms of the demographic variables.
Fig. 1.
CONSORT flow diagram for Trial 1.
Table 2 shows the uptake of the population, who received the invitation, varied between 22.7% (benefit of early detection message) and 19.4% (scarcity message), with no significant differences according to experimental conditions ((6, N = 3131) = 1.803, p = 0.937). The logistic regression in Table 3 confirms the non-parametric results. Only the dummy variable for individuals older than 60 years is significant at the 5% level, indicating that participation is higher for older people (25.3% vs. 17.5%, aOR 1.60; 95% 1.34–1.90, p < 0.001). The separate regression models for men and women tested whether the individual regression coefficients differ significantly between the two gender subgroups. For men, no behavioral message performed significantly differently to the control. While the social responsibility message appeared to decrease screening participation among men by 5.2% (17.3% vs. 23.5%, aOR 0.66; 95% 0.42–1.05, p = 0.080), the same message increased female participation by 8.5 points (25.6% vs. 17.1%, aOR 1.67; 95% 1.05–2.66, p = 0.031), resulting in an overall statistically insignificant effect of 0.7% (21.1% vs. 20.4%, aOR 1.04; 95% 0.76–1.45, p = 0.772). For this reason, the social responsibility message was selected to be tested in a second experiment with a larger sample. The almost statistically significant effect of the message for men was considered in the decision.
Table 3.
Adjusted logistic regression models for cancer screening screened in Trial 1.
| Model 1: Overall population |
Model 2: Male population only |
Model 3: Female population only |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total(%) | Odds ratio | 95% CI | p-value | Total(%) | Odds ratio | 95% CI | p-value | Total(%) | Odds ratio | 95% CI | p-value | |
| Overall | 20.7 | 20.6 | 20.8 | |||||||||
| Condition | ||||||||||||
| Control | 20.4 | Ref. | 23.5 | Ref. | 17.1 | Ref. | ||||||
| Social responsibility | 21.1 | 1.049 | 0.759–1.450 | 0.772 | 16.9 | 0.661 | 0.417–1.050 | 0.080 | 25.6 | 1.670 | 1.049–2.658* | 0.031 |
| Anticipated regret | 20.9 | 1.025 | 0.741–1.419 | 0.913 | 19.9 | 0.804 | 0.512–1.262 | 0.298 | 21.8 | 1.344 | 0.837–2.157 | 0.336 |
| Account effect | 19.9 | 0.982 | 0.708–1.362 | 0.882 | 19.3 | 0.786 | 0.503–1.227 | 0.343 | 20.6 | 1.270 | 0.781–2.065 | 0.221 |
| Benefit of early detect. | 22.7 | 1.164 | 0.845–1.604 | 0.352 | 24.7 | 1.082 | 0.702–1.669 | 0.721 | 20.7 | 1.281 | 0.794–2.068 | 0.310 |
| Scarcity | 19.4 | 0.927 | 0.667–1.290 | 0.654 | 17.3 | 0.671 | 0.422–1.065 | 0.091 | 21.6 | 1.312 | 0.814–2.116 | 0.265 |
| Social norms | 20.8 | 1.034 | 0.747–1.431 | 0.841 | 23.0 | 0.978 | 0.635–1.508 | 0.921 | 18.4 | 1.097 | 0.669–1.798 | 0.714 |
| Age | ||||||||||||
| 50–59 | 17.5 | Ref. | 17.4 | Ref. | 17.7 | Ref. | ||||||
| 60–69 | 25.3 | 1.597 | 1.342–1.900** | <0.001 | 25.2 | 1.617 | 1.267–2.064** | <0.001 | 25.3 | 1.581 | 1.232–2.028** | <0.001 |
| Gender | ||||||||||||
| Male | 20.6 | Ref. | ||||||||||
| Female | 20.8 | 1.010 | 0.849–1.202 | 0.909 | ||||||||
| N | 3131 | 1604 | 1527 | |||||||||
| R2 (Nagelkerke) | 0.015 | 0.022 | 0.019 | |||||||||
* p < 0.05; ** p < 0.01.
3.3. Trial 2 – ITT analysis
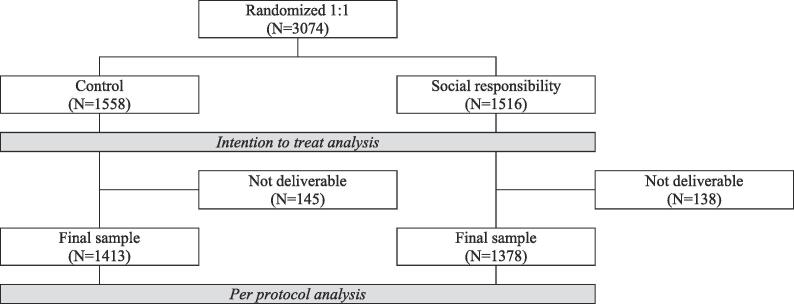
Trial 2 randomly allocated 3074 screening eligible men and women to the control condition and the social responsibility condition (see Fig. 2). Overall, uptake was 18.8%. The univariate analysis did not reveal any statistically significant differences in screening participation between the two conditions (social responsibility 18.9% vs. control 18.7%, (6, N = 3074) = 0.032, p = 0.857).
Fig. 2.
CONSORT flow diagram for Trial 2.
3.4. Trial 2 – PP analysis
After excluding 293 (9.2%) individuals who had not received the invitation letter due to a wrong address, the sample for PP analysis consisted of 1394 men (49.9%) and 1397 women (50.1%). Table 1 in the supplementary files shows that more individuals in the PP sample were between 50 and 59 years old (N = 1570, 56.3%), than between 60 and 69 years old (N = 1221, 43.7%). Similar to Trial 1, there were no statistically significant difference in gender and age across the two experimental conditions.
Overall, uptake was similar to Trial 1 (20.7%, see Table 4). While, similarly to Trial 1, the social responsibility condition had higher participation than the control condition, a Chi-square test of independence showed no significant difference between the two groups (intervention: 20.8% vs control: 20.6% (1, N = 2791) = 0.023, p = 0.879). Differently, while the logistic regressions in Table 4 did not find a significant effect for either the male or female samples (both p’s > 0.05), the directions were inverted (i.e. female participation was higher in the control and male participation was higher in the intervention). Thus, the second experiment did not reproduce the positive effect for the social responsibility message on female screening participation. Only gender and age were significant predictors of screening behavior, in that women and people aged 60 or older were more likely to participate in the screening program.
Table 4.
Adjusted logistic regression models for cancer screening screened in Trial 2.
| Model 1: Overall population |
Model 2: Male population only |
Model 3: Female population only |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total(%) | Odds ratio | 95% CI | p-value | Total(%) | Odds ratio | 95% CI | p-value | Total(%) | Odds ratio | 95% CI | p-value | |
| Overall | 20.7 | 17.7 | 23.7 | |||||||||
| Condition | ||||||||||||
| Control | 20.6 | Ref. | 17.0 | Ref. | 24.3 | Ref. | ||||||
| Social responsibility | 20.8 | 1.000 | 0.832–1.202 | 0.996 | 18.5 | 1.100 | 0.835–1.448 | 0.499 | 23.1 | 0.926 | 0.723–1.185 | 0.540 |
| Age | ||||||||||||
| 50–59 | 18.7 | Ref. | 15.9 | Ref. | 21.4 | Ref. | ||||||
| 60–69 | 23.3 | 1.444 | 1.200–1.737** | <0.001 | 20.0 | 1.314 | 0.998–1.732 | 0.052 | 26.7 | 1.342 | 1.047–1.718* | 0.020 |
| Gender | ||||||||||||
| Male | 17.7 | Ref. | ||||||||||
| Female | 23.7 | 1.329 | 1.106–1.598** | 0.002 | ||||||||
| N | 2791 | 1394 | 1,397 | |||||||||
| R2 (Nagelkerke) | 0.014 | 0.005 | 0.006 | |||||||||
* p < 0.05; ** p < 0.01.
4. Conclusion
To our knowledge, this is one of the first studies to test different messages that leverage behavioral economics principles for CRC screening in a real-world setting (Schwartz et al., 2017, Stoffel et al., 2019, Bakr et al., 2020) In two field experiments, we identified and tested promising behavioral messages for CRC screening. Trial 1 found, unexpectedly, that men and women responded to the behavioral messages in different ways. While women responded well to the social responsibility message, men responded badly to the same message. Thus, as the social responsibility message increased participation of women, it almost decreased male participation. While this result was consistent with previous studies that show that female participation in breast and cervical cancer screening is strongly associated with the feeling of moral obligation, the observed gender differences raises questions that require further work (Lechner et al., 1997, Howson, 1999, Tacken et al., 2007, Judah et al., 2009). An experimental study on hand-washing found that men responded better to disgust-based messages and women to messages about the dangers of failing to wash hands (Judah et al., 2009).
The second trial found that the social responsibility message from the first experiment did not affect female uptake when replicated with a larger number of participants, per trial arm, in a rural environment.
In line with Schwartz and colleagues (Schwartz et al., 2017) and Stoffel and colleagues (Stoffel et al., 2019 Feb) we did not find that including behavioral messages that highlight the benefit of screening, or the costs of non-attendance, influenced screening behavior. It is important to note that while Bakr and colleagues have found a positive effect for their intervention with implied scarcity, their study design leveraged several social psychology and behavioral economics principles, apart from the scarcity message. Their intervention letter also featured less text and multiple images (Bakr et al., 2020), making it impossible to determine whether the effect was due to implied scarcity.
The results raise the question why the social responsibility treatment worked for women in the first, but not in the second experiment. A possible explanation is that the first trial featured a significantly smaller sample with lower statistical power, which strongly reduces the chance of replication. An alternative explanation is that the two experiments featured different populations. While participants in the first experiment came from a town with around 20,000 inhabitants, and a relatively low share of people aged 50 or older (18.8%), the second experiment drew its participants from three small municipalities with a relatively high share of residents older than 50 years (between 28.4% and 33.7%). In this sense, participants in the rural setting could have been more likely to be aware of the social consequences, as they have a relatively larger social network of peers. This reasoning is consistent with results from previous studies that have shown that older adults in larger communities have fewer social interactions (Amato, 1993).
Strengths of our study include the use of a RCT design with objective data for participation and the replication of the experimental intervention in a larger trial to determine external validity and reliability. The non-significant effect of the interventions, based on behavioral economics, show the importance of proof-of-concept experiments to generate reliable evidence of the interventions in different settings (Stoffel et al., 2019).
There are several limitations to this study. The behavioral messages were not co-developed with patients, but stakeholders in the screening program. It is, therefore, possible that the messages did not communicate the information effectively. We would, therefore, advocate future studies to involve patients to develop behavioral messages. Additionally, some messages, such as the social responsibility and anticipated regret messages, were based on the theory of planned behavior and target intentions, which are often poor predictors of behavior (Sheeran and Webb, 2016).
Furthermore, we only collected information about the participant’s gender and age for the analysis. Little is known about how other socio-economic variables, such as education and health literacy, influence the perception of the behavioral messages, as no previous study has collected information about these variables. We suggest that future studies could test whether the effect of messages leveraged behavioral economics principles is mitigated by individuals’ socio-economic characteristics. Additionally, the behavioral messages were only displayed as the third paragraph in a relatively long invitation letter. It is possible that the insignificant effect of the messages could therefore be caused by individuals stop reading the letter prior to the paragraph. A small change like shortening the baseline letter could have increased the visibility of the behavioral message and the effectiveness of the interventions (Fox et al., 2020).
Furthermore, we conducted the two experiments in two distinct areas of Cyprus, the urban Aradippou in trial 1 and the rural villages of Meneou, Kiti and Dromolaxia in trial 2, which limits the comparability between the two trials. Finally, the first exploratory experiment contained an underpowered sample, which hinders the identification of efficacious messages. Thus, it may have led to spurious findings.
We conclude that the two experiments show the importance of proof-of-concept experiments to generate reliable evidence of the interventions. We recognize that more research on using messages from behavioral economics is needed and that the current study has raised several issues that warrant further exploration. While several studies have shown that combining multiple behavioral messages can increase screening uptake, it is important to investigate their effects individually. As the effect of behavioral messages may depend on socio-demographic characteristics, tailored messages may be required (Marcus et al., 2005, Noar et al., 2007 Jul).
5. Data availability statement
An anonymous data file is publicly available via the Open Science Framework and can be accessed at https://osf.io/wx7je/.
CRediT authorship contribution statement
Sandro Stoffel: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft. Stala Kioupi: Conceptualization, Methodology, Investigation, Writing - review & editing. Despina Ioannou: Conceptualization, Methodology, Investigation, Writing - review & editing. Robert S. Kerrison: Writing - review & editing. Christian von Wagner: Writing - review & editing. Benedikt Herrmann: Conceptualization, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was partially co-funded by The Cyprus Ministry of Health and the European Commission. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Aradippou has a population of 19,228 with around 18.8% of them being older than 50 years.[32]
Meneou, Dromolaxia, and Kiti are three small municipalities on the outskirt of the city of Larnaca. The population of these villages vary between 1625 for Meneou, 4252 for Kiti and 5064 for Dromolaxia in 2011.[32] The same statistics identified 28.4% of the residents in Kiti, 28.7% in Meneou and 33.7% in Dromolaxia to be older than 50 years.
The invitation letter consisted of one page and the length of the baseline invitation letter was 355 words. Hence, the interventions made the letter on average 17.2% longer.
The invitations to participate in the colorectal cancer screening were restricted to the full duration of the pilot (i.e. 2 months after receiving the invitation letter).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101499.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abraham C., Sheeran P. Deciding to exercise: The role of anticipated regret. British J. Health Psychol. 2004 May;9(2):269–278. doi: 10.1348/135910704773891096. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50(2):179–211. [Google Scholar]
- Amato P.R. Urban-rural differences in helping friends and family members. Social Psychology Q. 1993;56(4):249. doi: 10.2307/2786662. [DOI] [Google Scholar]
- Arkes H.R., Blumer C. The psychology of sunk cost. Organ. Behav. Hum. Decis. Process. 1985;35(1):124–140. [Google Scholar]
- Bakr O., Afsar-Manesh N., Raja N., Dermenchyan A., Goldstein N.J., Shu S.B., May F.P. Application of Behavioral Economics Principles Improves Participation in Mailed Outreach for Colorectal Cancer Screening. Clinical Transl. Gastroenterology. 2020;11(1) doi: 10.14309/ctg.0000000000000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes A.J., Groskaufmanis L., Thomson N.B., III Promising approaches from behavioral economics to improve patient lung cancer screening decisions. J. Am. College Radiol. 2016;13(12):1566–1570. doi: 10.1016/j.jacr.2016.09.004. [DOI] [PubMed] [Google Scholar]
- Basu P., Ponti A., Anttila A., Ronco G., Senore C., Vale D.B., Segnan N., Tomatis M., Soerjomataram I., Primic Žakelj M., Dillner J., Elfström K.M., Lönnberg S., Sankaranarayanan R. Status of implementation and organization of cancer screening in The European Union Member States—Summary results from the second European screening report. Int. J. Cancer. 2018;142(1):44–56. doi: 10.1002/ijc.31043. [DOI] [PubMed] [Google Scholar]
- Beeker C., Kraft J.M., Southwell B.G., Jorgensen C.M. Colorectal cancer screening in older men and women: qualitative research findings and implications for intervention. J. Community Health. 2000;25(3):263–278. doi: 10.1023/a:1005104406934. [DOI] [PubMed] [Google Scholar]
- Bell D.E. Regret in decision making under uncertainty. Oper. Res. 1982;30(5):961–981. [Google Scholar]
- BROCK TIMOTHY.C. Psychological Foundations of Attitudes. Elsevier; 1968. pp. 243–275. [DOI] [Google Scholar]
- Champion V.L., Skinner C.S. The health belief model. Health Behavior Health Educ.: Theory, Res. Practice. 2008;4:45–65. [Google Scholar]
- Cohen J. 1988. Statistical power analysis for the behavioral sciences, 2nd edn. Á/L.
- Conner M., McEachan R., Taylor N., O'Hara J., Lawton R. Role of affective attitudes and anticipated affective reactions in predicting health behaviors. Health Psychol. 2015 Jun;34(6):642–652. doi: 10.1037/hea0000143. [DOI] [PubMed] [Google Scholar]
- Cotrim H., Pereira G. Impact of colorectal cancer on patient and family: implications for care. European Journal of Oncology Nursing. 2008;12(3):217–226. doi: 10.1016/j.ejon.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Cox D., Cox A.D. Communicating the consequences of early detection: The role of evidence and framing. J. Marketing. 2001;65(3):91–103. [Google Scholar]
- Duffy S.W., Myles J.P., Maroni R., Mohammad A. Rapid review of evaluation of interventions to improve participation in cancer screening services. J. Med. Screen. 2017;24(3):127–145. doi: 10.1177/0969141316664757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farazi P.A. Cancer trends and risk factors in Cyprus. Ecancermedicalscience. 2014;8:389. doi: 10.3332/ecancer.2014.389. Published 2014 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer R.A., Klein W.M.P., Zajac L.E., Land S.R., Ling B.S. An affective booster moderates the effect of gain-and loss-framed messages on behavioral intentions for colorectal cancer screening. J. Behav. Med. 2012;35(4):452–461. doi: 10.1007/s10865-011-9371-3. [DOI] [PubMed] [Google Scholar]
- Fox C.R., Doctor J.N., Goldstein N.J., Meeker D., Persell S.D., Linder J.A. Details matter: predicting when nudging clinicians will succeed or fail. BMJ. 2020;370 doi: 10.1136/bmj.m3256. [DOI] [PubMed] [Google Scholar]
- Frazier A.L., Colditz G.A., Fuchs C.S., Kuntz K.M. Cost-effectiveness of screening for colorectal cancer in the general population. JAMA. 2000;284(15):1954–1961. doi: 10.1001/jama.284.15.1954. [DOI] [PubMed] [Google Scholar]
- Garcia M., Borràs J.M., Milà N., Espinàs J.A., Binefa G., Fernández E., Farré A., Pla M., Cardona A., Moreno V. Factors associated with initial participation in a population-based screening for colorectal cancer in Catalonia, Spain: a mixed-methods study. Prev. Med. 2011;52(3–4):265–267. doi: 10.1016/j.ypmed.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Greiner K.A., Born W., Nollen N., Ahluwalia J.S. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J. Gen. Intern. Med. 2005;20(11):977–983. doi: 10.1111/j.1525-1497.2005.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirst Y., Stoffel S., Baio G., McGregor L., von Wagner C. Uptake of the English Bowel (Colorectal) Cancer Screening Programme: an update 5 years after the full roll-out. Eur. J. Cancer. 2018;1(103):267–273. doi: 10.1016/j.ejca.2018.07.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard K., Salkeld G. Does attribute framing in discrete choice experiments influence willingness to pay? Results from a discrete choice experiment in screening for colorectal cancer. Value in health. 2009;12(2):354–363. doi: 10.1111/j.1524-4733.2008.00417.x. [DOI] [PubMed] [Google Scholar]
- Howson A. Cervical screening, compliance and moral obligation. Sociol. Health Illn. 1999;21(4):401–425. [Google Scholar]
- Huf S., Kerrison R.S., King D., Chadborn T., Richmond A., Cunningham D., Friedman E., Shukla H., Tseng F.-M., Judah G., Darzi A., Vlaev I. Behavioral economics informed message content in text message reminders to improve cervical screening participation: Two pragmatic randomized controlled trials. Prev. Med. 2020;139:106170. doi: 10.1016/j.ypmed.2020.106170. [DOI] [PubMed] [Google Scholar]
- Judah G., Aunger R., Schmidt W.-P., Michie S., Granger S., Curtis V. Experimental pretesting of hand-washing interventions in a natural setting. Am. J. Public Health. 2009;99(S2):S405–S411. doi: 10.2105/AJPH.2009.164160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson N., Loewenstein G., Seppi D. The ostrich effect: Selective attention to information. Journal of Risk and uncertainty. 2009;38(2):95–115. [Google Scholar]
- Karsa L.V., Anttila A., Ronco G., Ponti A., Malila N., Arbyn M., Segnan N., Castillo-Beltran M., Boniol M., Ferlay J., Hery C. Cancer screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. 2008. Cancer screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. [Google Scholar]
- Klabunde C., Blom J., Bulliard J.-L., Garcia M., Hagoel L., Mai V., Patnick J., Rozjabek H., Senore C., Törnberg S. Participation rates for organized colorectal cancer screening programmes: an international comparison. J. Med. Screen. 2015;22(3):119–126. doi: 10.1177/0969141315584694. [DOI] [PubMed] [Google Scholar]
- Lechner L., de Vries H., Offermans N. Participation in a breast cancer screening program: influence of past behavior and determinants on future screening participation. Prev. Med. 1997;26(4):473–482. doi: 10.1006/pmed.1997.0161. [DOI] [PubMed] [Google Scholar]
- Marcus A.C., Mason M., Wolfe P., Rimer B.K., Lipkus I., Strecher V., Warneke R., Morra M.E., Allen A.R., Davis S.W., Gaier A., Graves C., Julesberg K., Nguyen L., Perocchia R., Speyer J.B., Wagner D., Thomsen C., Bright M.A. The efficacy of tailored print materials in promoting colorectal cancer screening: results from a randomized trial involving callers to the National Cancer Institute's Cancer Information Service. J. Health Comm. 2005;10(sup1):83–104. doi: 10.1080/10810730500257754. [DOI] [PubMed] [Google Scholar]
- McGregor S.E., Hilsden R.J., Li F.X., Bryant H.E., Murray A. Low uptake of colorectal cancer screening 3 yr after release of national recommendations for screening. Am. J. Gastroenterol. 2007;102(8):1727–1735. doi: 10.1111/j.1572-0241.2007.01217.x. [DOI] [PubMed] [Google Scholar]
- Mehta S.J., Feingold J., Vandertuyn M., Niewood T., Cox C., Doubeni C.A., Volpp K.G., Asch D.A. Active choice and financial incentives to increase rates of screening colonoscopy–a randomized controlled trial. Gastroenterology. 2017;153(5):1227–1229.e2. doi: 10.1053/j.gastro.2017.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S.J., Khan T., Guerra C., Reitz C., McAuliffe T., Volpp K.G., Asch D.A., Doubeni C.A. A Randomized Controlled Trial of Opt-in Versus Opt-Out Colorectal Cancer Screening Outreach. Am. J. Gastroenterology. 2018;113(12):1848. doi: 10.1038/s41395-018-0151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerowitz B.E., Chaiken S. The effect of message framing on breast self-examination attitudes, intentions, and behavior. J. Pers. Soc. Psychol. 1987;52(3):500–510. doi: 10.1037//0022-3514.52.3.500. [DOI] [PubMed] [Google Scholar]
- Myers R.E., Ross E.A., Wolf T.A., Balshem A., Jepson C., Millner L. Behavioral interventions to increase adherence in colorectal cancer screening. Med. Care. 1991;29(10):1039–1050. doi: 10.1097/00005650-199110000-00009. [DOI] [PubMed] [Google Scholar]
- Myers R.E., Ross E., Jepson C., Wolf T., Balshem A., Millner L., Leventhal H. Modeling adherence to colorectal cancer screening. Rehabilitation Oncol. 1997;15(1):28–29. doi: 10.1006/pmed.1994.1020. [DOI] [PubMed] [Google Scholar]
- Noar S.M., Benac C.N., Harris M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol. Bull. 2007 Jul;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- O'Carroll R.E., Foster C., McGeechan G., Sandford K., Ferguson E. The, “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol. 2011 Mar;30(2):236–245. doi: 10.1037/a0022379. [DOI] [PubMed] [Google Scholar]
- Okeefe D.J., Jensen J.D. The advantages of compliance or the disadvantages of noncompliance? A meta-analytic review of the relative persuasive effectiveness of gain-framed and loss-framed messages. Ann. Int. Commun. Assoc. 2006;30(1):1–43. [Google Scholar]
- Panidi, K., 2015. Ostrich Effect in Health Care Decisions: Theory and Empirical Evidence. Available at SSRN 2932181. 2015 Feb.
- Ponti A., Anttila A., Ronco G., Senore C., Basu P., Segnan N. European Commission; Brussels: 2017. Cancer screening in the European Union. [Google Scholar]
- Power E., Miles A., von Wagner C., Robb K., Wardle J. Uptake of colorectal cancer screening: system, provider and individual factors and strategies to improve participation. Future Oncol. 2009;5(9):1371–1388. doi: 10.2217/fon.09.134. [DOI] [PubMed] [Google Scholar]
- Purnell J.Q., Thompson T., Kreuter M.W., McBride T.D. Peer reviewed: Behavioral economics:“nudging” underserved populations to be screened for cancer. Preventing Chronic Disease. 2015;12 doi: 10.5888/pcd12.140346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman A.J., Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol. Bull. 1997;121(1):3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- Rothman A.J., Salovey P., Antone C., Keough K., Martin C.D. The influence of message framing on intentions to perform health behaviors. J. Exp. Soc. Psychol. 1993;29(5):408–433. [Google Scholar]
- Schultz P.W., Nolan J.M., Cialdini R.B., Goldstein N.J., Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol. Sci. 2007;18(5):429–434. doi: 10.1111/j.1467-9280.2007.01917.x. [DOI] [PubMed] [Google Scholar]
- Schwartz P.H., Perkins S.M., Schmidt K.K., Muriello P.F., Althouse S., Rawl S.M. Providing quantitative information and a nudge to undergo stool testing in a colorectal cancer screening decision aid: a randomized clinical trial. Med. Decis. Making. 2017;37(6):688–702. doi: 10.1177/0272989X17698678. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Harris P.R., Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol. Bull. 2014 Mar;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Webb T.L. The intention–behavior gap. Soc. Pers. Psychol. Compass. 2016;10(9):503–518. [Google Scholar]
- Sieverding M., Decker S., Zimmermann F. Information about low participation in cancer screening demotivates other people. Psychol. Sci. 2010;21(7):941–943. doi: 10.1177/0956797610373936. [DOI] [PubMed] [Google Scholar]
- Stoffel S., Benito L., Milà N., Travier N., Binefa G., Vidal C., Espinosa J., Moreno V., Garcia M. Testing behavioral interventions to optimize participation in a population-based colorectal cancer screening program in Catalonia. Spain. Preventive Med. 2019;119:58–62. doi: 10.1016/j.ypmed.2018.12.013. [DOI] [PubMed] [Google Scholar]
- Stoffel S.T., Goodwin M., Sieverding M., Vlaev I., von Wagner C. Testing verbal quantifiers for social norms messages in cancer screening: evidence from an online experiment. BMC public health. 2019;19(1):658. doi: 10.1186/s12889-019-6997-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffel S.T., Yang J., Vlaev I., von Wagner C., Quaife M. Testing the decoy effect to increase interest in colorectal cancer screening. PLoS ONE. 2019;14(3):e0213668. doi: 10.1371/journal.pone.0213668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffel S.T., Kerrison R.S., Vlaev I., von Wagner C. Offering male endoscopists as decoy option to nudge disinclined women to have colorectal cancer screening. J Behav Med. 2020;43(3):511–518. doi: 10.1007/s10865-019-00095-4. [DOI] [PubMed] [Google Scholar]
- Stoffel S.T., Bombagi M., Kerrison R.S., von Wagner C., Herrmann B. Testing Enhanced Active Choice to Optimize Acceptance and Participation in a Population-Based Colorectal Cancer Screening Program in Malta. Behav. Med. 2021;15:1–6. doi: 10.1080/08964289.2020.1828254. [DOI] [PubMed] [Google Scholar]
- Tacken M.A., Braspenning J.C., Hermens R.P., Spreeuwenberg P.M., Van Den Hoogen H.J., De Bakker D.H., Groenewegen P.P., Grol R.P. Uptake of cervical cancer screening in The Netherlands is mainly influenced by women's beliefs about the screening and by the inviting organization. Eur. J. Public Health. 2007;17(2):178–185. doi: 10.1093/eurpub/ckl082. [DOI] [PubMed] [Google Scholar]
- Tversky A., Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- Verhallen T.M.M. Scarcity and consumer choice behavior. J. Econ. Psychol. 1982;2(4):299–322. [Google Scholar]
- Verhallen T.M.M., Robben H.S.J. Scarcity and preference: An experiment on unavailability and product evaluation. J. Econ. Psychol. 1994;15(2):315–331. [Google Scholar]
- von Karsa L., Patnick J., Segnan N., Atkin W., Halloran S., Lansdorp-Vogelaar I., Malila N., Minozzi S., Moss S., Quirke P., Steele R.J. European guidelines for quality assurance in colorectal cancer screening and diagnosis: overview and introduction to the full supplement publication. Endoscopy. 2013;45(1):51. doi: 10.1055/s-0032-1325997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Wagner C., Hirst Y., Waller J.o., Ghanouni A., McGregor L.M., Kerrison R.S., Verstraete W., Vlaev I., Sieverding M., Stoffel S.T. The impact of descriptive norms on motivation to participate in cancer screening–Evidence from online experiments. Patient Educ. Couns. 2019;102(9):1621–1628. doi: 10.1016/j.pec.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, J.L., Herdman, R.C., Wadhwa, S., 1991. Cost effectiveness of colorectal cancer screening in the elderly. [DOI] [PubMed]
- Weitzman E.R., Zapka J., Estabrook B., Goins K.V. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev. Med. 2001;32(6):502–513. doi: 10.1006/pmed.2001.0838. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
An anonymous data file is publicly available via the Open Science Framework and can be accessed at https://osf.io/wx7je/.