Abstract
Background and Purpose: Transverse abdominis plane (TAP) block has been suggested to reduce post-operative pain after laparoscopic cholecystectomy (LC). However, the literature is divided on whether ultrasound (USG)-guided TAP block is effective for pain control after LC. The present meta-analysis therefore evaluated the efficacy of USG-guided TAP block vs. controls and port site infiltration for pain control after LC.
Methods: A comprehensive literature search of online academic databases was performed for published randomized controlled trials (RCTs) for studies published to January 31, 2021. The primary outcome analyzed was post-operative pain score at 0, 6, 12, and 24 h post-surgery, both during rest and while coughing. Secondary outcomes included morphine consumption and post-operative nausea and vomiting (PONV) incidence.
Results: A total of 23 studies with data on 1,450 LC patients were included in our meta-analysis. A reduction in pain intensity at certain post-operative timepoints was observed for USG-guided TAP block patients compared to control group patients. No reduction in pain intensity was observed for patients receiving USG-guided TAP block patients vs. conventional Port site infiltration.
Conclusion: This meta-analysis concludes that TAP block is more effective than a conventional pain control, but not significatively different from another local incisional pain control that is port site infiltration. Additional prospective randomized controlled trials are required to further validate our findings.
Keywords: laparoscopic cholecystectomy, analgesia, transverse abdominis plane block, ultrasound, pain control
Introduction
Laparoscopic cholecystectomy (LC) is currently the gold standard treatment for symptomatic gall bladder disorders, including cholelithiasis and cholecystitis (1, 2). However, LC, while minimally invasive, is associated with post-operative pain, especially within the first 24 h. This pain is routinely managed using opiates, which are associated with a number of side effects, including excessive sedation and post-operative nausea and vomiting (PONV). As these side effects may increase hospital stay durations, proper pain control and management are therefore critical for improving clinical outcomes and promoting earlier ambulation post-surgery (3–5).
Transversus abdominis plane (TAP) block is a regional anesthetic technique that has gradually become an alternative for post-operative pain control. It involves the infusion of local anesthetic into the fascial plane of the abdominal wall where the T6 to L1 nerves are found (5). Conventionally, TAP block was performed using anatomical landmarks, but ultrasound (USG)-guided TAP block has become more popular in recent years (6–10).
A previously published meta-analysis detailing seven randomized controlled trials (RCTs) showed TAP block to be effective when compared with standard analgesia in adults undergoing LC (11). However, they lacked evidence to compare the efficacy of TAP block against conventional port site infiltration for post-LC pain control. The current study aims to systematically review all available RCTs to evaluate the efficacy of USG-guided TAP block against conventional analgesia and port site infiltration in LC patients.
Materials and Methods
Search Strategy
This meta-analysis was performed using Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (12). A comprehensive literature search for RCTs published prior to January 31, 2021 was conducted using the following electronic databases: PubMed, Google scholar, Cochrane Library, Scopus, and TRIP. The following search terms were employed: “Transabdominal abdominis plane block” OR “Tap block” OR “Plane Block” OR “Ultrasound guided TAP block” AND “Laparoscopic cholecystectomy” AND “Pain Control” AND “Analgesic” OR “Local Anesthesia” OR “Infiltration anesthesia.” Literature cited by included studies were also manually searched for additional eligible studies. The literature search did not restrict for language.
Study Eligibility Criteria
RCTs involving adult patients undergoing elective LC that compared the efficacy of USG-guided TAP block against either control or port-site infiltration groups were included. Studies that did not report pain outcomes were not included. Studies where full-texts were not available were not included.
Data Collection and Analysis
All eligible studies were screened by two independent reviewers using the selection criteria listed above. Screening first entailed abstract review, followed by full-text review. Any discrepancies were settled through discussion with a third reviewer. Articles published in a language other than English were machine translated using Google Translate and considered for inclusion. The following information was extracted from each included study: number of patients, investigation groups, types of analgesia used, outcome measurements, treatments, interventions, and adverse effects.
Primary Outcome
The primary outcome evaluated in this study was pain control in LC patients, as measured using 1–10 rating scales such as the visual analog scale (VAS) or numerical rating scale (NRS). Measurements at 0, 6, 12, and 24 h post-operation, both at rest and while coughing, were noted.
Secondary Outcomes
Secondary outcomes in this study included morphine consumption and post-operative nausea and vomiting (PONV) incidence.
Quality Assessment
Studies were assessed for quality using a modified JADAD score (13) that evaluated study methods, randomization approaches, blinding, withdrawals and dropouts, inclusion and exclusion criteria, approaches used to assess adverse effects, and statistical analysis. Scores ranged from 0 (lowest quality) to 8 (highest quality). Study quality was assessed independently by two reviewers. All discrepancies were resolved through discussion.
Publication Bias
Publication bias was assessed using funnel plot analysis. Funnel plot asymmetry was assessed using Egger's regression test (14, 15).
Statistical Analysis
Mean difference (MDs) with 95% confidence intervals (CIs) was calculated for the continuous outcome. Risk ratios (RR) with 95% CIs were calculated for categorical outcomes to estimate pooled findings. Study heterogeneity was evaluated using the I2 statistic. For I2 values >50%, a random-effects model was applied. For I2 values below 50%, a fixed-effect model was applied. Statistical analyses were conducted using Review Manager software (Version 5.3, Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration 2014).
Results
Literature Search
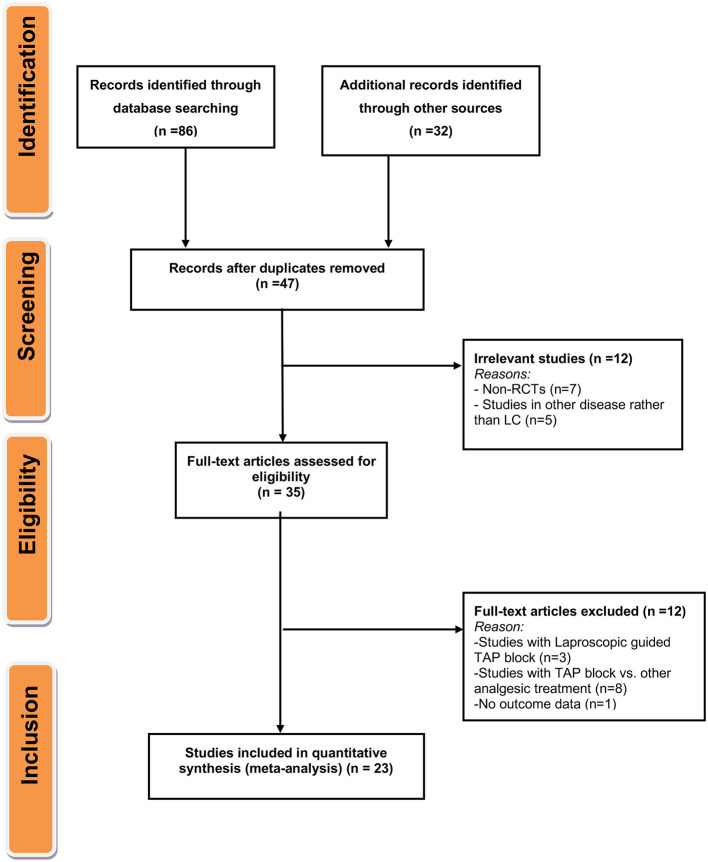
Primary screening yielded 118 candidate articles. Of these, 47 underwent full-text screening and review. Ultimately, 23 studies containing data on 1,450 patients met inclusion criteria (Figure 1).
Figure 1.
Flow diagram for the selection of studies and specific reasons for exclusion from the present meta-analysis.
Characteristics of Included Studies
A full summary of extracted data from included studies is presented in Table 1. Included studies were published between 2009 and 2020, with individual study samples ranging from 40 to 120 individuals. All included studies were of moderate or high quality based on JADAD Score (Table 2). Out of 23 included studies, 14 studies (16–18, 23–25, 27, 30, 31, 34–38, 40) were conducted in Caucasian individuals, with the remaining nine studies (19–22, 26, 28, 29, 32, 33) were conducted on an Asian population.
Table 1.
Baseline and clinical characteristic of the included studies in the meta-analysis for the efficacy of transversus abdominis plane block for pain control after laparoscopic cholecystectomy.
| S. No | References | Country | Ethnicity | Groups investigated | TAP approach | Comparator | Treatment | Anesthesia | Post-operative analgesia |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Arik et al. (16) | Turkey | Caucasian | TAP Block (n = 24) Control (n = 24) Port Site Infiltration (n = 24) |
Patients received unilateral subcostal TAP block | Patients received intravenously patient-controlled analgesia (IV PCA) or local anesthetic infiltration at port sites | 0.25% bupivacaine | Propofol, fentanyl, and rocuronium | Paracetamol IV, 1 mg/kg tramadol IV, and ondansetron 0.1 mg/kg IV |
| 2 | Tulgar et al. (17) | Turkey | Caucasian | Subcostal TAP Block (n = 20) Control (n = 20) |
OSTAP blocks | Control as standard analgesia plan with no block | No details provided | Propofol 2–3 mg/kg, fentanyl 100 μg, and rocuronium bromide 0.6 mg/kg. 0.6 minimum alveolar concentration sevoflurane and 0.08 μg/kg/min remifentanil infusion | 1 gm paracetamol and 20 mg tenoxicam. |
| 3 | Houben et al. (18) | Belgium | Caucasian | Subcostal TAP Block (n = 26) Control (n = 26) |
USG guided bilateral subcostal TAP block with 20 ml of levobupivacaine 0.375% and epinephrine 5 mg/ml_ | Patients receiving 0.9% saline with epinephrine 5 mg/ml | levobupivacaine 0.375% and epinephrine 5 mg/ml | Propofol 2 mg/kg and sufentanil 0.1 mg/kg. Rocuronium 0.6mg/kg | Paracetamol and morphine in addition to the pre-operative NSAID and intra-operative ketamine and dexamethasone |
| 4 | Baral and Poudel (19) | Nepal | Asian | Subcostal TAP Block (n = 30) Port Site Infiltrate (n = 30) |
Bilateral USG guided subcostal TAP block with 10 mL of 0.25% bupivacaine after the completion of surgery. | Patients receiving similar amount of local anesthetic infiltrated over all the laparoscopic port sites | 0.25% bupivacaine | Fentanyl (2 mcg/kg), propofol (2 mg/kg), and vecuronium (0.8 mg/kg). | Injection Paracetamol 1 gm 6 hourly |
| 5 | Bava et al. (20) | India | Asian | TAP Block (n = 21) Port Site Infiltration (n = 21) |
USG bilateral mid-axillary TAP blocks with 0.375% ropivacaine | Local anesthetic infiltration of the port site | 0.375% ropivacaine | intravenously (IV)-administered propofol 2 mg/kg, fentanyl 2 μg/kg, and atracurium 0.5 mg/kg | 0.5 μg/kg IV fentanyl |
| 6 | Khandelwal et al. (21) | India | Asian | TAP Block (n = 40) Control (n = 40) |
USG guided STA block with 0.25% levobupivacaine both sides | Patients received 0.25% levobupivacaine through intraperitoneal route. | 0.25% levobupivacaine | Propofol 2–3 mg/kg, fentanyl 2 μg/kg, and vecuronium 0.1 mg/kg | Paracetamol 15 mg/kg |
| 7 | Suseela et al. (22) | India | Asian | TAP Block (n = 40 Port Site Infiltration (n = 40) |
USG guided bilateral subcostal TAP block (T) with 0.25% bupivacaine 20 ml each side | Port-site infiltration with 0.5% bupivacaine 5 ml each at 4 ports (I) | 0.5% bupivacaine | Propofol 2 mg/kg IV and injection fentanyl 2 μg/kg IV. | Tramadol 1 mg/kg intravenous bolus and diclofenac 1 mg/kg intravenous infusion |
| 8 | Ortiz et al. (23) | USA | Caucasian | TAP Block (n = 39) Port Site Infiltration (n = 35) |
Bilateral USG guided TAP blocks | Preincisional infiltration of the 4-trocar insertion | 15 mL of ropivacaine 0.5% | fentanyl 2 Kg/kg and propofol 2.5 mg/kg. | Morphine, Fentanyl, Hydrocodone |
| 9 | Saliminia et al. (24) | Iran | Caucasian | Control (n = 18) TAP Block (n =18) Bupivacaine, sufentanil TAP Block (n =18) Bupivacaine |
TAP block with bupivacaine and TAP block with bupivacaine plus sufentanil | TAP block with normal saline | bupivacaine 0.5% /2 mL (10 mg) sufentanil | 50 mg fentanyl with lockout at 8-min | 2 mg/kg intravenous (IV) propofol and 3 mg/kg IV fentanyl, tracheal intubation was facilitated by 0.6 mg/kg IV atracurium and anesthesia was maintained with 80e100 mg/kg/min propofol and 1 mg/kg IV fentanyl and 0.3 mg/kg IV atracurium administrated every 30 min. |
| 10 | Basaran et al. (25) | Turkey | Caucasian | Subcostal TAP group (n = 38) control group (n = 38). |
Bilateral ultrasound-guided OSTAP blocks | Control Group | 20 ml 0.25% bupivacaine | propofol 1–1.5 mg/kg and fentanyl 2 μg/kg. | tenoxicam, Morphine, Fantanyl, Tremadol |
| 11 | Ra et al. (26) | Korea | Asian | Control (n = 18) TAP block 0.25% (n = 18) TAP block 0.5% (n = 18 |
USG guided TAP block | Standard general anesthetic as control | Bilateral 15 ml of 0.25 or 0.5% L-bupivacaine after induction | Midazolam/propofol/ remifentanil | Ketorolac 30 mg and fentanyl 20 μg in the recovery room if needed, ketorolac 30 mg every 8 h on the ward |
| 12 | El-Dawlatly et al. (27) | Austria | Caucasian | TAP Block (n = 21) Control (n = 21) |
USG guided bilateral TAP block | Standard general anesthetic as control | Bilateral 15 ml of 0.5 % Bupivacaine after induction | Propofol/sufentanil/ sevoflurane | PCA morphine bolus 1.5 mg IV with no basic infusion and 15 min lock out time |
| 13 | Chen et al. (28) | Malaysia | Asian | Control (n = 20) Subcostal TAP block (n = 20) |
Bilateral OSTAP block using 1.5 mg/kg ropivacaine on each side | IV morphine 0.1 mg/kg | Bilateral 20 ml of 0.375% ropivacaine after induction | Propofol /fentanyl/ sevoflurane | Morphine 0.05 mg/kg, i.v., if needed |
| 14 | Shin et al. (29) | South Korea | Asian | Control (n = 15) TAP block (n = 15) Subcostal STAP block (n = 15) |
TAP block or OSTAP block | Standard postoperative pain control alone | Bilateral 20 ml of 0.375% ropivacaine after induction | Propofol/ fentanyl/ sevoflurane | Fentanyl 25 μg, i.v. + ketorolac 30 mg in the recovery room and nalbuphine 10 mg on the ward if needed |
| 15 | Dost et al. (30) | Turkey | Caucasian | TAP block (n = 25) 0.25% levobupivacaine TAP block (n = 25) 0.5% levobupivacaine Control group (n = 25) |
20 mL of levobupivacaine 0.5% and 30 mL 0.25% levobupivacaine was applied with a USG-guided TAP block | No TAP block or LAI was applied to the control group | levobupivacaine 0.5%/0.25% | IV propofol and 1 mcg / kg IV fentanyl | Mephridine, fentanyl, tremadol |
| 16 | Petersen et al. (31) | Denmark | Caucasian | Control (n = 37) TAP block (n = 37) |
Bilateral USG guided posterior TAP blocks (20 mL 0.5% ropivacaine) | placebo blocks | Bilateral 20 ml of 0.5% ropivacaine after induction | Propofol/ remifentanil/ sufentanil | Oral acetaminophen 1 g and ibuprofen 400 mg every 6 h, morphine 2.5 mg, i.v., in the recovery room and oral ketobemidone 2.5 mg on the ward if needed |
| 17 | Venkatraman et al. (32) | India | Asian | Subcostal TAP block (n = 40) Control (n = 40) |
USG guided Subcostal TAP block | Laparoscopy-guided subcostal TAP block | 20 mL of 0.2%ropivacaine and 8 mg dexamethasone. | Propofol 2 mg/kg and cisatracurium 1.5 mg/kgwas | Fentanyl 2 μg/kg |
| 18 | Bhatia et al. (33) | India | Asian | Control (n = 20) TAP block (n = 20) Subcostal TAP block (n = 20) |
Patients received an USG guided posterior TAP block using 15 mL of 0.375% ropivacaine on each side; and patients underwent a subcostal TAP block with 15 mL of 0.375% ropivacaine on each side | Patients received standard general anesthesia (control group); | Bilateral 15 ml of 0.375% ropivacaine | Propofol/morphine/ nitrous oxide/ isoflurane | Acetaminophen 1 g, i.v., every 6 h, tramadol 2 mg/kg, i.v., as an initial dose and 1 mg/kg if needed |
| 19 | Breazu et al. (34) | Romania | Caucasian | Subcostal TAP-Placebo (n = 25) OSTAP-Bupivacaine (n = 25) OSTAP-Pethidine (n = 25) |
OSTAP-Bupivacaine (treated with 0.25% bupivacaine) and OSTAP-Pethidine (treated with 1% pethidine). | OSTAP-Placebo (treated with normal saline); | Bilateral 0.25% bupivacaine/ 20 ml of 1% pethidine | 7.5 mg of midazolam, 60 min before the surgery, followed by the induction with 2 mcg/kg of fentanyl, 2 mg/kg of propofol, 0.6 mg/kg of rocuronium or 0.5 mg/kg of atracurium | 1 g of IV acetaminophen at 8 h |
| 20 | Breazu et al. (35) | Romania | Caucasian | Subcostal TAP block (n =30) Subcoastal Placebo (n = 30) |
Bilateral OSTAP Block receiving preoperatively with 0.25% bupivacaine. | Bilateral OSTAP Placebo receiving preoperatively with sterile normal saline | Bilateral 0.25% bupivacaine | Midazolam 7.5 mg orally 60 min before surgery, fentanyl 2 μg/kg, propofol 2 mg/kg, rocuronium 0.6 mg/kg or atracurium 0.5 mg/kg | Acetaminofen 15–20 mg/kg |
| 21 | Vrsajkov et al. (36) | Serbia | Caucasian | Subcostal TAP (n = 36) Control (n = 36) |
USG guided subcostal TAP block | Control receiving standard postoperative analgesia | 0.33% bupivacaine | Propofol (2.5 mg/kg), fentanyl (3 mcg/kg) and rocuronium (0.6–0.8 mg/kg) | Tramadol 1 mg/kg per 6 h |
| 22 | Tor et al. (37) | Turkey | Caucasian | TAP Block (n = 50) Port Site Infiltrate (n = 50) |
USG guided TAP block with 30 ml 0.25% bupivacaine solution | 20 ml 0.25% bupivacaine solution injected in three port incision sites. | Bilateral 15 ml of 0.5% bupivacaine | Propofol/fentanyl /Rocuronium | 50 mg Tramadol and 800 mg Ibuprofen |
| 23 | Tolchard et al. (38) | UK | Caucasian | Subcostal STAP (n = 21) Port Site Infiltrate (n = 22) |
USG guided STA block | port-site infiltration of local anesthetic | 1 mg/kg bupivacaine | Propofol (2.5 mg/kg), fentanyl (3 mcg/kg), and atracurium (0.6 mg/kg), | Paracetamol(15–20 mg/kg) and diclofenac (0.5 mg/kg) |
Table 2.
Quality assessment using modified Jadad scores (Points 1–8) for the included studies in the meta-analysis.
| References | Was the research described as randomized? | Was the approach of randomization appropriate? | Was the research described as blinding? | Was the approach of blinding appropriate? | Was the approach used to assess adverse effects described? | Was there a presentation of the inclusion/exclusion criteria?# | Was there a presentation of withdrawals and dropouts?# | Was the approach of statistical analysis described? | Total score (max-8) |
|---|---|---|---|---|---|---|---|---|---|
| Arik et al. (16) | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Tulgar et al. (17) | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 |
| Vindal et al. (39) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Houben et al. (18) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Baral and Poudel (19) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Bava et al. (20) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Khandelwal et al. (21) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Suseela et al. (22) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Ortiz et al. (23) | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Saliminia et al. (24) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Basaran et al. (25) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Ra et al. (26) | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 4 |
| El-Dawlatly et al. (27) | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 3 |
| Chen et al. (28) | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Shin et al. (29) | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Dost et al. (30) | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 3 |
| Baytar et al. (40) | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Petersen et al. (31) | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 3 |
| Venkatraman et al. (32) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Bhatia et al. (33) | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Breazu et al. (34) | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Breazu et al. (35) | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Vrsajkov et al. (36) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Tor et al. (37) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Tolchard et al. (38) | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
“1” means “Yes”, “0” means “Not described”.
For the primary outcome of pain control at rest and during coughing, out of 23 studies, 22 studies were included in the analysis for which references have been provided in Table 3. Some of the included studies had reported data only for one or two timepoints for post-operative pain score either for 0 or 6 or 12 or 24 h at rest or during coughing (17, 18, 20, 22–24, 26, 28, 30, 36–38). A single study by El-Dawlatly et al. (27) only provided the data for morphine consumption. PONV data was available for 12 studies (16, 18, 19, 21, 23, 25, 28, 29, 31, 33, 36, 37) (750 LC patients). Information on morphine consumption up to 24 h post-operation was reported by seven studies (16, 17, 23, 27–29, 31) (348 LC subjects).
Table 3.
Summary of findings for the included studies investigating the efficacy of TAP block for pain control after LC.
| Timepoint after surgery | Groups | Status | No. of studies | Total participants | MD (95% CI) | p-value | I2 (%) | References |
|---|---|---|---|---|---|---|---|---|
| 0 h | USG TAP block vs. Control | Rest | 13 | 850 | −1.53 [−2.21, −0.84] | <0.0001 | 98 | (16, 17, 21, 24, 25, 29–36) |
| Coughing | 9 | 578 | −1.72 [−2.48, −0.97] | <0.0001 | 92 | (16, 17, 21, 29, 31–35) | ||
| USG TAP block vs. Port site Infiltrate | Rest | 6 | 385 | −0.26 [−1.03, 0.51] | 0.51 | 93 | (16, 19, 20, 23, 37, 38) | |
| Coughing | 3 | 208 | −1.28 [−2.73, 0.16] | 0.08 | 84 | (16, 20, 37) | ||
| 6 h | USG TAP block vs. Control | Rest | 12 | 730 | −1.19 [−1.62, −0.77] | <0.0001 | 94 | (16, 21, 24–26, 29, 31–35) |
| Coughing | 9 | 582 | −0.53 [−0.94, −0.13] | 0.010 | 90 | (16, 17, 21, 29, 31–35) | ||
| USG TAP block vs. Port site Infiltrate | Rest | 5 | 322 | −0.41 [−1.37, 0.56] | 0.41 | 94 | (16, 19, 20, 22, 23) | |
| Coughing | 3 | 168 | −0.36 [−0.97, 0.25] | 0.25 | 0 | (16, 19, 20) | ||
| 12 h | USG TAP block vs. Control | Rest | 8 | 512 | −0.75 [−1.24, −0.27] | 0.002 | 85 | (16, 17, 21, 24, 26, 32, 33, 36) |
| Coughing | 6 | 398 | −0.49 [−1.06, 0.09] | 0.10 | 79 | (16, 17, 21, 30, 33, 35) | ||
| USG TAP block vs. Port site Infiltrate | Rest | 5 | 322 | −0.53 [−1.51, 0.45] | 0.29 | 95 | (16, 19, 20, 22, 23) | |
| Coughing | 3 | 168 | −1.44 [−3.25, 0.37] | 0.12 | 93 | (16, 19, 20) | ||
| 24 h | USG TAP block vs. Control | Rest | 12 | 746 | −0.53 [−0.83, −0.23] | 0.0005 | 86 | (16, 17, 21, 24, 25, 29, 31–35) |
| Coughing | 9 | 578 | −0.37 [−0.66, −0.08] | 0.01 | 87 | (16, 17, 21, 25, 29–31, 33, 35) | ||
| USG TAP block vs. Port site Infiltrate | Rest | 5 | 322 | 0.22 [−1.12, 1.55] | 0.75 | 97 | (16, 19, 20, 22, 23) | |
| Coughing | 3 | 168 | −0.36 [−0.85, 0.12] | 0.14 | 0 | (16, 19, 20) |
Bold values of mean differences (MD) represent statistically significant results (p-value < 0.05).
Clinical Outcomes
Post-operative Pain Intensity at Rest
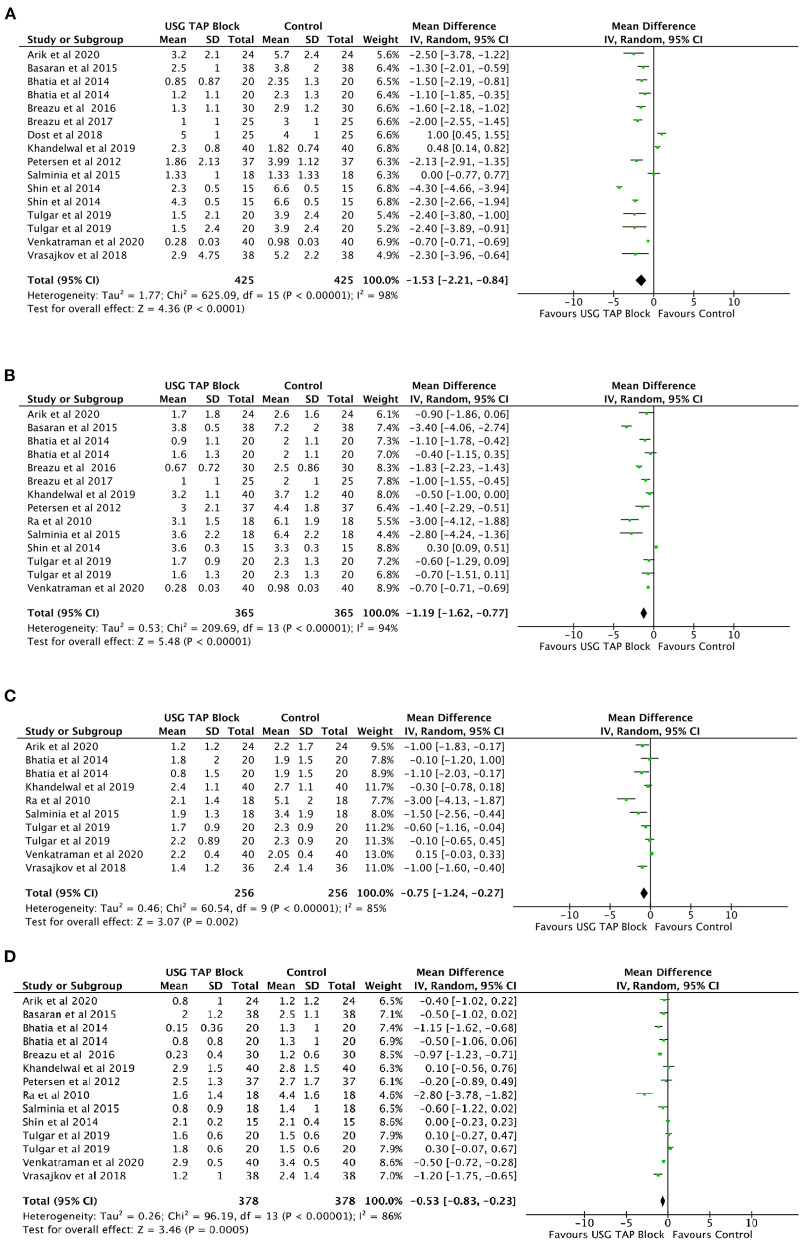
Analysis of the included studies suggested significantly reduced pain intensity in patients receiving USG-guided TAP block relative to control group patients at 0, 6, 12, and 24 h post-operation (Figures 2A–D). However, no such reduction was noted when USG-guided TAP block patients were compared to Port site infiltration group patients (Table 3). A high degree of heterogeneity was present in all included studies at all timepoints (0 h: I2 = 98%, p < 0.0001; 6 h: I2 = 94%, p < 0.0001; 12 h: I2 = 85%, p < 0.0001; 24 h: I2 = 87%, p < 0.0001).
Figure 2.
(A–D) Forest plot representing for Pain Intensity at Rest for USG guided TAP block vs. control group at (A) 0 h; (B) 6 h; (C) 12 h and (D) 24 h timepoints after operation.
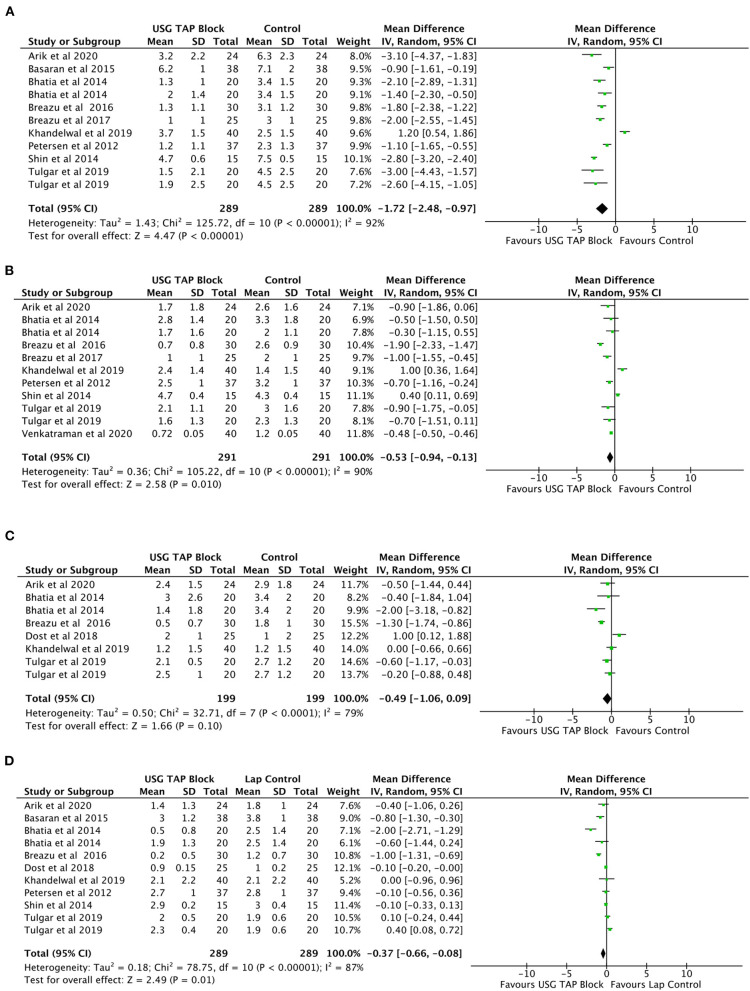
Post-operative Pain Intensity While Coughing
A significant reduction in pain intensity while coughing was observed at 0, 6, and 24 h post-operation in USG-guided TAP block patients relative to control group patients (Figures 3A–D). No significant change in pain intensity was noted at 12 h post-operation. No significant changes were noted when comparing USG-guided TAP block patients to Port site infiltration group patients at all post-operative time-point (Table 3).
Figure 3.
(A–D) Forest plot representing for Pain Intensity after operation during coughing for USG TAP block vs. control group (A) 0 h; (B) 6 h; (C) 12 h and (D) 24 h.
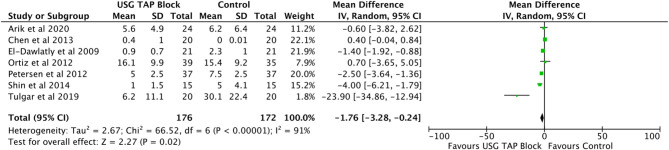
Morphine Consumption During 24 h After Operation
Analysis of seven studies (16, 17, 23, 27–29, 31) involving 348 LC subjects showed a significant reduction in morphine consumption during the first 24 h after surgery (MD = −1.76 mg, 95% CI: −3.28 to −0.24) in patients receiving TAP blocks compared to control subjects (Figure 4). A high degree of heterogeneity was observed (I2 = 91%, p < 0.0001).
Figure 4.
Forest plot representing for morphine consumption in the recovery room USG guided TAP block vs. control group.
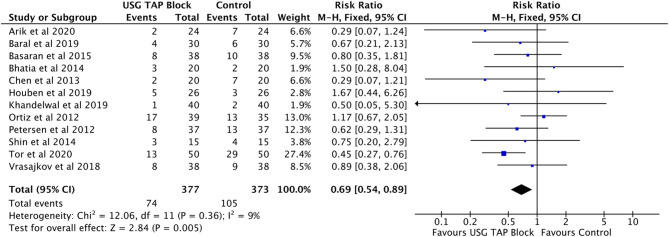
Post-operative Nausea and Vomiting (PONV) Incidence
Analysis of 12 studies (16, 18, 19, 21, 23, 25, 28, 29, 31, 33, 36, 37) involving 750 LC subjects showed a decreased incidence of PONV in patients receiving USG guided TAP blocks compared to control subjects (RR = 0.69, 95% CI: 0.54–0.89) (Figure 5). No significant heterogeneity between the studies was observed (I2 = 9%, p = 0.36).
Figure 5.
Forest plot representing for adverse events (PONV) in USG guided TAP block vs. control group.
Publication Bias
No significant publication bias was detected using Funnel plots or Egger's tests for (a) Post-Operative Pain Intensity at Rest for all timepoints (0 h: p = 0.54; 6 h: p = 0.32; 12 h: p = 0.98; 24 h: p = 0.63); (b) Post-Operative Pain Intensity during coughing for all timepoints (0 h: p = 0.12; 6 h: p = 0.76; 12 h; p = 0.91, 24 h: p = 0.17), (c) Morphine consumption during 24 h after operation (p = 0.36), (d) Post-operative nausea and vomiting (PONV) incidence (p = 0.71). All funnel plots showed symmetric shape for all the comparison.
Discussion
This study evaluated the efficacy of USG guided TAP block for reducing pain intensity at rest and while coughing in LC patients for up to 24 h post-operation. We noted a significant reduction in pain intensity in patients who received USG-guided TAP block relative to control group patients, as well as reduced morphine consumption and incidence of PONV. However, no such reduction was noted when USG-guided TAP block patients were compared to Port site infiltration group patients at rest and during coughing at all post-operative timepoints upto 24 h.
Severe pain for LC patients generally occurs during the first 24 h post-surgery, and is thought to arise mainly from visceral tissue damage and the surgical incision (with the latter taking precedent) (41). As such, analgesic planning must focus on incisional pain rather than visceral pain. The absence of significant difference of pain control after port site infiltration advocates too for an incisional pain control. Our results showed that USG-guided TAP block led to significantly reduced post-operative pain, as well as reduced morphine consumption and PONV incidence. These findings concur with a previous analysis of seven studies by Peng et al. (11). Recent RCTs have suggested that USG-guided TAP block plays an important role in multimodal pain therapy through proper visualization and improved accuracy. However, few studies have compared the effects of subcoastal TAP block with those of posterior TAP block. As such, our meta-analysis included RCTs that looked at both USG-guided TAP blocks and oblique subcostal TAP blocks. Nonetheless, we noted high heterogeneity between studies, suggesting that our meta-analysis results need to be treated with caution.
Our study has several limitations: (1) included studies had relatively small sample sizes; (2) extended follow-up data on chronic pain, long-term analgesic use, and adverse events was lacking; (3) multiple pain score scales were used; (4) a diverse range of anesthesia dosages were administered across the studies, and (5) insufficient study numbers for important factors such as laproscopic guided TAP block and fentanyl, tramadol, and opioid consumption, thereby precluding subgroup analysis.
Conclusion
This meta-analysis concludes that TAP block is more effective than a conventional pain control, but not significatively different from another local incisional pain control that is port site infiltration. Additional prospective randomized controlled trials are required to further validate our findings.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
WW conceived and designed the study. WW and LW did literature search and analyzed the data. YG wrote the paper, reviewed, and edited the manuscript. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Keus F, de Jong JaF, Gooszen HG, van Laarhoven CJHM. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst. Rev. (2006) 2006:CD006231. 10.1002/14651858.CD006231 [DOI] [PubMed] [Google Scholar]
- 2.Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. (2011) 98:1695–702. 10.1002/bjs.7689 [DOI] [PubMed] [Google Scholar]
- 3.Barczyński M, Herman RM. A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc. (2003) 17:533–8. 10.1007/s00464-002-9121-2 [DOI] [PubMed] [Google Scholar]
- 4.Bisgaard T. Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology. (2006) 104:835–46. 10.1097/00000542-200604000-00030 [DOI] [PubMed] [Google Scholar]
- 5.Rozen WM, Tran TMN, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat N Y N. (2008) 21:325–33. 10.1002/ca.20621 [DOI] [PubMed] [Google Scholar]
- 6.Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst. Rev. (2010) 2010:CD007705. 10.1002/14651858.CD007705.pub2 [DOI] [PubMed] [Google Scholar]
- 7.Siddiqui MRS, Sajid MS, Uncles DR, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth. (2011) 23:7–14. 10.1016/j.jclinane.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 8.Johns N, O'Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis Off J Assoc Coloproctology G B Irel. (2012) 14:e635–42. 10.1111/j.1463-1318.2012.03104.x [DOI] [PubMed] [Google Scholar]
- 9.Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. (2013) 166:1–9. 10.1016/j.ejogrb.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 10.De Oliveira GS, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. (2014) 118:454–63. 10.1213/ANE.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 11.Peng K, Ji F, Liu H, Wu S. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract Int J Kuwait Univ Health Sci Cent. (2016) 25:237–46. 10.1159/000444688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord. (2001) 12:232–6. 10.1159/000051263 [DOI] [PubMed] [Google Scholar]
- 14.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- 15.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arik E, Akkaya T, Ozciftci S, Alptekin A, Balas S. Unilateral transversus abdominis plane block and port-site infiltration : comparison of postoperative analgesic efficacy in laparoscopic cholecystectomy. Anaesthesist. (2020) 69:270–6. 10.1007/s00101-020-00746-1 [DOI] [PubMed] [Google Scholar]
- 17.Tulgar S, Kapakli MS, Kose HC, Senturk O, Selvi O, Serifsoy TE, et al. Evaluation of ultrasound-guided erector spinae plane block and oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: randomized, controlled, prospective study. Anesth Essays Res. (2019) 13:50–6. 10.4103/aer.AER_194_18 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Houben AM, Moreau A-SJ, Detry OM, Kaba A, Joris JL. Bilateral subcostal transversus abdominis plane block does not improve the postoperative analgesia provided by multimodal analgesia after laparoscopic cholecystectomy: a randomised placebo-controlled trial. Eur J Anaesthesiol. (2019) 36:772–7. 10.1097/EJA.0000000000001028 [DOI] [PubMed] [Google Scholar]
- 19.Baral B, Poudel PR. Comparison of analgesic efficacy of ultrasound guided subcostal transversus abdominis plane block with port site infiltration following laparoscopic cholecystectomy. J Nepal Health Res Counc. (2019) 16:457–61. 10.33314/jnhrc.v16i41.1486 [DOI] [PubMed] [Google Scholar]
- 20.Bava EP, Ramachandran R, Rewari V, Chandralekha Bansal VK, Trikha A. Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: a randomized controlled trial. Anesth Essays Res. (2016) 10:561–7. 10.4103/0259-1162.186620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khandelwal H, Parag K, Singh A, Anand N, Govil N. Comparison of subcostal transversus abdominis block with intraperitoneal instillation of levobupivacaine for pain relief after laparoscopic cholecystectomy: a prospective study. Anesth Essays Res. (2019) 13:144–8. 10.4103/aer.AER_3_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suseela I, Anandan K, Aravind A, Kaniyil S. Comparison of ultrasound-guided bilateral subcostal transversus abdominis plane block and port-site infiltration with bupivacaine in laparoscopic cholecystectomy. Indian J Anaesth. (2018) 62:497–501. 10.4103/ija.IJA_55_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. (2012) 37:188–92. 10.1097/AAP.0b013e318244851b [DOI] [PubMed] [Google Scholar]
- 24.Saliminia A, Azimaraghi O, Babayipour S, Ardavan K, Movafegh A. Efficacy of transverse abdominis plane block in reduction of postoperation pain in laparoscopic cholecystectomy. Acta Anaesthesiol Taiwanica Off J Taiwan Soc Anesthesiol. (2015) 53:119–22. 10.1016/j.aat.2015.07.003 [DOI] [PubMed] [Google Scholar]
- 25.Basaran B, Basaran A, Kozanhan B, Kasdogan E, Eryilmaz MA, Ozmen S. Analgesia and respiratory function after laparoscopic cholecystectomy in patients receiving ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: a randomized double-blind study. Med Sci Monit Int Med J Exp Clin Res. (2015) 21:1304–12. 10.12659/MSM.893593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. (2010) 58:362–8. 10.4097/kjae.2010.58.4.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Dawlatly AA, Turkistani A, Kettner SC, Machata A-M, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. (2009) 102:763–7. 10.1093/bja/aep067 [DOI] [PubMed] [Google Scholar]
- 28.Chen CK, Tan PCS, Phui VE, Teo SC. A comparison of analgesic efficacy between oblique subcostal transversus abdominis plane block and intravenous morphine for laparascopic cholecystectomy. A prospective randomized controlled trial. Korean J Anesthesiol. (2013) 64:511–6. 10.4097/kjae.2013.64.6.511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shin H-J, Oh A-Y, Baik J-S, Kim J-H, Han S-H, Hwang J-W. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: a randomized, controlled, observer-blinded study. Minerva Anestesiol. (2014) 80:185–93. [PubMed] [Google Scholar]
- 30.Dost B, Yalçin Sezen G, Iskender A, Özlü O. A comparison of transversus abdominis plane block guided with ultrasonography and local anesthetic infiltration in laparoscopic cholecystectomy operations. Agri Agri Algoloji Derneginin Yayin Organidir J Turk Soc Algol. (2018) 30:51–7. 10.5505/agri.2018.45822 [DOI] [PubMed] [Google Scholar]
- 31.Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. (2012) 115:527–33. 10.1213/ANE.0b013e318261f16e [DOI] [PubMed] [Google Scholar]
- 32.Venkatraman R, Saravanan R, Dhas M, Pushparani A. Comparison of laparoscopy-guided with ultrasound-guided subcostal transversus abdominis plane block in laparoscopic cholecystectomy - a prospective, randomised study. Indian J Anaesth. (2020) 64:1012–7. 10.4103/ija.IJA_528_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhatia N, Arora S, Jyotsna W, Kaur G. Comparison of posterior and subcostal approaches to ultrasound-guided transverse abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. J Clin Anesth. (2014) 26:294–9. 10.1016/j.jclinane.2013.11.023 [DOI] [PubMed] [Google Scholar]
- 34.Breazu CM, Ciobanu L, Bartos A, Bodea R, Mircea PA, Ionescu D. Pethidine efficacy in achieving the ultrasound-guided oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: a prospective study. Bosn J Basic Med Sci. (2017) 17:67–73. 10.17305/bjbms.2016.1647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breazu CM, Ciobanu L, Hadade A, Bartos A, Mitre C, Mircea PA, et al. The efficacy of oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy - a prospective, placebo controlled study. Romanian J Anaesth Intensive Care. (2016) 23:12–8. 10.21454/rjaic.7518.231.obq [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vrsajkov V, Mančić N, Mihajlović D, Milićević ST, Uvelin A, Vrsajkov JP. O bloqueio do plano transverso abdominal subcostal pode melhorar a analgesia após colecistectomia laparoscópica. Braz J Anesthesiol. (2018) 68:149–53. 10.1016/j.bjan.2017.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tor IH, Çelik EC, Aydin ME. Analgesic effect of combined transversus abdominis plane block and rectus sheath block in laparoscopic cholecystectomy: prospective randomized study. Ain-Shams J Anesthesiol. (2020) 12:58. 10.1186/s42077-020-00108-4 [DOI] [Google Scholar]
- 38.Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol. (2012) 28:339–43. 10.4103/0970-9185.98331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vindal A, Sarda H, Lal P. Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: results of a triple blind randomized controlled trial. Surg Endosc. (2021) 35:1713–21. 10.1007/s00464-020-07558-9 [DOI] [PubMed] [Google Scholar]
- 40.Baytar Ç, YIlmaz C, Karasu D, Topal S. Comparison of ultrasound-guided subcostal transversus abdominis plane block and quadratus lumborum block in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical study. Pain Res Manage. (2019) 2019:2815301. 10.1155/2019/2815301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. (2001) 90:261–9. 10.1016/S0304-3959(00)00406-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.