Key Points
Question
Do individuals from racial and ethnic minority groups receive lower rates of ambulatory care access and quality than individuals of other races and ethnicities in Medicare Advantage and/or traditional Medicare, and how do the 2 programs compare on these measures for minority beneficiaries?
Findings
In this exploratory study of a nationally representative sample of 26 887 Medicare beneficiaries in 2015-2018, enrollment in Medicare Advantage compared with traditional Medicare was significantly associated with better outcomes on 1 of 3 access measures and 3 of 3 quality measures for minority beneficiaries; however, minority beneficiaries were also significantly more likely to experience worse outcomes for most access and quality metrics compared with other beneficiaries within both programs.
Meaning
Medicare Advantage, compared with traditional Medicare, was significantly associated with better outcomes for ambulatory care access and quality among minority beneficiaries, but minority beneficiaries nonetheless experienced worse outcomes for most of these measures compared with other beneficiaries within both Medicare programs.
Abstract
Importance
There are racial inequities in health care access and quality in the United States. It is unknown whether such differences for racial and ethnic minority beneficiaries differ between Medicare Advantage and traditional Medicare or whether access and quality are better for minority beneficiaries in 1 of the 2 programs.
Objective
To compare differences in rates of enrollment, ambulatory care access, and ambulatory care quality by race and ethnicity in Medicare Advantage vs traditional Medicare.
Design, Setting, and Participants
Exploratory observational cohort study of a nationally representative sample of 45 833 person-years (26 887 persons) in the Medicare Current Beneficiary Survey from 2015 to 2018, comparing differences in program enrollment and measures of access and quality by race and ethnicity.
Exposures
Minority race and ethnicity (Black, Hispanic, Native American, or Asian/Pacific Islander) vs White or multiracial; Medicare Advantage vs traditional Medicare enrollment.
Main Outcomes and Measures
Six patient-reported measures of ambulatory care access (whether a beneficiary had a usual source of care in the past year, had a primary care clinician usual source of care, or had a specialist visit) and quality (influenza vaccination, pneumonia vaccination, and colon cancer screening).
Results
The final sample included 6023 persons (mean age, 68.9 [SD, 12.6] years; 57.3% women) from minority groups and 20 864 persons (mean age, 71.9 [SD, 10.8] years; 54.9% women) from White or multiracial groups, who accounted for 9816 and 36 017 person-years, respectively. Comparing Medicare Advantage vs traditional Medicare among minority beneficiaries, those in Medicare Advantage had significantly better rates of access to a primary care clinician usual source of care (79.1% vs 72.5%; adjusted marginal difference, 4.0%; 95% CI, 1.0%-6.9%), influenza vaccinations (67.3% vs 63.0%; adjusted marginal difference, 5.2%; 95% CI, 1.9%-8.5%), pneumonia vaccinations (70.7% vs 64.6%; adjusted marginal difference, 6.1%; 95% CI, 2.7%-9.4%), and colon cancer screenings (69.4% vs 61.1%; adjusted marginal difference, 7.1%; 95% CI, 3.8%-10.3%). Comparing minority vs White or multiracial beneficiaries across both programs, minority beneficiaries had significantly lower rates of access to a primary care clinician usual source of care (adjusted marginal difference, 4.7%; 95% CI, 2.5%-6.8%), specialist visits (adjusted marginal difference, 10.8%; 95% CI, 8.3%-13.3%), influenza vaccinations (adjusted marginal difference, 4.3%; 95% CI, 1.2%-7.4%), and pneumonia vaccinations (adjusted marginal difference, 6.4%; 95% CI, 3.9%-9.0%). The interaction of race and ethnicity with insurance type was not statistically significant for any of the 6 outcome measures.
Conclusions and Relevance
In this exploratory study of Medicare beneficiaries in 2015-2018, enrollment in Medicare Advantage vs traditional Medicare was significantly associated with better outcomes for access and quality among minority beneficiaries; however, minority beneficiaries were significantly more likely to experience worse outcomes for most access and quality measures than White or multiracial beneficiaries in both programs.
This observational study uses data from the Medicare Current Beneficiary Survey from 2015 to 2018 to compare differences in rates of enrollment, ambulatory care access, and ambulatory care quality for minority beneficiaries vs White or multiracial beneficiaries in Medicare Advantage vs traditional Medicare plans.
Introduction
Due to structural racism, health inequities are disproportionally concentrated within racial and ethnic minority communities in the United States.1 A key way these inequities operate is via reduced access to high-quality ambulatory care.2,3 Individuals who lack such care are more likely to experience preventable complications of their conditions, leading to higher rates of hospitalization and death.4,5 Providing access to high-quality ambulatory care for Medicare beneficiaries is therefore an important strategy to improve outcomes, reduce inequities, and prevent expensive complications of disease.6,7
Medicare beneficiaries receive their benefits from the traditional Medicare program administered by the Centers for Medicare & Medicaid Services (CMS) or from private health insurance plans in the Medicare Advantage program. Racial and ethnic minority beneficiaries experience lower rates of access and quality and worse outcomes in both programs.8,9 Racial and ethnic minority beneficiaries are less likely to receive annual wellness visits,10 preventive care,8,9 and specialty care11 and appear to be segregated within a smaller set of low-quality clinicians.8,9 They experience higher rates of hospitalization and mortality, as well as higher costs of care.8,12,13
It is unknown whether there are differences in care quality or access for racial and ethnic minority beneficiaries between the Medicare Advantage and traditional Medicare programs. If there are differences in ambulatory care access and quality, that may have implications for Medicare Advantage vs traditional Medicare enrollment decisions, as well as equity implications for Medicare. However, it is unknown how differences in ambulatory care access and quality by race and ethnicity compare in Medicare Advantage vs traditional Medicare.
This study therefore focused on 4 questions: (1) Does enrollment in Medicare Advantage vary by race and ethnicity? (2) How do ambulatory care access and quality for racial and ethnic minority beneficiaries vs other beneficiaries compare in both programs? (3) How do differences in access and quality by race and ethnicity compare in Medicare Advantage vs traditional Medicare? and (4) Are ambulatory care access and quality better for racial and ethnic minority beneficiaries enrolled in Medicare Advantage or traditional Medicare?
Methods
This study was deemed exempt by the Saint Louis University Institutional Review Board and informed consent was waived.
Data and Study Population
An exploratory observational cohort study was conducted using a national sample of Medicare Advantage and traditional Medicare beneficiaries in the Medicare Current Beneficiary Survey (MCBS) linked to Medicare administrative data for the years 2015-2018. The MCBS is an annual, nationally representative survey of the Medicare population with a rotating cohort design.14 The most recently reported response rate for the MCBS in 2018 was 65.4%.15 The sample was limited to community-dwelling beneficiaries with at least 12 months of exclusive Part A and Part B enrollment in Medicare Advantage or traditional Medicare, completion of the annual MCBS, and residence in a US zip code and Dartmouth Atlas of Health Care hospital referral region (HRR). Beneficiaries meeting the above study inclusion criteria but missing data on race and ethnicity or other key study variables were excluded. The unit of analysis was the person-year, with some persons appearing in multiple years of the data. The MCBS survey weights were used to compute nationally representative estimates. These weights account for the overall selection probability of each person sampled and include adjustments for stratified sampling design and survey nonresponse.14
Exposures: Medicare Advantage vs Traditional Medicare Enrollment and Race and Ethnicity
Medicare Advantage vs traditional Medicare insurance enrollment was identified using beneficiaries’ annual Medicare enrollment data taken from their administrative records. Beneficiaries self-reported their own race and ethnicity in the MCBS. This is the gold standard for race and ethnicity classification and is more accurate than Medicare administrative records.16 The National Institute on Minority Health and Health Disparities racial and ethnic framework was used to identify beneficiaries as minority beneficiaries if they self-reported a race or ethnicity of Black, Hispanic, Native American, or Asian/Pacific Islander.17 Beneficiaries who self-reported they were White or multiracial and not Hispanic were identified as the comparator group.
Beneficiary Characteristics
Enrollment and demographic, social risk, health status, and local area characteristics were assessed on beneficiaries in the study.
Current Medicare entitlement status (age, disability, or end-stage kidney disease), dual enrollment in Medicaid, age, and sex were measured using Medicare enrollment records.
Social risk factors were measured using patient-reported measures of material capital (annual income), human capital (highest level of education attained), and social support (living alone).
Health status was measured using patient-reported data on self-rated health, functional impairment, and presence of chronic conditions. Poor self-rated health was identified for those who rated their health in the past year as “fair” or “poor.” Functional impairment was measured as counts (ranging from 0 to 6) of self-reported difficulty with activities of daily living and instrumental activities of daily living. In addition, 5 of the most common chronic conditions in Medicare populations—diabetes, heart failure, ischemic heart disease, asthma/chronic obstructive pulmonary disease, and depression—were identified if beneficiaries self-reported “ever” having those conditions.
Local area variables were assessed by using beneficiaries’ counties of residence to identify the local Medicare Advantage market penetration (ie, uptake) rate using CMS data.18 Beneficiaries’ residential zip codes were used to identify the HRRs19 in which they resided and to classify their residence as rural (nonmetropolitan) vs urban (metropolitan) using Rural-Urban Commuting Area codes.20
Ambulatory Care Access and Quality Outcomes
The outcomes were 6 patient-reported measures of ambulatory care access and quality. Some questions were asked in the following year in reference to the prior year, and respondents who dropped out of the MCBS at the end of the prior year were excluded.
The outcomes were binary indicators of whether a beneficiary had a usual source of care in the past year, had a primary care clinician usual source of care, had a specialist visit, received an annual influenza vaccination, received a pneumonia vaccination, or had been screened for colon cancer. The colon cancer screening measure was assessed for beneficiaries aged 45 years or older who self-reported not having colon cancer and the outcome was considered met if beneficiaries reported having received within the past 5 years either (1) a colonoscopy or sigmoidoscopy in a physician’s office or (2) a fecal occult blood test at home or in a physician’s office. Each of these preventive measures has an evidence base supporting their use as measures of quality of care.21
Statistical Analysis
Descriptive statistics were computed for minority beneficiaries’ and White or multiracial beneficiaries’ characteristics, including rates of enrollment in Medicare Advantage and traditional Medicare, and the Wald test was used to compare differences in proportions (or means) by beneficiaries’ race and ethnicity.
Unadjusted rates of the 6 outcomes were calculated among 4 groups: (1) minority beneficiaries enrolled in Medicare Advantage; (2) minority beneficiaries enrolled in traditional Medicare; (3) White or multiracial beneficiaries enrolled in Medicare Advantage; and (4) White or multiracial beneficiaries enrolled in traditional Medicare. Absolute differences with 95% CIs were also calculated for these rates by Medicare Advantage vs traditional Medicare program type and by minority race and ethnicity vs White or multiracial.
Multivariable logistic regression models were estimated at the person-year level to assess the association between the exposure variables of Medicare Advantage (vs traditional Medicare) enrollment, minority race and ethnicity (vs White or multiracial), and the interaction between Medicare Advantage enrollment and minority race and ethnicity, and the 6 outcome variables among all beneficiaries. A significant coefficient on the interaction indicates a difference in racial and ethnic differences between the programs. Models were adjusted for the characteristics listed above as well as county-level Medicare Advantage market penetration rates and fixed effects for HRRs. The Medicare Advantage market penetration rates and HRR fixed effects controlled for the local area spillover effect of Medicare Advantage onto traditional Medicare and for market differences that may influence local Medicare Advantage plan offerings. Results are reported as marginal differences, which can be interpreted as percentage-point differences in the outcomes associated with the exposure variables. All models included year fixed effects to control for secular trend and adjusted for the complex survey design of the MCBS, and clustered standard errors on beneficiaries to adjust for intraperson correlation over time.
Stratified multivariable logistic regression models were estimated at the person-year level to assess the association between Medicare Advantage (vs traditional Medicare) enrollment and the 6 outcomes among (1) minority beneficiaries and (2) White or multiracial beneficiaries, using the process described above.
In secondary analyses, descriptive statistics were assessed on the exposure, outcome, and other variables by individual minority racial and ethnic group (Black, Hispanic, Native American, Asian/Pacific Islander) and White or multiracial beneficiaries. The multivariable regression models above were reestimated among the subgroup of Black and White beneficiaries to assess associations with the outcomes among the 2 largest racial and ethnic groups in Medicare.
Descriptive statistics were computed on the characteristics of beneficiaries excluded from the study sample due to a lack of 12 months of enrollment and/or missing data on key study variables, and the Wald test was used to compare differences in proportions (or means) between the excluded and sample beneficiaries.
The threshold for statistical significance was P < .05 with 2-sided tests. Analyses were performed using SAS version 9.4 and Stata version 16. Because of the potential for type I error due to multiple comparisons, findings for the analyses should be interpreted as exploratory.
Results
Study Population Characteristics
Of 52 587 person-years contributed by individuals living in the community with some Medicare Part A and Part B enrollment, 47 861 had exclusive annual enrollment in Medicare Advantage or traditional Medicare with residence in a US zip code and HRR (eFigure 1 in the Supplement). After excluding 3.4% of the sample missing data on race and ethnicity and key study variables, the final sample consisted of 45 833 person-years (26 887 unique persons). The final sample included 6023 persons (mean age, 68.9 [SD, 12.6] years; 57.3% women) from minority groups and 20 864 persons (mean age, 71.9 [SD, 10.8] years; 54.9% women) from White or multiracial groups, who accounted for 9816 and 36 017 person-years, respectively. Beneficiaries not included in the study had less enrollment and were more likely to die during the year (eTable 1 in the Supplement).
Minority beneficiaries were significantly more likely to enroll in Medicare Advantage than White or multiracial beneficiaries (53.0% vs 39.8%; absolute difference, 13.2%; 95% CI, 10.0%-16.4%; P < .001) (Table 1). Minority beneficiaries were younger (mean age, 68.9 vs 71.9 years; absolute difference, 2.9 years; 95% CI, 2.5-3.4 years; P < .001), more likely to be female (57.3% vs 54.9%; absolute difference, 2.4%; 95% CI, 0.4%-4.4%; P = .02), more likely to be disabled (21.5% vs 12.5%; absolute difference, 9.1%; 95% CI, 7.3%-10.8%; P < .001), more likely to be enrolled in Medicaid (39.2% vs 12.2%; absolute difference, 27.0%; 95% CI, 24.6%-29.4%; P < .001), and more likely to have poor self-rated health (34.2% vs 19.9%; absolute difference, 14.3%; 95% CI, 12.5%-16.1%; P < .001). Black beneficiaries had the most representation among minority beneficiaries, and White beneficiaries had the most representation among White and multiracial beneficiaries (eTable 2 in the Supplement).
Table 1. Characteristics of Medicare Beneficiaries by Race and Ethnicity, 2015-2018.
| Characteristics | Beneficiary race and ethnicity | Absolute difference (95% CI) | P valueb | |
|---|---|---|---|---|
| Minoritya | White or multiracial | |||
| Total No. of patient-years | ||||
| Unweighted | 9816 | 36 017 | ||
| Weightedc | 36 999 201 | 140 187 965 | ||
| Age, mean (SD), y | 68.9 (12.6) | 71.9 (10.8) | –2.9 (–3.4 to –2.5) | <.001 |
| Sex, % | ||||
| Male | 42.7 | 45.1 | –2.4 (–4.4 to –0.4) | .02 |
| Female | 57.3 | 54.9 | 2.4 (0.4 to 4.4) | |
| Annual income, mean (SD), $ | 32 755 (47 014) | 57 952 (95 387) | –25 197 (–27 873 to –22 521) | <.001 |
| Education, % | ||||
| No high school or college | 36.0 | 11.5 | 24.6 (21.9 to 27.2) | <.001 |
| High school/some college | 49.5 | 59.9 | –10.5 (–12.9 to –8.0) | <.001 |
| College/graduate school | 14.5 | 28.6 | –14.1 (–16.4 to –11.8) | <.001 |
| Living alone, % | 27.9 | 30.1 | –2.1 (–4.1 to –0.1) | .04 |
| Locality of residence, % | ||||
| Rural | 12.8 | 23.4 | –10.6 (–14.6 to –6.5) | <.001 |
| Urban | 87.2 | 76.6 | 10.6 (6.5 to 14.6) | |
| Medicare Advantage market penetration rate, %d | 35.6 | 32.4 | 3.2 (1.5 to 4.9) | <.001 |
| Medicare program, % | ||||
| Medicare Advantagee | 53.0 | 39.8 | 13.2 (10.0 to 16.4) | <.001 |
| Traditional Medicaref | 47.0 | 60.2 | –13.2 (–16.4 to –10.0) | <.001 |
| Current Medicare entitlement status, % | ||||
| Age | 78.3 | 87.5 | –9.2 (–11.0 to –7.4) | <.001 |
| Disability | 21.5 | 12.5 | 9.1 (7.3 to 10.8) | <.001 |
| End-stage kidney disease | 2.1 | 0.4 | 1.6 (1.1 to 2.1) | <.001 |
| Medicaid dual enrollment, % | 39.2 | 12.2 | 27.0 (24.6 to 29.4) | <.001 |
| Poor self-rated health | 34.2 | 19.9 | 14.3 (12.5 to 16.1) | <.001 |
| Difficulty with ADLs, mean (SD)g | 0.89 (1.55) | 0.63 (1.27) | 0.26 (0.21 to 0.32) | <.001 |
| Difficulty with IADLs, mean (SD)g | 1.12 (1.67) | 0.75 (1.37) | 0.36 (0.30 to 0.42) | <.001 |
| Diabetes, % | 44.2 | 30.0 | 14.2 (12.2 to 16.1) | <.001 |
| Depression, % | 27.5 | 26.5 | 1.0 (–0.8 to 2.8) | .26 |
| Chronic obstructive pulmonary disease/asthma, % | 18.4 | 21.1 | –2.7 (–4.3 to –1.1) | .001 |
| Ischemic heart disease, % | 14.8 | 16.4 | –1.7 (–3.0 to –0.3) | .02 |
| Heart failure, % | 8.3 | 7.0 | 1.3 (0.0 to 2.6) | .04 |
Abbreviations: ADLs, activities of daily living; IADLs, instrumental ADLs.
Minority beneficiaries are individuals with a self-reported race and ethnicity of Black, Hispanic, Native American, or Asian/Pacific Islander.
P value on the Wald test of significance for difference in means or percentages by minority race and ethnicity vs White or multiracial, equivalent to the F statistic for continuous variables and the χ2 statistic for categorical variables.
Weighted estimates from the 2015-2018 Medicare Current Beneficiary Survey (MCBS) using cross-sectional weights accounting for the overall annual selection probability of each person sampled and including adjustments for the stratified sampling design, survey nonresponse, and coverage error.
Percentage of total beneficiaries enrolled in both Medicare Part A and Part B in the county who opted into Medicare Advantage plans.
Medicare Advantage beneficiaries living in a community in a US zip code and Dartmouth Atlas hospital referral region with at least 1 calendar year of exclusive continuous enrollment in Medicare Advantage benefits and completing the annual survey round in the MCBS.
Medicare beneficiaries living in a community in a US zip code and Dartmouth Atlas hospital referral region with at least 1 calendar year of exclusive continuous enrollment in traditional Medicare benefits and completing the annual survey round in the MCBS.
Beneficiaries’ self-reported difficulty with activities of daily living (ADLs) and instrumental ADLs (IADLs). These counts ranged from 0 to 6 and were summed from 6 binary ADL and 6 binary IADL question responses that asked beneficiaries if they “could not do” or “had difficulty doing” daily living activities such as bathing and dressing or instrumental daily living activities such as shopping or paying bills. Higher counts indicate greater functional impairment on ADLs and IADLs.
Unadjusted Differences in Access and Quality by Race and Ethnicity and Program Type
In unadjusted results, minority beneficiaries had significantly better rates of access to a usual source of care (91.0% vs 88.1%; absolute difference, 3.0%; 95% CI, 0.9%-5.0%) and access to a primary care clinician usual source of care (79.1% vs 72.5%; absolute difference, 6.6%; 95% CI, 3.5%-9.8%), as well as better rates of influenza vaccinations (67.3% vs 63.0%; absolute difference, 4.3%; 95% CI, 0.8%-7.8%), pneumonia vaccinations (70.7% vs 64.6%; absolute difference, 6.0%; 95% CI, 2.7%-9.4%), and colon cancer screenings (69.4% vs 61.1%; absolute difference, 8.4%; 95% CI, 5.3%-11.5%) in Medicare Advantage vs traditional Medicare (Figure). However, minority beneficiaries had significantly worse rates of access on 3 of 3 measures and worse rates of quality on 2 of 3 measures than White or multiracial beneficiaries in both Medicare Advantage and traditional Medicare (P < .05). White or multiracial beneficiaries had significantly better rates of access on 2 of 3 measures and better rates of quality on 3 of 3 measures in Medicare Advantage vs traditional Medicare (P < .05 for all).
Figure. Unadjusted Rates and Absolute Differences for Ambulatory Care Access and Quality in Medicare Advantage and Traditional Medicare by Race and Ethnicity, Minority vs White or Multiracial, 2015-2018.
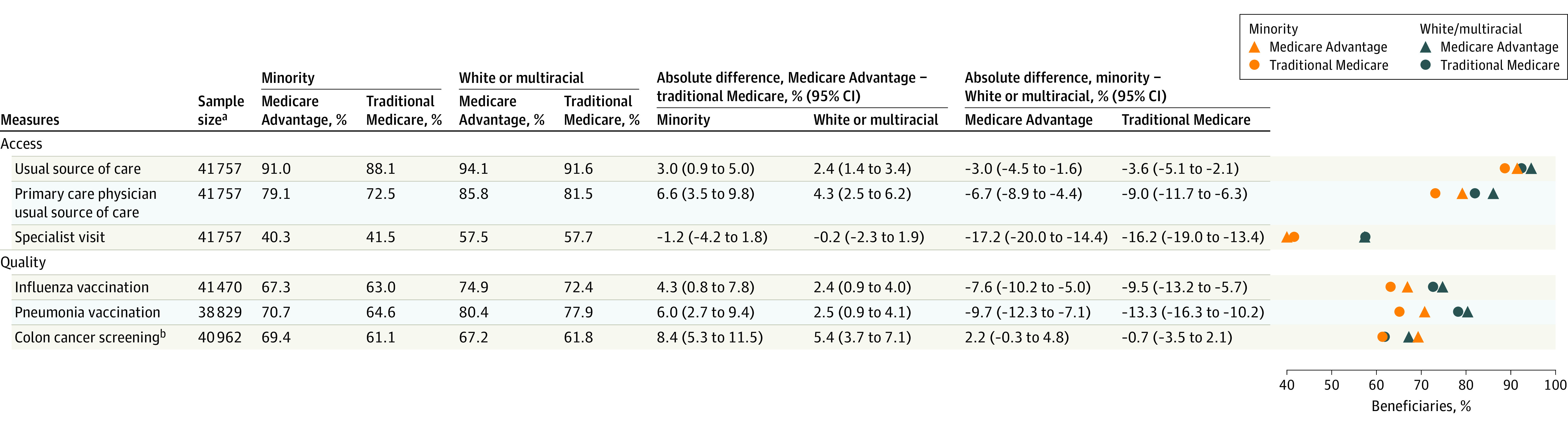
Minority Medicare Advantage beneficiaries were 11.1% of the total; minority traditional Medicare beneficiaries, 9.8%; White or multiracial Medicare Advantage beneficiaries, 31.5%; and White or multiracial traditional Medicare beneficiaries, 47.6%.
aUnweighted sample sizes of patients who met baseline study inclusion and exclusion criteria as listed in Table 1 and responded to Medicare Current Beneficiary Survey questions for outcome variables.
bFecal occult blood test at home or in physician’s office or colonoscopy or sigmoidoscopy within the past 5 years, excluding patients who self-reported having colon cancer or were younger than 45 years.
Adjusted Differences in Access and Quality by Program Type and Race and Ethnicity
In adjusted results, all beneficiaries in Medicare Advantage had significantly higher rates of access to a usual source of care (1.5%; 95% CI, 0.8%-2.2%) and a usual source of care that was a primary care clinician (3.0%; 95% CI, 1.8%-4.3%) compared with those in traditional Medicare (Table 2). In addition, beneficiaries in Medicare Advantage vs traditional Medicare had significantly higher rates of influenza vaccinations (2.2%; 95% CI, 0.9%-3.6%), pneumonia vaccinations (2.0%; 95% CI, 0.4%-3.6%), and colon cancer screenings (4.4%; 95% CI, 3.1%-5.8%). Comparing Medicare Advantage vs traditional Medicare among minority beneficiaries, those in Medicare Advantage had significantly better rates of access to a primary care clinician usual source of care (4.0%; 95% CI, 1.0%-6.9%), influenza vaccinations (5.2%; 95% CI, 1.9%-8.5%), pneumonia vaccinations (6.1%; 95% CI, 2.7%-9.4%), and colon cancer screenings (7.1%; 95% CI, 3.8%-10.3%).
Table 2. Adjusted Marginal Differences for Association of Medicare Program Type and Race and Ethnicity With Ambulatory Care Access and Quality, 2015-2018a.
| Measures | % (95% CI) | ||||
|---|---|---|---|---|---|
| Medicare Advantage vs traditional Medicare | Minority race and ethnicity vs White or multiracial among all Medicare beneficiaries | Interaction of Medicare Advantage and minority race and ethnicity | |||
| Among all beneficiaries | Among minority beneficiaries | Among White or multiracial beneficiaries | |||
| Access | |||||
| Usual source of care | 1.5 (0.8 to 2.2) | 1.0 (0.0 to 2.0) | 1.3 (0.7 to 1.9) | –1.0 (–2.1 to 0.1) | –0.1 (–1.6 to 1.4) |
| Primary care physician usual source of care | 3.0 (1.8 to 4.3) | 4.0 (1.0 to 6.9) | 1.3 (0.7 to 1.9) | –4.7 (–6.8 to –2.5) | 0.9 (–2.0 to 3.8) |
| Specialist visit | –0.5 (–2.3 to 1.3) | –1.7 (–5.0 to 1.5) | –0.6 (–2.4 to 1.2) | –10.8 (–13.3 to –8.3) | –1.8 (–5.5 to 1.9) |
| Quality | |||||
| Influenza vaccination | 2.2 (0.9 to 3.6) | 5.2 (1.9 to 8.5) | 2.1 (0.7 to 3.4) | –4.3 (–7.4 to –1.2) | 0.8 (–2.4 to 4.1) |
| Pneumonia vaccination | 2.0 (0.4 to 3.6) | 6.1 (2.7 to 9.4) | 1.7 (0.2 to 3.1) | –6.4 (–9.0 to –3.8) | 1.6 (–1.0 to 4.2) |
| Colon cancer screeningb | 4.4 (3.1 to 5.8) | 7.1 (3.8 to 10.3) | 4.7 (3.3 to 6.0) | 1.9 (–0.7 to 4.5) | 2.1 (–1.2 to 5.4) |
Multivariable logistic regression models were estimated for each outcome that also adjusted for the characteristics listed in Table 1. Fixed effects were added for the Dartmouth Atlas hospital referral regions that beneficiaries resided in to control for market-level differences in supply of medical services, clinician practice intensity, and coding intensity. Year fixed effects were included to control for secular trend and P values were adjusted for the complex survey design of the MCBS and intraperson correlation over time. The Stata Margins command was used to report marginal differences as the change in the mean probability of the outcome variable associated with Medicare Advantage vs traditional Medicare enrollment, minority race and ethnicity vs White or multiracial, and the interaction of Medicare Advantage enrollment with minority race and ethnicity. Also shown are the marginal differences of Medicare Advantage vs traditional Medicare enrollment in separate models that were stratified by race and ethnicity.
Fecal occult blood test at home or in physician’s office or colonoscopy or sigmoidoscopy within past 5 years, excluding patients who self-reported having colon cancer or were younger than 45 years. A linear probability model was estimated for colon cancer screening because the logistic regression model would not converge.
In adjusted results, comparing minority vs White or multiracial beneficiaries across both programs, minority beneficiaries had significantly lower rates of access to a primary care clinician usual source of care (4.7%; 95% CI, 2.5%-6.8%), specialist visits (10.8%; 95% CI, 8.3%-13.3%), influenza vaccinations (4.3%; 95% CI, 1.2%-7.4%), and pneumonia vaccinations (6.4%; 95% CI, 3.9%-9.0%). The interaction of race and ethnicity with insurance type was not statistically significant for any of the 6 outcome measures.
In secondary analyses, Hispanic (60.1%) and Black (51.1%) beneficiaries had the highest rates of enrollment in Medicare Advantage (eTable 2 in the Supplement). Adjusted results were similar for differences in access and quality for Black vs White beneficiaries by race and ethnicity and Medicare Advantage vs traditional Medicare enrollment as in the main analysis for minority vs White or multiracial beneficiaries (eTables 3-5 in the Supplement).
Discussion
In this nationally representative exploratory study of Medicare beneficiaries, minority beneficiaries were significantly more likely to enroll in Medicare Advantage than White or multiracial beneficiaries and received significantly better access to and quality of care in Medicare Advantage than in traditional Medicare. However, compared with White or multiracial beneficiaries, minority beneficiaries experienced lower rates of ambulatory care access and quality on most measures in both programs.
These results confirm actuarial reports that minority beneficiaries enrolled in Medicare Advantage at substantially higher rates than White or multiracial beneficiaries in recent years,22 although the reasons are unclear. The finding that Medicare Advantage market penetration rates were higher in counties where minority beneficiaries lived suggests that enrollment decisions were partly driven by local plan availability. However, enrollment decisions likely also reflected beneficiary preferences for specific plan features, including the (perhaps accurate) perception that Medicare Advantage provides better quality of care.
Studies from past decades, when Medicare Advantage enrollment was much lower, found better rates of influenza vaccination and cancer screening for minority beneficiaries in Medicare Advantage vs traditional Medicare.23,24 The present study findings indicate that as Medicare Advantage enrollment rates have grown substantially and as quality measures have been implemented in both Medicare Advantage and traditional Medicare over the past decade, these patterns persist. The mechanisms underlying such findings merit investigation. Medicare Advantage plans systematically track quality measures, such as influenza vaccinations and cancer screenings, because these affect their star ratings and reimbursement.25 Thus, Medicare Advantage plans may provide reminders for cancer screening to patients and clinicians or extra supports and services to enable that screening, such as transportation or scheduling assistance.26 Medicare Advantage plans may also selectively contract with clinicians that provide higher-quality care, whereas traditional Medicare is unable to exclude low-quality clinicians. More research is needed to confirm this. The finding that differences by race and ethnicity in access and quality were not significantly different between Medicare Advantage and traditional Medicare suggests that none of these mechanisms were enough to eliminate health inequities.
Differences in rates of access and quality by race and ethnicity were statistically significant in both the Medicare Advantage and traditional Medicare programs. Although prior research has found inequities in both programs,8,9,23,27,28 the present study extends these findings to a more recent time period and further found that lower rates of access and quality for minority beneficiaries compared with White or multiracial beneficiaries were not significantly different in both programs. Minority beneficiaries had significantly lower access and quality on the majority of measures, even after adjusting for health status and chronic conditions. Given prior research suggesting that beneficiaries with chronic conditions who lacked annual specialist visits were much more likely to experience preventable hospitalizations and deaths,4,5 it is possible that these differences in access contribute to worse outcomes observed for racial and ethnic minority populations with chronic diseases such as diabetes, cardiovascular disease, and stroke. This study did not examine whether differences in access and quality were directly tied to outcomes, such as contracting influenza. This is an important area for future study.
Direct measurement and incentivization of equity may be required to meaningfully close gaps in access and quality between minority and nonminority patients in both programs. CMS could develop and implement equity measures for Medicare Advantage (via the Star Ratings system) and traditional Medicare (via the Quality Payment Program) to incentivize plans and clinicians to develop effective strategies to improve access and quality for minority patients.29 Medicare Advantage plans could also begin tracking such measures on their own in order to improve the quality of their plans for the growing market of Medicare beneficiaries who are racial and ethnic minority beneficiaries. As a step toward this goal, the CMS Office of Minority Health has begun tracking quality measures in Medicare Advantage by race and ethnicity.30
Limitations
This study has several limitations. First, Hispanic and Asian/Pacific Islander beneficiaries in this study represent large and diverse groups by race and ethnicity. Due to data availability and sample size restrictions, these groups could not be further disaggregated, which may mask different patterns based on country of origin or other factors.
Second, diagnosis upcoding in the Medicare Advantage program can make Medicare Advantage beneficiaries appear sicker than they are31,32,33; the use of patient-reported health data in this study should have minimized this bias, but the populations still may have differed in unobservable ways.
Third, Medicare Advantage plans selectively enter local markets based on favorable conditions related to population health and health services supply,34 and Medicare Advantage has a restraining effect on health services use that may spill over to the traditional Medicare program in local areas.35 The use of HRR fixed effects to control for local market differences and adjustment for county-level Medicare Advantage penetration controlled for this, but it does not rule out confounding due to other unobserved factors, and therefore the observed estimates may not imply causal relationships.
Fourth, both Medicare Advantage and traditional Medicare are heterogeneous programs. Beneficiaries in Medicare Advantage may enroll in special-needs plans and beneficiaries in traditional Medicare may enroll in accountable care organizations or other care models. These results represent averages for the Medicare Advantage and traditional Medicare programs; more research is needed to identify components in each that may be better at meeting the needs of minority beneficiaries.
Conclusions
In this exploratory study of Medicare beneficiaries in 2015-2018, enrollment in Medicare Advantage vs traditional Medicare was significantly associated with better outcomes for access and quality among minority beneficiaries; however, minority beneficiaries were significantly more likely to experience worse outcomes for most access and quality measures than White or multiracial beneficiaries in both programs.
eFigure 1. Study Sample Selection Flowchart
eTable 1. Comparing Medicare Beneficiaries Included Versus Excluded From Study Sample, 2015-2018
eTable 2. Characteristics of Study Sample Beneficiaries by Race and Ethnicity, 2015-2018
eTable 3. Association of Black Versus White Race With Ambulatory Care Access and Quality in Medicare Advantage and Traditional Medicare, 2015-2018
eTable 4. Association of Medicare Advantage vs. Traditional Medicare With Ambulatory Care Access and Quality by Beneficiary Black and White Race, 2015-2018
eTable 5. Association of Medicare Advantage vs. Traditional Medicare With Differences in Access and Quality for Black vs. White Race Beneficiaries, 2015-2018
References
- 1.Braveman P. Health inequalities by class and race in the US: what can we learn from the patterns? Soc Sci Med. 2012;74(5):665-667. doi: 10.1016/j.socscimed.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 2.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. doi: 10.17226/12875 [DOI] [PubMed] [Google Scholar]
- 3.Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. 2016;37(1):375-394. doi: 10.1146/annurev-publhealth-032315-021439 [DOI] [PubMed] [Google Scholar]
- 4.Johnston KJ, Hockenberry JM. Are two heads better than one or do too many cooks spoil the broth? the trade-off between physician division of labor and patient continuity of care for older adults with complex chronic conditions. Health Serv Res. 2016;51(6):2176-2205. doi: 10.1111/1475-6773.12600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnston KJ, Wen H, Joynt Maddox KE. Lack of access to specialists associated with mortality and preventable hospitalizations of rural Medicare beneficiaries. Health Aff (Millwood). 2019;38(12):1993-2002. doi: 10.1377/hlthaff.2019.00838 [DOI] [PubMed] [Google Scholar]
- 6.National Academies of Science, Engineering, and Medicine . Systems Practices for the Care of Socially At-Risk Populations. National Academies Press; 2016. doi: 10.17226/21914 [DOI] [PubMed] [Google Scholar]
- 7.Millman AM, ed; Institute of Medicine Committee on Monitoring Access to Personal Health Care Services . Access to Health Care in America. National Academies Press; 2009. [Google Scholar]
- 8.Centers for Medicare & Medicaid Services . 2018 National Impact Assessment Quality Measures Report. Dept of Health and Human Services; 2018. Accessed March 12, 2021. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Downloads/2018-Impact-Assessment-Report.pdf
- 9.Centers for Medicare & Medicaid Services . Racial, Ethnic, and Gender Disparities in Health Care in Medicare Advantage. Centers for Medicare & Medicaid Services; April 2020. Accessed March 12, 2021. https://www.cms.gov/files/document/2020-national-level-results-race-ethnicity-and-gender-pdf.pdf
- 10.Lind KE, Hildreth KL, Perraillon MC. Persistent disparities in Medicare’s annual wellness visit utilization. Med Care. 2019;57(12):984-989. doi: 10.1097/MLR.0000000000001229 [DOI] [PubMed] [Google Scholar]
- 11.Johnston KJ, Mittler J, Hockenberry JM. Patient social risk factors and continuity of care for Medicare beneficiaries. Health Serv Res. 2020;55(3):445-456. doi: 10.1111/1475-6773.13272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010;38(4):381-388. doi: 10.1016/j.amepre.2009.12.026 [DOI] [PubMed] [Google Scholar]
- 13.Figueroa JF, Burke LG, Horneffer KE, Zheng J, John Orav E, Jha AK. Avoidable hospitalizations and observation stays: shifts in racial disparities. Health Aff (Millwood). 2020;39(6):1065-1071. doi: 10.1377/hlthaff.2019.01019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services . 2018 Medicare Current Beneficiary Survey Methodology Report. Centers for Medicare & Medicaid Services; 2018. Accessed July 9, 2021. https://www.cms.gov/research-statistics-data-and-systemsresearchmcbscodebooks/2018-mcbs-methodology-report
- 15.Centers for Medicare & Medicaid Services . Medicare Current Beneficiary Survey 2018 Data User’s Guide: Public Use File. Centers for Medicare & Medicaid Services; 2020:1-30. Accessed June 2, 2021. https://www.cms.gov/files/document/2018-mcbs-puf-user-guide.pdf
- 16.Jarrín OF, Nyandege AN, Grafova IB, Dong X, Lin H. Validity of race and ethnicity codes in Medicare administrative data compared with gold-standard self-reported race collected during routine home health care visits. Med Care. 2020;58(1):e1-e8. doi: 10.1097/MLR.0000000000001216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities research framework. Am J Public Health. 2019;109(S1):S16-S20. doi: 10.2105/AJPH.2018.304883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services . Medicare Advantage state/county penetration. Accessed December 31, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MCRAdvPartDEnrolData/MA-State-County-Penetration
- 19.Center for Evaluative Clinical Sciences at Dartmouth . Hospital and Physician Capacity Update. Center for Evaluative Clinical Sciences at Dartmouth; 2009:1-19.
- 20.US Department of Agriculture . Rural-Urban Commuting Area codes. Accessed March 2, 2021. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx
- 21.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645. doi: 10.1056/NEJMsa022615 [DOI] [PubMed] [Google Scholar]
- 22.Murphy-Barron C, Pyenson B, Ferro C, Emery M. Comparing the Demographics of Enrollees in Medicare Advantage and Fee-For-Service Medicare. Milliman; October 2020. Accessed March 25, 2021. https://bettermedicarealliance.org/wp-content/uploads/2020/10/Comparing-the-Demographics-of-Enrollees-in-Medicare-Advantage-and-Fee-for-Service-Medicare-202010141.pdf
- 23.Schneider EC, Cleary PD, Zaslavsky AM, Epstein AM. Racial disparity in influenza vaccination: does managed care narrow the gap between African Americans and whites? JAMA. 2001;286(12):1455-1460. doi: 10.1001/jama.286.12.1455 [DOI] [PubMed] [Google Scholar]
- 24.Ayanian JZ, Landon BE, Zaslavsky AM, Newhouse JP. Racial and ethnic differences in use of mammography between Medicare Advantage and traditional Medicare. J Natl Cancer Inst. 2013;105(24):1891-1896. doi: 10.1093/jnci/djt333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Timbie JW, Bogart A, Damberg CL, et al. Medicare Advantage and fee-for-service performance on clinical quality and patient experience measures: comparisons from three large states. Health Serv Res. 2017;52(6):2038-2060. doi: 10.1111/1475-6773.12787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyers DJ, Durfey SNM, Gadbois EA, Thomas KS. Early adoption of new supplemental benefits by Medicare Advantage plans. JAMA. 2019;321(22):2238-2240. doi: 10.1001/jama.2019.4709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaiser Family Foundation . Racial and ethnic health inequities and Medicare. Published February 16, 2021. Accessed March 12, 2021. https://www.kff.org/medicare/report/racial-and-ethnic-health-inequities-and-medicare/
- 28.Li Y, Cen X, Cai X, Thirukumaran CP, Zhou J, Glance LG. Medicare Advantage associated with more racial disparity than traditional Medicare for hospital readmissions. Health Aff (Millwood). 2017;36(7):1328-1335. doi: 10.1377/hlthaff.2016.1344 [DOI] [PubMed] [Google Scholar]
- 29.Agniel D, Martino SC, Burkhart Q, et al. Incentivizing excellent care to at-risk groups with a health equity summary score. J Gen Intern Med. 2019. doi: 10.1007/s11606-019-05473-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CMS Office of Minority Health . Stratified reporting. Published 2020. Accessed March 31, 2021. https://www.cms.gov/About-CMS/Agency-Information/OMH/research-and-data/statistics-and-data/stratified-reporting
- 31.Kronick R, Welch WP. Measuring coding intensity in the Medicare Advantage program. Medicare Medicaid Res Rev. 2014;4(2):mmrr2014.004.02.a06. doi: 10.5600/mmrr.004.02.sa06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobs PD, Kronick R. Getting what we pay for: how do risk-based payments to Medicare Advantage plans compare with alternative measures of beneficiary health risk? Health Serv Res. 2018;53(6):4997-5015. doi: 10.1111/1475-6773.12977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Newhouse JP, Landrum MB, Price M, McWilliams JM, Hsu J, McGuire TG. The comparative advantage of Medicare Advantage. Am J Health Econ. 2019;5(2):281-301. doi: 10.1162/ajhe_a_00120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freed M, Damico A, Neuman T. A dozen facts about Medicare Advantage in 2020. Kaiser Family Foundation; January 13, 2020. Accessed October 27, 2020. https://www.kff.org/medicare/issue-brief/a-dozen-facts-about-medicare-advantage-in-2020/
- 35.Feyman Y, Pizer SD, Frakt AB. The persistence of Medicare Advantage spillovers in the post-Affordable Care Act era. Health Econ. 2021;30(2):311-327. doi: 10.1002/hec.4199 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Study Sample Selection Flowchart
eTable 1. Comparing Medicare Beneficiaries Included Versus Excluded From Study Sample, 2015-2018
eTable 2. Characteristics of Study Sample Beneficiaries by Race and Ethnicity, 2015-2018
eTable 3. Association of Black Versus White Race With Ambulatory Care Access and Quality in Medicare Advantage and Traditional Medicare, 2015-2018
eTable 4. Association of Medicare Advantage vs. Traditional Medicare With Ambulatory Care Access and Quality by Beneficiary Black and White Race, 2015-2018
eTable 5. Association of Medicare Advantage vs. Traditional Medicare With Differences in Access and Quality for Black vs. White Race Beneficiaries, 2015-2018


