Abstract
Background:
Prospective studies evaluating second-look imaging of meniscus root repair using a transtibial pull-out technique are limited; therefore, optimal surgical indications and the technique for meniscus root repair remain uncertain.
Hypothesis:
It was hypothesized that there would be a high rate of healing, improvement in meniscal extrusion, and prevention of articular cartilage degeneration and subchondral bone abnormalities after meniscus root repair.
Study Design:
Case series; Level of evidence, 4.
Methods:
Consecutive patients undergoing transtibial root repair were prospectively enrolled at 2 orthopaedic centers between March 2017 and January 2019. Pre- and postoperative magnetic resonance imaging (MRI) scans were reviewed by a musculoskeletal radiologist in a blinded fashion for meniscal healing, quantification of extrusion, articular cartilage grade, subchondral bone changes, and coronary/meniscotibial ligament abnormalities. Given persistent extrusion observed on postoperative MRI scans, an additional 10 patients gave consent and were enrolled for immediate (before weightbearing) postoperative MRI scans.
Results:
A total of 45 patients (16 male, 29 female; mean ± standard deviation age, 42.3 ± 12.9 years; body mass index, 31.6) were prospectively enrolled in the study; there were 47 meniscus root repairs: 29 medial and 18 lateral (2 with both). Postoperative MRI was obtained at an average of 6.3 months (range, 5.1-8 months); 98% of meniscal repairs had evidence of healing. Mean extrusion increased significantly, from 1.9 ± 1.5 mm preoperatively to 2.6 ± 1.4 mm postoperatively (P = .03). There was no significant progression of chondromalacia grade, subchondral edema, insufficiency fracture, subchondral cysts, or subchondral collapse. In the additional 10-patient cohort, the mean preoperative extrusion (1.6 ± 1.2 mm) was not significantly different from that immediately postoperatively (2.0 ± 1.0 mm; P = .23).
Conclusion:
Prospective MRI analysis of transtibial meniscus root repair confirmed a high rate of meniscal healing and no observable progression of cartilage degeneration or subchondral bone abnormalities at the short-term follow-up. However, meniscal extrusion worsened in the first 6 months after surgery.
Registration:
NCT03037242 (ClinicalTrials.gov identifier).
Keywords: meniscus, meniscus root, meniscal extrusion, meniscal tear, transtibial pull-out repair, prospective cohort
The meniscus root is a critical structure, as it helps the meniscus maintain its normal function as a shock absorber and secondary stabilizer.13,42 Meniscal extrusion can occur with root injuries and has been shown to be associated with degenerative osteochondral damage, especially during axial loading of the tibiofemoral joint.18 The loss of tibial attachment at the root of the meniscus impairs the ability to maintain hoop stress when the tibiofemoral joint is loaded. This loss of hoop stress is responsible for the increased contact pressures within the tibiofemoral joint, which can lead to early osteoarthritis.2,11,30
This new awareness has surgeons considering surgical repair for the treatment of meniscus root tears since it has been shown that nonoperative treatment and partial meniscectomy can lead to poor outcomes.17,23 Biomechanical data reported by Marzo and Gurske-DePerio33 demonstrated that repair of the meniscus root avulsion restored tibiofemoral contact pressures to a more favorable level. Clinical results from Ozkoc et al37 showed that mean Lysholm scores improved from 53 to 67 after repair of meniscus root avulsions. Arthroscopic transtibial pullout has become the most common technique for meniscus root repair.11,22–24,31,36 Although short-term clinical outcomes after meniscus root transtibial pull-out repair have been favorable, some studies have shown incomplete healing with persistent or increased extrusion.36,43 While there are several excellent studies on assessment of healing from centers in Asia, there is a lack of postoperative imaging data from patients in North America, where issues such as higher body mass index (BMI) may affect outcomes.15,19
The purpose of this study was to compare the prospective magnetic resonance imaging (MRI) outcomes of meniscus root repair in patients undergoing a transtibial pull-out technique in order to answer the following questions: (1) What is the rate of meniscus root healing on MRI in a prospective multicenter cohort of patients after transtibial root repair? (2) Does root repair and postoperative rehabilitation affect cartilage and subchondral bone health in the early postoperative period? (3) Is meniscal extrusion corrected using transtibial root repair? We hypothesized a high rate of healing, the prevention of both articular cartilage degeneration and subchondral bone abnormalities, and improvement in meniscal extrusion after meniscus root repair using a transtibial pull-out technique.
Methods
Study Population and Design
This multicenter prospective clinical and radiographic study included eligible patients undergoing meniscus root repair at 2 high-volume orthopaedic centers (Mayo Clinic and Columbia Orthopedic Group). After gaining approval from the institutional review board, patients were evaluated and gave consent to participate in research. The cohort inclusion criteria were patients aged 18 to 65 years with meniscus root avulsion tears requiring repair. These were defined as meniscus posterior horn root avulsions or full-thickness tears within 9 mm of the root attachment.27 Patients were enrolled between March 2017 and January 2019. Patients with ligamentous injuries who underwent concomitant reconstruction or those with malalignment who underwent corrective osteotomy were included. Root repair was typically performed to completion before ligamentous reconstruction. In the case of malalignment, corrective osteotomy was performed first, followed by root repair as a single surgery. Exclusion criteria included >5° malalignment without corrective osteotomy, Kellgren-Lawrence (K-L) grade >2 arthritis, workers’ compensation status, subchondral collapse on preoperative MRI, intraoperative Outerbridge grade ≥3 chondromalacia, or poor-quality meniscal tissue. This study was prospectively registered at ClinicalTrials.gov (NCT03037242).
Surgical Technique
Meniscus root repair was performed by experienced arthroscopic surgeons (A.J.K., P.A.S., and M.J.S.). Standard knee arthroscopy portals were created, including an ipsilateral portal made under direct visualization to ensure access to the posterior meniscus root. The posterior horn attachment was inspected and assessed. Percutaneous medial collateral ligament lengthening and reverse notchplasty were performed, as needed. A tibial socket was created at the meniscus root attachment. The targeting of the location was accomplished using a specialized transtibial root guide placed through the ipsilateral portal (Arthrex). Once the guide was positioned at the center of the meniscus root footprint, a 6-mm FlipCutter (Arthrex) was introduced into the joint through the drill sleeve on the medial proximal tibia. The FlipCutter was deployed, and a 6-mm diameter socket was created to a depth of 5 to 10 mm. The drill sleeve was tapped 7 mm in the tibia, and the FlipCutter was removed and replaced by a FiberStick (Arthrex), to be used later as a shuttle for passage of the meniscal sutures through the tibia. The FiberStick passing suture was retrieved through the contralateral viewing portal to avoid tangling during suture passage into the meniscus. A PassPort Button cannula (Arthrex) was then placed through the ipsilateral working portal to both prevent a soft tissue bridge and aid in suture management. A free No. 0 nonabsorbable Fiberlink suture (Arthrex) was then passed through the torn meniscus in a cinch stitch configuration using a self-retrieving suture passing device (Knee Scorpion; Arthrex). Two cinch sutures were placed along with a simple “leader” stitch close to the socket, which was used to lead the meniscal tissue into the socket during tensioning. All sutures were then shuttled through the tibial socket using the previously placed passing suture. The leader stitch was tensioned first, followed by the cinch sutures to reduce the meniscus back to the root attachment. The knee was then cycled to remove any potential creep from the meniscus-suture interface. Tibial fixation was obtained using a 4.75-mm SwiveLock anchor (Arthrex) placed into the proximomedial tibia through the previous incision near 90° of knee flexion.
Rehabilitation Protocol
During the first 6 weeks after surgery, full knee extension and nonweightbearing in a brace and knee flexion to 90° were allowed. After 6 weeks, brace use was discontinued, and the patient was allowed to begin progression to full weightbearing and full knee range of motion as tolerated. Knee loading at flexion angles >90° was not permitted until 4 months postoperatively. Return to athletic activity occurred at a minimum of 6 months postoperatively, if indicated.
Outcome Measures
Individual medical records were reviewed to obtain patient information, including age, sex, laterality, medial or lateral meniscus, and concomitant surgical procedures. Initial and follow-up knee MRI scans were evaluated by a board-certified musculoskeletal radiologist (A.C.J.) who was blinded to pre- and postoperative status. Follow-up MRI scans were obtained on average 6.3 months after surgery (range, 5.1-8 months). A 1.5-T MRI scanner at one site and a 3-T MRI scanner at the other site were utilized for pre- and postoperative imaging. The amount of meniscal extrusion, defined as protrusion of the peripheral margin of the meniscus beyond the tibial plateau except for osteophytes, was measured on coronal images at the midpoint of the medial femoral condyle of the initial and final MRI scans by measuring the distance from a vertical line intersecting the outer margin of the medial tibial plateau to the outer edge of the medial meniscus.5 Meniscal healing was classified as complete (continuity in sagittal, coronal, and axial MRI views), partial (loss of continuity in any 1 view), and not healed (no continuity in any view).23 The technique for assessing healing of meniscus root repairs and extrusion has been well established, and previous literature on interobserver reliability assessments has shown rates of ≥0.90.5,45 The femoral condyles and tibial plateau articular cartilage surfaces were evaluated and graded using the modified Outerbridge classification system.41,26 MRI scans were also assessed for coronary/meniscotibial ligament abnormalities, subchondral cysts, subchondral edema, insufficiency fractures, and subchondral collapse using the Whole-Organ Magnetic Resonance Imaging Score.12,40 Meniscus root tear was defined as a radial tear or complete avulsion of the meniscus within 9 mm of the root attachment.27 Subchondral edema was defined as focal bone marrow signal change with increased signal on T2-weighted imaging and hazy intermediate signal on T1-weighted imaging.6 Subchondral cysts were identified as well-defined areas or increased signal intensity in the subchondral bone on the fat-suppressed T2-weighted images. Insufficiency fractures were defined as curvilinear foci of low signal on T1-weighted and low to high signal on T2-weighted images, which are surrounded by edema-like marrow signal. These lesions are adjacent to, but at some distance from, subchondral bone plate.16 Radiographs were reviewed to evaluate osteoarthritis severity using the K-L grading system.21 Preoperative baseline and postoperative anteroposterior knee radiographs were reviewed. Osteoarthritis was graded as none (grade 0), doubtful (grade 1), minimal (grade 2), moderate (grade 3), or severe (grade 4). Patients with K-L grade >2 preoperatively were excluded. Long-leg standing radiographs were reviewed to assess mechanical axis alignment.
Observation of persistent or worsening extrusion on MRI, particularly on the medial side, generated concern that extrusion was not corrected using the root repair. Therefore, an additional 10 patients gave consent and were enrolled for immediate postoperative MRI scans within the first few weeks after surgery before the onset of weightbearing.
Statistical Analysis
Univariate analysis was calculated for patient, clinical, and radiologic variables. The Wilcoxon rank sum test was used for continuous variables, and the Fisher exact test or chi-square analysis was used for categorical variables between initial and follow-up MRI scans. The McNemar test was used to compare dichotomous variables between initial and final MRI scans. All tests were 2-sided, and P values <.05 were considered significant. Analysis was performed using SAS JMP Version 14.1.0 (SAS).
RESULTS
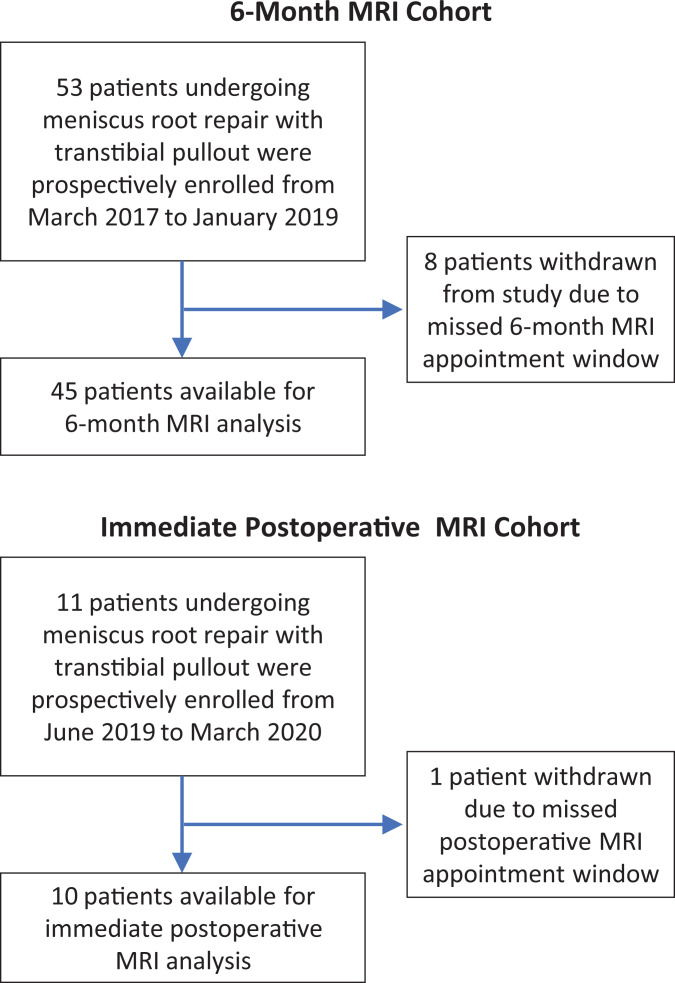
A total of 45 patients, including 29 women and 16 men, underwent 47 meniscus root repairs between March 2017 and January 2019. A flow diagram of patient eligibility and inclusion for analysis is shown in Figure 1. Characteristics of the patient cohort are listed in Table 1. One patient had both medial and lateral root repairs on their ipsilateral knee, while another had the left medial and right lateral roots repaired. Four knees did not have postoperative MRI scans for analysis. The final study cohort included 47 knees, including 43 knees with both pre- and postoperative MRI scans. The postoperative MRI scan was obtained on average 6.3 months (range, 5.1-8 months) after surgery. The average preoperative K-L grade was 0.46 (range, 0-2), with the average postoperative grade being 0.84 (range, 0-2) (P = .01). The postoperative K-L grade was obtained on average 17.6 months (range, 1.4-26.1 months) after surgery. Long-leg standing radiographs were available for 21 of the 47 knees.
Figure 1.
Flowchart of study patients in the 6-month magnetic resonance imaging (MRI) and immediate postoperative MRI cohorts.
Table 1.
Summary of Patient Characteristicsa
| Sex | |
| Male | 16 (36) |
| Female | 29 (64) |
| Age at surgery, y | 42.28 ± 12.92 |
| Body mass index | 31.6 ± 7.29 |
| Side involved | |
| Left | 28 (60) |
| Right | 19 (40) |
| Medial meniscal involvement | 29 (62) |
| Lateral meniscal involvement | 18 (38) |
| Time to postoperative MRI, mo | 6.3 (5.1-8) |
| Time to postoperative radiograph, mo | 17.6 (1.4-26.1) |
| Time from injury to surgery, d | 65.6 (1-898) |
aContinuous variables are reported as mean ± SD; discrete variables, as mean (range); and dichotomous variables, as n (%). MRI, magnetic resonance imaging.
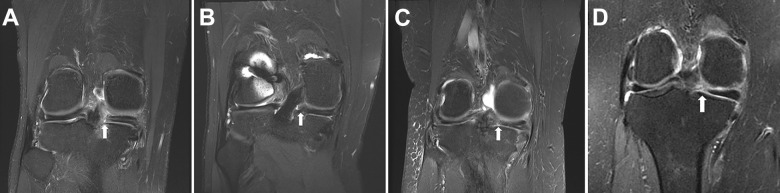
Of the 43 root tears with pre- and postoperative MRI scans, 98% had complete or partial healing after root repair. Specifically, 17 (40%) meniscus root tears healed completely, 25 (58%) healed partially, and 1 (2.3%) did not heal after surgery (Figure 2).
Figure 2.
Visualization of meniscus root tears (arrows) on coronal magnetic resonance imaging scans. (A) Preoperative meniscus root tear. (B) Postoperative healed meniscus root tear. (C) Postoperative partially healed meniscus root tear. (D) Postoperative nonhealed meniscus root tear.
There was no significant progression in articular cartilage grade, subchondral edema, insufficiency fracture, subchondral cysts, subchondral collapse, or coronary/meniscotibial ligament abnormality (Table 2). In review of the available long-leg standing radiographs, there was no correlation between mechanical axis and amount of extrusion, presence of major extrusion >3 mm, or progression of extrusion. There was also no correlation between BMI and preoperative (P = .92) or postoperative (P = .20) extrusion. The presence of concomitant ligamentous reconstruction or corrective osteotomy procedures was negatively correlated with pre- and postoperative extrusion. Patients who underwent isolated meniscus root repair were more likely to have preoperative extrusion (P = .03) and postoperative extrusion (P < .01) at the 6-month MRI follow-up.
Table 2.
Summary of Magnetic Resonance Imaging Characteristicsa
| Preoperatively | Postoperatively | P Value | |
|---|---|---|---|
| Articular cartilage Outerbridge grade, femur | 1 (0-4) | 1 (0-4) | .66 |
| Articular cartilage Outerbridge grade, tibia | 0 (0-2) | 1 (0-3) | .15 |
| Subchondral edema, femur | 10 (23) | 7 (16) | .59 |
| Subchondral edema, tibia | 16 (37) | 9 (21) | .15 |
| Insufficiency fracture, femur | 5 (12) | 0 (0) | .06 |
| Insufficiency fracture, tibia | 6 (14) | 1 (2) | .11 |
| Subchondral cysts, femur | 0 (0) | 5 (12) | .06 |
| Subchondral cysts, tibia | 0 (0) | 0 (0) | ≥.99 |
| Subchondral collapse, femur | 2 (5) | 0 (0) | .49 |
| Subchondral collapse, tibia | 1 (2) | 1 (2) | ≥.99 |
| Coronary/meniscotibial ligament abnormality | 26 (60) | 30 (70) | .50 |
aDiscrete variables are reported as mean (range) and dichotomous variables as number (%).
A total of 28 (65%) knees demonstrated meniscal extrusion preoperatively, which increased to 36 (84%) postoperatively (Figure 2). Table 3 contains a summary of preoperative and postoperative meniscal characteristics of the cohort. Of the 26 knees with medial meniscus root tears, 19 had evidence of preoperative extrusion, while all 26 had postoperative extrusion (P = .01). Nine of the 17 knees with lateral meniscus root tears experienced preoperative extrusion, with 11 experiencing postoperative extrusion (P = .73). The amount of overall meniscal extrusion increased from an average of 1.9 mm preoperatively to 2.6 mm postoperatively (P = .03). Medial meniscal extrusion increased from an average of 2.3 mm preoperatively to 3.2 mm postoperatively (P = .01). Lateral meniscal extrusion increased from an average of 1.3 mm preoperatively to 1.8 mm postoperatively (P = .44). In the 17 knees that experienced complete healing of their meniscus root tears, 12 had extrusion before surgery, and 14 had extrusion after surgery (P = .69). The mean overall meniscal extrusion in the fully healed knees increased from 1.9 mm preoperatively to 2.4 mm postoperatively (P = .18). In the 25 knees that experienced partial healing of their meniscus root tears, 15 had extrusion before surgery, and 21 had extrusion after surgery (P = .11). The mean overall meniscal extrusion in the partially healed root cohort increased from 2.0 preoperatively to 2.7 mm postoperatively (P = .11).
Table 3.
Summary of Preoperative and Postoperative Meniscal Characteristicsa
| Preoperatively | Postoperatively | P Value | |
|---|---|---|---|
| Meniscal extrusion | 28 (65) | 36 (84) | .08 |
| Meniscal extrusion, mm | 1.9 ± 1.5 | 2.6 ± 1.4 | .03 |
| Medial meniscal extrusion | 19 (73) | 26 (100) | .01 |
| Medial meniscal extrusion, mm | 2.3 ± 1.5 | 3.2 ± 0.9 | .01 |
| Lateral meniscal extrusion | 9 (53) | 11 (65) | .73 |
| Lateral meniscal extrusion, mm | 1.3 ± 1.5 | 1.8 ± 1.6 | .44 |
| Meniscal healing | |||
| Complete | 17 (40) | ||
| Extrusion | 12 | 14 | .69 |
| Extrusion, mm | 1.9 ± 1.6 | 2.4 ± 1.4 | .18 |
| Partial | 25 (58) | ||
| Extrusion | 15 | 21 | .11 |
| Extrusion, mm | 2.0 ± 1.5 | 2.7 ± 1.5 | .11 |
| Nonhealed | 1 (2) | ||
| Extrusion | 1 | 1 | |
| Extrusion, mm | 3.3 | 4.2 |
aContinuous variables are reported as mean ± SD, and dichotomous variables are reported as n (%). Bolded P values indicate a statistically significant difference between pre- and postoperatively (P < .05). Blank cells indicate that no value was available since healing was assessed as a postoperative outcome.
The 10-patient cohort underwent postoperative MRI at a mean of 15.6 days after root repair. The mean extrusion increased from 1.64 ± 1.19 mm before surgery to 2.0 ± 0.98 mm after surgery, although this finding did not reach statistical significance (P = .23). Seven of the 10 enrolled patients experienced preoperative extrusion. All of the patients who experienced preoperative extrusion continued to have extrusion postoperatively. Additionally, 2 of the patients without preoperative extrusion developed extrusion after surgery (Table 4). Of the 7 patients with preoperative extrusion, 3 had decreased extrusion, 1 patient had no change, and 3 patients had increased extrusion on postoperative MRI. The average improvement measured 0.63 mm, and the average worsening measured 1.1 mm. Extrusion was unchanged in 2 patients, 1 of whom had no extrusion at any time.
Table 4.
Pre- and Postoperative Meniscal Extrusion With Postoperative Magnetic Resonance Imaging Obtained on Average 15.6 Days Postoperatively
| Preoperatively | Postoperatively | P Value | |
|---|---|---|---|
| No. of patients (%) | 7 (70) | 9 (90) | 0.58 |
| Mean ± SD | 1.64 ± 1.19 | 2.0 ± 0.98 | 0.23 |
Discussion
Interest in meniscus root tears has been growing since Pagnani et al38 initially described posterior root tears and associated meniscal extrusion. While there has been an increased focus on repair of meniscus root tears, few prospective studies have evaluated the optimal surgical indications and technique. The purpose of this prospective study was to determine the clinical and radiographic outcomes of meniscus root repair using a transtibial pull-out technique, specifically focusing on MRI rate of healing, cartilage preservation, and meniscal extrusion. Our findings demonstrated that meniscus root repair results in a high rate of healing and no observable subchondral bone abnormalities at short-term follow-up. However, meniscal extrusion did not improve and actually got worse.
It has been well documented that meniscus root repair significantly improves pain and function while limiting progression of knee osteoarthritis.22,28,29,31 Our study illustrated that short-term outcomes of meniscus root repair utilizing a transtibial pull-out technique are very good, with 98% complete or partial healing at 6 months postoperatively. These results are compatible with the current literature. Lee et al31 reported complete healing of the meniscus root after pull-out suture repair for all 10 patients when examined using second-look arthroscopy. Kim et al23 compared medial meniscus root repair to meniscectomy and demonstrated that on second-look MRI scans and radiographs, the repair cohort had a slower progression of knee osteoarthritis with decreased joint space narrowing and 93.3% of the patients experienced complete or partial healing of the meniscus on postoperative follow-up MRI. Moon et al36 showed good healing in 90.3% of their patients after arthroscopic pull-out repair. Feucht et al,11 in a systemic review, showed that there was complete or partial healing in 96% of 137 patients examined using second-look arthroscopy and MRI.
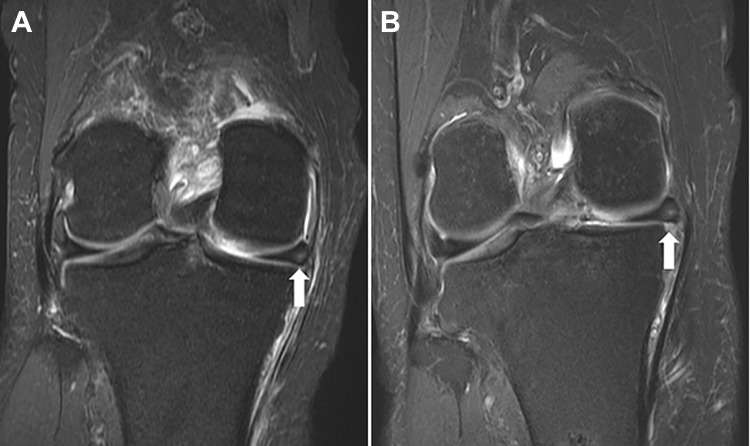
The posterior horn of the meniscus is critical to maintaining normal knee biomechanics, as it helps to distribute hoop stresses and prevent meniscal extrusion. It has been shown that posterior meniscus root tears are biomechanically similar to subtotal meniscectomy with regard to knee function and progression to osteoarthritis.1 Late detection methods such as plain radiographs can show subchondral bone changes as well as cartilage thinning.4 While plain radiographs are useful in their indirect examination of the articular cartilage, MRI assessment provides a more detailed picture that can provide specific information regarding the nature of the cartilage and subchondral bone.14,39 Our results showed that meniscus root repair may be chondroprotective at short-term follow-up. When compared with the preoperative MRI, the postoperative MRI showed no difference in cartilage degeneration, subchondral cysts, or subchondral collapse. There was actually a trend toward improvement in subchondral edema and insufficiency fractures (Figure 3). At least at the 6-month time frame after transtibial root repair, our finding of worsening extrusion—although worrisome from the biomechanical standpoint—does not promote articular cartilage deterioration, but we need longer follow-up on the true effect of this extrusion. Longer-term follow-up with careful assessment of extrusion magnitude is required to determine if meniscus root repair prevents articular cartilage degeneration, and there may be a threshold of critical extrusion that is biomechanically important to resist hoop stress.
Figure 3.
(A) Preoperative meniscal extrusion (arrow) and (B) worsening postoperative meniscal extrusion (arrow) on coronal magnetic resonance imaging scans.
Meniscus root tears are known to be associated with meniscal extrusion.3,32,38 Meniscal extrusion has been shown to lead to accelerated joint destruction and progression of osteoarthritis.10,30 This is further evidenced by a recent biomechanical investigation of medial meniscal extrusion in the presence of intact roots, which demonstrated significantly reduced tibiofemoral contact areas with extrusion of ≥4 mm.9 The present study demonstrated that while transtibial pull-out repair resulted in a significant rate of meniscal healing, it did not halt meniscal extrusion. The data regarding improvement of meniscal extrusion utilizing a transtibial pull-out technique are mixed. Kim et al23 showed that mean extrusion decreased from 3.13 mm to 2.94 mm after transtibial pull-out repair at a mean follow-up of 48.5 months. Masuda et al34 also demonstrated improvement in meniscal extrusion after pull-out repair. However, there are other studies that have demonstrated no improvement or worsening of meniscal extrusion after root repair. A meta-analysis by Chung et al7 reported an increase in meniscal extrusion after medial meniscus posterior root tear fixation. Moon et al36 described a mean meniscal extrusion increase from 3.6 mm to 5.0 mm after transtibial pull-out repair at a mean follow-up of 24 months. Chung et al8 also showed that while medial meniscus posterior root tear pull-out fixation can lead to favorable outcomes, it does not always improve extrusion. Our study also demonstrated an increase in coronary/meniscotibial ligament abnormalities, which have been shown to be associated with meniscal extrusion.25
Additionally, our data showed that while patients with both fully healed roots and partially healed roots experienced increased extrusion postoperatively, those with partially healed roots did have a greater amount of overall extrusion compared with the fully healed cohort. When comparing medial versus lateral meniscus root tears pre- and postoperatively, we found a statistically significant increase of meniscal extrusion in medial root tears compared with lateral root tears.
Our data also demonstrated a negative relationship between the presence of concomitant ligamentous reconstruction or corrective osteotomy and extrusion, both pre- and postoperatively. Patients with additional injuries had less extrusion compared with patients with isolated root tears. This finding is likely because of the more acute and traumatic nature of injuries experienced by patients who underwent additional ligamentous reconstruction, which may affect the degree of meniscal extrusion. On the other hand, patients who were evaluated with isolated root tears likely experienced a more chronic and degenerative meniscal pathology, allowing for greater extrusion to develop over a longer period of altered knee biomechanics.
The additional 10-patient cohort demonstrated that meniscal extrusion remained persistent in the immediate postoperative period after transtibial pull-out repair. There are limited available data regarding assessment of meniscal extrusion immediately after repair. Kamatsuki et al20 evaluated 3-month postoperative MRI scans after pull-out repair and found mean medial meniscal extrusion to be 4.3 ± 1.5 mm compared with 4.2 ± 1.2 mm preoperatively. They concluded that early arthroscopic surgery for medial meniscus root repair was more effective in preventing an increase in extrusion compared with delayed surgery.
BMI could play a role in the increased instance of meniscal extrusion seen in our study. The average BMI of our cohort was 31.6, which is greater than that of other cohorts in the literature. The average BMI in the study by Masuda et al34 was 26.6, and the average BMI in the study by Kim et al23 was 26.8 in the repair cohort. Both of these studies showed improvement in meniscal extrusion after transtibial pull-out repair. Additionally, a recent investigation by Zhang et al44 of patients undergoing transtibial pull-out repair for medial meniscus root tears reported high BMI (>30) as a significant risk factor for decreased postoperative International Knee Documentation Committee scores at the 1-year follow-up; however, the relationship between meniscal extrusion and clinical outcomes remains unclear.
The multicenter prospective nature of our study with inclusion of both medial and lateral root repairs allows our data to be generalizable and is a relative strength. However, our study is not without limitations. We utilized postoperative MRI to evaluate surgical outcomes as opposed to second-look arthroscopy. However, MRI healing has been well documented in other studies to correlate with arthroscopic findings.35 Additionally, the imaging protocols between the 2 sites regarding pre- and postoperative imaging were not completely standardized—one site utilized a 1.5-T scanner, while the other site used a 3-T scanner. Each site, however, adhered to their respective standardized imaging protocols among patients for both pre- and postoperative imaging. While we blinded our radiologist to pre- and postoperative status, completely anonymizing this was difficult because of the presence of transtibial tunnels. Long-limb radiographs were available for less than half of the studied knees, which could lead to a skewed analysis of alignment and how it correlates with worsening extrusion. Additionally, this study may not have been sufficiently powered to detect differences among the studied variables, particularly with only 10 patients in the immediate postoperative MRI cohort. The primary objective of this study was to examine structural MRI changes in the meniscus, cartilage, and bone after transtibial root repair; as such, patient outcomes were excluded.
Conclusion
Prospective MRI analysis of transtibial meniscus root repair confirmed a high rate of meniscal healing and no observable progression of cartilage degeneration or subchondral bone abnormalities at short-term follow-up. However, meniscal extrusion worsened, even in the immediate postoperative period. Additional studies should evaluate techniques to improve meniscal extrusion.
Footnotes
Final revision submitted February 24, 2021; accepted March 2, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Arthrex provided research support for this study and financial support for study coordinator efforts. Support was also received from the Foderaro/Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund, and B.M.S. received partial funding from the National Institutes of Health (NIH)–National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). The contents of this study are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. A.J.K. has received grant support from Aesculap, Ceterix, Histogenics, Exactech, and Gemini Mountain; consulting fees from Arthrex, Joint Restoration Foundation, and Responsive Arthroscopy; speaking fees from Arthrex; honoraria from Vericel and Joint Restoration Foundation; royalties from Arthrex; and personal fees from DePuy; and is a board member for the Musculoskeletal Transplant Foundation. A.C.J. has received hospitality payments from Encore Medical and Zimmer Biomet. P.A.S. has received consulting fees from Arthrex, nonconsulting fees from Alpha Orthopedic Systems, education payments from Elite Orthopedics, speaking fees from Medical Device Business Services, and personal fees from Spinal Simplicity. M.J.S. has received grants from Arthrex and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Mayo Clinic (No. 16-005841).
References
- 1.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 2.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 3.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–810. [DOI] [PubMed] [Google Scholar]
- 4.Buckland-Wright C. Subchondral bone changes in hand and knee osteoarthritis detected by radiography. Osteoarthritis Cartilage. 2004;12(suppl A):S10–S19. [DOI] [PubMed] [Google Scholar]
- 5.Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–1606. [DOI] [PubMed] [Google Scholar]
- 6.Choi JY, Chang EY, Cunha GM, et al. Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol. 2014;203(6):1286–1292. [DOI] [PubMed] [Google Scholar]
- 7.Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–1468. [DOI] [PubMed] [Google Scholar]
- 8.Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. [DOI] [PubMed] [Google Scholar]
- 9.Debieux P, Jimenez AE, Novaretti JV, et al. Medial meniscal extrusion greater than 4 mm reduces medial tibiofemoral compartment contact area: a biomechanical analysis of tibiofemoral contact area and pressures with varying amounts of meniscal extrusion. Knee Surg Sports Traumatol Arthrosc. Published online November 22, 2020. doi:10.1007/s00167-020-06363-0 [DOI] [PubMed] [Google Scholar]
- 10.Emmanuel K, Quinn E, Niu J, et al. Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24(2):262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feucht MJ, Kuhle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. [DOI] [PubMed] [Google Scholar]
- 12.Filardo G, Kon E, Tentoni F, et al. Anterior cruciate ligament injury: post-traumatic bone marrow oedema correlates with long-term prognosis. Int Orthop. 2016;40(1):183–190. [DOI] [PubMed] [Google Scholar]
- 13.Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990;252:19–31. [PubMed] [Google Scholar]
- 14.Folkesson J, Olsen OF, Pettersen P, Dam E, Christiansen C.Combining binary classifiers for automatic cartilage segmentation in knee MRI. In: Liu Y, Jiang T, Zhang C, eds. Lecture Notes in Computer Science. Vol 3765. Springer; 2005:230–239. [Google Scholar]
- 15.Furumatsu T, Okazaki Y, Hiranaka T, et al. An MRI-based suspension bridge sign can predict an arthroscopically favorable meniscal healing following the medial meniscus posterior root repair. J Orthop Sci. 2021;26(2):237–242. [DOI] [PubMed] [Google Scholar]
- 16.Gorbachova T, Amber I, Beckmann NM, et al. Nomenclature of subchondral nonneoplastic bone lesions. AJR Am J Roentgenol. 2019;213(5):963–982. [DOI] [PubMed] [Google Scholar]
- 17.Han SB, Shetty GM, Lee DH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326–1332. [DOI] [PubMed] [Google Scholar]
- 18.Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189–192. [DOI] [PubMed] [Google Scholar]
- 19.Hiranaka T, Furumatsu T, Kamatsuki Y, et al. The distance between the tibial tunnel aperture and meniscal root attachment is correlated with meniscal healing status following transtibial pullout repair for medial meniscus posterior root tear. Knee. 2020;27(3):899–905. [DOI] [PubMed] [Google Scholar]
- 20.Kamatsuki Y, Furumatsu T, Miyazawa S, et al. The early arthroscopic pullout repair of medial meniscus posterior root tear is more effective for reducing medial meniscus extrusion. Acta Med Okayama. 2019;73(6):503–510. [DOI] [PubMed] [Google Scholar]
- 21.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim JH, Chung JH, Lee DH, et al. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. [DOI] [PubMed] [Google Scholar]
- 23.Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–354. [DOI] [PubMed] [Google Scholar]
- 24.Kim YM, Rhee KJ, Lee JK, et al. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22(7):795.e791-e794. [DOI] [PubMed] [Google Scholar]
- 25.Krych AJ, Bernard CD, Leland DP, et al. Isolated meniscus extrusion associated with meniscotibial ligament abnormality. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3599–3605. [DOI] [PubMed] [Google Scholar]
- 26.Krych AJ, Johnson NR, Mohan R, et al. Arthritis progression on serial MRIs following diagnosis of medial meniscal posterior horn root tear. J Knee Surg. 2018;31(7):698–704. [DOI] [PubMed] [Google Scholar]
- 27.LaPrade CM, James EW, Cram TR, et al. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 28.LaPrade CM, James EW, LaPrade RF. A modified transtibial pull-out repair for posterior root avulsions of the lateral meniscus with concomitant anterior cruciate ligament reconstruction: a report of two cases. JBJS Case Connect. 2014;4(4):e96. [DOI] [PubMed] [Google Scholar]
- 29.LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–891. [DOI] [PubMed] [Google Scholar]
- 30.Lee DH, Lee BS, Kim JM, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. [DOI] [PubMed] [Google Scholar]
- 31.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 32.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–574. [DOI] [PubMed] [Google Scholar]
- 33.Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–129. [DOI] [PubMed] [Google Scholar]
- 34.Masuda S, Furumatsu T, Okazaki Y, et al. Transtibial pullout repair reduces posterior extrusion of the medial meniscus. Acta Med Okayama. 2019;73(6):495–501. [DOI] [PubMed] [Google Scholar]
- 35.Miao Y, Yu JK, Ao YF, et al. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011;39(4):735–742. [DOI] [PubMed] [Google Scholar]
- 36.Moon HK, Koh YG, Kim YC, et al. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40(5):1138–1143. [DOI] [PubMed] [Google Scholar]
- 37.Ozkoc G, Circi E, Gonc U, et al. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. [DOI] [PubMed] [Google Scholar]
- 38.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297–300. [DOI] [PubMed] [Google Scholar]
- 39.Pakin SK, Tamez-Pena JG, Totterman S, Parker KJ. Segmentation, surface extraction, and thickness computation of articular cartilage. Proc SPIE Int Soc Opt Eng. 2002;4684:155–166. [Google Scholar]
- 40.Peterfy CG, Guermazi A, Zaim S, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12(3):177–190. [DOI] [PubMed] [Google Scholar]
- 41.Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee: an evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80(9):1276–1284. [DOI] [PubMed] [Google Scholar]
- 42.Radin EL, de Lamotte F, Maquet P. Role of the menisci in the distribution of stress in the knee. Clin Orthop Relat Res. 1984;185:290–294. [PubMed] [Google Scholar]
- 43.Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39(1):99–107. [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, Furumatsu T, Okazaki Y, et al. High body mass index is a risk factor for unfavorable clinical outcomes after medial meniscus posterior root repair in well-aligned knees. J Orthop Sci. 2021;26(3):430–434. [DOI] [PubMed] [Google Scholar]
- 45.Zhuo H, Pan L, Xu Y, Li J. Functional, magnetic resonance imaging, and second-look arthroscopic outcomes after pullout repair for avulsion tears of the posterior lateral meniscus root. Am J Sports Med. 2021;49(2):450–458. [DOI] [PubMed] [Google Scholar]