Abstract
Background:
Comminuted inferior pole patellar fractures can be treated in numerous ways. To date, there have been no studies comparing the biomechanical properties of transosseous tunnels versus suture anchor fixation for partial patellectomy and tendon advancement of inferior pole patellar fractures.
Hypothesis:
Suture anchor repair will result in less gapping at the repair site. We also hypothesize no difference in load to failure between the groups.
Study Design:
Controlled laboratory study.
Methods:
Ten cadaveric knee extensor mechanisms (5 matched pairs; patella and patellar tendon) were used to simulate a fracture of the extra-articular distal pole of the patella. The distal simulated fracture fragment was excised, and the patellar tendon was advanced and repaired with either transosseous bone tunnels through the patella or 2 single-loaded suture anchors preloaded with 1 suture per anchor. Load to failure and elongation from cycles 1 to 250 between 20 and 100 N of force were measured, and modes of failure were recorded. Statistical analysis was performed using a paired 2-tailed Student t test.
Results:
The suture anchor group had less gapping during cyclic loading as compared with the transosseous tunnel group (mean ± SD, 6.83 ± 2.23 vs 13.30 ± 5.74 mm; P = .047). There was no statistical difference in the load to failure between the groups. The most common mode of failure was at the suture-anchor interface in the suture anchor group (4 of 5) and at the knot proximally on the patella in the transosseous tunnel group (4 of 5).
Conclusion:
Suture anchors yielded similar strength profiles and less tendon gapping with cyclic loading when compared with transosseous tunnels in the treatment of comminuted distal pole of the patellar fractures managed with partial patellectomy and patellar tendon advancement.
Clinical Relevance:
Suture anchors may offer robust repair and earlier range of motion in the treatment of fractures of the distal pole of the patella. Clinical randomized controlled trials would help clinicians better understand the difference in repair techniques and confirm the translational efficacy in clinical practice.
Keywords: knee, patellar fracture, patellar tendon, suture anchors, transpatellar tunnels, transosseous sutures, biomechanics
Fractures of the inferior pole of the patella are relatively common, accounting for >10% of all patellar fractures.10 These fractures typically occur as the result of direct impact onto a flexed knee with simultaneous contraction of the quadriceps musculature, resulting in an eccentric load and avulsion about the extra-articular inferior pole of the patella. These fractures are typically managed operatively, given the disruption of the extensor mechanism. There is no consensus regarding the ideal method of treating these injuries. Options include tension band wiring, circumferential wiring, fixation with plate and screws, and, in the setting of inferior pole comminution, a partial patellectomy with reattachment of the patellar tendon.5,12,16–18 A common technique is partial patellectomy and patellar tendon reattachment using transosseous tunnel (TT), with data demonstrating superior patient-reported outcomes and fewer hardware-related complications when compared with tension band wiring.8
Recently, there has been interest in the use of suture anchor (SA) for patellar tendon repairs. Biomechanical studies that evaluated tendon repair using SAs (without an inferior pole patellar fracture) demonstrated less gap formation with cyclic loading and higher loads to failure when compared with transosseous tendon repair.6,9 These benefits may allow patients to initiate earlier range of motion and potentially decrease the risk of failure. However, there are limited reports on the use of SA repair for inferior pole patellar fractures, which involves placing the anchors into cancellous bone as opposed to fixation in cortical bone in patellar tendon tears alone (with no fracture). In 2010, Anand et al1 reported on the use of SA for patellar tendon reattachment after partial patellectomy for inferior pole patellar fracture. While the results showed a good range of motion without any failures at follow-up, the study was limited by its retrospective design, lack of a comparison arm, and small sample size (n = 5).
The lack of SA use in the setting of inferior pole fracture may stem from the relative paucity of biomechanical data demonstrating efficacy of this repair technique. Furthermore, when compared with isolated patellar tendon repair, the presence of an inferior pole fracture requires that anchors be placed into cancellous bone after the partial patellectomy, potentially increasing the risk of pullout attributed to poor bone quality.14 In this study, we perform a biomechanical analysis of SA repair versus TT repair after partial patellectomy for inferior patellar pole fractures. We hypothesized that there would be less gapping with cyclic loading in the SA group, with equivalent loads to failure between the groups.
Methods
Ten fresh-frozen cadaveric specimens (5 matched pairs) were used. These specimens were donated by the Rhode Island Hospital Orthopedic Foundation. An a priori power analysis was performed utilizing an effect size of 0.3 (G*Power Version 3.1). This was based on previous load-to-failure and displacement data.6,9 With an alpha of .05 and a power of 0.90 (1 – beta error probability), it was determined that we would achieve adequate power with the inclusion of 5 specimens in each group. The extensor mechanisms of the cadaveric knees were carefully dissected from the surrounding soft tissue and joint. The quadriceps tendon was transected 5 cm from its attachment to the patella, all soft tissues around the patella and the patellar tendon were removed sharply, and the patellar tendon was taken directly off its attachment on the tibial tubercle. Tendons were thoroughly inspected, and no apparent signs of damage or degeneration were found. Each specimen had dual-energy x-ray absorptiometry (DEXA) testing performed before the dissection to ensure adequate bone quality. Only specimens with a T score > –1.0 (normal range) were used in this study. After proper thawing, all specimens were kept at room temperature and wrapped in moist gauze (0.9% NaCl) to maintain the moisture of the tendon during preparation and testing.
Fracture Creation
Inferior pole patellar fractures were created distal to the inferior articular surface of the patella using a sagittal saw. The distal fragment was sharply excised from the tendon, with care taken to excise only the bony fragment. Matched-pair specimens were randomized to either repair with the TT method or SA. The schematic for repair in shown in Figure 1.
Figure 1.
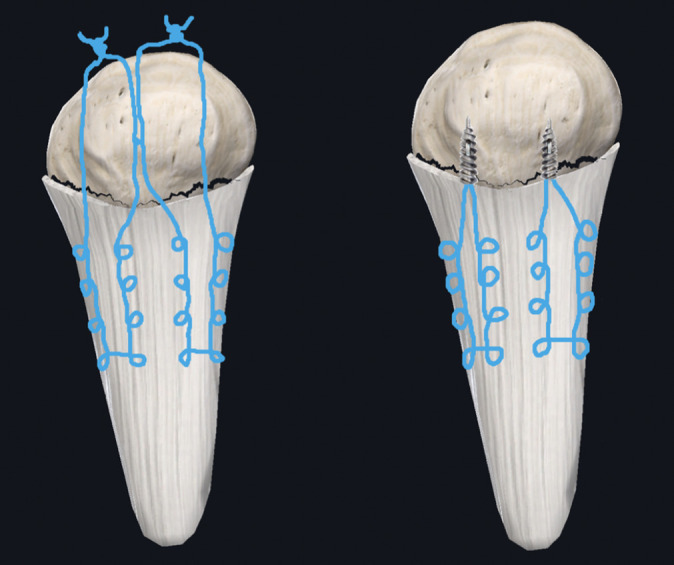
Schematic of repair strategies: left, transosseous tunnel repair using suture; right, suture anchor repair.
Transosseous Repair
Three transpatellar tunnels were drilled inferior to superior in each third of the patella (medial to lateral) using a 2.5-mm drill bit. Attention was taken to ensure that the articular cartilage was not penetrated and that the drill tunnels were parallel and in the midsubstance of the bone. The patellar tendon was sutured with No. 2 FiberWire (Arthrex) in a standard Krackow fashion with 4 throws. This was done twice: once on the medial side of the patellar tendon and once on the lateral side to create 4 suture limbs. The sutures were passed through the TT (1 in the medial tunnel, 2 in the middle tunnel, and 1 in the lateral tunnel) and hand tied with 6 square knots on the superior aspect of the patella over the bone bridge created by the tunnels (Figure 1).
SA Repair
Two 4.5-mm drill holes were placed in the cancellous fracture bed at the medial and lateral thirds of the bone, at the junction between the anterior third and posterior two-thirds of the bone. Two TWINFIX Ti 5.0-mm anchors preloaded with No. 2 Ultrabraid sutures (Smith & Nephew) were fixed in the drill holes. One suture limb from each anchor was then run in a standard Krackow fashion with 4 throws on the medial and lateral side of the tendon. The suture ends were then tied to the remaining limb with 6 square knots at the anchor-tendon interface with the knot buried on the posterior aspect of the tendon (Figure 1).
Testing
Biomechanical evaluation of the constructs was performed using an Instron ElectroPuls E1000 Testing System (Instron). After repair but before testing was initiated, all specimens in both groups demonstrated 0 mm of gapping at the repair site. Specimens were mounted onto the testing system using custom tensile loading fixtures (Figure 2). Specimens were first pretensioned with 20 N for 30 seconds. Of note, all specimens had 0 mm of gapping after the pretensioning phase. They were then cyclically loaded between 20 and 100 N for 250 cycles at a frequency of 1 Hz. Next, the preload was decreased from 20 to 10 N and held for 30 seconds. Finally, the specimens were pulled in tension at a constant displacement rate of 20 mm/s until failure. Load and displacement data were collected digitally at a frequency of 100 Hz. This technique is similar to previous studies using human cadaveric specimens.8 The elongation during cyclic loading and the maximum failure load were recorded for each specimen. Maximum failure load was defined as the maximum value before sudden deviation on the load/displacement curve. To measure the amount of elongation, a mark was made at the tendon-bone interface and 1 cm distally in the patellar tendon. The elongation (gapping) was measured with a 0.01-mm dial caliper (Grainger). The mode of failure was recorded for each specimen. Statistical analysis was performed using a paired 2-tailed Student t test. Dependent variables included elongation between cycles 1 and 250 and maximum load to failure, with P < .05 used to determine statistical significance.
Figure 2.
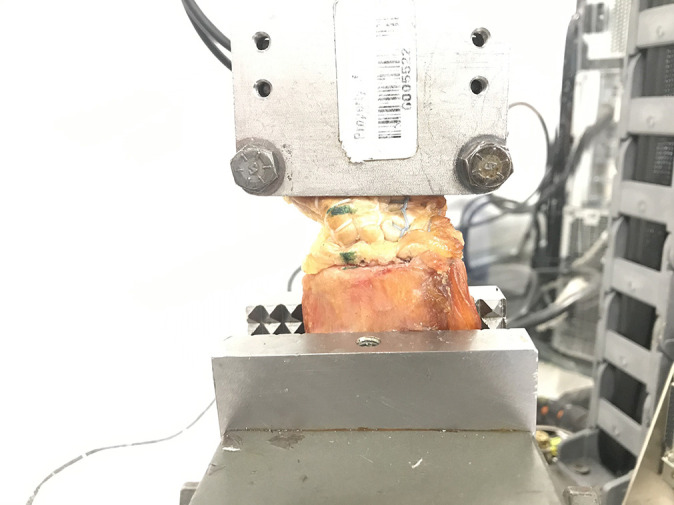
Testing setup for biomechanical evaluation using the ElectroPulsTM E1000 Testing System (Instron). The patellar tendon is clamped superiorly, and the patella is clamped inferiorly.
Results
Of the 5 paired extensor mechanisms harvested for this study, 4 specimens were male and 1 was female. The mean ± SD age was 58.4 ± 22.6 years. The mean T score of the patella from the DEXA testing was 0.46 ± 1.3 (Table 1).
TABLE 1.
Demographic Information for the Cadaveric Specimensa
| Sex | Age, y | Height, in | T Score |
|---|---|---|---|
| Female | 76 | 65 | 0.8 |
| Male | 31 | 70 | 2.5 |
| Male | 42 | 68 | –0.6 |
| Male | 85 | 69 | –0.5 |
| Male | 58 | 62 | 0.1 |
aBone quality for each case: normal.
Cyclic Loading
SA repair demonstrated less elongation (gapping) between cycles 1 and 250 when compared with TT repair. SA constructs had 6.83 ± 2.23 mm of gapping while TT had 13.30 ± 5.74 mm of gapping (P = .047). This difference was statistically significant (P < .05) (Table 2).
TABLE 2.
Biomechanical Testing: Suture Anchor vs Transosseous Tunnelsa
| Transosseous Tunnel | Suture Anchor | P Value | |
|---|---|---|---|
| Maximum load to failure, N | 288.19 ± 129.40 | 257.67 ± 104.64 | .69 |
| Cyclic elongation, mm | 13.30 ± 5.74 | 6.83 ± 2.23 | .047 |
aData are reported as mean ± SD. Bold P value indicates statistically significant difference between groups (P < .05).
Load to Failure
The maximum load to failure in the SA group was 257.67± 104.64 N as compared with 288.19 ± 129.40 N in the TT repair group. There was no statistically significant difference in the load to failure between the groups (P = .69) (Table 2).
Failure Mode
For the SA group, 4 of the 5 specimens failed at the suture-anchor interface, whereby the suture pulled out of the anchor but the anchor stayed in the bone. The remaining specimen failed by the anchor pulling out of the bone. For the TT group, 4 of the 5 specimens failed at the knot that secured the repair on the proximal aspect of the patella. The remaining specimen failed by the suture cutting out of the tendon at the Krackow stitch.
Discussion
In the present study, we performed a comparative biomechanical study evaluating TT and SA use in the setting of inferior pole patellar fractures treated with partial patellectomy and patellar tendon advancement. Our data reflected significantly less gap formation with the use of SA fixation with cyclic loading. Conversely, there was no difference in the maximal load to failure between SA repair and TT repair. When these findings are applied to clinical practice, it may be postulated that SA repair allows adequate time-zero strength for the repair. This may permit earlier range of motion given the reduced gap formation noted during cyclic loading. Clinically, SA may need a smaller incision, decrease the surgical time, and even minimize the risk of proximal patellar fracture, which may occur when drilling.3
Multiple studies have evaluated the biomechanical strength of SA repair with regard to patellar tendon ruptures.4,6,9,11,13 Using a porcine model, Lanzi et al9 found less gap formation and stronger load to failure in an SA group as compared with a TT group. Ettinger et al6 reported similar results in a human cadaveric model; however, techniques were slightly different (creation of tendon rupture 3 mm distal to the patella vs creation of an inferior pole of the patellar fracture), and SA repair had significantly higher maximum loads to failure. Sherman et al15 also used a cadaveric model and had similar results to the current study, with no difference in load to failure but decreased gapping in the SA group. While these studies are similar to ours, it is difficult to directly compare results. SAs in the current study are placed directly in cancellous bone to mimic a partial patellectomy, whereas in the referenced patellar tendon repair studies, the patella has an intact inferior cortex into which the anchor is placed, which may add some inherent strength as well as resistance to anchor pullout.
However, the literature is scarce in terms of examining TT versus SA repair for inferior pole patellar fractures treated with partial patellectomy and patellar tendon repair. Anand et al1 has conducted the only study to date investigating the role of SA in the treatment of comminuted distal pole of the patellar fracture. This retrospective clinical study examined patient-reported outcome measures and objective data (range of motion and strength), concluding that SAs were a viable option for fixation in a cancellous fracture bed of the inferior patella, as the authors reported no failures and had positive outcomes. However, the study was limited by the lack of a comparison group and a small sample size (5 patients). Despite these limitations, our study supports their findings, which suggests that SAs are a viable treatment option for inferior pole patellar fractures.
It is interesting to note that 4 of the 5 SAs failed as the result of suture breakage at the suture-anchor interface and only 1 anchor pulled out of bone. This was different from the mode of failure in the study by Ettinger et al,6 in which the titanium anchors either completely pulled out of the bone (5 specimens) or the suture itself pulled out of the tendon but the anchor stayed in bone (5 specimens). This difference may be due to the suture number and anchor design. The anchors in their study were double loaded, using 4 sutures, while the current study used single-loaded anchors using a total of 2 sutures. The 1 suture in the single-loaded SA may theoretically experience more force through the suture-anchor interface as opposed to the 2 sutures in the double-loaded SA, which may distribute the force between the 2 sutures. Therefore, this may increase the propensity for the suture to break at the interface in the single-loaded as opposed to the double-loaded anchor. It may also be related to the bone quality of the specimens. In the referenced studies, the authors did not include any data regarding the specimen demographics or the bone mineral densities.6 The failure method in our study demonstrates that the anchor purchase in the cancellous bone of the fracture bed may be strong enough to withstand the normal load seen at the patella–patellar tendon interface, which is typically 3 times the body weight throughout normal activities.11 Future research should consist of clinical randomized controlled trials comparing SA and other fixation strategies, including TT, for treating inferior pole patellar fracture to ensure that SAs are a safe and effective treatment option for patients with these injuries.
This study is not without limitations. As with any biomechanical study, this is a time-zero study and may not directly mimic the clinical scenario or the repeated loads that patients encounter during daily ambulation and physical therapy. The SA came preloaded with No. 2 Ultrabraid, while the TT used No. 2 FiberWire to repair the tendon. While these are both nonabsorbable ultrahigh molecular weight polyethylene sutures, there may be inherent biomechanical differences. Previous testing has shown that there is no difference in overall load to failure between these sutures, but Ultrabraid does show less secure knots when compared with those tied with FiberWire, according to Ilahi et al.2,7 The number of sutures and SA design may also play a role in repair strength and may be a limitation in this study. The SAs in this study were single loaded, utilizing 2 sutures overall (1 for each anchor). A double-loaded anchor with 4 sutures may have reduced the load on each suture and potentially transferred more load to the anchor-bone interface, possibly affecting the strength of the repair. Another limitation is that cadaveric specimens were used and the bone quality, despite having normal bone density, may not be equivalent to that of a living patient, so it is possible that results may differ in the clinical setting. In addition, patients who sustain these types of fracture patterns may have poor bone quality overall; therefore, the results of this study may not be generalizable to the general population. Furthermore, surgically created fracture may not reflect the biomechanical environment of a real fracture, although in the setting of our biomechanical study, with surrounding soft tissue stripped, this seems unlikely to have an effect on our results. The small sample size in the study was based on the availability of cadaveric tissue with adequate bone quality and repair supplies. However, an a priori power analysis did show that the study was adequately powered.
Conclusion
This biomechanical cadaveric study demonstrated that SA repair in the cancellous bone after inferior pole patellar fractures is comparable with repair with TTs in terms of pullout strength. SA repair showed less elongation with cyclic loading. This suggests that SA is a viable option for repair of the patellar tendon to the distal cancellous patella after partial patellectomy.
Acknowledgments
The authors acknowledge and thank Rachel Schilkowsky, BS, MEng, and Peter Wronski for their help with testing and specimen procurement.
Footnotes
Final revision submitted January 8, 2021; accepted February 23, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: D.F.W. has received hospitality payments from Stryker. B.D.O. is a paid consultant for Medical Device Business Systems, MTF/ConMed, Mitek, and Linvatec; has received honoraria from Vericel; and is a paid associate editor for The American Journal of Sports Medicine. S.F.D. has received hospitality payments from Medical Device Business Services and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1.Anand A, Kumar M, Kodikal G. Role of suture anchors in management of fractures of inferior pole of patella. Indian J Orthop. 2010;44(3):333–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bisson LJ, Manohar LM, Wilkins RD, Gurske-Deperio J, Ehrensberger MT. Influence of suture material on the biomechanical behavior of suture-tendon specimens: a controlled study in bovine rotator cuff. Am J Sports Med. 2008;36(5):907–912. [DOI] [PubMed] [Google Scholar]
- 3.Bonazza NA, Lewis GS, Lukosius EZ, Roush EP, Black KP, Dhawan A. Effect of transosseous tunnels on patella fracture risk after medial patellofemoral ligament reconstruction: a cadaveric study. Arthroscopy. 2018;34(2):513–518. [DOI] [PubMed] [Google Scholar]
- 4.Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: a biomechanical study. Am J Sports Med. 2006;34(9):1492–1499. [DOI] [PubMed] [Google Scholar]
- 5.Chang S-M, Ji X-L. Open reduction and internal fixation of displaced patella inferior pole fractures with anterior tension band wiring through cannulated screws. J Orthop Trauma. 2011;25(6):366–370. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger M, Dratzidis A, Hurschler C, et al. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: a cadaveric study. Am J Sports Med. 2013;41(11):2540–2544. [DOI] [PubMed] [Google Scholar]
- 7.Ilahi OA, Younas SA, Ho DM, Noble PC. Security of knots tied with Ethibond, Fiberwire, Orthocord, or Ultrabraid. Am J Sports Med. 2008;36(12):2407–2414. [DOI] [PubMed] [Google Scholar]
- 8.Joshi RR, Dwivedi R, Byanjankar S, Shrestha R. Outcome of inferior patellar pole avulsion fractures. J Lumbini Med Coll. 2016;4(2):84. [Google Scholar]
- 9.Lanzi JT, Felix J, Tucker CJ, et al. Comparison of the suture anchor and transosseous techniques for patellar tendon repair. Am J Sports Med. 2016;44(8):2076–2080. [DOI] [PubMed] [Google Scholar]
- 10.Larsen P, Court-Brown CM, Vedel JO, Vistrup S, Elsoe R. Incidence and epidemiology of patellar fractures. Orthopedics. 2016;39(6):e1154–e1158. [DOI] [PubMed] [Google Scholar]
- 11.Lighthart WA, Cohen DA, Levine RG, Parks BG, Boucher HR. Suture anchor versus suture through tunnel fixation for quadriceps tendon rupture: a biomechanical study. Orthopedics. 2008;31(5):441. [DOI] [PubMed] [Google Scholar]
- 12.Patel VR, Parks BG, Wang Y, Ebert FR, Jinnah RH. Fixation of patella fractures with braided polyester suture: a biomechanical study. Injury. 2000;31(1):1–6. [DOI] [PubMed] [Google Scholar]
- 13.Petri M, Dratzidis A, Brand S, et al. Suture anchor repair yields better biomechanical properties than transosseous sutures in ruptured quadriceps tendons. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1039–1045. [DOI] [PubMed] [Google Scholar]
- 14.Poukalova M, Yakacki CM, Guldberg RE, et al. Pullout strength of suture anchors: effect of mechanical properties of trabecular bone. J Biomech. 2010;43(6):1138–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherman SL, Black B, Mooberry MA, et al. Biomechanical evaluation of suture anchor versus transosseous tunnel patellar tendon repair techniques. J Knee Surg. 2019;32(8):825–832. [DOI] [PubMed] [Google Scholar]
- 16.Srikant K, Mishra D, Sinha V, Pradhan S. Management of comminuted extraarticular inferior pole patella fractures with partial patellectomy and patellar tendon repair by transosseous sutures. Int J Med Sci Public Heal. 2017;6(11):1. [Google Scholar]
- 17.Swensen S, Fisher N, Atanda A, Egol KA. Suture repair of a pole patella fracture. J Orthop Trauma. 2017;31(8):S28–S29. [DOI] [PubMed] [Google Scholar]
- 18.Veselko M, Kastelec M. Inferior patellar pole avulsion fractures: osteosynthesis compared with pole resection. Surgical technique. J Bone Joint Surg Am. 2005;87(suppl 1, pt 1):113–121. [DOI] [PubMed] [Google Scholar]


